Summary
Positive and negative costimulation by members of the CD28 family is critical for the development of productive immune responses against foreign pathogens and their proper termination to prevent inflammation-induced tissue damage. In addition, costimulatory signals are critical for the establishment and maintenance of peripheral tolerance. This paradigm has been established in many animal models and has led to the development of immunotherapies targeting costimulation pathways for the treatment of cancer, autoimmune disease, and allograft rejection. During the last decade, the complexity of the biology of costimulatory pathways has greatly increased due to the realization that costimulation does not affect only effector T cells but also influences regulatory T cells and antigen-presenting cells. Thus, costimulation controls T-cell tolerance through both intrinsic and extrinsic pathways. In this review, we discuss the influence of costimulation on intrinsic and extrinsic pathways of peripheral tolerance, with emphasis on members of the CD28 family, CD28, cytotoxic T-lymphocyte antigen-4 (CTLA-4), and programmed death-1 (PD-1), as well as the downstream cytokine interleukin-1 (IL-2).
Keywords: costimulation, tolerance, CD28, CTLA-4, PD-1, Tregs
Introduction
Understanding the mechanisms underlying immunological tolerance is a formidable challenge that could have far reaching implications for therapeutic strategies in autoimmune diseases and transplantation. The notion of costimulatory signals first introduced by Lafferty and colleagues (reviewed in 1) marked a milestone in the tolerance field that was followed by the important discovery of CD28 and its crucial role in T-cell activation. CD28 represented the quintessential costimulatory molecule not only in that CD28 ligation allows T-cell receptor (TCR)-mediated signals to result in productive T-cell activation but also in the functional unresponsiveness ensuing TCR engagement in the absence of CD28 costimulation (2, 3). This finding generated enormous interest and CD28 blockade was initially perceived as a silver bullet to achieve tolerance with widespread clinical applications. While targeting the CD28 pathway is still the subject of intense investigation and the therapeutic potential of CD28 blockade is currently evaluated in clinical trials (4, 5), the field of costimulation and tolerance has greatly evolved since CD28 was first described, with heightened complexity on both sides of the equation. Indeed, on the one hand, it is now apparent that while representing a central component of the T-cell activation molecular machinery, CD28 is only one of many members of the costimulatory molecule family, which relative importance varies depending on the cell subset, activation status, anatomical location and stage of the immune response (6, 7). Furthermore, an inherent intricacy of the costimulatory molecule family is that it contains both activating (such as CD28) and inhibitory [such as cytotoxic T-lymphocyte antigen-4 (TLA-4) and programmed death-1 (PD-1)] molecules that can have antagonistic influences on immune responses (3, 8). On the other hand, the range of molecular pathways and cell subsets involved in establishing or maintaining tolerance has considerably widened since CD28 was discovered, in particular with the avalanche of evidence showing that regulatory T cells (Tregs) are critical for peripheral tolerance (9, 10). Importantly, costimulatory signals affect Treg development, homeostasis, and suppressive function independently of their effect on effector T cells (11). Thus, costimulation now appears to control tolerance at multiple levels through signals mediated by positive and negative costimulatory molecules that affect effector T cells by both cell-intrinsic and -extrinsic mechanisms. In this review, we summarize studies from our laboratory and others that have defined the role of members of the CD28 family of costimulatory molecules, CD28, CTLA-4, and PD-1, and the cytokine interleukin-2 (IL-2) in effector T-cell-intrinsic and -extrinsic pathways of T-cell tolerance. Moreover, the appreciation that a given costimulation pathway can have distinct effects on different cell subsets, with outcomes that can be synergistic or opposite, has complicated the task of predicting the effect of a given pathway in a disease setting. We review the current state and challenges of targeting these pathways for therapeutic purposes.
Mechanisms of tolerance
The immune system has evolved to include several complementary mechanisms designed to preserve self-tolerance while allowing robust responses against pathogens. In the thymus, central tolerance processes ensure that the majority of potentially autoreactive lymphocytes are deleted during negative selection. This is achieved in large part through interactions of developing thymocytes with medullary thymic epithelial cells (mTECs) expressing the autoimmune regulator (AIRE) that drives the ectopic expression of peripheral tissue-specific antigens (TSA) in the thymus (12). The importance of AIRE in immune tolerance is notably illustrated by the development of multi-organ autoimmunity in patients and mice defective or deficient in AIRE (13, 14). Of note, although this is still a controversial issue, recent reports have suggested that AIRE function may not be limited to thymic development but may also participate in peripheral tolerance by inducing TSA expression in secondary lymphoid organs that ultimately results in deletion of autoreactive T cells in the periphery (12, 15). Indeed, despite negative selection, a significant number of potentially autoreactive T-cell clones emerge from the thymus and are usually controlled by both intrinsic and extrinsic peripheral mechanisms of tolerance. Intrinsic mechanisms of tolerance encompass processes that directly affect self-antigen specific T cells to result in unresponsiveness and include immunological ignorance, anergy, and peripheral deletion (reviewed in 16). Autoreactive T cells can ignore tissues expressing their cognate antigens due to their anatomical separation, the naive/immature state of both T cells and APCs as it relates to immunologically privileged sites and the low avidity for self-antigens that allowed these T cells to escape thymic negative selection (17, 18). T-cell anergy is a state of functional inactivation usually resulting from suboptimal stimulation due to reduced TCR signaling and/or defective costimulation. Importantly, Schwartz and colleagues (reviewed in 19) have proposed that T-cell unresponsiveness induced in different experimental conditions could represent distinct functional states and molecular pathways of anergy and thus could have distinct requirements for costimulatory signals or lack thereof for their induction and maintenance. Finally, apoptosis and clonal deletion are crucial to restore T-cell homeostasis after immune responses and prevent autoimmune diseases (20). Apoptotic pathways have been involved in both thymic and peripheral T-cell death and have been shown to prevent autoimmunity through effects on T cells and other cell types including APCs (21, 22). Almost by definition, it has been recognized that costimulation is inherently linked to intrinsic mechanisms of peripheral tolerance, but we now have a better understanding of the influence of distinct costimulatory molecules on these different mechanisms and a recent appreciation that they do not just result in passive unresponsiveness but are active processes depending on specific signaling pathways and active transcription. Tregs represent a subset of CD4+ T cells widely defined by expression of CD25 and the lineage marker forkhead box protein 3 (Foxp3), and they are central to the extrinsic control of T-cell tolerance (reviewed in 23). Similar to conventional T cells, CD4+CD25+Foxp3+ Tregs are generated in the thymus, but they display a repertoire distinct from conventional T cells and are skewed for T-cell receptors (TCRs) of high affinity for self-peptides (24, 25). Furthermore, adaptive Tregs can be generated in the periphery from CD4+CD25−Foxp3− conventional T cells, although the relative contribution of thymic (natural) versus adaptive Tregs in the maintenance of tolerance remains controversial (26). Tregs have been reported to suppress conventional T cells through multiple mode of actions, including the production of immunosuppressive cytokines such as tissue growth factor-β (TGF-β) or IL-10 and direct alterations of effector T cells or APCs (9, 10). Tregs are master regulators of peripheral lymphocytes, as evidenced by the development of widespread autoimmune diseases in Foxp3-deficient IPEX patients and scurfy mice (27, 28). As discussed below, the discovery that costimulatory molecules control Treg homeostasis and function has redefined the field of costimulation and tolerance, providing new insights into the molecular and cellular targets of costimulation and new challenges in predicting the net biological effect of given costimulatory pathways. Finally, accumulating evidence during the last decade has underlined an important role for tolerogenic APCs in the maintenance of peripheral tolerance and prevention of autoimmunity (29). Complex bidirectional interactions between dendritic cells (DCs) and effector or regulatory T cells involve a number of costimulatory molecules that participate in the balance of signals skewing these interactions towards immune responses versus tolerance.
Intrinsic control of tolerance by costimulation
CD28: the quintessential costimulatory molecule
CD28 was the first costimulatory molecule discovered after the concept that productive T-cell activation requires an antigen-specific ‘signal 1’ through the TCR and an accessory ‘signal 2’ through soluble factors or costimulatory molecules was developed in the 1980s (1, 30). While it is now clear that other costimulatory pathways contribute to T-cell activation at different stages of the immune response and in different T-cell subsets (reviewed in 6, 7), the interaction of CD28 with its ligands B7-1 (CD80) and B7-2 (CD86) remains the best characterized pathway and is the object of intense investigation for therapeutic purposes. CD28 signals are critical for T-cell activation, proliferation, and survival upon T-cell interaction with APCs presenting their cognate antigen (2, 3). CD28 colocalizes with the TCR in the central region of the immunological synapse [central supramolecular activation cluster (cSMAC)] (31), where integration of TCR and CD28 signals leads to accumulation of lipid rafts and subsequent enhancement of tyrosine phosphorylation of a number of molecules critical for T-cell activation (32, 33). CD28 can thus lower the threshold necessary for efficient T-cell stimulation (34) but, as discussed below, CD28 does not only amplify phosphorylation of TCR-dependent kinases in TCR-CD28 microclusters (35) but also initiates a distinct signaling and transcriptional program. Additionally, CD28 costimulation is required to increase glucose uptake and glycolysis through both phosphoinositol 3-kinase (PI3K)-Akt-dependent and -independent pathways to meet elevated metabolic demand following T-cell activation (36). The control of T-cell expansion by CD28 is both a direct consequence of entry and progression into the cell cycle through CD28-mediated expression of cyclins, activation of cyclin-dependent kinases (cdk), and downregulation of cdk inhibitor p27kip1, and an indirect outcome of increased production of the T-cell growth factor IL-2, one of the most critical targets downstream of CD28 signaling (30, 37-39). Furthermore, CD28 controls T-cell survival by enhancing expression of the anti-apoptotic factor Bcl-XL (40-43). Interestingly, as will be discussed further below, discrete regions of the CD28 cytoplasmic tail influence distinct molecular pathways that function autonomously upon CD28 signaling and independently of endogenous IL-2. Indeed, regulation of T-cell proliferation and IL-2 production versus upregulation of survival factor Bcl-XL map to separate regions of the CD28 cytoplasmic domain (44, 45). Furthermore, CD28 regulation of cell cycle is independent of endogenous IL-2 in the early stages of cell cycle progression while sustained proliferation is dependent on IL-2 production (38, 39). This is in agreement with reports that CD28 costimulation is required for initiating T-cell responses while other molecular interactions become predominant at later time points (42, 46, 47). While memory T cells are less dependent than naive T cells on CD28 signals, CD28 costimulation can nevertheless affect the optimal development of secondary responses, proliferation of memory CD4+ and CD8+ T cells and clearance of viral infections (48, 49).
The consequence of this array of CD28 functions, as it pertains to T-cell tolerance, is that activation of naive T cells in the absence of costimulation not only precludes the development of an effective T-cell response but also can lead to a state of tolerance achieved by additive mechanisms. Thus, blockade of CD28-B7 interactions promotes transplantation tolerance that initially depends on massive T-cell deletion and can be abrogated when apoptotic pathways are compromised (50-52). Additionally, T-cell activation in the absence of CD28 costimulation can lead to a state of anergy characterized by defective phospholipase C-γ1 (PLCγ-1) activation and intracellular calcium mobilization (53). The anergic state resulting from altered CD28 signaling is also associated with increased levels of the cdk inhibitor p27kip1 and mice deficient in p27kip1 protein or function failed to be tolerized after CD28/CD40L costimulation blockade in vivo (37, 54, 55). These reports suggest that p27kip1 plays a critical role in T-cell tolerance achieved through blockade of the CD28 pathway, at least in part by preventing the downstream phosphorylation of the signal transducer Smad3 (55). Of note, given the important affect of CD28 costimulation on T-cell proliferation (2, 3), CD28 signals thus participate directly and indirectly in tolerance since anergy avoidance in T cells has been shown to depend on cell cycle progression as well as costimulatory signals (56, 57).
