Abstract
Background
Eliminating measles in Europe by 2015 is a WHO health goal. In Germany, physicians are legally required to report measles cases, yet it seems likely that reporting is less than universal. The goal of this study is to compare the number of measles cases that are reflected by data from the statutory health insurance (SHI) carriers with the number of physician-reported cases during and after a recent outbreak in the German state of North Rhine–Westphalia (NRW).
Methods
We analyzed the billing data of SHI carriers relating to measles in 2006 and 2007, as well as the measles cases that were reported in NRW over this period as required by law. We calculated the incidence of measles as the number of measles cases per 100 000 insurees (SHI carrier data) or per 100 000 persons in the overall population (reporting data).
Results
The measles outbreak in the first half of 2006 comprised 1713 measles cases according to the SHI data and 1665 cases that were reported as required by law (ratio, 1.02:1). From mid-2006 to the end of 2007, the SHI data reflected 821 cases, but only 349 cases were reported (ratio, 2.35:1). Younger patients were more commonly found among the cases reflected in the SHI data than among the reported cases.
Conclusion
Our study confirms that the system of legally mandated reporting underestimates the true number of measles cases, particularly in times when most cases are sporadic, and particularly in children who are less than 5 years old.
Eliminating measles in Europe by 2015 is a WHO health goal (1). This goal is achieved for a particular country if the incidence there is less than one case per million inhabitants. There must be no measles cases among the country’s inhabitants, and any measles arriving from abroad must not spread any further within the country. Successful elimination requires, on the one hand, a vaccination rate among the population of more than 95%, for two doses of vaccine, to offset vaccine failure and guarantee herd immunity for those who have not been vaccinated, and on the other hand, disease surveillance in which reporting of individual cases is as complete as possible, allowing targeted interventions by public health services.
According to Germany’s Law on Protection Against Infectious Diseases (Infektionsschutzgesetz, IfSG), suspected illness, illness, and death resulting from measles and laboratory confirmation of the measles virus must be reported to the appropriate health authority (2). On the basis of the case definition, the health authority decides which cases are to be reported to the Robert Koch Institute via the appropriate regional authorities. The case definition is fulfilled when there is a clinical case of measles (Box), measles has been confirmed by laboratory diagnosis, or a clinical/epidemiological relationship between a patient and a case of measles confirmed by laboratory diagnosis can be established (3).
Box. The Robert Koch Institute’s clinical case definition for measles (3).
Generalized rash (maculopapular) lasting more than 3 days and
Fever (above 38.5 °C [101.3 °F]) and
-
At least one of the following:
Cough
Head cold (runny nose)
Koplik spots
Conjunctivitis
In 2004, the Sentinel of Associations of Statutory Health Insurance Physicians (KV Sentinel), a joint project of Germany’s associations of statutory health insurance physicians (Kassenärztliche Vereinigungen, KVs) and the Robert Koch Institute, was established as a further disease surveillance tool. This provides the Robert Koch Institute with data on billed diagnoses of measles, whooping cough, chickenpox, mumps, and (since 2006) herpes zoster, and on performed vaccinations. This yields data on vaccination-preventable diseases and administered vaccinations from the whole population covered by statutory health insurance and being treated by a physician practicing in Germany or a physician authorized by an association of statutory health insurance physicians in a hospital. Data reporting by associations of statutory health insurance physicians to national and regional health reporting institutions for longer-term analysis is governed by the Social Security Code V, which came into force in 2003 (4). All 17 associations of statutory health insurance physicians (KVs) report their billing data to the Robert Koch Institute.
In 2006 there was a measles outbreak in the German state of North Rhine–Westphalia, in which cases increased in schools and public facilities in particular (5). It reached a peak between the 7th and 23rd weeks (February to June) of 2006 and was most severe in Duisburg (6).
