Abstract
This study examined risk and determinants of rehospitalization of children and adolescents (n = 186) following a first psychiatric hospitalization. It specifically examined the role of post-discharge services. Data were collected for a 30-month follow-up period through structured telephone interviews with caregivers and case record abstractions. 43% of youth experienced readmissions during the follow-up period. Risk of rehospitalization was highest during the first 30 days following discharge and remained elevated for 3 months. 72% of youth received 284 post-discharge services during the follow-up period, which significantly reduced the risk of rehospitalization. Longer first hospitalizations and a higher risk score at admission increased risk.
Keywords: Psychiatric rehospitalization, Psychiatric readmission, Inpatient psychiatric care, Post-discharge services, Aftercare services
Introduction
Inpatient psychiatric hospitalization remains the most costly and restrictive intervention available for children and adolescents with severe emotional disorders (SED) (Stroul and Friedman 1986). In 2000, there were 100,000 inpatient psychiatric episodes among children and adolescents in the United States (Owens et al. 2003). Readmission into inpatient psychiatric care is considered a particularly unfavorable outcome for several reasons. (1) Rehospitalizations are costly, both in terms of dollars spent as well as stress exacted on the children and families involved (Causey et al. 1998). (2) Rehospitalizations raise questions about the effectiveness of inpatient psychiatric treatment itself (Fontanella et al. 2006) and the availability and utilization of effective community-based aftercare services (e.g., Burns and Hoagwood 2002; Nierman and Lyons 2001). (3) Rehospitalization rates have increased significantly since the adoption of managed care. Prior to this event, about one-quarter of youth experienced read-missions within 1 year of discharge (e.g., Parham et al. 1987; Pfeffer et al. 1992; Segal et al. 1995; Solomon et al. 1993). More recent rates range between 30 and 50% across studies (Arnold et al. 2003; Blader 2004; Dickey et al. 2001; Fontanella et al. 2006; Heggestad 2001; Lien 2002; Saunders and Heflinger 2003). As such, rehospitalizations are viewed as a target for quality improvement within child-serving systems of care, and knowledge about how to reduce their occurrence is crucial.
Post-Discharge Services
Among the factors that may be associated with higher rehospitalization rates, the role of post-discharge services is perhaps of greatest interest to mental health providers because development of and linkages to such services are both promising and costly, and would therefore have important service delivery and policy implications (Daniel et al. 2004; Pottick et al. 1993). However, studies of post-discharge services in the context of inpatient psychiatric care remain scant, and findings are equivocal (Daniel et al. 2004).
Romansky et al. (2003) examined service reports and clinical ratings of 500 randomly selected psychiatrically hospitalized children and adolescents in the Illinois child welfare system. Results revealed that rehospitalized youth when compared to non-rehospitalized youth had received fewer aftercare service hours. A much earlier study (Solomon et al. 1993) investigated the use of community services by 62 psychiatrically hospitalized youth and found that when compared with post-discharge service receivers, a higher proportion of non-receivers were rehospitalized. In addition, results of the study pointed to high rates of rehospitalization even among those who did receive post-discharge services and raised questions about the appropriateness of both hospital and post-discharge treatment.
Other studies have failed to find an association between post-discharge service use and rehospitalization. Blader (2004) reported that less involvement in aftercare services did not increase rehospitalization risk. Interestingly, children not involved in psychotherapy had lower rates of rehospitalization, which, according to the investigator, suggests the need for appropriate matching of care to need. Previously, Foster (1999) focused on the effect of aftercare services on psychiatric rehospitalization as part of the Fort Bragg Demonstration Project. Using insurance claims data, the study examined psychiatric readmissions for 204 youth. The study failed to identify a relationship between aftercare services and risk of readmission. A study by Pavkov et al. (1997) concluded that after controlling for demographic and clinical factors, service factors, i.e., an organized array of community-based mental health services, did not decrease the likelihood of rehospitalization.
The scant and inconclusive literature further suggests that a study of post-discharge services might have to include distinctions between different types of services. For instance, Fontanella (2008) found that youths discharged to lower levels of care were significantly more likely to be rehospitalized compared to those discharged to residential treatment.
Other Predictors of Psychiatric Rehospitalization Among Children and Adolescents
A number of studies have investigated the role of child, family and service factors in the rate and timing of psychiatric rehospitalizations, with renewed interest in this area reflected in several studies published during the last 5 years (e.g., Blader 2004, 2006, 2007; Bobier and Warwick 2005; Chung et al. 2008; Fontanella 2008; Fontanella et al. 2006, 2008). The reader is referred to these studies for in-depth reviews of the literature on various predictors of rehospitalization. Altogether, findings about the effects of child, family and service factors on psychiatric rehospitalization have been inconsistent depending on operational definitions of rehospitalization, study design, nature of the sample, data sources and combination of predictors used (Fontanella 2008).
The most consistent predictors of rehospitalization have been clinical factors, such as diagnosis, symptom severity, co-morbidity or suicidal behavior (Arnold et al. 2003; Blader 2004; Fontanella 2008; Romansky et al. 2003). With regard to demographic or other nonclinical child characteristics, findings are contradictory. For instance, both younger age at admission (Arnold et al. 2003; Bobier and Warwick 2005; Pavkov et al. 1997) as well as older age (Fontanella 2008; Foster 1999) have been reported as increasing the risk of rehospitalization. A few studies have investigated parental factors in relation to rehospitalization. Most found lower rates of readmission with higher rates of parental involvement, whether parental influence was operationalized as increased involvement or engagement (Brinkmeyer et al. 2004; Chung et al. 2008; Lakin et al. 2004) or as parental satisfaction with care (Brinkmeyer et al. 2004). Beyond post-discharge services, several other treatment or service factors have been linked to higher rehospitalization rates, such as prior hospitalizations, stays in residential treatment facilities (Chung et al. 2008; Fontanella 2008; Pavkov et al. 1997; Romansky et al. 2003), longer length of stay during hospitalization (Fontanella 2008) and medication non-adherence (Bobier and Warwick 2005). Fontanella (2008) found significant differences in rehospitalization rates between different hospital providers after controlling for other salient child, family and treatment variables, perhaps suggesting that contextual factors, such as organizational policies and structures might also impact the likelihood of rehospitalization.
Purpose of Current Study
The current study had two specific aims that built upon the current research but also improved on methodological short-comings of prior work. First, it aimed to examine the risk of rehospitalization of children and youth within 2½ years of their first psychiatric hospitalization, and secondly, it investigated the association between post-discharge services and risk of rehospitalization after controlling for salient child, family and service use variables.
The study improved on prior work in several important ways. (1) It collected detailed post-discharge services data, using a standardized instrument (Child and Adolescent Services Assessment [CASA]) (Ascher et al. 1996). (2) It extended the follow-up period to 30 months (2½ years) following a first psychiatric hospitalization. (3) It controlled for the effect of prior hospitalizations and subsequent interventions by including only children and adolescents with a first psychiatric hospitalization. Controlling statistically for the effect of prior hospitalizations (as has been done in most studies) is problematic as a prior hospitalization might lead to a host of “interventions” (e.g., post-discharge services, medication treatment, increased family involvement) that may further modify the relationship and would have to be accounted for to derive unbiased estimates.
Methods
Setting
The study was conducted at a large private nonprofit psychiatric facility located in the Southwest of the US, providing a full range of mental health services across all age groups, including inpatient and intensive outpatient treatment. This 89-bed facility is one of two remaining comprehensive psychiatric facilities in the largest county in the United States, and the only one in a smaller region in the county offering care to children under 13 years of age. The facility has 29 beds for its child and adolescent programs. The majority of the patients hold private insurance; approximately 20% are admitted through public insurance. More than 50% of the patient population is white, followed by Hispanic, African-American and Asian.