In addition to its influence on T-cell deletion and anergy, CD28 qualitatively controls T-cell responses through its effect on T-cell differentiation and cytokine production. Indeed, the overall strength-of-signal plays an important role in the differentiation of naive T cells towards the T-helper 1 (Th1) or Th2 subsets, with strong TCR and CD28 signals favoring Th2 differentiation while engagement of the inhibitory molecule, CTLA-4, has the opposite effect (42, 58-60). Thus, CD28 blockade is highly beneficial in Th2-dependent diseases such as allergic airway inflammation in models of asthma and autoantibody-mediated lupus-like syndrome in NZB/NZW mice (61, 62). Conversely, CD28 costimulation favors Th2 skewing and immunoregulation in chronic inflammatory Th1-mediated autoimmune diseases such as diabetes in the non-obese diabetic (NOD) mouse (63, 64). As discussed further below, this led to the unexpected realization that CD28 signaling could directly participate in the induction of immunoregulation and tolerance, complicating the prospect of blocking this pathway for therapeutic purposes (65). Although more studies are needed to fully answer this question, recent reports suggest that the strength of signal could also influence the differentiation of pro-inflammatory Th17 cells. Indeed, CD28 blockade using CTLA-4-immunoglobulin (Ig) fusion protein was shown to inhibit IL-17 production in vitro and in vivo (66). However, high strength stimulation, in particular CD28 costimulation itself, was also shown to hinder the differentiation of both human and murine cells into the Th17 lineage (67, 68). Thus, while this issue will have to be resolved in vitro and investigated further in animal models, it is possible that the CD28 pathway could influence Th17-mediated autoimmune responses in vivo, raising once more the possibility of unexpected consequences of CD28 blockade on T-cell tolerance versus autoreactivity.
Signaling pathways downstream of CD28
CD28 costimulation regulates a wide range of genetic and biochemical processes required for complete T-cell activation. Following antigen recognition by the TCR, the membrane-proximal signaling mechanism activated by CD28 ligation generates a specific gene expression program, which subsequently mediates the specific cellular outcomes described in the previous section. The initial signal transduction cascades are dependent on specific association of proteins with the different CD28 cytoplasmic motifs (69). The phosphorylation of the proximal motif via Src family kinases allows the binding of PI3K, Grb2 and GADS (70, 71) (Fig. 1). In contrast, Lck or Fyn kinases primarily phosphorylate the distal cytoplasmic motif although Grb2 and Filamin-A are also able to bind this motif (72-74). Finally, a third proline-rich region, particularly close to the proximal motif, is associated with Itk binding (75).
Fig. 1. Biochemical and transcriptional effects of the CD28 signaling pathways.
Summary of biochemical signaling events downstream of the proximal and distal CD28 motifs that can modulate the T-cell transcription pattern after costimulation. Among the different mechanisms, we can distinguish a direct effect on gene expression by regulation of transcription factors or an indirect effect through increases in mRNA stability.
The biochemical cascades associated with the proximal CD28 motif are mainly mediated by PI3K, which has a critical role in T-cell activation by inducing the production of PIP3, the main D3-lipid in the TCR/CD28 synapse (76) (Fig. 1). The resulting recruitment and phosphorylation of protein kinase B (PKB)/Akt led to mammalian target of rapamycin (mTOR) and inhibitor of nuclear factor κB (IκB) activation, simultaneously with the repression of GSK3β and Bad (77, 78). Besides, recent studies showed that PI3K can also enhance TCR-induced signaling by breaking the negative cyclic adenosine monophosphate (cAMP) negative feedback via recruitment of β-arrestin/PDE4 complex to the lipid rafts (79). In addition to PI3K pathways, CD28 signaling events are initiated by binding of the adapter protein Grb2, which has the ability to interact with the proximal and distal CD28 motifs (Fig. 1). Grb2 is able to initiate two signaling pathways through the recruitment of the exchange factor Vav (80). On one hand, the binding of Vav with the SH2 leukocyte protein of 76 kDa (SLP-76)/linker for activated T cells (LAT) complex activates PLCγ1 that increases intracellular Ca2+ and triggers PKCθ function via the Bcl10 (B-cell lymphoma 10)/MALT1 (mucosal associated lymphoid tissue 1)/CARMA-1 [caspase-recruitment domain (CARD) membrane-associated guanylate kinase (MAGUK) protein 1] complex (81, 82). On the other hand, Vav mediates c-Jun N-terminal kinase (JNK) activation by MEKK1 signaling through Rac1/CDC42 phosphorylation (83, 84). Furthermore, the distal motif actively contributes to the immunological synapse rearrangements. CD28 is tethered to the lipid raft by binding to Filamin-A through the distal motif (85). Lck also binds this region, thus participating in CD28-dependent signaling in the SMAC via PKCθ activation (86).
Despite advances in identifying the membrane-proximal signaling events downstream of CD28, how these complex networks of pathways are integrated with the transcriptional pattern and the cellular outcome is not completely understood. Specific mutations in different CD28 tail motifs have been performed in order to clarify the functional role of the implicated signaling pathways (87, 88). Although the distal CD28 motifs proved to have a critical role in T cell activation, little is known about their specific effects in gene expression. Different CD28-dependent pathways can modulate several transcriptional regulatory families involved in T-cell activation (Fig. 1). Moreover, the observed effects can be partially redundant between various signaling cascades (89). The NF-κB transcriptional activity can be trigged by a PI3K-dependent signaling via mTOR and IκB or independently through PKCθ signaling (82, 90, 91). The expression of NFAT-dependent genes can be activated by Akt and PKCθ phosphorylation, which inhibits GSK3β, a kinase that promotes the nuclear export of the transcription factor. NFAT nuclear translocation is also triggered by increases in intracellular Ca2+, a PI3K-independent pathway (92). Other transcription factors involved in CD28 costimulation are the activator protein-1 (AP-1) family, such as c-fos and Jun. JNK activation by Vav modulates the expression of AP-1 target genes (93). In addition, JNK is able to regulate the post-transcriptional mRNA stabilization of several cytokines (94).
In addition to their intrinsic complexity, the signaling cascades that characterize CD28 function are strongly interconnected with the intracellular TCR signaling machinery. As a consequence of this partial redundancy in signaling processes, the primary role of CD28 costimulation in T-cell activation has been controversial. Specifically, it is still unclear whether CD28 can activate distinct signaling pathways independent of TCR-mediated signaling or functions principally by amplifying TCR-triggered pathways. Microarray analysis performed to investigate the effect of costimulation on gene expression level during T-cell activation has not identified a specific CD28-dependent transcriptional pattern (95, 96). These data supported the hypothesis that CD28 costimulation constitutes mostly a ‘quantitative’ signal in T-cell activation required to overcome signaling thresholds that are not attainable by ligation of the TCR alone. The alternative model defines CD28 costimulation as a ‘qualitative’ signal, not only indispensable to achieve a complete T-cell activation but also responsible for a TCR-independent transcription pattern. The activation of T cells using superagonistic anti-CD28 antibodies suggests that CD28 can function in the absence of a TCR-derived signal (97). Although these results are controversial, the existence of both TCR-dependent and -independent pathways is not mutually exclusive, and it is probable that both are operative and functionally relevant.
We have recently begun to reinvestigate this question using global gene expression analyses performed on highly purified human naïve CD4+CD45RA+ T cells. Preliminary results suggest that CD28 signaling affects T-cell activation both quantitatively and qualitatively (Esensten J, Martinez-Llordella M, Bluestone JA, and colleagues, manuscript submitted). The differences between this and previous studies (95, 96) may reflect the use of the naive T cells, which are known to be exquisitely CD28-dependent. Thus, we propose CD28 costimulation supports TCR signaling during the early stages of T-cell activation. However, a qualitative effect provided by the CD28 pathway is also present early after T-cell stimulation and increases throughout the activation process.
CTLA-4: a potent immunoregulatory molecule with a complex biology and function CTLA-4 (CD152) was the first described ‘costimulation’ molecule with inhibitory properties on T cells (reviewed in 2, 3). The immunoregulatory properties of CTLA-4 were dramatically exemplified by the lymphoproliferative disease occurring in CTLA-4 knockout (KO) mice that resulted in the death of all animals by three to four weeks of age (98). Functionally, CTLA-4 was shown to inhibit T-cell proliferation, cell cycle progression, and IL-2 production (99, 100). Additionally, CTLA-4 signals influence CD4+ T-cell differentiation. Indeed, CTLA-4-deficient mice and T cells were shown to be strongly skewed towards a Th2 phenotype, even in the absence of the Th2 lineage transcription factor signal transducer and activator of transcription-6 (Stat-6) (58, 59). CTLA-4 was also recently shown to influence Th17 responses, as blockade of CTLA-4 with anti-CTLA-4 monoclonal antibodies or using CTLA-4Ig and CD28KO T cells resulted in increased Th17 differentiation and IL-17 production in vitro and in vivo (66). These data imply that CTLA-4 signals inhibit Th17 responses and, together with the still controversial role of CD28 in Th17 differentiation, suggest that the Th17 lineage will be influenced by the overall strength of signal of T cell-APC interactions and in particular by the nature and intensity of costimulatory signals. This is reminiscent of the control of Th1/Th2 differentiation, which was shown to depend both on TCR and costimulatory signals as well as the cytokine microenvironment. The CTLA-4 receptor binds the same B7-1 and B7-2 ligands as CD28 on APCs (2, 3). Together with the requirement for CTLA-4 and TCR ligation to occur in cis (e.g. during interactions with the same APC) (101), which resulted in relatively inefficient anti-CTLA-4 agonistic reagents, this property has created serious challenges for the study of CTLA-4 signals in intrinsic T-cell function in vivo. Thus, we developed a single-chain membrane-bound anti-CTLA-4 antibody (scαCTLA-4) that can be expressed directly on antigen-presenting B cells in vivo. We found that expression of the scαCTLA-4 transgene (Tg) on antigen-presenting B cells profoundly inhibited antigen-specific T-cell responses in vitro and in vivo (101-103). Indeed, T-cell proliferation and cytokine production during an allogeneic mixed lymphocyte reaction in vitro as well as T-cell-dependent antibody production and class switching in vivo were greatly diminished when B cells expressed the scαCTLA-4 Tg (102). Alegre and colleagues (104) further showed that expression of an scαCTLA-4 Tg on allogeneic tumor cells prevented their rejection by antigen-specific CD8+ T cells in vivo. In autoimmune diabetes, expression of the scαCTLA-4 transgene in B cells affected the activation and differentiation of autoreactive T cells in the pancreatic lymph nodes and decreased the incidence of diabetes both in NOD mice and in Treg-deficient NOD-B7-1/2KO mice (102). Together, these data point to a critical role of CTLA-4 for controlling T-cell responses to foreign and self-antigens in an intrinsic manner. However, as discussed later, this does not preclude an extrinsic role of CTLA-4, and it is now clear that CTLA-4 controls immune responses at multiple levels and by affecting several cell subsets, perhaps explaining that its absence has such a profound effect on T-cell homeostasis and self-tolerance. Interestingly, the role of CTLA-4 in peripheral tolerance is not uniform in all circumstances and biological contexts. CTLA-4 blockade or genetic deficiency prevents T-cell tolerance induced by high-dose systemic antigen in the absence of adjuvant or by antigen-fixed ECDI-coupled spleen cells (105, 106). In an adoptive transfer model of autoimmune diabetes using islet antigen-specific TCR-Tg T cells and tolerogenic antigen-coupled spleen cells, we found that CTLA-4 was important for the induction of tolerance, but CTLA-4 blockade could not revert the antigen-specific T-cell anergic state (107). These results suggest that CTLA-4 is more critical for the induction phase than the maintenance phase of tolerance to self-antigens. However, the immunological context is key, as T-cell tolerance induced by antigen-coupled spleen cells could be abrogated by CTLA-4 blockade when it was administered together with high-dose antigen in complete Freund's adjuvant (105). The requirement and function of CTLA-4 as it pertains to the immune environment and the quantity and form of the antigenic challenge may relate to the differential role of CTLA-4 in T cells of varying affinities for their cognate antigen. Indeed, Egen and Allison (108) showed that the TCR signal strength correlated with expression levels of CTLA-4 at the immunological synapse. These data led to the hypothesis that by proportionally exerting a stronger inhibition on high-affinity T cells, CTLA-4 allowed lower affinity T cells to participate in the immune response and thus broadened the T-cell repertoire at the population level.