Surveillance systems for infectious diseases generally reveal under-reporting. Data from the measles sentinel established in Switzerland in 1986 indicate incidence rates 2 to 36 times higher than reported (7). Comparable under-reporting is suspected for measles in Germany (8– 10). Thus this paper uses the measles cases in 2006 and 2007 in North Rhine–Westphalia to ascertain how many cases occurred according to the KV Sentinel and according to physician reporting as stipulated by the Law on Protection Against Infectious Diseases. It also examines whether the ratio between the two systems’ results varies depending on whether or not an outbreak is ongoing at the time.
Methods
Data from associations of statutory health insurance physicians
Data on measles diagnoses among 15.4 million people covered by statutory health insurance (85.5% of the population of North Rhine–Westphalia) were analyzed. The data were reported to the associations of statutory health insurance physicians in North Rhine and Westphalia–Lippe as part of quarterly billing by practicing physicians and physicians authorized by associations of statutory health insurance physicians in hospitals. After performing quality control the associations of statutory health insurance physicians sent anonymized data to the Robert Koch Institute. A detailed description of the methods used to gather, verify, and analyze the data submitted to the Robert Koch Institute is published elsewhere (11). The data set includes the following:
Month and year of birth
Sex
First three digits of postal code
Region of residence
Specialty of billing physician and region or borough of his/her practice
Quarter to which billing corresponds
ICD-10 code
Degree of certainty of diagnosis, diagnosis status.
Using the additional information on the degree of certainty of diagnoses, the categories “confirmed diagnosis,” “suspected,” “post-disease,” and “disease ruled out” can be established. Diagnosis status divides diagnoses into “acute” and “non-acute” and indicates whether a diagnosis was made during the quarter being billed or in a previous quarter.
Internal data validation took the form of verification of whether a case had already been diagnosed as measles with degree of certainty “confirmed diagnosis” or “post-disease” in 2004 (the beginning of data collection) or 2005.
If there were several ICD-10 codes for a single case, the most serious condition was used. Data sets that met the following criteria were considered to be measles:
ICD-10 code B05.0, B05.1, B05.2, B05.3, B05.4, B05.8, or B05.9
Degree of certainty of diagnosis “suspected” or “confirmed diagnosis”
Diagnosis status “acute”.
Only diagnoses from the data set which were made for the first time in 2006 or 2007 were taken into consideration.
Data according to the Law on Protection Against Infectious Diseases
The reported data concern individuals with both statutory and private health insurance as well as those with no insurance and those entitled to free health care. Cases were reported by the following:
Physicians working on an inpatient or outpatient basis
Community facility managers
Alternative practitioners
Pilots
Ships’ captains
Laboratory employees (2)
The data on measles cases submitted by health authorities to regional authorities as part of mandatory reporting, and by them to the Robert Koch Institute, included the following:
When reported
Symptom onset
Region or borough in which patient lives or usually resides
Patient age
Patient sex.
This research includes all cases in which symptoms began between January 1, 2006 and December 31, 2007. The time of reporting was used when the time of illness onset was unknown. Dual reporting has been ruled out, as health authorities examine, enter, and collate each individual case.
Calculating incidence rates
The incidence rate is calculated on the basis of the data from associations of statutory health insurance physicians as the number of documented measles diagnoses per 100 000 people covered by statutory health insurance in North Rhine–Westphalia (12). The KM 6 statistics (statutory health insurance: insured persons) of the German Federal Ministry of Health and the population statistics of the Federal Statistical Office for 2006 and 2007 were used to determine what proportion of North Rhine–Westphalia’s total population were covered by statutory health insurance (13). The annual incidence rate according to the Law on Protection Against Infectious Diseases is based on the number of reported measles cases per 100 000 inhabitants of North Rhine–Westphalia.
Statistical analysis
Differences between the measles incidence rates based on data from associations of statutory health insurance physicians and as reported according to the Law on Protection Against Infectious Diseases were tested using the chi-square test for statistical significance.