Study Participants and Sampling Procedures
The study collected data on 200 child and adolescent cases that experienced their first psychiatric hospitalization between January 1, 2002 and December 31, 2005. This period was chosen to allow examination of rehospitalization and post-discharge services over the 24-month period following discharge. Due to a longer than expected data collection period, we were able to extend this period to 30 months or 2½ years.
About 3,500 children and adolescents had been psychiatrically hospitalized for the first time during the specified study period and were eligible for inclusion into the study. After eliminating cases with insufficient contact information, the final sampling frame consisted of 3,341 cases. Cases were initially randomly sampled from the sampling frame. However, in order to secure a sample size of 200, which was our target sample size, all 3,341 cases had to be contacted, which means that we utilized the full sample. We were unable to establish contact with 3,141 cases for a range of reasons, but primarily due to disconnected or wrong numbers and ‘no answers.’ Once contact was established, about one-fifth of eligible subjects declined to participate. Of the 200 cases successfully recruited into the study, 11 cases were lost as it was determined that prior hospitalizations had occurred; an additional 3 cases could not be used due to missing case records, yielding a final sample size of 186.
Missing Data
Regulations under the Health Information Portability and Accountability Act (HIPAA) (U.S. Department of Health and Human Services 1996) prevented us from obtaining case record data on patients who had not consented to be in the study. This hampered our ability to conduct sensitivity analyses about missing cases. However, basic contact information provided some insight into differences between our final sample and otherwise eligible cases. We randomly chose 200 missing cases and entered data on the few available variables. There were no differences in terms of gender distribution. However, missing cases were about 1 year older at the time of their first psychiatric hospitalization (mean = 14.52; SD = 3.00) than cases in our sample (mean = 13.59; SD = 2.84) (P < .01). We were unable to determine differences in racial/ethnic background as the initial contact information sheet provides such information unreliably. There were no differences in terms of the lengths of stay during the first hospitalization. The rate of rehospitalization at the index facility was similar for the two groups.
Study Design and Procedures
This prospective observational cohort study involved two data collection phases—interviews with caregivers (Phase I) and case record abstractions (Phase II). All study methods and procedures were reviewed and approved by the Institutional Review Board at Loma Linda University, and subsequently pilot tested. The intervals between discharge following the first psychiatric hospitalization and data collection varied across respondents; however, follow-up data was collected for all respondents for a 30-month period following the first psychiatric hospitalization.
Phase I commenced in June 2007 and took 13 months. In this phase, caregivers of former child patients were contacted after having been randomly selected from the sampling frame. In cases where former child patients had reached adulthood (age 18 and above), we contacted them directly and obtained consent for study participation, which also included obtaining permission to subsequently access the former child patient’s case record. Attempts to collect data on youth who were currently in foster or group care were abandoned given difficulties of identifying a worker or caregiver who would be able to provide reliable information on the youth’s mental health services history. After obtaining consent and determining that the eligibility criterion (i.e., first psychiatric hospitalization) was met, telephone interviews were conducted in both English and Spanish by trained graduate student interviewers. This phase involved the collection of post-discharge services data, using the follow-up version of the Child and Adolescent Services Assessment [CASA] (Ascher et al. 1996). We also asked a few questions about the family’s involvement during the child’s inpatient stay, such as ‘During the time your child was first hospitalized, were you ever invited by hospital staff to participate in (a) family therapy, (b) treatment planning, (c) discharge planning, (d) other unit activities?’ and ‘How frequently did you visit your child?’ Interviews took an average of 40 min.
In Phase II, we conducted case record abstractions. Using a standardized case record abstraction instrument, developed and pilot-tested based on an earlier review of the case record, trained graduate level students abstracted demographic, diagnostic and historical background information about each study participant. It should be noted that case record data are based on ‘usual care’ intake/discharge clinical and psychosocial assessments conducted with the index child and his/her family. Case abstraction was also used to verify the participants’ study eligibility. Case record reviews took an average of 45–60 min. Interrater reliability was checked after 20 case records had been reviewed. The process involved randomly choosing 5 case records for independent review by each abstractor. The goal was to establish a 90% agreement rate. The pre-established guideline specified that coders would be retrained should interrater reliability fall below 90%. It was determined to be at K = 0.94.
Variables and Measures
Dependent Variable
The dependent variable ‘rehospitalization’ was a categorical variable (yes/no) and was derived from both interview data and hospital case records. Given that the psychiatric facility is one of only two in the area, the vast majority of rehospitalizations occurred at the index facility. If a child had been rehospitalized elsewhere, Phase I interviews provided that information.
Main Covariate: Post-Discharge Services
The Child and Adolescent Services Assessment [CASA] (Ascher et al. 1996) follow-up version was used in Phase I to collect post-discharge mental health services data. The original CASA is a self-report instrument with both child and parent versions that assesses use of mental health services by children and adolescents, ages 8–18 years. The CASA has good psychometric properties with reliability being the highest for reporting on the most restrictive settings (Ascher et al. 1996). The follow-up interview was developed by its authors to facilitate collection of services data across time (Ascher et al. 1996). It commences with an update of information about the patient which included the current address, phone number, school, and whether the child has lived with the parent or caretaker in the intervening period. Respondents are asked whether the child used any of the services on the CASA services screen “over the past 3 months or since the last interview.” For purposes of our study, the wording was changed to “since the first hospitalization.” Post-discharge services received at the index facility, could additionally be derived from case record review. As we were interested in the association between post-discharge services and rehospitalization, the current study reports on post-discharge services until (1) the first rehospitalization, or (2) the end of the follow-up study period (30 months) in the event rehospitalization did not occur.
We collected data on a range of post-discharge services, varying in type, intensity and duration. A few services require additional explanation: Partial hospitalization (PH) is a highly structured therapeutic day treatment program lasting 6 h, 5 days per week, and is offered at the index facility. Patients attend this program, including school, on-site, but return to their family in the evening. Partial hospitalization is intended as a step-down program following an inpatient episode or as a way to prevent hospitalization. The Intensive Outpatient Program (IOP) offers treatment for the child or adolescent and his/her family 2–3 times a week for 3 h each time. Treatment is provided in a group format but is tailored to individual family needs. This program also offers chemical dependency and dual diagnosis tracks where applicable. Since these two services (PH and IOP) were exclusively provided at the index facility, case record data provided information about their use. Follow-up interviews confirmed information about these intensive mental health services and provided additional information about other types of post-discharge services, such as weekly or biweekly mental health outpatient treatment, school counseling, religious support, or involvement with service systems, such as juvenile justice or child welfare.