A distinct but related question, which is still controversial, is the antigen specificity of CD4+ T cells that proliferate in an uncontrolled manner in CTLA-4KO mice and cause multi-organ infiltration and inflammation (98). Namely, it is unclear whether lymphoproliferation in these mice stems from a lower threshold of activation due to CTLA-4 deficiency that results in the proliferation of T cells receiving signals from self-MHC molecules, in a manner similar to homeostatic proliferation, or from the selective expansion of T cells specific for tissue-associated self-antigens. TCR repertoire analyses by CDR3 spectratyping, which can identify antigen-specific T-cell expansions at the population levels, yielded conflicting results, with one study identifying restricted profiles suggestive of antigen-driven responses and another report finding Gaussian spectratyping profiles typical of polyclonal expansions (109, 110). However, both studies examined the repertoire of splenic T cells, which may not reflect the nature of T-cell infiltrates in tissues. Recently, Murphy and colleagues reexamined this question using CTLA-4KO mice on a TCR β chain transgenic background. Contrary to TCRαβ-Tg CTLA-4KO mice on a RAGKO background, which are protected from the lymphoproliferative disease (106), CTLA-4KO mice with a fixed TCRβ repertoire developed lymphoproliferation and died prematurely but with slower kinetics than CTLA-4KO mice (111). Characterization of tissue-infiltrating T cells in TCRβ-Tg CTLA-4KO mice revealed that they were specific for tissue-specific antigens (111), suggesting that the CTLA-4KO disease results from defective tolerance of self-antigen specific T cells. An alternative explanation could be that the CTLA-4KO disease begins with the ‘homeostatic proliferation’ of T cells receiving signals from self-MHC molecules but that tissue infiltration gradually reflects an enrichment in tissue antigen-specific T cells, either because of distinct functions of CTLA-4 as it relates to its structure, as discussed later, or because tissue-specific autoreactive T cells become relatively enriched in the corresponding tissue as enhanced expansion and/or survival occur as a result of cognate interactions with their self-antigens. These mechanisms are not mutually exclusive, and it is possible that CTLA-4 plays an important role both in the control of homeostatic proliferation triggered by self-MHC molecules and in the termination of immune responses to self or foreign antigens.
Structure of the CTLA-4 molecule and molecular basis for its immunoregulatory function The CTLA-4 gene is composed of 4 exons encoding a protein of 223 amino acids (aa) that forms a homodimer of 41-43 kDa. Exon 1 encodes the leader peptide, and exon 2 encodes an Ig-V like domain containing the ligand-binding site in the extracellular portion of the receptor. Exon 3 encodes the transmembrane part, and exon 4 encodes the cytoplasmic tail. The overall homology between the murine and human CTLA-4 protein is 76%, with the greatest divergence observed at the N-terminus, representing the extracellular portion of the receptor. An exception within this domain is the B7-1/B7-2 ligand binding site, which is 100% conserved among mammals, as is the 36 aa intracellular domain (112). The cytoplasmic tail contains a lysine- and a proline-rich motif, as well as 2 tyrosine phosphorylation sites at position 201 and 218 (113), and it appears that the biochemical basis for cell-intrinsic CTLA-4 function depends on the association of a variety of signaling molecules with these sites. A body of work has focused on the interaction of CTLA-4 with its ligands B7-1 and B7-2 to address the mechanisms underlying CTLA-4 inhibitory function upon T-cell activation. Notably, both CTLA-4 and CD28 bind B7-1 and B7-2 using the same MYPPPY motif located in their extracellular domains and therefore directly compete for ligand binding (114). Multiple groups demonstrated the significance of this motif within CTLA-4 and CD28 using single amino acid mutagenesis approaches (115, 116). Importantly, as discussed in detail in the next section, Kuchroo and colleagues have described an alternatively spliced form of CTLA-4, named ligand-independent CTLA-4 (liCTLA-4), which lacks exon2 including the MYPPPY motif essential for binding to ligands B7-1 and B7-2. The fact that CD28 is constitutively expressed on T cells, whereas CTLA-4 is first upregulated upon TCR activation, supports the idea that one role of CTLA-4 is to limit T-cell responses after cells have received an adequate costimulatory signal. In this context, the higher affinity and avidity of CTLA-4 for both B7 ligands compared to CD28 appears to be key (117). The superior binding of CTLA-4 to the B7 molecules are based on residues located N-terminally of the MYPPPY motif in the CDR1-region of CTLA-4, which are not conserved in the CD28 molecule (115, 118). It is important to mention that ligands B7-1 and B7-2 show distinct expression profiles on APCs, which mimic those of CD28 and CTLA-4 on T cells. B7-2 is constitutively expressed on resting APCs, whereas B7-1 is induced after activation, leading to the conclusion that B7-2 is the prevalent ligand for CD28 and B7-1 binds predominantly CTLA-4 (2, 3). The observations that B7-1 mediates recruitment of CTLA-4 to the immunological synapse (IS) and that B7-2 stabilizes CD28 in the IS upon TCR stimulation support this idea (116, 119). In addition, biophysical studies establishing the affinity and avidity of the various receptor-ligand combinations and the crystal structure of B7-1 and B-2 binding to CTLA-4 established a hierarchy in these different molecular interactions that clearly fits the functional model (117, 120-122). Indeed, B7-2 has a higher relative affinity for CD28 than B7-1, and the interaction between B7-1 and CTLA-4 has the highest affinity of all the different combinations (117). Additionally, the B7-2/CD28 and B7-1/CTLA-4 interactions appears structurally different, with single CD28 homodimers binding to single B7-2 monomers versus interaction of bivalent CTLA-4 dimers with B7-1 homodimers that leads to the formation of an organized lattice with high avidity interactions (117, 122).
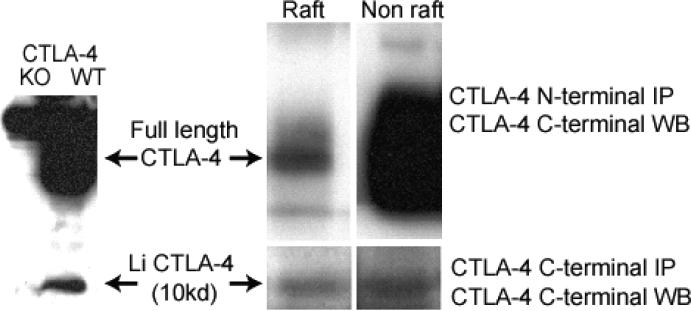
Saito and colleagues (119) recently showed that CTLA-4 and CD28 compete for B7 binding in the CD3low ‘signaling’ subregion of the cSMAC in the IS, especially in conditions of low B7 density. The accumulation of CTLA-4 at the cSMAC hinders the CD28-dependent recruitment of PKC-θ and the subsequent formation of the CARMA-1 complex, possibly altering downstream NF-κB signaling events. Intriguingly, CTLA-4 was first translocated to the TCR microclusters and then moved to the cSMAC, suggesting that CTLA-4 could antagonize both TCR-dependent and CD28-dependent signals. Moreover, the translocation of CTLA-4 to the IS was completely dependent on B7 binding and the MYPPPY motif (119). In this regard, we have found that CTLA-4 accumulates in lipid rafts where it interacts with the TCR complex and controls signaling events in both B7-dependent and B7-independent manner (123, 124, Chikuma S. and Bluestone J.A, unpublished observations). Indeed, we showed that full-length CTLA-4 (flCTLA-4) formed a complex with phosphorylated TCRζ within lipid rafts and that this interaction resulted in the control of levels of phosphorylated TCRζ by CTLA-4 (124). Additionally, we developed a C-terminal anti-CTLA-4 antibody that, in combination with standard N-terminal anti-CTLA-4 antibodies, allowed us to compare the distribution of flCTLA-4 and li-CTLA-4 in lipid rafts vs. non-raft membrane compartments by western blot (Fig. 2). We found that the relative amount of CTLA-4 in the lipid raft fraction was much higher for the ligand-independent form than the full-length molecule (123, 124, Chikuma S. and Bluestone J.A, unpublished observations) (Fig. 2). Moreover, the liCTLA-4 form interacted with TCR components as a consequence of TCR signaling but independently of B7 ligation (Chikuma S. and Bluestone J.A, unpublished observations). We generated Tg mice expressing a mutant (MYPPPY →MYPPAA) ligand non-binding CTLA-4 in the T-cell lineage. We showed that Tg T cells proliferated less vigorously than non-Tg T cells, and this was associated with a marked inhibition of ERK phosphorylation in Tg T cells (125). These data suggest a model in which ligand-independent CTLA-4 inhibits ERK phosphorylation independently of B7 ligands, but dephosphorylation of the TCR requires B7 ligation to stabilize CTLA-4 in the IS.
Fig. 2. Preferential localization of liCTLA-4 in lipid rafts.
2×108 T cells were activated for 3 days by plate-bound anti-CD3 and anti-CD28 mAbs + IL-2 and lysed. Lysates were subjected to sucrose gradients to separate lipid rafts and membrane fractions. The full length and li forms were immunoprecipitated using anti-CTLA-4 N-terminal (4F10) or anti-CTLA-4 C-terminal (polyclonal) Abs and detected by c-terminal polyclonal Abs by western blot analysis.
Besides the competition with CD28 for B7 binding, the inhibitory function of CTLA-4 is in large parts mediated by its cytoplasmic tail. One important feature associated with the intracellular domain is the sub-cellular localization of CTLA-4. In contrast to CD28 which is preferentially localized on the cell surface, the majority of CTLA-4 molecules are found in the trans Golgi network (TGN) as well as in lysosomal and endosomal compartments (in memory T cells) (reviewed in 126). This is mainly mediated by binding of the adapter proteins AP-1 and AP-2 to the non-phosphorylated Y201VKM motif in the cytoplasmic tail of CTLA-4. AP-2 is responsible for retaining CTLA-4 in the TGN and for endocytosis of the receptor from the surface, whereas AP-1 mediates shuttling CTLA-4 from the TGN to lysosomes for degradation (127, 128). Upon T-cell activation, CTLA-4 is rapidly translocated to the site of TCR engagement, and surface expression is stabilized by phosphorylation of the Y201VKM motif, therefore abolishing AP-2 binding and internalization (129, 130). Tyrosine kinases like lck, lyn, and rlk can phosphorylate CTLA-4 at tyrosine 201, thereby allowing the association of PI3K to the Y201VKM sequence (129, 131, 132). While PI3K is known to affect T-cell stimulation by binding to CD28, Rudd and colleagues recently proposed a mechanism by which PI3K activation through CTLA-4 triggers the PKB/Akt pathway, resulting in inactivation of the pro-apoptotic factor BAD and upregulation of the survival factor Bcl-XL (133). These data provide new insights into how CTLA-4 may mediate peripheral tolerance by inducing T-cell unresponsiveness without inducing cell death. However, PKB/Akt is a regulator of multiple signaling pathways and is also activated upon CD28 costimulation. Therefore, it might be not surprising that CTLA-4 was also proposed to inhibit PKB/Akt activation (reviewed in 134, 135). Other biochemical events that have been proposed to be involved in CTLA-4 function include the association of phosphatases like SH2 domain-containing phosphatase-1 (SHP-1), SHP-2, and protein phosphatase 2A (PP2A) with the cytoplasmic tail of CTLA-4. Thus, CTLA-4 ligation was shown to reduce phosphorylation of TCR-ζ as well as other components of the TCR complex like LAT and ζ-associated protein of 70 kDa (ZAP70) (129, 132, 136, 137). This provides a potential mechanism for CTLA-4 inhibitory function by blocking TCR proximal signaling and consequently attenuating cell cycle progression, cytokine production, and proliferation. Moreover, ligation of CTLA-4 was demonstrated to inhibit ERK as well as c-JNK phosphorylation/activation and therefore additionally regulate distal signaling members of the mitogen-associated protein kinase (MAPK) family (138). The overall importance of the cytoplasmic tail and the Y201VKM sequence is most evident in CTLA-4 mutant mice that either lack the entire intracellular domain or carry a point mutation within the Y201VKM motif (139, 140). These mice are not completely protected from the lymphadenopathy observed in CTLA-4KO animals although CTLA-4 surface expression levels are increased, due to abolished AP-2 binding to the Y201VKM sequence (141). Taken together, these observations demonstrate that competing for ligand binding through the extracellular domain is required but by itself not sufficient to block T-cell activation and that the cytoplasmic tail and especially the Y201VKM motif is important to fully mediate CTLA-4 inhibitory function.