Results
During the period covered by the research, physicians billing as authorized by associations of statutory health insurance physicians diagnosed measles in 4653 patients in North Rhine–Westphalia. 2119 of these diagnoses were “suspected”, and 2534 were “confirmed” according to bills (Table 1). The most common ICD-10 code in the quarter in which a measles diagnosis was billed for the first time was B05.9, “measles without complication.” Complications occurred in 393 (15.5%) of patients with confirmed diagnoses. The most frequent complication was otitis. Of all measles diagnoses billed with associations of statutory health insurance physicians, 1160 (46%) were diagnosed by family doctors, 581 (23%) by pediatricians, and 309 (12%) by internal medicine specialists. The remaining 484 diagnoses were billed by other specialists (212, 8%) or physicians with several specialties (272, 11%).
Table 1. Billed measles diagnoses by ICD-10 code, with degree of certainty of diagnosis „confirmed diagnosis“ and „suspected“ in 2006 and 2007.
| ICD-10 code | Disease | Confirmed diagnoses (%) | Suspected diagnoses (%) |
| B05 | Measles | 7 (0.3) | 0 (0) |
| B05.0 | Measles complicated by encephalitis | 49 (1.9) | 23 (1.1) |
| B05.1 | Measles complicated by meningitis | 13 (0.5) | 2 (0.1) |
| B05.2 | Measles complicated by pneumonia | 35 (1.4) | 7 (0.3) |
| B05.3 | Measles complicated by otitis media | 225 (8.9) | 20 (0.9) |
| B05.4 | Measles with intestinal complications | 12 (0.5) | 2 (0.1) |
| B05.8 | Measles with other complications | 59 (2.3) | 35 (1.7) |
| B05.9 | Measles without complication | 2134 (84.2) | 2030 (95.8) |
| Total | 2534 (100) | 2119 (100) |
A total of 2014 measles cases were reported according to the Law on Protection Against Infectious Diseases in 2006 and 2007. Of these, around a third were confirmed by laboratory diagnosis. During the first half of 2006, the year of the measles outbreak, 1665 cases were reported according to the Law on Protection Against Infectious Diseases (Table 2). In the same period, 1713 confirmed cases of measles were billed. In the second half of 2006 and in 2007, when there were only sporadic measles cases, a total of 349 measles cases were reported to health authorities, but 821 confirmed cases of measles were recorded in documents of associations of statutory health insurance physicians.
Table 2. Number of measles cases in North Rhine–Westphalia by quarter, based on data from associations of statutory health insurance physicians (KV) and as reported according to the Law on Protection Against Infectious Diseases in 2006 and 2007 (outbreak shaded in beige).
| Quarter | Confirmed cases of measles (KV data) | Measles cases (report data) | Confirmed cases of measles (KV data) : measles cases (report data) ratio |
| 1st quarter 2006 | 618 | 608 | 1.02 : 1 |
| 2nd quarter 2006 | 1095 | 1057 | 1.04 : 1 |
| 3rd quarter 2006 | 170 | 84 | 2.02 : 1 |
| 4th quarter 2006 | 83 | 13 | 6.38 : 1 |
| 1st quarter 2007 | 166 | 53 | 3.13 : 1 |
| 2nd quarter 2007 | 224 | 188 | 1.19 : 1 |
| 3rd quarter 2007 | 90 | 9 | 10 : 1 |
| 4th quarter 2007 | 88 | 2 | 44 : 1 |
| Total | 2534 | 2014 | 1.26 : 1 |
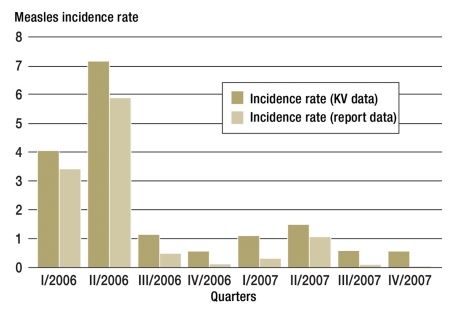
The outbreak in North Rhine–Westphalia came to a peak in the second quarter of 2006. In the first and second quarters of 2006 the incidence of confirmed cases of measles was 4.0 and 7.1 per 100 000 people covered by statutory health insurance, falling drastically in the following quarters (Figure). The cumulative measles incidence rate according to data from associations of statutory health insurance physicians was higher than the measles incidence rate as reported according to the Law on Protection Against Infectious Diseases, both during the outbreak in the first and second quarters of 2006 (11.1 per 100 000 and 9.2 per 100 000, p = 0.4) and for the third quarter of 2006 through the fourth quarter of 2007, after the outbreak (5.3 per 100 000 and 1.9 per 100 000, p <0.001).