Other Covariates
All other covariates (except for the covariate family involvement) are based on case record data. Sociodemographic data included gender (male/female), race (white, Black, Hispanic, other; for multivariate analysis, this covariate was dichotomized—white/nonwhite—to avoid empty or small cell sizes), and age at first admission. A risk factor score (range 0–6) was derived from six known psychosocial risk factors: (1) abuse/violence history; (2) history of abandonment; (3) adopted; (4) academic functioning below average/failing; (5) family history of mental illness and/or drug abuse; (6) head trauma and/or seizures. We used 5 clinical and/or treatment variables: (1) Axis I discharge diagnosis (diagnoses could be classified into three mutually exclusive groups: mood disorders; disorders of conduct and impulse control; mixed mood disorder and conduct/impulse control disorders); (2) Axis V discharge GAF score as an indicator of functional impairment;1 (3) length of stay during first hospitalization—continuous variable measured in days; (4) alcohol/ drug use—this variable was based on the initial assessment and/or psychosocial history taken during the first hospitalization in the case record. Current alcohol/drug use was indicated either through diagnosis or narrative. (5) Family involvement during 1st hospitalization—based on interview data; this was a categorical (yes/no) variable computed out of the following questions: “During your child’s first psychiatric hospitalization, did you participate in (a) family therapy; (b) treatment planning; (3) discharge planning; or (4) other.”2
Data Analysis
Descriptive analyses were conducted to determine the timing, rate and number of rehospitalizations. Survival analytic methods not only model the rate at which an event occurs and what factors are associated with the occurrence of the event (e.g., Allison 1984; Singer and Willett 2003), but also provide a mechanism for addressing censored cases that do not experience the event within the study period. The use of these censored events is particularly appropriate for this investigation, as 57.0% of cases did not experience a rehospitalization (“Results”). The life table, survival distribution, and Kaplan–Meier survival function estimation are all descriptive methods for estimating the distribution of survival times from a sample and were calculated in this study. This study also calculated the hazard rate of rehospitalization, which is defined as the probability per time unit that a case that has survived to the beginning of the respective interval will fail in that interval (Allison 1984).
We tested relationships between covariates and conducted bivariate analyses, using chi-square and t-tests. Subsequently, Cox regression was used to investigate the effect of post-discharge services on the risk of rehospitalization controlling for salient covariates. While Cox regression is not based on any assumptions concerning the nature or shape of the underlying survival distribution, it does assume that the effects of the predictor variables upon survival are constant over time and are additive in one scale. Testing of the proportionality assumption indicated no violations and Cox regression was conducted with covariates entered in blocks using the ENTER procedure. All analyses were conducted using SPSS 17.0.
Results
Descriptive Findings
Sample Description
More than half of our sample was female (53.2%) and white (62.4%). The average age of admission was 13.6 (SD = 2.8). Table 1 presents the remaining characteristics of the study sample. We also looked at the year in which the child or adolescent was first hospitalized. Only seven youth (3.8%) experienced their first hospitalization in 2002; almost equal numbers of participants were recruited from years 2003 (59, 31.7%), 2004 (59, 31.7%), and 2005 (61, 32.8%).
Table 1.
Sample characteristics and bivariate findings by rehospitalization status (n = 186)
| Total | Rehospitalizationa |
P | ||
|---|---|---|---|---|
| Yes N (%) or mean (SD) |
No N (%) or mean (SD) |
|||
| Sociodemographics | ||||
| Gender | .444 | |||
| Male | 87 (46.8) | 40 (46.0) | 47 (54.0) | |
| Female | 99 (53.2) | 40 (40.4) | 59 (59.6) | |
| Race | .592 | |||
| Caucasian | 116 (62.4) | 52 (44.8) | 64 (55.2) | |
| Black | 12 (6.5) | 6 (50.0) | 6 (50.0) | |
| Hispanic | 46 (24.7) | 16 (34.8) | 30 (65.2) | |
| Other | 12 (6.5) | 6 (50.0) | 6 (50.0) | |
| Age at 1st admission | 13.6 (2.8) | 13.0 (2.8) | 14.1 (2.8) | .008 |
| Living situation at time of 1st hospitalization | .092 | |||
| Bio/adoptive parents | 91 (48.9) | 34 (37.4) | 57 (62.6) | |
| One bio/adoptive parent | 52 (28.0) | 21 (40.4) | 31 (59.6) | |
| Extended family | 30 (16.1) | 19 (63.3) | 11 (36.7) | |
| Foster care/group home | 13 (7.0) | 6 (46.2) | 7 (53.8) | |
| Psychosocial risk factors | ||||
| Risk factor index | 2.3 (1.1) | 2.5 (0.9) | 2.1 (1.2) | .030 |
| Clinical/treatment variables | ||||
| Discharge Axis I diagnosis | .672 | |||
| Mood disorder | 119 (64.3%) | 50 (42.0%) | 69 (58.0%) | |
| Conduct/impulse disorder | 32 (17.3%) | 13 (40.6%) | 19 (59.4%) | |
| Both mood and conduct | 34 (18.4%) | 17 (50.0%) | 17 (50.0%) | |
| Discharge GAF score | 44.0 (9.1) | 44.1 (8.5) | 43.9 (9.6) | .896 |
| Days hospitalized | 5.5 (2.7) | 6.2 (2.8) | 5.0 (2.5) | .002 |
| Current alcohol use | .587 | |||
| Yes | 61 (32.8) | 23 (37.7) | 38 (62.3) | |
| No | 118 (63.4) | 54 (45.8) | 64 (54.2) | |
| DK | 7 (3.8) | 3 (42.9) | 4 (57.1) | |
| Family involvement | .073 | |||
| Yes | 110 (59.1) | 51 (46.4) | 59 (53.6) | |
| No | 62 (33.3) | 27 (43.5) | 35 (56.5) | |
| DK | 14 (7.5) | 2 (14.3) | 12 (85.7) | |
| Post-discharge services | ||||
| Post-discharge services | .000 | |||
| Intensive & nonintensive | 32 (17.1) | 10 (31.2) | 22 (68.8) | |
| Intensive MH | 20 (10.8) | 13 (65.0) | 7 (35.0) | |
| Nonintensive MH | 69 (37.1) | 20 (29.0) | 49 (71.0) | |
| Other Supportive | 13 (7.0) | 4 (30.8) | 9 (69.2) | |
| None | 52 (28.0) | 33 (63.5) | 19 (36.5) | |
For bivariate results, row percentages are reported
Post-Discharge Services
For this analysis, post-discharge services are reported following the child’s first psychiatric hospitalization until a rehospitalization occurred or the end of the study period (30 months) if rehospitalization did not occur. Respondents reported 284 post-discharge services during that period, encompassing services such as intensive mental health services, traditional weekly or biweekly outpatient therapy as well as involvement with child-serving systems (Table 2). Youth received from 0 to 6 services, with an average of 1.5 services (SD = 1.4).
Table 2.
Post-discharge services between 1st psychiatric hospitalization and (1) rehospitalization or (2) the end of the 30-month follow-up period
| Types of services | n (%) |
|---|---|
| Intensive MH services | |
| Partial hospitalization | 18 (6.34) |
| Intensive outpatient | 48 (16.90) |
| Residential treatment | 2 (0.07) |
| Intensive MH services total | 68 (23.94) |
| Non-intensive MH services | |
| Regular outpatient therapy | 101 (35.56) |
| Outpatient drug/alcohol treatment | 7 (2.46) |
| Wraparound services | 2 (0.70) |
| Anger management | 2 (0.70) |
| Behavior modification treatment | 1 (0.35) |
| Home-based counseling | 5 (1.76) |
| Therapy for sexual perpetration | 1 (0.35) |
| Non-intensive MH services total | 119 (41.90) |
| Other services | |
| School counseling | 40 (14.08) |
| Religious support | 14 (4.93) |
| AA/NA self-help group | 1 (0.35) |
| Informal counseling | 4 (1.41) |
| Foster care | 5 (1.76) |
| Group home care | 5 (1.76) |
| Crisis (mobile) team | 1 (0.35) |
| Respite care | 1 (0.35) |
| Involvement with child welfare | 2 (0.70) |
| Involvement with juvenile justice/probation | 19 (6.69) |
| Neurological/developmental services | 3 (1.06) |
| Mentoring | 1 (0.35) |
| Case management | 1 (0.35) |
| Other services total | 97 (34.15) |
| All services total | 284 (100) |
We subsequently classified these services into 5 mutually exclusive groups that could be utilized for analysis (see Table 1 for descriptive and bivariate statistics on this variable). According to our classification schema, 17% of youth received both intensive (partial hospitalization [PH], intensive outpatient [IOP], and or residential treatment) plus nonintensive mental health services; 10.8% received only intensive mental health services; 36.6% received nonintensive outpatient mental health services without receiving intensive mental health services. These three groups may have also received additional support services, such as religious support or school counseling. Almost 8% were involved in other support services only, which encompassed different types of services and service involvement that are generally not considered to be specialty mental health services and may vary in intensity. Twenty-eight percent of youth received no post-discharge care.