CTLA-4 isoforms and their role in its immunoregulatory functions
As the inhibitory function of CTLA-4 is most obvious upon antigen-specific T-cell activation, many efforts have focused on the development of therapeutic approaches that selectively engage the ligand-dependent signaling pathway and significant achievements were observed using CTLA-4-Ig and anti-CTLA-4 antibody therapy in treating autoimmune diseases and various types of cancer, respectively (reviewed in 142). Multiple splice variant isoforms of CTLA-4 have been described, including a ligand non-binding (liCTLA-4) as well as a soluble, secreted variant (sCTLA-4) (143-145). The latter was identified in mouse and human, and elevated levels have been described in patients with autoimmunity but the mechanism of action of sCTLA-4 has yet to be established (143, 146). Importantly, polymorphisms in the CTLA-4 gene, resulting in differential expression of the splice variants, have been associated with the susceptibility to multiple autoimmune diseases, including type 1 diabetes (T1D), multiple sclerosis, rheumatoid arthritis, Grave's disease, hypothyroidism, and systemic lupus erythematosus (144, 147, 148). The recent discovery of the B7-independent, ligand non-binding variant increases the complexity of CTLA-4 biology. This isoform is genetically linked to T1D in the NOD mouse, and the CTLA-4 gene was recently identified as the candidate gene for susceptibility locus Idd5.1 (149). Consequently, diabetes-susceptible NOD mice express only 20% of liCTLA-4 compared to diabetes-resistant mouse strains. Basis for the lack of liCTLA-4 in the NOD background appears to be a single nucleotide polymorphism in exon 2, affecting alternative splicing in favor of inclusion of exon 2 in the final transcript (144, 145). So far, liCTLA-4 has only been described in mouse, where it is expressed at higher levels in naive T cells and resting memory/regulatory T cells (defined as CD4+CD25hi) and downregulated upon T-cell activation, unlike the full-length isoform (flCTLA-4), which is constitutively expressed on Tregs but upregulated on effector T cells only following antigenic stimuli (145, 150-152). This has led to the hypothesis that full length CTLA-4 and liCTLA-4 may display different functions at different stages of immunity and have distinct influences on homeostatic lymphoproliferation, immune activation, and T-cell tolerance.
Previous studies had pointed to a ligand-independent function of CTLA-4 in controlling homeostatic lymphoproliferation, although not necessarily to the existence of an isoform lacking the ectodomain. Indeed, Sharpe and colleagues (153) demonstrated that CTLA-4KO mice are protected from developing lethal lymphoproliferative disease (LPD) when bred onto a B7-1/B7-2 double-KO background to eliminate CD28-dependent T-cell activation required for initiation of the disease process. Consistent with this idea, treatment of these triple KO mice with stimulatory anti-CD28 antibody induced LPD (153). Surprisingly, we discovered that anti-CD28 did not induce disease in the B7 double-KO setting, suggesting that CTLA-4 can function in the absence of ligand binding (8). These studies cannot rule out the presence of an unidentified ligand other than B7 molecules, but they suggest that CTLA-4 can function in naive T cells and control T-cell homeostasis in a B7-independent manner. Consistent with this hypothesis, initial studies by the group of Vijay Kuchroo (145), using a retroviral transfection system, described that liCTLA-4 is capable of negatively signaling into T cells, resulting in a significant decrease in T-cell proliferation and IFN-γ production upon APC/anti-CD3 stimulation. In this setting, liCTLA-4 was even more potent in reducing TCR-ζ phosphorylation than flCTLA-4. Recently, two different transgenic mutant mice, selectively expressing only liCTLA-4 in the knockout background, were generated in our laboratory and the Kuchroo laboratory (125, 149). In both Tg mouse models, constitutive expression of only liCTLA-4 resulted in a partial rescue of the highly activated T-cell phenotype observed in CTLA-4KO mice as well as reduced IFN-γ production. Importantly, a significant delay in lethality caused by the development of LPD, which was consistent with milder clinical symptoms, was observed. In addition, we further demonstrated decreased ERK1 and ERK2 phosphorylation in in vitro stimulated T cells from mice expressing only liCTLA-4, indicating that the B7 non-binding CTLA-4 molecule actively signals into T cells (125). Finally, in studies by Kuchroo and Wicker's group (149), expressing a CD2 promoter driven liCTLA-4 transgene reduced diabetes in the NOD background. However, in both mouse models, there is reasonable concern that expression levels of these transgenes are not appropriate, as they are driven by constitutive promoters and therefore do not reflect the physiological expression pattern of CTLA-4 in different T-cell subsets and at different time points. Thus, to study the in vivo role of liCTLA-4 in regulating T-cell responses and autoimmunity in a more physiological setting, we have engineered a B6.CTLA-4 (floxed-Ex2)-BAC-transgene, resulting in selective expression of liCTLA-4 upon Cre-mediated deletion of exon 2. It is important to mention that the B6-BAC of approximately 20kb contains exclusively the CTLA-4 locus encompassing the endogenous gene promoter and flanking regulatory sequences, shown to be important for CTLA-4 transcriptional regulation. By introducing the B6.CTLA-4-BAC into the NOD background, which appears genetically deficient for liCTLA-4 (144, 145), we were able to restore expression of liCTLA-4 to levels comparable to B6 mice (M. Stumpf and J.A. Bluestone, unpublished observations) and observed that the incidence of cyclophosphamide-induced diabetes was significantly reduced in normal NOD mice as compared to transgenic NOD animals (Stumpf et al., manuscript in preparation). In summary, these studies suggest that the ligand independent CTLA-4 isoform has protective properties for the development of autoimmunity.
Diane Mathis and colleagues (154) previously demonstrated that CTLA-4KO mice in the islet antigen-specific TCR-Tg NOD.BDC2.5 background are protected from LPD and systemic organ infiltration but rapidly develop diabetes by 5-7 weeks of age. It remains possible that the role of liCTLA-4 could be more prominent in the control of homeostatic T-cell proliferation, as evident in both transgenic mouse models discussed above (125, 149), but that the extracellular portion of the receptor appears to be critical to control T-cell activation and tolerance. This is consistent with the finding that expression of liCTLA-4 is downregulated upon T-cell activation, whereas flCTLA-4 is upregulated (145, 150-152). As discussed previously, CTLA-4 appears to be more important for the induction than the maintenance of tolerance (107). The liCTLA-4 may play an important role in the induction of tolerance. In conclusion, a body of work clearly demonstrates that the extracellular and the intracellular portions of the receptor orchestrate and are both key mediators of CTLA-4 inhibitory function. However, the naturally occurring B7-independent CTLA-4 isoform also has biological significance selectively controlling homeostatic proliferation of naive T cells versus T-cell activation and peripheral tolerance.
PD-1: a negative regulator crucial for the maintenance of tolerance in peripheral tissues PD-1 (CD279) is another member of the CD28 family that is expressed on activated T and B cells (6). PD-1 is believed to negatively regulate T and B-cell responses and as such became of interest in the tolerance field. The role of PD-1 in tolerance and autoimmunity has been addressed recently in several reviews (8, 155), therefore we focus on results from our laboratory pertaining to the mechanisms of action of PD-1 in T-cell biology. PD-1 interacts with the two related ligands, PD-L1 and PD-L2 (156, 157). Importantly, PD-L1 and PD-L2 have very different expression patterns, with PD-L2 being expressed mostly on DCs and monocytes in an inducible manner, while PD-L1 is constitutively expressed on T cells, APCs, and many types of non-hematopoietic cell types including vascular endothelial cells, pancreatic islet cells, and neurons (8, 155). This differential expression could relate to the distinct ability of the ligands to induce PD-1-mediated immunomodulation, with PD-L1 usually being more effective than PD-L2 at triggering PD-1 inhibition, and to the scope of PD-1 function in tolerance, which is believed to be predominant at later time points and in peripheral tissues (8). The role of PD-1 in immune tolerance and the prevention of autoimmunity was evidenced the development of autoimmunity in PD-1KO mice. Intriguingly, the tissue tropism of the autoimmune attack depended on the genetic background of the PD-1KO mice. Indeed, PD-1KO mice on a C57BL/6 background displayed arthritis and glomerulonephritis, while PD-1KO BALB/c mice succumbed to autoimmune cardiomyopathy, and PD-1KO NOD mice develop accelerated diabetes (158-160). Polymorphism in the PD-1 gene has also been associated with susceptibility to several autoimmune diseases in humans, including T1D, rheumatoid arthritis, multiple sclerosis, Grave's disease, and systemic lupus erythematosus (161-163). Contrary to CD28 and CTLA-4, PD-1 participates in central tolerance in the thymus and has been shown to be important for both negative and positive selection (164, 165). In addition, our group and others have shown that PD-1 is critical for the maintenance of peripheral tolerance and the prevention of autoimmune diseases, including diabetes and experimental autoimmune encephalitis (8, 107, 155, 166, 167). We examined the pathways, cell subsets, and mechanisms involved in the control of autoimmune diabetes by PD-1. First, we showed that PD-1 interactions with PD-L1, not PD-L2, were essential for the tolerogenic properties of anti-CD3 monoclonal antibodies and antigen-coupled ECDI-fixed cells in the NOD mouse (107). In the model of antigen-specific tolerance induced by ECDI-fixed cells, we found that both PD-1 and CTLA-4 blockade could prevent the unresponsiveness of BDC2.5 T cells and resulted in rapid diabetes in an adoptive transfer model (107). Thus, both PD-1 and CTLA-4 are implicated in the induction of peripheral tolerance. Conversely, PD-1 interactions with PD-L1 uniquely controlled the maintenance of tolerance induced by fixed splenocytes or anti-CD3 therapy (107). Since these tolerogenic protocols do not result in the clearance of tissue infiltration and PD-L1 is expressed on islet cells, these data suggested that interaction of PD-1 on autoreactive T cells with PD-L1 on islet cells could be important for the maintenance of tolerance induced by fixed APCs. In agreement with this hypothesis, we found that fixed APCs isolated from PD-L1KO mice could induce tolerance as efficiently as wildtype cells, suggesting a critical role for PD-L1 expression in the tissue. In concordance with this observation, Sharpe and colleagues (166), using bone marrow chimeras and mice deficient for PD-L1 and/or PD-L2, demonstrated that expression of PD-L1 in the islet tissue rather than in hematopoietic cells was critical to protect against autoimmune diabetes. As a consequence, PD-1 blockade is most effective at precipitating autoimmunity when autoreactive T cells already infiltrate the targeted tissue. This was strikingly illustrated in NOD-B7-2KO mice, which are protected from diabetes and infiltration in pancreatic islets due to defective activation of diabetogenic T cells in pancreatic lymph node but instead develop an autoimmune peripheral neuropathy (168, 169). Indeed, we found that in contrast to NOD mice, treatment of 10-week-old NOD-B7-2KO mice with anti-PD-L1 monoclonal antibodies did not lead to autoimmune diabetes but instead resulted in accelerated peripheral neuropathy (Bour-Jordan H and Bluestone JA, unpublished observations). Collectively, these data suggest a model in which CTLA-4 and PD-1 play complementary and non-overlapping roles in peripheral tolerance, with CTLA-4 predominantly controlling T-cell responses early in lymphoid organs and PD-1 acting at later stages and in peripheral tissues (8).