Figure.
Measles incidence rates in North Rhine–Westphalia, 2006 and 2007; incidence rate (KV data) = confirmed measles diagnoses per 100 000 individuals with statutory health insurance; incidence rate (report data) = reported cases of measles, according to Germany’s Law on Protection Against Infectious Diseases, per 100 000 inhabitants. KV, association of statutory health insurance physicians
The most significant differences between data from associations of statutory health insurance physicians and data reported according to the Law on Protection Against Infectious Diseases are seen when measles cases are grouped by age (Table 3). While approximately 87% of billed measles diagnoses occurred in children less than 10 years old, this age group accounted for only 40% of the cases reported according to the Law on Protection Against Infectious Diseases (p <0.001). The age distribution within each of the data sources is the same both during and after the outbreak. The differing age distribution between the data sources, however, is unconnected with the outbreak. All patients with billed measles diagnoses were less than 40 years old. Of the 2014 new cases reported to health authorities, 1950 (97%) were in patients aged under 40.
Table 3. Measles diagnoses described as confirmed in bills according to KV data and measles cases reported according to the Law on Protection Against Infectious Diseases, by age, in North RhineWestphalia in 2006 and 2007.
| Age (years) | No. (%) of confirmed KV diagnoses | No. (%) of cases reported according to the Law on Protection Against Infectious Diseases |
| <5 | 1747 (69%) | 419 (21%) |
| 5 to 9 | 486 (18%) | 385 (19%) |
| 10 to 14 | 196 (8%) | 492 (24%) |
| 15 to 19 | 91 (4%) | 344 (17%) |
| 20 to 24 | 13 (1%) | 117 (6%) |
| ≥25 | 1 (<1%) | 257 (13%) |
| Total | 2534 (100%) | 2014 (100%) |
KV, association of statutory health insurance physicians
Discussion
Eliminating measles by 2015 is a health target established in Germany. Early diagnosis and prevention of further cases are necessary if this goal is to be achieved. Reporting of individual cases must be as complete as possible so that the first, isolated measles case and anyone who has come into contact with the patient can be monitored. Action such as vaccination can then be taken to prevent further spread of measles. Physicians have a key role to play in this. When cases are reported by physicians, the appropriate health authority is able to begin background investigations early on and to carry out post-exposure vaccinations.
The essential questions addressed by the study were how many measles cases had been reported through the KV Sentinel and through the reporting system according to the Law on Protection Against Infectious Diseases, and whether the data-gathering systems differed from each other during an outbreak and when there was no outbreak. During the 2006 outbreak in North Rhine–Westphalia, the numbers of cases reported and billed by physicians were almost the same. It seems likely that the extensive media coverage of the 2006 measles outbreak, particularly in connection with the Soccer World Cup, raised physicians’ awareness of their duty to report measles cases. In addition, the need and importance of reporting measles cases to the appropriate health authority probably seemed greater in the context of an outbreak.
However, when comparing the two data-collection systems it should be remembered that certain population groups are not part of the study population of the KV Sentinel and are therefore not included in the data. These groups include the following:
Those with private health insurance
Those with voluntary health insurance
Residents of North Rhine–Westphalia who are entitled to free health care (e.g. federal police officers, firefighters, soldiers, and those carrying out civilian service)
Those without insurance.
In contrast, measles cases reported according to the Law on Protection Against Infectious Diseases include suspected and confirmed cases of measles among all individuals living in Germany, as reported by physicians working on an inpatient or outpatient basis, community facility managers, alternative practitioners, pilots, and ships’ captains (2). Under-reporting of measles is therefore probably more extensive than indicated here. The fact that measles was under-reported during the outbreak has also been shown in an earlier study on the outbreak. In one school in Duisburg, a total of 53 children fell ill in 2006, but only 27 (50.9%) were reported to the appropriate health authority (6). This made the health authority’s task of informing those who had come into contact with patients more difficult.