Rate and Timing of Rehospitalization
Of the 186 youth, 80 (43.0%) experienced rehospitalizations over the 2½ year period. Fifty-nine youth experienced a readmission during the first year post-discharge; 15 youth were readmitted in the second year following their first psychiatric hospitalization, and 6 experienced a rehospitalization during the third year. These youth experienced from one to six rehospitalizations during this time period with half of them (n = 40) experiencing one readmission.
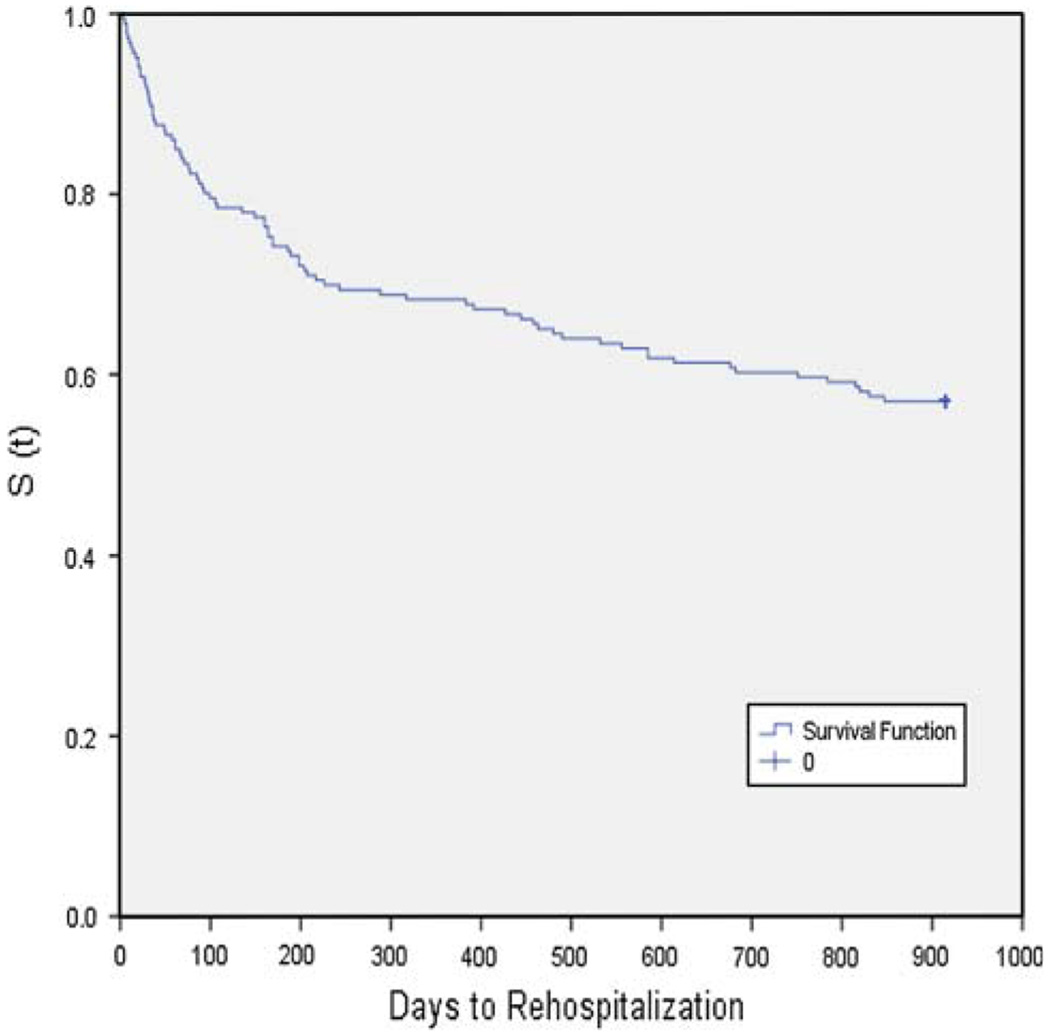
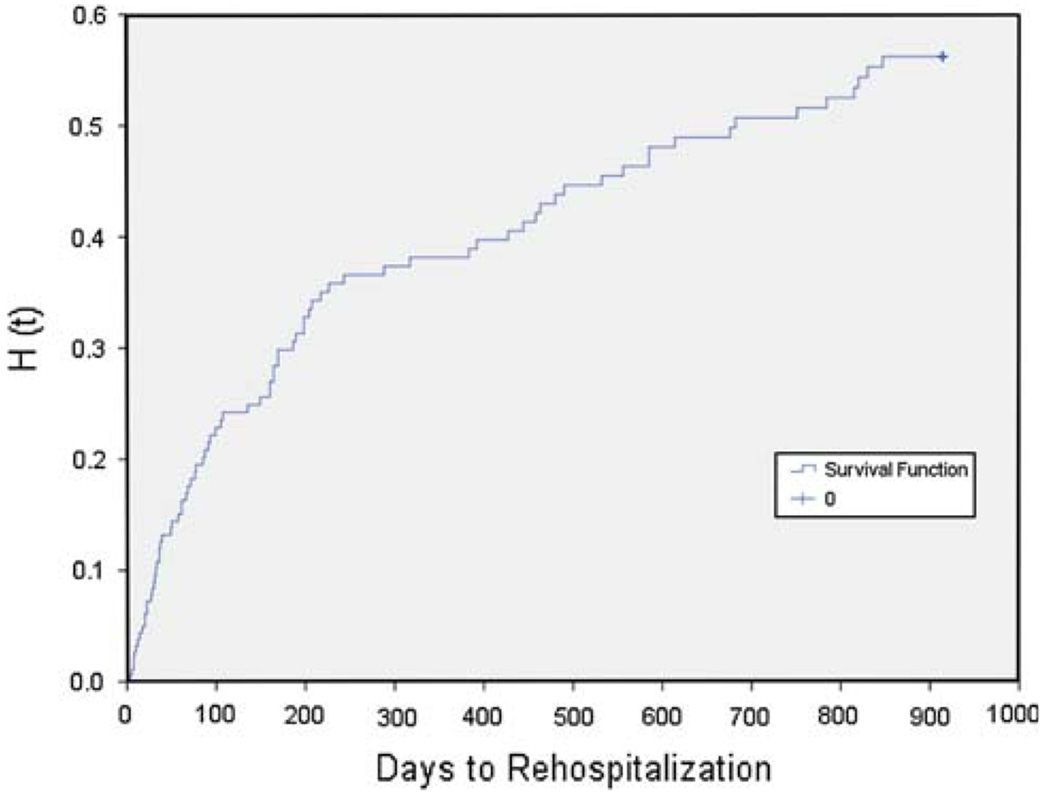
Figures 1 and 2 present the sample’s survival function and cumulative hazard rate, respectively, of experiencing a rehospitalization following a first psychiatric inpatient episode. The survival probability for each individual is the probability of not having experienced a readmission by a specified time (Allison 1984; Singer and Willett 2003). The probability decreases most rapidly during the first 30 days post-discharge, with a rate of survival of 91%. In other words, the risk of readmission during this period was 9%. It was altogether 15% after 60 days, 19% after 90 days and 32% after 1 year. The risk of readmission by the end of the 2½ year (or 914-day) study period was 43%. The cumulative hazard function “assesses, at each point in time, the total amount of accumulated risk that individual i has faced from the beginning of time until the present” (Singer and Willett 2003, p. 488). The cumulative hazard function can be estimated using the negative log survivor function method, which is based on Kaplan–Meier survivor function estimates. The diminishing slope to the curve in Fig. 2 indicates that the risk of a readmission grows at a slower rate over time. The risk or hazard is greatest during the first 30 days following a discharge. The hazard curve diminishes in steepness after 30 days, and again after about 100 days. One year post-discharge it flattens significantly.