We have examined the mechanisms of PD-1-mediated tolerogenic effects on autoreactive T cells. Using islet antigen-specific TCR-Tg BDC2.5 effector and regulatory T cells, we showed in an adoptive transfer model that PD-L1 blockade did not affect the ability of BDC2.5 Tregs to control diabetes, suggesting that the control of immune responses by PD-1 is mostly effector T-cell intrinsic (107). However, in a model of maternal-fetal tolerance, PD-L1-expressing Tregs were crucial to maintain tolerance (170). Additionally, PD-L1 was shown to be important for the generation and maintenance of induced Tregs in vitro and in vivo and for their suppressive function in suboptimal conditions of low Treg:T-effector (Teff) cell ratio (171). In contrast, a recent study on human Tregs suggested that PD-1/PD-L1 interactions negatively regulated Treg expansion and suppressive function (172). Thus, while it is clear that PD-1 inhibit effector T cells intrinsically, it is possible that this pathway is operative in Tregs as well. It remains to be determined whether the relative role of PD-1/PD-L1 interactions on Teff vs. Tregs and natural vs. adaptive Tregs correlates with their predominant kinetics and site of action.
We examined the molecular basis for the tolerogenic effect of PD-1 signals on autoreactive T cells using an adoptive transfer model of islet-specific BDC2.5 T cells to induce diabetes and antigen-coupled ECDI-fixed spleen cells to prevent disease and induce tolerance (107). We observed that tolerized autoreactive T cells displayed defects in calcium flux, TCRζ phosphorylation, and Erk phosphorylation (173). Using two-photon laser-scanning microscopy (TPLSM) in antigen-bearing lymph nodes, we found that tolerized T cells had much higher velocity and displacement than non-tolerant T cells (173), for which the observed slower movement and swarming pattern are consistent with interactions with antigen-bearing APCs (174). Importantly, blockade of PD-1/PD-L1 interactions in tolerized animals decreased the velocity and movement of antigen-specific T cells to levels similar to non-tolerized animals, whereas CTLA-4 blockade had no effect (173). As a consequence of this effect of PD-1/PD-L1 interactions on the ‘stop signal’, T cells formed more prolonged and stable interactions with DCs after PD-L1 blockade. In turn, these stronger interactions correlated with increased Erk phosphorylation and amplified effector function as measured by IFN-γ production (173). Neither the formation of T cell-APC conjugate nor TCR proximal signaling and cytokine production were altered by CTLA-4 blockade in tolerized animals. Taken together, these data support a critical and unique role of PD-1/PD-L1 interactions in the maintenance of tolerance and suggest that this is achieved at least in part by the influence of PD-1 on the antigen-specific TCR-induced stop signal.
Extrinsic control of tolerance by costimulatory signals
The role of CD28 in Treg generation, survival, and function
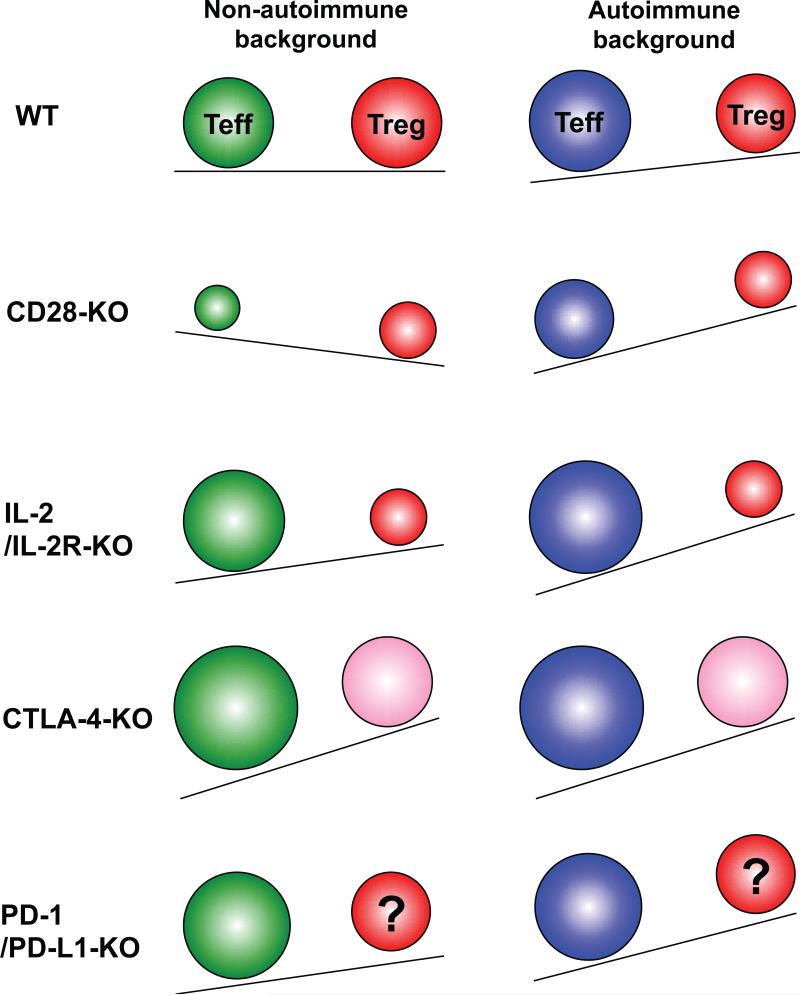
Shortly after Tregs made a comeback on the immunosuppression scene, the importance of CD28 costimulation for their homeostasis and its subsequent effect on autoimmunity was dramatically illustrated in the NOD mouse. Indeed, NOD mice deficient either for CD28 or for its ligand B7-1 and B7-2 developed an aggressive form of diabetes, with accelerated kinetics and increased penetrance, which was associated with a profound reduction in the number of CD4+CD25+ Tregs (152). CD28KO and B7-1/2KO mice are deficient for Tregs in the periphery and in the thymus, and CD28 blockade using CTLA-Ig leads to rapid decline of Treg numbers in both the thymus and secondary lymphoid organs (152, 175, 176). Importantly, adoptive transfer of polyclonal or islet-antigen specific Tregs prevented diabetes in NOD-CD28KO mice (152, 177), demonstrating the critical role of CD28 in the homeostasis of Tregs and the maintenance of tolerance in autoimmune-prone individuals. These observations have therapeutic implications as it relates to treatments currently exploring CD28 blockade in autoimmunity and transplantation, as discussed later in this review.
Thymectomy and adoptive transfer studies have shown that the numerical reduction in Tregs reflects a direct effect of CD28 on the homeostasis of Tregs both in the thymus and in the periphery (176). The mechanisms underlying the control of Treg numbers by CD28 were unclear, but among the CD28 functions known to affect effector T-cell homeostasis, proliferation, IL-2 production, and survival mediated by Bcl-XL upregulation were the most likely suspects. However, constitutive expression of a Bcl-XL transgene did not rescue Tregs after CD28 blockade (176). In addition, the PI3K-binding domain of the CD28 cytoplasmic tail, which has been implicated in the upregulation of Bcl-XL by CD28 in conventional T cells (44), was not necessary for CD28-mediated Foxp3 stabilization and Treg development (88, 178), suggesting that Bcl-XL is not involved in the CD28 control of the Treg population. On the other hand, CD28 is important in Treg proliferation. Although Tregs were initially believed to be anergic based on in vitro data (179, 180), Tregs have since been shown to vigorously proliferate in lymphopenic and non-lymphopenic hosts in vivo (176, 181, 182). CD4+CD25+ Tregs were even found to proliferate more vigorously in vivo than their CD4+CD25− counterparts, a property that may be related to and reflect the fact that their TCR repertoire is skewed towards autoreactivity (24, 25, 183, 184). Using adoptive transfers in non-lymphopenic recipients, we showed that blocking CD28 costimulation completely prevented the spontaneous proliferation of Tregs in vivo (176). It is important to note that the role of CD28 in Treg expansion could control their total numbers in vivo but could also affect their tissue distribution as its relates to self-tolerance and autoimmunity. Indeed, autoreactive Tregs specific for tissue-restricted self-antigens preferentially proliferate and accumulate in lymph nodes draining the relevant tissue, in effect enriching the local milieu for tissue-specific immunoregulation (177, 185). Thus, CD28 is important both to quantitatively maintain the total number of Tregs and to qualitatively improve their efficacy on the population level at the proximity of a given tissue, since tissue antigen-specific Tregs have been shown to be more efficacious than polyclonal Tregs at preventing autoreactivity targeting this tissue (177, 186). A third major mechanism that underlies the role of CD28 in Treg homeostasis could be an indirect influence of IL-2 and IL-2 signaling. Indeed, as discussed below, IL-2 and the IL-2 receptor have been shown to be critically important for the maintenance of the Treg population in the periphery (187-189). Nevertheless, the function of CD28 and IL-2 in Treg homeostasis only partially overlaps. This is best exemplified by the Treg requirement for CD28 signals both in the thymus and periphery, whereas IL-2 appears dispensable for the thymic development of Tregs but instead controls their survival as well as Foxp3 expression in the periphery (187, 190). Using bone marrow chimeras, Singer and colleagues (88) further demonstrated that while CD28 signals were required for IL-2-mediated effects on Treg survival, IL-2 could not rescue CD28-deficient Treg cells. Additionally, we showed in NOD-CD28KO mice that while low steady-state levels of IL-2 contributed to the overall reduction in Treg numbers, exogenous IL-2 could not prevent the rapid depletion of wildtype Tregs following CD28 blockade in vivo (176). Similar results were obtained for human Tregs, as CD28 played a unique role in Treg proliferation while IL-2 predominantly prevented their apoptosis (191).
Intriguingly, while IL-2 signals did not fully recapitulate CD28 costimulation, we found in adoptive transfer experiments that CD28 blockade dramatically lowered CD25 expression independently of IL-2 (176). The direct control of CD25 expression by CD28 costimulation could thus be mechanistically related to the influence of CD28 signals on Treg homeostasis. Taken together, these studies suggest that distinct mediators downstream of CD28 ultimately control the homeostasis of Tregs in the thymus and the periphery. These mediators have yet to be identified, but this will be an important task to gain a better understanding of the molecular pathways controlling Treg development and homeostasis. Of note, while the decrease in Treg numbers due to deficient CD28 signals was observed in all mouse strains tested (NOD, BALB/c, C57BL/6) (152, 175, 176), only NOD-CD28KO mice developed autoimmune diseases. These data suggest that while CD28 costimulation is strictly required for Treg homeostasis, CD28 signals are dispensable for the activation of autoreactive T cells in an autoimmune-prone background and in a Treg-deficient environment. This could be related to the presence of a distinct repertoire skewed towards autoreactivity in NOD mice, to compensatory mechanisms resulting in the use of alternative costimulation molecules, and/or to chronic stimulation by self-antigens that could bypass the need for CD28 costimulation, reminiscent of what has been observed after repeated viral infections (192, 193). The flip side of this coin is the observation that CD28KO mice on non-autoimmune backgrounds do not develop spontaneous autoimmunity despite a profound deficit in Tregs. CD28KO or CTLA-4Ig-treated mice on non-autoimmune background accept mismatched allografts in some circumstances and induced autoimmune diseases such as experimental autoimmune encephalitis and systemic lupus erythematosus. Taken together, these observations suggest that in individuals who are not genetically prone to autoimmunity, the dominant effect of CD28 blockade will be T-cell effector intrinsic and results in hindered immune responses as long as CD28 costimulation is not bypassed by various mechanisms (chronic antigenic stimulation, high-dose/affinity antigen, etc.). Nevertheless, low levels of B7 molecules were later shown to control T-cell stimulation by both self and foreign antigens in a Treg-dependent manner (194, 195), and the importance of CD28 for Treg-mediated immunosuppression has been shown in multiple models, including colitis, graft-versus-host disease, and cardiac allograft rejection (196, 197). Finally, residual Tregs found in CD28KO mice expressed normal levels of Foxp3 and CD25 and could suppress effector T cells as efficiently as wildtype Tregs, suggesting that while CD28 controls Treg numbers, it is not required for their function (175, 176, 180, 198).