When there are only isolated cases of measles, as in the second half of 2006 and in 2007, the incidence rate calculated on the basis of the number of measles diagnoses billed was around three times as high as the measles incidence rate according to the number of cases reported in line with the Law on Protection Against Infectious Diseases. Sporadically-occurring measles is therefore being significantly under-reported in terms of mandatory reporting. This could be because reporting sporadic cases is seen as less important than reporting during an outbreak. When asked in a questionnaire why cases of infectious diseases had not been reported as required, physicians gave the following reasons:
Forgot to report
Lack of habit
Unsure whether an infection had to be reported
Lack of time
Complicated procedure (14).
Analysis of billing data shows that most measles diagnoses billed occur in children less than 5 years old, although half of all reported measles cases are in children and young people of school age. The reasons for this discrepancy are unclear. The conjecture that children of school age are admitted to hospital with complications more often than children aged under 5 and are therefore reported by hospital physicians (who do not bill with associations of statutory health insurance physicians) could not be confirmed by subsidiary analysis. The extent to which patients more than 10 years old with private insurance contracted measles and as a result were reported according to the Law on Protection Against Infectious Diseases but not billed by physicians authorized by associations of statutory health insurance physicians remains unclear. Health authorities’ own investigations or reports by community facility managers made only an insignificant contribution to the discrepancy. The reasons for the age group–specific differences in reporting and diagnosis behavior must therefore be discussed further.
In order to come closer to eliminating measles, the rate of new cases must be reduced. Early diagnosis of measles and measles vaccination, including post-exposure vaccination, play an important part in this. 2008 school entry medical examinations showed that the WHO goal of at least 95% take-up for the first measles vaccination has been achieved in Germany. However, most regions of Germany still lag far behind 95% take-up for the second measles vaccination (15). Due to Germany’s uneven vaccination, it has one of the highest measles incidence rates in Europe (16).
Conclusion and recommendations
The results of this study confirm that measles is being under-reported in Germany even though reporting is mandatory, particularly when measles cases are sporadic. Under-reporting is greatest in children less than 5 years old. In order to achieve the goal of eliminating measles, physicians can play a key role in two ways: On the one hand, they can stress the importance of measles vaccination to parents, in conversation, on the other, measures to prevent the spread of measles can only be taken if treating physicians observe their legal obligation to report all suspected or confirmed cases of measles to the appropriate health authority.
Acknowledgments
Translated from the original German by Caroline Devitt, MA.
Footnotes
Conflict of interest statement
The authors declare that no conflict of interest exists.
References
- 1.World Health Organization Europe. Renewed commitment to elimination of measles and rubella and prevention of congenital rubella syndrome by 2015 and sustained support for polio-free status in the WHO European Region (EUR/RC60/R12) Moscow 13-16 September 2010. www.euro.who.int/__data/assets/pdf_file/0016/122236/RC60_eRes12.pdf [Google Scholar]