Fig. 1.
Survival function of days to rehospitalization (n = 186)
Fig. 2.
Cumulative hazard function of days to rehospitalization (n = 186)
Bivariate and Multivariate Analyses
Results of bivariate analyses using chi-square and t-tests indicated that youth who were rehospitalized tended to be younger by over 1 year (P < .01), had a slightly higher risk factor score (P < .05), and experienced longer stays during their first hospitalization (P < .01). Receipt of post-discharge services also significantly distinguished the two groups of youth (P < .001). A higher percentage of children did not experience a rehospitalization if they had received either intensive plus nonintensive services (68.8 vs. 31.2%), nonintensive mental health services (71.0 vs. 29.0%) or other support services (69.2 vs. 30.8%). However, a higher percentage of children who had gone through the partial hospitalization or intensive outpatient program only were rehospitalized (65.0 vs. 35.0%); similarly, children with no support services were more likely to be rehospitalized (63.5 vs. 36.5%).
Cox regression results are presented for the final model after all variable blocks had been entered (Table 3). None of the sociodemographic characteristics significantly increased the hazard of rehospitalization. However, with each additional psychosocial risk factor, the risk of rehospitalization increased by 36%. Of the clinical/treatment variables only the length of the first hospitalization predicted the risk of rehospitalization at a statistically significant rate. With each additional day hospitalized during the first psychiatric inpatient episode, the risk of rehospitalization increased by 17%. Finally, receipt of post-discharge services significantly reduced the risk of rehospitalization in this sample. More specifically, receipt of other supportive services reduced risk by 76% compared to not receiving any post-discharge services; receipt of nonintensive mental health services reduced risk by 75%; intensive mental health services reduced risk by 17% while receiving both intensive and nonintensive mental health services reduced risk by 76%. The log-likelihood chi-squares at the bottom of the table indicate differences in models with and without the covariates. The final model was statistically significant at P < .0001.
Table 3.
Final cox regression model of the hazard of rehospitalization with all covariates entered (n = 185)
| Hazard ratio (95% CI) | P | |
|---|---|---|
| Entered in Block 1—sociodemographics | ||
| Gender (female = 0) | 0.92 (0.56, 1.51) | .742 |
| Race (white = 0) | 1.05 (0.62, 1.80) | .846 |
| Age at 1st Admission | 0.96 (0.88, 1.06) | .440 |
| Living situation at time of 1st hospitalization (with both bio/adoptive = 0) | ||
| Foster family/group home | 1.25 (0.50, 3.13) | .637 |
| Extended family | 1.32 (0.70, 2.47) | .395 |
| One bio/adoptive parent | 0.91 (0.50, 1.67) | .769 |
| Entered in Block 2—risk factors | ||
| Risk factors | 1.36 (1.08, 1.72) | .010 |
| Entered in Block 3—clinical/treatment variables | ||
| Discharge Axis I diagnosis (mixed mood/conduct = 0) | .344 | |
| Mood disorder only | 1.17 (0.62, 2.20) | |
| Conduct/impulse disorder only | 0.65 (0.30, 1.43) | |
| Discharge GAF score | 1.00 (0.98, 1.03) | .666 |
| Days hospitalized (1st hospitalization) | 1.17 (1.07, 1.27) | .000 |
| Current alcohol/drug use (yes = 0) | .115 | |
| No | 1.87 (1.01, 3.45) | |
| Unknown | 2.35 (0.63, 8.79) | |
| Family involvement 1st hospitalization (yes = 0) | .058 | |
| No | 0.59 (0.35, 1.00) | |
| Unknown | 0.30 (0.07, 1.33) | |
| Entered in Block 4—post-discharge services | ||
| Post-discharge services (no = 0) | .000 | |
| Other (supportive) services | 0.24 (0.08, 0.76) | |
| Outpatient nonintensive MH only | 0.25 (0.14, 0.46) | |
| Intensive MH services only | 0.83 (0.41, 1.70) | |
| Both intensive and nonintensive MH | 0.24 (0.11, 0.52) |
| −2 Log likelihood | χ2 | df | Overall P | Change from previous block P | |
|---|---|---|---|---|---|
| Without covariates | 794.90 | ||||
| Block1 | 785.19 | 10.99 | 6 | .089 | .137 |
| Block2 | 782.19 | 13.79 | 7 | .055 | .084 |
| Block3 | 766.44 | 27.36 | 15 | .026 | .046 |
| Block4 | 736.56 | 57.47 | 19 | .000 | .000 |
Note: One case was lost due to a diagnosis that could not be categorized
Discussion
This study examined the risk of rehospitalization of children and adolescents within 30 months of their first psychiatric hospitalization. It further collected post-discharge data until a youth’s rehospitalization or until the end of the 30-month follow-up period to determine whether post-discharge services, in particular the facility’s partial hospitalization and intensive mental health programs, are associated with lowering risk of rehospitalization.
Summary and Interpretation of Findings
The Rate and Timing of Rehospitalization
Of the children and youth in this sample admitted to inpatient care, 43% experienced rehospitalizations over the 30-month follow-up period. The rate of rehospitalization in this study falls within the range of rates reported by prior studies (Arnold et al. 2003; Blader 2004; Fontanella 2008; Fontanella et al. 2006). In this study, close to three-quarters of the rehospitalizations were experienced during the first year. The risk of rehospitalization was highest during the first 30 days following a first psychiatric hospitalization and remained elevated until about 90 days post-discharge, after which the risk began to decrease notably. Despite the extended follow-up period, this is consistent with findings previously reported by Blader (2004) and Fontanella (2008). It underscores the vulnerability of youth psychiatrically hospitalized during the immediate post-discharge period and supports the need for explicit linkages between inpatient psychiatric care and community-based outpatient services. The finding also calls into question the purpose and effectiveness of psychiatric hospitalizations. In today’s managed care environment, psychiatric hospitalizations imply acute care. This means that patients are generally not psychiatrically hospitalized unless they are considered to be a threat to self or others (Sharfstein 2009). Treatment tends to focus on stabilization, and use of psychotropic medication plays a central role in achieving stabilization (Sharfstein 2009). Rehospitalizations indicate that a youth continues to be in crisis.