Extrinsic control of tolerance by the IL-2 pathway
CD4+ and CD8+ T cells rapidly produce IL-2 upon activation. It exerts its activity by binding to the trimeric IL-2 receptor composed of the high affinity IL-2Rα chain (CD25), the IL-2Rβ (CD122) chain, and the common γ chain (CD132) also shared by IL-7, IL-15, IL-4, IL-9, and IL-21 receptors. IL-2Rα is expressed on T cells and natural killer (NK) cells upon activation, allowing them to respond to low levels of IL-2 in vivo. The trimeric receptor signals through the Janus kinase (Jak)/STAT as well as PI3K and Ras/MAPK pathways. The main consequence of IL-2 signaling is cell cycle progression and increased survival due to transcription of cyclins and anti-apoptotic proteins, such as Bcl-2 (199, 200). In addition, IL-2 signaling upregulates IL-2Rα transcription, creating a positive feedback loop (201). Although it was originally thought that the main role of IL-2 was in the priming and expansion of T-cell responses, analysis of IL-2KO mice revealed that IL-2 had a non-redundant function in controlling T-cell responses, as these mice develop lymphoproliferation and multi-organ autoimmunity (202). Similar results were observed in IL-2Rα KO and IL-2Rβ KO mice (203, 204) as well human patients with mutations in the IL-2Rα gene (205). IL-2 intrinsically promotes T-cell tolerance by mediating the downregulation of the Fas antagonist c-FLIP and thus favoring Fas-mediated apoptosis (206). Furthermore, it was later shown that the multi-organ autoimmunity seen in mice with defective IL-2 signaling was also related to a Treg defect, as the transfer of wildtype Tregs to mice deficient in IL-2Rα or IL-2Rβ prevents lymphoproliferation and autoimmunity (207, 208).
Treg homeostasis is dependent on IL-2, although they do not produce it. In fact, Foxp3 in cooperation with Runx1 and NFAT binds to the IL-2 promoter and inhibits its transcription (40, 209). The role of IL-2 for the induction, survival, and function of Tregs has been widely studied. Initial experiments using high CD25 expression as the sole marker for Tregs concluded that IL-2 was necessary for Treg development, because IL-2Rβ KO mice were completely devoid of CD4+CD25+ cells (188). However, more recent analysis of mice lacking IL-2 or CD25 showed that these mice only have a 50% reduction in the percentage of Foxp3-expressing Tregs in the thymus and periphery (190). Therefore, it is now believed that IL-2 is not strictly required for Treg induction in the thymus.
In the periphery, IL-2 is the major cytokine controlling Treg homeostasis and it is required for optimal Treg maintenance. Neutralization of IL-2 in vivo results in a decrease in the percentage and total number of CD4+CD25+ cells, a decrease in Foxp3 mRNA levels and the development of autoimmune gastritis on the BALB/c background, and exacerbated diabetes on the NOD background (189). Conversely, administration of anti-IL-2/IL-2 complexes, which sustain the biological activity of IL-2 in vivo likely by increasing its half life, leads to increased Treg proliferation resulting in higher Treg percentage and numbers (210). Tregs return to pre-treatment levels 15 days after treatment is discontinued, suggesting that IL-2 availability controls the size of the Treg ‘niche’ (211). This treatment resulted in increased levels of Foxp3 as well as CD25, GITR, CTLA4, and PD-1 expression, which are considered markers of activation and crucial for Treg suppressive function.
To distinguish between the survival and function-promoting roles of IL-2 in Tregs, IL-2 KO mice were crossed with Bim KO mice to allow for the survival of Tregs in the absence of IL-2. These double KO mice have comparable number and percentage of Foxp3+ Tregs as wildtype mice. Interestingly, these mice still succumb to anemia on the BALB/c background similarly to IL-2KO mice (212). It is likely that IL-7 or IL-15, which share the common γ chain in their receptors, can activate some of the same signaling pathways as IL-2. However, these experiments demonstrate that there exist several IL-2-specific pathways that are required for Treg suppressive function. Therefore, while other cytokines are able to partially substitute for IL-2 to maintain Treg survival when IL-2 is limiting or absent, it is required for Treg function, and other cytokines cannot compensate for this role in vivo. Although it was thought that IL-2 mainly acted in an autocrine manner in conventional T cells, it has been shown that the first wave of IL-2 produced by activated CD4+ cells in vivo preferentially binds to and induces STAT5 phosphorylation in Tregs rather than the cells that actually produce the IL-2 (213). This is not due to lack of CD25 expression on the effector cells but likely to expression of the inhibitory molecule suppressor of cytokine signaling 3 (SOCS3). This finding raises the hypothesis that one of the first events after naive T-cell activation in vivo is activation of Tregs, either to prevent autoreactive T-cell activation or to prevent excessive responses to foreign antigens that may lead to tissue damage.
The role of IL-2 in the induction of adaptive Tregs (aTregs) is still controversial. In vitro, IL-2 is required for Foxp3 induction in naive CD4+CD25− T cells (214, 215). However, the effects of IL-2 on aTregs in vivo have been hard to dissect from its effects on nTregs. This will become easier as we find markers to differentiate these two populations. We now know that nTregs express high levels of the transcription factor Helios, while aTregs express low levels (216); further analysis using this marker will elucidate the role of IL-2 in aTreg generation and function. Nonetheless, some aTregs express high levels of CD25; therefore, it is likely that at least a portion of them are also dependent on IL-2 for their homeostasis.
Further evidence of the importance of IL-2 in tolerance and autoimmunity comes from genome wide association studies of patients with autoimmune diseases, which have found single nucleotide polymorphisms (SNPs) and polymorphisms in the IL-2 (217) and IL-2RA/CD25 (218) genes as well as the phosphatase PTPN22 (219), which likely influences IL-2 signaling. In the NOD mouse model, one of the genetic loci necessary for diabetes development, called Idd3, includes the IL-2 gene (220, 221). Moreover, Yamanouchi et al. recently published that the IL-2 gene is the primary genetic determinant of Idd3 and that polymorphism in the IL-2 gene resulted in lower IL-2 production and reduced Treg frequency and function in autoimmune-prone strains (222). Our laboratory has studied the relationship between IL-2, Tregs, and autoimmunity using the NOD model (223). We found that at the time of disease onset, the percentage of Tregs preferentially increases in the pancreatic lymph nodes (PLNs) compared to the inguinal lymph nodes (ILNs). These Tregs are activated, based on decreased CD62L expression, and functional, based on their ability to prevent proliferation of naive BDC2.5 TCR-Tg T cells as well as their clustering and swarming behavior around DCs observed by two-photon microscopy. However, analysis of islet-infiltrating lymphocytes showed that the percentage of Tregs negatively correlates with the size of the infiltrate such that the larger the infiltrate surrounding an individual islet, the lower the percentage of Tregs. Further analysis of pancreas infiltrating Tregs revealed that they have lower expression of CD25 and Foxp3 compared to PLN or ILN Tregs and lower expression of Bcl-2, which is an IL-2-driven anti-apoptotic effector molecule. CD4+ T cells isolated from the islets transcribed significantly lower amounts of IL-2 mRNA in response to restimulation compared to CD4+ T cells from the spleen, suggesting that lack of IL-2 in the inflamed tissue may contribute to changes in the phenotype and function of Tregs. Importantly, treatment of prediabetic NOD mice with low dose anti-IL-2/IL-2 complexes prevented diabetes development and increased the percentage of Tregs in the pancreas as well as their CD25 expression. Furthermore, in collaboration with Salomon and Piaggio, we recently showed that a low-dose IL-2 treatment of only five days restored normoglycemia in new-onset diabetic mice and enhanced CD25 and Foxp3 expression in Tregs (224). Gene expression analysis further revealed that low-dose IL-2 treatment selectively affected the transcription profile of Tregs as compared to effector T cells. We theorize that decreased IL-2 production in the pancreas leads to decreased CD25 expression in pancreas resident Tregs, which results in poor survival and/or function of these cells, contributing to deregulated autoreactive T cells and destruction of the tissue. In addition to being unable to control autoreactive T cells, CD25low Tregs may become unstable. In fact, our laboratory showed that Foxp3 expression can be lost in Tregs, and since the Treg repertoire is skewed towards self-reactivity, this might result in a pathogenic population (225).
Whether the decrease in CD25 expression seen in pancreas-resident Tregs of NOD mice is specific for this model or can be generalized to other autoimmune diseases is still controversial. Lazarski et al. (226) reported that Tregs in the dermis after intradermal OVA-CFA challenge also had lower CD25 expression and concluded that this was a general phenomenon in inflamed tissues rather than a characteristic of autoimmunity. However, in double transgenic mice expressing OVA in the islets (RIP-OVA) and the OVA-reactive TCR DO11.10, which develop rapid diabetes, pancreas-resident Tregs express normal levels of CD25 (226). Therefore, not all Tregs lose CD25 expression in the context of an inflammatory response and autoimmunity is not seen in some cases of reduced CD25 expression. Rather, we believe that the IL-2 pathway deficiency that is genetically programmed in the autoimmune-prone NOD mouse directly relates to subsequent defects in Tregs and immune tolerance and ultimately the development of autoimmune diabetes.