- 2.Gesetz zur Neuordnung seuchenrechtlicher Vorschriften (Seuchenrechtsneuordnungsgesetz - SeuchRNeuG) vom 20. Juli 2000. Artikel 1 Gesetz zur Verhütung und Bekämpfung von Infektionskrankheiten beim Menschen (Infektionsschutzgesetz - IfSG) Fundstelle BGBl. I S. 1045 2000 [Google Scholar]
- 3.Robert Koch-Institut. Falldefinitionen des Robert Koch-Instituts zur Übermittlung von Erkrankungs- oder Todesfällen und Nachweisen von Krankheitserregern, Ausgabe 2007, gemäß § 4 Abs. 2 des Gesetzes zur Verhütung und Bekämpfung von Infektionskrankheiten beim Menschen (Infektionsschutzgesetz - IfSG) www.rki.de/cln_178/nn_200532/DE/Content/Infekt/IfSG/Falldefinition/IfSG/Falldefinition,templateId=raw,property=publicationFile.pdf/Falldefinition.pdf [Google Scholar]
- 4.Sozialgesetzbuch (SGB) Fünftes Buch (V) Berlin: 2008. Gesetzliche Krankenversicherung. § 303f Datenverarbeitung und -nutzung. [Google Scholar]
- 5.Schröter M, Wichmann O, Santibanez S, van Treeck U. Erfahrungen mit dem Masernausbruch NRW 2006. Westfälisches Ärzteblatt. 2007;07:23–25. [Google Scholar]
- 6.Wichmann O, Hellenbrand W, Sagebiel D, et al. Large measles outbreak at a German public school, 2006. Pediatric Infectious Disease Journal. 2007;26:782–786. doi: 10.1097/INF.0b013e318060aca1. [DOI] [PubMed] [Google Scholar]
- 7.Richard JL, Vidondo B, Mausezahl M. A 5-year comparison of performance of sentinel and mandatory notification surveillance systems for measles in Switzerland. Eur J Epidemiol. 2008;23:55–65. doi: 10.1007/s10654-007-9187-1. [DOI] [PubMed] [Google Scholar]
- 8.Hauri AM, Westbrock HJ, Fitzenberger J, Dreesman J. Untersuchung eines Listeriose-Clusters: Wie vollständig sind Labormeldungen? Gesundheitswesen. 2004;66:779–782. doi: 10.1055/s-2004-813822. [DOI] [PubMed] [Google Scholar]
- 9.Robert Koch-Institut. Impfquoten bei der Schuleingangsuntersuchung in Deutschland 2006. Epid Bull. 2008;7:55–57. [Google Scholar]
- 10.Schrauder A, Claus H, Elias J, Vogel U, Haas W, Hellenbrand W. Capture-recapture analysis to estimate the incidence of invasive meningococcal disease in Germany, 2003. Epidemiology and Infection. 2007;135:657–664. doi: 10.1017/S0950268806007151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reuss A, Feig M, Kappelmayer L, Eckmanns T, Poggensee G. Bestimmung von Impfquoten und Inzidenzen von Erkrankungen anhand von Daten der Kassenärztlichen Vereinigungen. Gesundheitswesen. 2010;72:340–346. doi: 10.1055/s-0030-1249691. [DOI] [PubMed] [Google Scholar]
- 12.Bundesministerium für Gesundheit. Statistik über Versicherte, gegliedert nach Status, Alter, Wohnort, Kassenart. www.bmg.bund.de/cln_160/nn_1193098/SharedDocs/Downloads/DE/Statistiken/Gesetzliche-Krankenversicherung/Mitglieder-und-Versicherte/2006-km6-lang-pdf.html. 2006 [Google Scholar]
- 13.Statistisches Bundesamt. Bevölkerung am 311 2. nach Geschlecht und Staatsangehörigkeit 2003 bis 2006. www.destatis.de/jetspeed/portal/cms/Sites/destatis/Internet/DE/Content/Statistiken/Bevoelkerung/Bevoelkerungsstand/Tabellen/Content50/GeschlechtStaatsangehoerigkeit,templateId=renderPrint.psml. 2007 [Google Scholar]
- 14.Klöckner G. Infektionskrankheiten-Aspekte der Meldepflicht, ein Beitrag zur Erfassung von Infektionskrankheiten durch die Arztmeldepflicht unter besonderer Berücksichtigung einer vergleichenden Befragung von Ärzten. http://nbn-resolvingde/urn:nbn:de:hbz:5M-06225. 2005 [Google Scholar]
- 15.Robert Koch-Institut. Impfquoten bei den Schuleingangsuntersuchungen in Deutschland 2008. Epid Bull. 2010;161:37–40. [Google Scholar]
- 16.Muscat M, Bang H, Wohlfahrt J, Glismann S, Molbak K. Measles in Europe: an epidemiological assessment. Lancet. 2009;373:383–389. doi: 10.1016/S0140-6736(08)61849-8. [DOI] [PubMed] [Google Scholar]