Inpatient psychiatric treatment also involves psychosocial interventions and therapies. Child and adolescent patients tend to participate in different group treatments throughout the day and are otherwise engaged in structured activities (Garrick and Ewashen 2001). At the index facility, patients participated in groups, such as anger management, feelings groups, stress management and multifamily groups. Yet much about inpatient psychiatric treatment, including the treatment planning and implementation process, remains a black box. During the past decade, knowledge about diagnostic-specific treatments of childhood and adolescent disorders has increased tremendously, and there are a number of evidence-based treatment models that are now available for most major disorders of childhood and adolescence (Burns et al. 1999; Silverman and Hinshaw 2008). However, the efficacy of these interventions in acute and time-limited settings remains unknown. In fact, none of the studies cited as part of recent in-depth reviews of evidence-based psychosocial treatments for children and adolescents in all major diagnostic categories contained studies that were conducted in acute inpatient psychiatric settings (Silverman and Hinshaw 2008). Interventions, such as Multisystemic Therapy (Henggeler et al. 1998) and Multidimensional Treatment Foster Care (Chamberlain 2002), which have a considerable evidence base for effectiveness, have been developed and tested specifically to serve as viable community-based alternatives to the restrictive intervention of inpatient psychiatric hospitalization. However, as long as such interventions are not widely available and as long as children and teens are treated in inpatient psychiatric facilities, there will be need to develop an evidence base for treatment models in acute and very time-limited settings as those settings are expected to continue being part of the continuum of services for youth. Progress in this area will in part depend on the development of valid assessment and outcome measures for such settings (Harnett et al. 2005).
Post-Discharge Services and Rehospitalization
The elevated risk of rehospitalization during the immediate post-discharge period also underscores the need as well as the potential for effective post-discharge services. Our study found that children and adolescents received a range of different post-discharge services, encompassing both intensive mental health services, traditional outpatient therapy as well as other support services, such as informal counseling, religious support or school-based services. A number of youth also had involvement with child-serving systems, such as the juvenile justice system and child welfare system. Within our classification schema, all types of post-discharge services reduced the risk of rehospitalization, however, to varying degrees. The risk of rehospitalization was lowered 75–76% for youth who received a combination of intensive and nonintensive mental health services, those receiving only nonintensive outpatient mental health services, and those receiving other support services. Youth who only received intensive outpatient mental health services, i.e. partial hospitalization or intensive outpatient treatment, experienced less of a reduction in risk. The lack of effect of intensive mental health services alone on rehospitalization is puzzling at first sight. When investigating this issue further, we found that a number of youth who participated in these programs were hospitalized again shortly afterwards.3 It is likely that the increased monitoring available when intensive services are provided would facilitate identification of youths who were discharged prematurely or were unable to maintain symptom stability. While rehospitalization may be seen as an adverse outcome, identifying patients who continue to be a risk to themselves or others and rehospitalizing them might in fact be an appropriate intervention. Our finding suggests that future studies should examine outcomes beyond rehospitalization, such as suicidality, symptom stability and functional impairment.
With regard to the lack of variability in the effect of the three different types of post-discharge services on read-mission risk, there is no definitive explanation. Why, for instance, would other support services that are generally not considered to offer specialty mental health services be similarly effective in reducing rehospitalization risk as a combination of intensive and nonintensive mental health services? A possible explanation may be that the dosage of services is ultimately more important than the type of service provided. While we collected detailed mental health services data, it is difficult to derive an accurate dosage estimation in our study. The CASA is considered to be most reliable when collecting data on the most restrictive mental health services and for shorter time periods (Ascher et al. 1996); therefore, a categorical operationalization of mental health service use seemed justified for our study. Studies need to begin tackling the question of what type of aftercare services are effective for what type of youth and at which dosage. Part of the problem is that so little is known about the appropriateness, adequacy and effectiveness of aftercare services (Burns et al. 1999; Fontanella et al. 2008). A recent study (Fontanella et al. 2008) pointed out that “there are virtually no assessment tools, guidelines, or level of care criteria to assist [professionals] in making appropriate decisions about aftercare placements” (p. 759). Rigorous evaluative studies using mixed methods are needed to answer questions about both the content and quality of aftercare services.
A final explanation for our post-discharge findings lies in selection bias about who uses or does not use post-discharge services. In other studies, many factors other than clinical considerations have been found to influence service use, such as resource and service availability (Hendryx et al. 1995; Pottick et al. 1999), administrative considerations (James 2004), and organizational level variables (Hurlburt et al. 2004; Warner et al. 2005). Differences on unknown observable and unobservable factors would influence findings and would pose a considerable barrier to producing unbiased estimates of the effects of post-discharge services on outcomes relevant to psychiatric care. Guided by theory, future studies should begin addressing the issue of selection bias.
Rehospitalization and Other Covariates
Besides post-discharge services, psychosocial risk factors and length of stay during the first hospitalization increased the risk of rehospitalization in our study. Expectedly, youth presenting with a higher risk factor score had an elevated rehospitalization risk, mirroring Fontanella’s (2008) recent finding. With regard to length of stay during first hospitalization, findings from prior studies have been mixed. Some have found shorter lengths of stays to be associated with an increased risk for readmissions (Case et al. 2007; Wickizer et al. 1999) whereas others have not (Fontanella 2008). It has been proposed that longer stays might in fact be a proxy for illness severity; however, follow-up analyses (not shown here) did not reveal a significant correlation between discharge diagnosis or functional impairment and length of hospitalization. Other possible explanations include discharge difficulties or the initial timing of the admission. Follow-up discussions with hospital staff suggested that children and youth admitted over the weekend might not be receiving the same type of treatment as a patient who is admitted during the work week where staffing capacity and consequently, treatment intensity might be greater. Clinical diagnosis and functional impairment as reflected in the GAF score were not significant predictors of rehospitalization, contrary to some previous studies (e.g., Arnold et al. 2003; Blader 2004; Fontanella 2008). We found diagnostic data difficult to use. Many children were given multiple diagnoses at admission, and we had been advised by hospital personnel to use discharge diagnoses. However, given the many initial diagnoses, the obscurity of the rule out process, and the few days most youth spent in inpatient psychiatric care, the validity of the diagnoses remains unclear.
As is true for all other current regionally-based studies in this area, this study was not able to disentangle the inconsistent web of predictive factors of rehospitalization that have been identified in the literature so far. National studies using probability sampling procedures will be needed to accomplish this task.
Limitations
The following study limitations should be considered when interpreting results. The final sample was small in comparison to the initial sampling frame. There are two explanations for the final sample size. First, the length of the post-discharge follow up period was 30 months with varying intervals between first psychiatric hospitalization and data collection. This made it difficult to establish contact with elements in the sampling frame and underscores the difficulties of collecting post-discharge data. Given repeated findings at this point that the greatest risk of rehospitalization is during the first few weeks following an episode in psychiatric care, future studies could from now on focus on the immediate post-discharge period, thus increasing the likelihood of participant retention. Regardless of our difficulties, however, we were encouraged by the relatively high response rate of participants who were willing to be interviewed once contact had been established.
We cannot ascertain definitively how representative our final sample is of the general child and adolescent patient population in this facility. Our limited sensitivity analysis of missing data provided some indication that there were few differences. Missing cases were older on average, and this would in part explain difficulties in consenting this group since they would have been more likely to be adults and living away from their caregivers. Like other prior studies we had to exclude youth who were in foster care at the time of the study given difficulties in finding someone who would be a reliable informant of post-discharge services. This exclusion along with a lower percentage of Medicaid patients compared to what was reported to us by hospital personnel, suggests that we might have captured respondents who were perhaps less disadvantaged. Collection of follow-up data for shorter time periods, as recommended earlier, will facilitate inclusion of more vulnerable groups who might be more transient and less accessible over time. However, it deserves mentioning that the study did include a number of youths who were in foster or group care at the time of their first psychiatric hospitalization. A youth’s living situation at the time of the first hospitalization was not a predictor of rehospitalization.