Control of distinct extrinsic immunoregulatory pathways by CTLA-4
The first evidence that CTLA-4 may control effector T-cell homeostasis and tolerance at least in part through extrinsic mechanisms came from the finding that recipients receiving mixed CTLA-4 wildtype and KO bone marrow or splenocytes did not develop the lymphoproliferative disease observed in CTLA-4KO mice or recipients of CTLA-4KO cells only (110, 227). Subsequently, the observation that Tregs constitutively expressed high levels of CTLA-4 (152, 198) suggested that CTLA-4 may be involved in their suppressive function and that Tregs could be the CTLA-4-dependent population able to control CTLA-4KO T cells. Using mixed blastocyst and bone marrow chimeras and adoptive transfer models, Chambers and colleagues (228) recently confirmed that control of CTLA-4KO cells by WT cells required the presence of Foxp3+ Tregs in the wildtype population. Furthermore, they showed that this process was reversible, as elimination of wildtype Tregs using a congenic marker after mixed chimeras were stably established rapidly led to the development of a lymphoproliferative disease caused by CTLA-4KO T cells (228). The functional role of CTLA-4 in Treg biology has been historically difficult to establish, as many in vitro and in vivo studies yielded conflicting results (11). This could be related to a number of factors, including the difficulty to distinguish the role of CTLA-4 in effector vs. regulatory T cells, technical issues such as the use of different experimental systems and reagents, and the complex models needed to study CTLA-4 blockade or deficiency while circumventing the lymphoproliferative disease. Although CTLA-4 blockade was found by some investigators to have no or modest effects on Treg suppressive function in vitro (180, 229, 230), we and others (198, 231, 232)demonstrated that the inhibition of Teff proliferation by Tregs could be abrogated in vitro using higher concentrations or other forms of anti-CTLA-4 monoclonal antibodies. To distinguish whether CTLA-4 blockade directly affects effector or regulatory T cells, several groups have exploited mix-and-match approaches in which CTLA-4 is selectively blocked or deficient on one or the other T-cell subset. Additionally, when CTLA-4KO cells were employed, the lymphoproliferative disease was circumvented either by blocking CD28 signals using CTLA-4Ig injections or B7-deficient mice (59, 153, 233), or by using congenically marked T cells from mixed WT/KO bone marrow chimeras (227). In vitro, our data showed that CTLA-4 blockade altered the suppression of CTLA-4-deficient effector cells by wildtype Tregs, suggesting a direct functional role of CTLA-4 on Tregs (232). Similarly, suppression of CTLA-4-deficient Teff by wildtype Tregs in an in vivo model of colitis was abrogated by CTLA-4 blockade (234). Unexpectedly, despite a loss of Treg function following CTLA-4 blockade, our and Fiona Powrie's laboratories (232, 234) observed that CTLA-4-deficient Tregs could suppress effector responses in vitro and in the colitis model in vivo. However, in both models, it appeared that CTLA-4KO Tregs inhibited Teff cells through immunoregulatory pathways (TGF-β and IL-10, respectively) distinct from other mechanisms often used by wildtype Tregs in these systems (232, 234). Thus, CTLA-4 seems important for Treg function, but Tregs developing in a CTLA-4-deficient environment may be able to overcome the need for CTLA-4 through compensatory mechanisms of suppression. Of note, the ability of CTLA-4KO Tregs to suppress immune responses using compensatory mechanisms is not universal and may depend on the experimental system. Indeed, CTLA-4KO Tregs have been found to inefficiently control Teff responses in vitro and in an autoimmune diabetes model in vivo (235, 236). The reason for these discrepancies is unclear but could relate to the system used to obtain CTLA-KO Tregs from lymphoproliferation-free animals. Nevertheless, it is important to emphasize that most studies evaluating the intrinsic role of CTLA-4 on Teff versus extrinsic function on Tregs have concluded that CTLA-4 is important both intrinsically on effector T cells and extrinsically on Tregs and that these functions synergize in the control of T-cell responses and peripheral tolerance by CTLA-4 (111, 235, 237). Peggs et al. (235) introduced a human CTLA-4 transgene consisting of human CTLA-4 in the extracellular portion of the molecule with a mouse transmembrane and cytoplasmic region. This human CTLA-4 transgene could bind to murine B7 molecules and was functional as evidenced by the ability of the transgene to rescue CTLA-4KO mice, but it allowed the authors to study CTLA-4 function on specific T-cell subsets using either anti-mouse or anti-human CTLA-4 antibodies. In a therapeutic model of tumor rejection, blockade of CTLA-4 only on effector cells improved tumor rejection, whereas Treg-specific blockade had little effect. However, the greatest effects on the kinetics and incidence of tumor rejection were found when CTLA-4 blockade affected both effector and regulatory T cells, indicating synergy in this model (235). Recently, two groups further analyzed the differential role of CTLA-4 on Teff vs. Tregs using mix-and-match models of self-antigen specific TCR-Tg CTLA-4 KO or WT Teff and Tregs, and a transgenic mouse system on a CTLA-4KO background in which the CTLA-4 gene is driven by the IL-2 promoter and thus is expressed in activated effector T cells but not Tregs (111, 237). Both reports confirmed a dual role of CTLA-4 on Teff and Tregs and further showed that CTLA-4 on Tregs was critical to prevent activation of autoreactive Teff in lymphoid tissues but CTLA-4 on Teff prevented infiltration and destruction of peripheral tissues (111, 237). Importantly, Sakaguchi and colleagues (238) generated CTLA-4 conditional KO (cKO) mice that lack CTLA-4 specifically in Foxp3-expressing Tregs. A Treg-specific role of CTLA-4 was illustrated by the finding that CTLA-4 cKO mice still succumbed to a fatal lymphoproliferative disease. However, CTLA-4 cKO mice developed the disease with slower kinetics than CTLA-4KO mice, demonstrating once again an effector T-cell-intrinsic role of CTLA-4 in maintaining T-cell homeostasis and tolerance (238). We recently demonstrated using a fluorescent reporter system in vivo that Foxp3+ T cells can downregulate expression of Foxp3 and that ‘exFoxp3’ cells can be generated from both unstable natural and adaptive Tregs (225). Since CTLA-4 cKO mice were generated using a floxed allele of CTLA-4 and Foxp3-driven Cre, it is thus important to keep in mind that CTLA-4-deficient exFoxp3 cells could contribute to the lymphoproliferative disease in CTLA-4 cKO mice (238). Finally, CTLA-4 is dispensable for the development, survival, and homeostasis of Tregs, as normal numbers and percentages of CD4+CD25+Foxp3+ Tregs are found in the absence of CTLA-4 (232, 238, 239).
The mechanisms underlying the control of Treg function by CTLA-4 are still unclear. Accumulating reports point to an altered TCR downstream signaling in Tregs, implicating decreased ERK1/2, CD3-ζ, and Akt phosphorylation (240, 241). Since all these molecules are targeted by CTLA-4 in effector T cells, it is possible that constitutive expression of CTLA-4 on Tregs participates in decreasing TCR signaling. Additionally, recent data by Saito and colleagues (119) suggest that constitutive expression of CTLA-4 blocked the accumulation of CD28 and PKCθ at the cSMAC in Tregs and participated in maintaining their anergic state, which has been associated with their suppressive function (119, 242, 243). Both Foxp3-deficient and CTLA-4-deficient mice develop lymphoproliferation and multi-organ autoimmunity, resulting in premature death of the animals. To examine the relationship between the two conditions, we performed complementation studies by reconstituting lethally irradiated RAGKO recipients with CTLA-4KO and Scurfy (Foxp3-deficient) bone marrow (BM) either separately or together (244). As expected, recipients receiving either CTLA-4KO or Scurfy BM alone developed a lymphoproliferative disease similar to the original strain. We found that reconstitution with a mixture of CTLA-4KO and Scurfy BM cells did not prevent lymphoproliferation and premature death in chimeric recipients, suggesting that CTLA-4 and Foxp3 must be expressed in cis in the same cell to fully prevent autoimmunity and lymphoproliferation (244). However, the mixture of CTLA-4KO and Scurfy BM afforded some level of protection, as mixed BM chimeric recipients developed lymphoproliferation with delayed kinetics compared to CTLA-4KO or Scurfy BM alone, suggesting that CTLA-4 has a Treg-independent extrinsic function in the control of T-cell tolerance and homeostasis (244). Consistent with this idea, gene expression studies performed on CTLA-4 KO and wildtype T cells isolated from mixed BM recipients revealed only very modest differences in gene expression, suggesting that CTLA-4+ Tregs controlled CTLA-4KO effector T cells at least in part indirectly through other cell populations (228). In this regard, we previously reported that Tregs were found to directly interact with APCs rather than Teff cells in lymph nodes using two-photon microscopy in situ (174). This correlated with a sharp reduction in the ability of APCs to induce the proliferation of autoreactive T cells. This obervation has led to the hypothesis that Tregs could control Teff responses partly by affecting APCs and that CTLA-4 could play a role in this process (10, 11). CTLA-4 did not affect the aggregation of Tregs around dendritic cells, suggesting that it may affect APCs functionally rather than disrupt the Treg-APC interaction (245). In this regard, incubation of DCs with Tregs, but not CD4+CD25− T cells, results in a decrease in B7-1 and B7-2 expression in DCs in vitro that could affect their ability to stimulate effector T cells (246). Importantly, the downmodulation of B7 expression required direct contacts between Tregs and APCs and was dependent on the presence of CTLA-4 on Tregs (236, 238, 245, 247). Furthermore, it appears to be a widely used mechanism across Treg and APCs subsets and species, as B7 downmodulation was observed on B cells and DCs after interactions with human or murine Tregs and adaptive or natural Tregs (236, 245, 246, 248, 249). A distinct mechanism for CTLA-4-dependent Treg-mediated modification of APC function could involve the production of the immunosuppressive enzyme indoleamine 2,3-dioxygenase (IDO) by APCs. IDO has been proposed to inhibit effector T-cell responses by triggering the degradation of tryptophan. Additionally, treatment of DCs with CTLA-4-Ig has been shown to induce IDO production by DCs involving reverse signaling through B7 molecules (250). IDO production by DCs has been implicated in the maintenance of peripheral tolerance in several settings, including fetal tolerance, autoimmunity, transplantation, and tumor immunity (reviewed in 251). Notably, interaction of Tregs with DCs was shown to trigger IDO production and tryptophan catabolism in DCs in a process dependent on interactions between CTLA-4 on Tregs and B7 molecules on DCs (252). Although it has not been formally proven to occur in Treg-mediated immunosuppression, recent discoveries on the influence of CTLA-4 on the transcription factor Foxo3 and its effect on T-cell responses suggest that this pathway could be involved in CTLA-4-dependent Treg immunosuppression. Indeed, binding of CTLA-4 to B7 molecules had been shown to trigger the nuclear translocation of the Foxo3 transcription factor (253). Hedrick and colleagues later reported that the CTLA-4-induced nuclear localization of Foxo3 in DCs limits their production of IL-6, which in turn controls expansion of the T-cell population (254) due to the pro-survival effects of IL-6 on activated T cells (255). Competition between CTLA-4 on Tregs and CD28 on Teff for B7 binding is unlikely to fully account for the CTLA-4-dependent inhibition of T-cell responses by Tregs due to the 5-10:1 ratio of Teff:Treg in CD4+ T cells. However, increasing B7 levels by expression of a B7-2 transgene abrogated the protection from lymphoproliferative disease observed in CTLA-4 KO and wildtype mixed BM chimeras, suggesting that competition for B7 binding may be an additional CTLA-4-dependent Treg-mediated extrinsic mechanism of tolerance (228). Finally, the fact that expression of the ligand independent form of CTLA-4 only results in a significant decrease of activated T cells in three transgenic mouse models compared to a CTLA-4KO background, as discussed previously (125, 149), raised the possibility that this phenotype is a consequence of improved Treg function by liCTLA-4. The involvement of liCTLA-4 in Tregs could help explain why the role of CTLA-4 in Treg function has been so difficult to establish using anti-CTLA-4 antibodies (11). By definition, liCTLA-4 cannot fully account for all CTLA-4-mediated mechanisms of Tregs function, since a number of them directly rely on interactions with B7 molecules, as described above. However, from a theoretical point-of-view, a role for liCTLA-4 in Tregs could help explain the following conundrum: Tregs constitutively express CTLA-4 and CTLA-4 binds B7 molecules with a higher affinity than CD28, but CD28 signals are necessary for Treg survival and homeostasis. Thus, now that the importance of CTLA-4 for Treg function is firmly established, it will be important to directly evaluate the relative role of full-length versus ligand-independent CTLA-4 in Treg function.
Targeting costimulatory pathways in immunotherapy
The profound importance of CD28, CTLA-4, and PD-1 for tolerance and immune system homeostasis in mouse models has prompted the development of several human drugs that target molecules involved in costimulation. Conversely, the seminal discovery that costimulation blockade can affect Tregs more than effector T cells (152) suggests that it is difficult to predict the effects of costimulation modulators. Thus, caution is warranted in using immunotherapeutics targeting CD28 or CTLA-4, several of which are already in clinical trials or approved for use by the Federal Drug Administration (FDA) (4, 256-258). Work in mice (52, 259) and non-human primates (260) has shown that blocking B7-1/2 with soluble CTLA-4 linked to an Ig heavy chain can induce durable tolerance to allografts and xenografts. CTLA-4-Ig binds to B7-1/2 with higher affinity than the endogenous CD28 expressed on T cells, preventing CD28-mediated costimulation (5). Subsequent trials of CTLA-4-Ig fusion proteins abatacept and a higher affinity variant, belatacept, have shown efficacy in a wide range of transplant and autoimmune settings. For example, a phase I open-label, dose-escalation trial of abatacept in 1999 showed that 46% of patients with psoriasis showed a 50% or greater improvement of their disease activity (261). Abatacept has subsequently been approved for the treatment of rheumatoid arthritis (RA) and juvenile rheumatoid arthritis (JRA). A randomized, double-blind placebo-controlled trial of abatacept in patients with RA who had an inadequate response to tumor necrosis factor (TNF) blockers demonstrated a 50.4% response rate in the abatacept-treated group (measured by American College of Rheumatology 20) compared to 19.5% response in the placebo group (262). In a double blind, controlled trial of patients with JRA, who had previously failed to respond to a disease-modifying therapy, abatacept decreased the risk of flare by more than 1/3 compared to placebo (263). Importantly, neither of these trials reported a significant increase in the rate of infection in treated patients, implying that the immunosuppressive properties of the drug are targeted to the pathological immune response and not to normal immunity against microbes. However, abatacept therapy did not appear to significantly affect flares of systemic lupus erythematosus in a phase IIb randomized, double-blind, placebo-controlled trial (264). Thus, unlike traditional immunosuppressive drugs, abatacept does not appear to compromise normal immunity, but its efficacy may be limited to diseases where CD28 costimulation is a central driver of the autoimmune process at the time of treatment. In patients who received a kidney transplant, belatacept has been shown not to be inferior to cyclosporine in preventing episodes of acute rejection (265). Importantly, belatacept does not have the serious nephrotoxic side effects of cyclosporine.