Measurement error related to medical record data is another limitation of this study. Case file data were not recorded using standardized instruments. There is great need to develop and implement a range of assessment and outcome measures that are relevant to acute inpatient psychiatric care. While there are a few available measures (e.g., Cornsweet-Barber et al. 2002; Lyons et al. 2006), these may not fit the needs of a particular setting, and adaptations may be required to facilitate successful implementation.
We relied on interview data to collect data on post-discharge services. While the CASA is a relatively reliable and valid measure, its psychometric properties are weaker for less restrictive services and for longer study periods (Ascher et al. 1996). The variability in intervals between first psychiatric hospitalization and data collection may have further confounded recall of types and dates of services. However, interview data has the advantage that respondents may recall services that might not be captured in administrative data (Garland et al. 1996). Finally, the validity of our schema to classify post-discharge services has not been established, and there might be other ways to conceptualize different types of post-discharge services.
Conclusion
Beyond the specific findings of this study, we want to emphasize the great need for renewed interest in the study of inpatient psychiatric care. The sheer size of the sampling frame at one facility connotes that inpatient psychiatric treatment continues to be used frequently despite advances in the development of community-based evidence-supported treatments. Rigorous studies, using both qualitative and quantitative methods, are needed to advance knowledge in this area.
Acknowledgments
This study was supported by The Silberman Faculty Grant Program (PI: S. James) and in part by NIMH Grant K01 MH077732-01A1 I (PI: S. James). Preliminary findings of this study were presented at the 13th Annual Conference of the Society for Social Work and Research, New Orleans, LA, January 16, 2009 under the title “Predicting and preventing the risk of psychiatric rehospitalization among children and adolescents.”
Footnotes
Clinical personnel indicated that the discharge diagnosis is more reliable than the admission diagnosis, which is generally considered an initial ‘working’ diagnosis.
It should be noted that we did not include medication usage as a covariate in this analysis as all patients were discharged with medications, most with multiple medications, and many had been on medication prior to their first hospitalization. We also did not include insurance type as 90% of respondents in this sample had private insurance.
These youths did not differ from other youths receiving different combinations of post-discharge services in terms of their clinical severity.
References
- Allison PD. Event history analysis. Bevely Hills, CA: Sage Publications; 1984. [Google Scholar]
- Arnold EM, Goldston DB, Ruggiero A, Reboussin BA, Daniel SS, Hickman EA. Rates and predictors or rehospitalization among formerly hospitalized adolescents. Psychiatric Services. 2003;54(7):994–998. doi: 10.1176/appi.ps.54.7.994. [DOI] [PubMed] [Google Scholar]
- Ascher BH, Farmer EMZ, Burns BJ, Angold A. The Child and Adolescent Services Assessment (CASA): Description and psychometrics. Journal of Emotional and Behavioral Disorders. 1996;4:12–20. [Google Scholar]
- Blader JC. Symptom, family, and service predictors of children’s psychiatric rehospitalization within one year of discharge. Journal of the American Academy of Child & Adolescent Psychiatry. 2004;43(4):440–451. doi: 10.1097/00004583-200404000-00010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blader JC. Pharmacotherapy and postdischarge outcomes of child patients admitted for aggressive behavior. Journal of Clinical Psychopharmacology. 2006;26(4):419–425. doi: 10.1097/01.jcp.0000227356.31203.8a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blader J. Longitudinal assessment of parental satisfaction with children’s psychiatric hospitalization. Administration & Policy in Mental Health & Mental Health Services Research. 2007;34(2):108–115. doi: 10.1007/s10488-006-0085-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bobier C, Warwick M. Factors associated with readmission to adolescent psychiatric care. Australian and New Zealand Journal of Psychiatry. 2005;39(7):600–606. doi: 10.1080/j.1440-1614.2005.01632.x. [DOI] [PubMed] [Google Scholar]
- Brinkmeyer M, Eyberg S, Nguyen M, Adams R. Family engagement, consumer satisfaction and treatment outcome in the new era of child and adolescent in-patient psychiatric care. Clinical Child Psychology & Psychiatry. 2004;9(4):553–566. [Google Scholar]
- Burns BJ, Hoagwood K, editors. Community treatment for youth: Evidence-based interventions for severe emotional and behavioral disorders. New York: Oxford University Press; 2002. [Google Scholar]
- Burns BJ, Hoagwood K, Mrazek PJ. Effective treatment for mental disorders in children and adolescents. Clinical Child and Family Psychology Review. 1999;2(4):199–254. doi: 10.1023/a:1021826216025. [DOI] [PubMed] [Google Scholar]
- Case BG, Olfson M, Marcus SC, Siegel C. Trends in the inpatient mental health treatment of children and adolescents in US community hospitals between 1990 and 2000. Archives of General Psychiatry. 2007;64:89–96. doi: 10.1001/archpsyc.64.1.89. [DOI] [PubMed] [Google Scholar]
- Causey DL, McKay M, Rosenthal C, Darnell C. Assessment of hospital-related stress in children and adolescents admitted to a psychiatric inpatient unit. Journal of Child & Adolescent Psychiatric Nursing. 1998;11(4):135–145. doi: 10.1111/j.1744-6171.1998.tb00029.x. [DOI] [PubMed] [Google Scholar]
- Chamberlain P. Treatment foster care. In: Burns BJ, Hoagwood K, editors. Community treatment for youth: Evidence-based interventions for severe emotional and behavioral disorders. New York: Oxford University Press; 2002. pp. 117–138. [Google Scholar]
- Chung W, Edgar-Smith S, Palmer R, Bartholomew E, Delambo D. Psychiatric rehospitalization of children and adolescents: Implications for social work intervention. Child and Adolescent Social Work Journal. 2008;25(6):483–496. [Google Scholar]
- Cornsweet-Barber CD, Neese T, Coyne L, Fultz J, Fonagy P. The target symptom rating: A brief clinical measure of acute psychiatric symptoms in children and adolescents. Journal of Clinical Child Psychology. 2002;31(2):181–192. doi: 10.1207/S15374424JCCP3102_04. [DOI] [PubMed] [Google Scholar]
- Daniel SS, Goldston DB, Harris AE, Kelley AE, Palmes GK. Review of literature on aftercare services among children and adolescents. Psychiatric Services. 2004;55(8):901–912. doi: 10.1176/appi.ps.55.8.901. [DOI] [PubMed] [Google Scholar]
- Dickey B, Normand SL, Norton EC, Rupp A, Azeni H. Managed care and children’s behavioral health services in Massachusetts. Psychiatric Services. 2001;52(2):183–188. doi: 10.1176/appi.ps.52.2.183. [DOI] [PubMed] [Google Scholar]
- Fontanella C. The influence of clinical, treatment, and healthcare system characteristics on psychiatric readmission of adolescents. American Journal of Orthopsychiatry. 2008;78(2):187–198. doi: 10.1037/a0012557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fontanella C, Early T, Phillips G. Need or availability? Modeling aftercare decisions for psychiatrically hospitalized adolescents. Children & Youth Services Review. 2008;30(7):758–773. [Google Scholar]
- Fontanella C, Zuravin S, Burry C. The effect of a medicaid managed care program on patterns of psychiatric readmission among adolescents: Evidence from Maryland. Journal of Behavioral Health Services & Research. 2006;33(1):39–52. doi: 10.1007/s11414-005-9004-0. [DOI] [PubMed] [Google Scholar]
- Foster EM. Do aftercare services reduce inpatient psychiatric readmissions? Health Services Research. 1999;34:715–736. [PMC free article] [PubMed] [Google Scholar]
- Garland AF, Landsverk J, Hough RL, Ellis-MacLeod E. Type of maltreatment as a predictor of mental health service use for children in foster care. Child Abuse and Neglect. 1996;20(8):675–688. doi: 10.1016/0145-2134(96)00056-7. [DOI] [PubMed] [Google Scholar]
- Garrick D, Ewashen C. An integrated model for adolescent inpatient group therapy. Journal of Psychiatric and Mental Health Nursing. 2001;8:165–171. doi: 10.1046/j.1365-2850.2001.00374.x. [DOI] [PubMed] [Google Scholar]
- Harnett PH, Loxton NJ, Sadler T, Hides L, Baldwin A. The Health of the Nation Outcome Scales for children and adolescents in an adolescent in-patient sample. Australian and New Zealand Journal of Psychiatry. 2005;39:129–135. doi: 10.1080/j.1440-1614.2005.01533.x. [DOI] [PubMed] [Google Scholar]
- Heggestad T. Operating conditions of psychiatric hospitals and early admission: Effects of high patient turnover. Acta Psychiatrica Scandinavica. 2001;103:196–202. doi: 10.1034/j.1600-0447.2001.00166.x. [DOI] [PubMed] [Google Scholar]
- Hendryx MS, Urdaneta ME, Borders T. The relationship between supply and hospitalization rates for mental illness and substance use disorders. Journal of Health Administration. 1995;2(2):167–176. doi: 10.1007/BF02518756. [DOI] [PubMed] [Google Scholar]
- Henggeler SW, Schoenwald SK, Borduin CM, Rowland MD, Cunningham PB. Multisystemic treatment of antisocial behavior in children and adolescents. New York: Guilford; 1998. [Google Scholar]
- Hurlburt MS, Leslie LK, Landsverk J. Contextual predictors of mental health service use among children open to child welfare. Archives of General Psychiatry. 2004;61(12):1217–1224. doi: 10.1001/archpsyc.61.12.1217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- James S. Why do foster care placements disrupt? An investigation of reasons for placement change in foster care. Social Service Review. 2004;78:601–627. [Google Scholar]
- Lakin B, Brambila A, Sigda K. Parental involvement as a factor in the readmission to a residential treatment center. Residential Treatment for Children & Youth. 2004;22(2):37–52. [Google Scholar]
- Lien L. Are readmission rates influenced by how psychiatric services are organized? Nordic Journal of Psychiatry. 2002;56:23–28. doi: 10.1080/08039480252803873. [DOI] [PubMed] [Google Scholar]
- Lyons JS, McCulloch J, Romansky J. Monitoring and managing outcomes in residential treatment: Practice-based evidence in search of evidence-based practice. Journal of the American Academy of Child & Adolescent Psychiatry. 2006;45(2):247–251. doi: 10.1097/01.chi.0000190468.78200.4e. [DOI] [PubMed] [Google Scholar]
- Nierman P, Lyons JS. State mental health policy: Shifting resources to the community: Closing the Illinois State Psychiatric Hospital for Adolescents in Chicago. Psychiatric Services. 2001;52:1157–1159. doi: 10.1176/appi.ps.52.9.1157. [DOI] [PubMed] [Google Scholar]
- Owens PL, Thompson J, Elixhauser A, Ryan K. Care of children and adolescents in U.S. hospitals. Rockville MD: Agency for Healthcare; 2003. Research and Quality, HCUP Fact Book No. 4. [Google Scholar]
- Parham C, Reid S, Hamer R. A long-range follow-up study of former inpatients at a children’s psychiatric hospital. Child Psychiatry and Human Development. 1987;17:199–209. doi: 10.1007/BF00706230. [DOI] [PubMed] [Google Scholar]
- Pavkov TW, Goerge RM, Lee BJ. State hospital reentry among youth with serious emotional disturbance: A longitudinal analysis. Journal of Child and Family Studies. 1997;6(3):373–383. [Google Scholar]
- Pfeffer CR, Peskin JR, Siefker CA. Suicidal children grown up-psychiatric-treatment during follow-up period. Journal of the American Academy of Child and Adolescent Psychiatry. 1992;31(4):679–685. doi: 10.1097/00004583-199207000-00015. [DOI] [PubMed] [Google Scholar]
- Pottick K, Hansell S, Gaboda D, Gutterman E. Child and adolescent outcomes of inpatient psychiatric services: A research agenda. Children and Youth Services Review. 1993;15(5):371–384. [Google Scholar]
- Pottick KJ, Hansell S, Miller JE, Davis DM. Youths living away from families in the U.S. Mental health system: Opportunities for targeted intervention. The Journal of Behavioral Health Services & Research. 1999;32(3):264–281. doi: 10.1007/BF02291827. [DOI] [PubMed] [Google Scholar]
- Romansky JB, Lyons JS, Lehner RK, West CM. Factors related to psychiatric hospital readmission among children and adolescents in state custody. Psychiatric Services. 2003;54:356–362. doi: 10.1176/appi.ps.54.3.356. [DOI] [PubMed] [Google Scholar]
- Saunders RC, Heflinger CA. Access to and patterns of use of behavioral health services among children and adolescents in TennCare. Psychiatric Services. 2003;54(10):1364–1371. doi: 10.1176/appi.ps.54.10.1364. [DOI] [PubMed] [Google Scholar]
- Segal HG, King CA, Naylor MW. Psychosocial functioning of severely disturbed adolescents after short-term hospitalization. Psychiatric Services. 1995;46(3):287–289. doi: 10.1176/ps.46.3.287. [DOI] [PubMed] [Google Scholar]
- Sharfstein SS. Goals of inpatient treatment for psychiatric disorders. Annual Review of Medicine. 2009;60:393–403. doi: 10.1146/annurev.med.60.042607.080257. [DOI] [PubMed] [Google Scholar]
- Silverman WK, Hinshaw SP. The second Special Issue on evidence-based psycho-social treatments for children and adolescents: A 10-year update. Journal of Clinical Child & Adolescent Psychology. 2008;37(1):1–7. [Google Scholar]
- Singer JD, Willett JB. Applied longitudinal data analysis: Modeling change and event occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Solomon P, Evans D, Delaney MA. Community service utilization by youths hospitalized in a state psychiatric facility. Community Mental Health Journal. 1993;29:333–346. doi: 10.1007/BF00761031. [DOI] [PubMed] [Google Scholar]
- Stroul B, Friedman R. A system of care for children and youth with severe emotional disturbances. Washington, DC: Georgetown University Child Development Center, National Technical Assistance Center for Children’s Mental Health; 1986. [Google Scholar]
- U.S. Department of Health and Human Services. Health information privacy. 1996 Retrieved 09/11/09 from http://www.hhs.gov/ocr/privacy/
- Warner LA, Pottick KJ, Bilder SM. Clinical and organizational correlates of medication for youths in U.S. Mental Health Services. Social Service Review. 2005;79(3):454–481. [Google Scholar]
- Wickizer TM, Lessler D, Wickizer JB. Effects of health care cost-containment programs on patterns of care and readmissions among children and adolescents. American Journal of Public Health. 1999;89(9):1353–1358. doi: 10.2105/ajph.89.9.1353. [DOI] [PMC free article] [PubMed] [Google Scholar]