Since B7-CD28 interactions are known to be critical for peripheral Treg homeostasis (11, 152), complete blockade of B7 in patients treated with abatacept/belatacept might paradoxically interfere with peripheral survival of Tregs and provoke autoimmunity. However, kidney transplant patients treated with belatacept did not have a long-term difference in the numbers of circulating Tregs, and, in fact, had increased numbers of Foxp3+ cells in graft biopsies, compared to patients treated with a calcineurin inhibitor (266). These data are in contrast to studies in mice, where blockade of B7/CD28 interactions caused a rapid decrease in Treg numbers (152, 176). These different results may arise from the subsaturating doses of belatacept used in human studies, which may affect effector T cells to a greater extent than regulatory T cells (266). The CD25-specific monoclonal antibody basiliximab is a FDA-approved drug that has been shown to reduce acute rejection of transplanted kidneys (267). Its proposed mechanism of action (shared with the similar antibody daclizumab) is blockade of the high affinity α-chain of the IL-2 receptor (CD25). This blockade is proposed to interfere with IL-2 growth signals and arrest proliferation of alloreactive T cells after transplantation. However, there is evidence in mouse models that regulatory T cells are more sensitive to local IL-2 levels than are effector T cells (223, 224). Importantly, mice lacking the IL-2 or the CD25 gene develop spontaneous autoimmunity, demonstrating the importance of these molecules in maintaining tolerance (268). Thus, it is unclear if the proposed mechanism of action accounts for the observed clinical outcomes.
In murine studies, blocking CD28 can induce tolerance, but blocking CTLA-4 with a monoclonal antibody has been used as an effective means to break tolerance, especially in tumor settings (256). Ipilimumab is a fully human monoclonal antibody that binds to human CTLA-4 and blocks its binding to B7. This drug has been shown to extend the lifespan of patients with stage 3 or 4 melanoma from a median of 6.4 to 10.0 months (269). The drug induces a strong cell-mediated immune response to tumor cells (270), but adverse immune-related side effects such as colitis, rashes, and endocrine abnormalities were collectively about twice as common in ipilimumab-treated cancer patients compared to control-treated cancer patients (269). These results indicate that ipilimumab can break tolerance against both abnormal cancer antigens and normal self-antigens or commensal flora. These serious toxicities of Ipilimumab may hinder its use in the treatment of cancers in which traditional chemotherapy has been established to be effective.
Pre-clinical studies in rats with a CD28-superagonist antibody showed that treatment expanded the numbers of Treg cells in vivo and that these Tregs showed enhanced suppressive functions in vitro and in vivo (271). These results prompted the development of a humanized anti-CD28 superagonist antibody by TeGenero, which paradoxically provoked a life-threatening cytokine storm and multi-organ failure in six volunteers treated with the antibody (0.1 mg/kg TGN1412) (272). This unexpected result may stem from differences in binding affinity between the rodent and human antibodies or from the differences in T-cell reactivity between laboratory strains of rats kept in clean facilities with small numbers of antigen-specific memory cells and human patients with many antigen-experienced T cells. A retrospective analysis of non-human primate studies suggested the activation properties of the monoclonal antibody, but these properties were underappreciated due to problems in the in vitro assays and differences in the post-translational modification of the CD28 molecule in this species.
A humanized anti-PD-1 monoclonal antibody (MDX-1106 (ONO-4538) has been developed by Ono Pharmaceuticals and is being tested by Medarex, Inc. in a Phase 1 study in patients with recurrent or treatment-refractory cancer. Preliminary data support the safety, tolerability and pharmacokinetic profile of a single-dose of the drug. In addition, preliminary evidence of anti-tumor activity was observed, including one patient with colorectal carcinoma who experienced a partial response was been durable for more than 6 months.
Drugs targeting these costimulatory pathways have great promise for the treatment of disease. However, the yin-yang activities of many of these pathways will require careful clinical development that cannot always be predicted by the rodent studies (186, 266). Moreover, the varied consequences of costimulatory blockade highlight the need for the development of combination immunomodulatory therapies that amplify and create predictable outcomes on immune system function.
Concluding remarks
Tremendous strides have been made in knowledge of the biology of costimulatory molecules and their influence on peripheral tolerance since the discovery of CD28. It is now clear that the simple concepts that governed the early days of the costimulation field—positive costimulators positively influence effector T cells and prevent tolerance, negative regulators negatively influence effector T cells and favor tolerance–have to be revised in view of the ever-increasing complexity of the system. In particular, the realization that costimulatory molecules controlled peripheral tolerance through both intrinsic and extrinsic mechanisms (Fig. 3) drastically changed the understanding of their mode of actions. Additionally, the net result of blockade of a given pathway can be different in autoimmune versus non-autoimmune backgrounds. Nevertheless, general conclusions can be made on the affect of individual costimulatory molecules on immune responses based on the recent body of literature (Fig. 3). Despite being critical for Treg homeostasis, CD28 remains the most important positive costimulatory molecule for effector T cells. Thus, CD28 costimulation can have opposite effects on immune responses depending on the immunological context and genetic background and consequences of CD28 blockade on any given immune response are perhaps the most difficult to predict. Similarly, IL-2 was initially described as a crucial growth factor for effector T cells but now appears deeply involved in immunoregulation through its effects on Tregs. Conversely, CTLA-4 does not appear to share the same duplicity as CD28 and IL-2, since its effect on effector T cells, Tregs, and APCs all poise the system for immunoregulation. PD-1 also negatively regulates immune responses, although at the moment its influence is more definitely established in effector T cells than Tregs. Moreover, the apparent redundancy between some of these pathways actually masks some fundamental differences in their influence on T-cell responses and tolerance, leaving a great deal still to be learned to better understand the role of these molecules in immunity and harness their activities for clinical intervention.
Fig. 3. Simplified model of the overall effect of the blockade of individual costimulatory pathways.
This simplified model shows the overall result of the blockade of individual costimulation pathways on the balance of effector (Teff) versus regulatory (Tregs) responses. In wildtype (WT) mice, Teff and Treg cells coexist to ensure productive immune responses and their efficient termination; in autoimmune backgrounds, the balance of Teff and Treg cells is skewed towards autoreactivity. In CD28KO mice on a non-autoimmune background, both Teff and Tregs are affected, but CD28 deficiency on Teff still precludes many immune responses. However, on an autoimmune background, Teff cells can bypass the need for CD28 to get fully activated and the defective Treg compartment leads to exacerbated autoimmunity. Deficiency in IL-2 signals affect both Teff and Tregs cells but result in autoreactivity due to improper Teff death and a defective Treg compartment. CTLA-4 deficiency dramatically affects Teff responses and inhibits Treg function (although not their numbers), resulting in dramatic lymphoproliferation and autoimmunity. PD-1 regulates self-antigen-specific T cells, and deficiency in the PD-1/PD-L1 pathway leads to autoimmunity in all backgrounds due to its effect at least on Teff cells and perhaps on Treg cells as well, with particularly dramatic consequences in autoimmune backgrounds.
Acknowledgements
The authors thank the members of the Bluestone laboratory for the many experiments that represent the basis for this review. We also wish to thank Drs. Abul Abbas and Mark Anderson for critical reading of the manuscript and helpful suggestions. This research was supported by grants from the NIH, JDRF and grateful donors over the past decade. JAB is a consultant for Becton-Dickenson and MacroGenics, Inc., who are developing regulatory T-cell technologies and anti-CD3 mAbs, respectively.
References
- 1.Mueller DL, Jenkins MK, Schwartz RH. Clonal expansion versus functional clonal inactivation: a costimulatory signaling pathway determines the outcome of T cell antigen receptor occupancy. Annu Rev Immunol. 1989;7:445–480. doi: 10.1146/annurev.iy.07.040189.002305. [DOI] [PubMed] [Google Scholar]
- 2.Lenschow DJ, Walunas TL, Bluestone JA. CD28/B7 system of T cell costimulation. Annu Rev Immunol. 1996;14:233–258. doi: 10.1146/annurev.immunol.14.1.233. [DOI] [PubMed] [Google Scholar]
- 3.Salomon B, Bluestone JA. Complexities of CD28/B7: CTLA-4 costimulatory pathways in autoimmunity and transplantation. Annu Rev Immunol. 2001;19:225–252. doi: 10.1146/annurev.immunol.19.1.225. [DOI] [PubMed] [Google Scholar]
- 4.Bluestone JA, St Clair EW, Turka LA. CTLA4Ig: bridging the basic immunology with clinical application. Immunity. 2006;24:233–238. doi: 10.1016/j.immuni.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Linsley PS, Nadler SG. The clinical utility of inhibiting CD28-mediated costimulation. Immunol Rev. 2009;229:307. doi: 10.1111/j.1600-065X.2009.00780.x. [DOI] [PubMed] [Google Scholar]
- 6.Greenwald RJ, Freeman GJ, Sharpe AH. The B7 family revisited. Annu Rev Immunol. 2005;23:515–548. doi: 10.1146/annurev.immunol.23.021704.115611. [DOI] [PubMed] [Google Scholar]
- 7.Agarwal A, Newell KA. The role of positive costimulatory molecules in transplantation and tolerance. Curr Opin Organ Transplant. 2008;13:366–372. doi: 10.1097/MOT.0b013e328306115b. [DOI] [PubMed] [Google Scholar]
- 8.Fife BT, Bluestone JA. Control of peripheral T-cell tolerance and autoimmunity via the CTLA-4 and PD-1 pathways. Immunol Rev. 2008;224:166–182. doi: 10.1111/j.1600-065X.2008.00662.x. [DOI] [PubMed] [Google Scholar]
- 9.Sakaguchi S, Yamaguchi T, Nomura T, Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133:775–787. doi: 10.1016/j.cell.2008.05.009. [DOI] [PubMed] [Google Scholar]
- 10.Tang Q, Bluestone JA. The Foxp3+ regulatory T cell: a jack of all trades, master of regulation. Nat Immunol. 2008;9:239–244. doi: 10.1038/ni1572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Bour-Jordan H, Bluestone JA. Regulating the regulators: costimulatory signals control the homeostasis and function of regulatory T cells. Immunol Rev. 2009;229:41–66. doi: 10.1111/j.1600-065X.2009.00775.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gardner JM, Fletcher AL, Anderson MS, Turley SJ. AIRE in the thymus and beyond. Curr Opin Immunol. 2009;21:582–589. doi: 10.1016/j.coi.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Aaltonen J, Bjorses P. Cloning of the APECED gene provides new insight into human autoimmunity. Ann Med. 1999;31:111–116. doi: 10.3109/07853899708998786. [DOI] [PubMed] [Google Scholar]
- 14.Anderson MS, et al. Projection of an immunological self shadow within the thymus by the aire protein. Science. 2002;298:1395–1401. doi: 10.1126/science.1075958. [DOI] [PubMed] [Google Scholar]
- 15.Gardner JM, et al. Deletional tolerance mediated by extrathymic Aire-expressing cells. Science. 2008;321:843–847. doi: 10.1126/science.1159407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mueller DL. Mechanisms maintaining peripheral tolerance. Nat Immunol. 11:21–27. doi: 10.1038/ni.1817. [DOI] [PubMed] [Google Scholar]
- 17.Goverman J. Autoimmune T cell responses in the central nervous system. Nat Rev Immunol. 2009;9:393–407. doi: 10.1038/nri2550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bianchi T, et al. Maintenance of peripheral tolerance through controlled tissue homing of antigen-specific T cells in K14-mOVA mice. J Immunol. 2009;182:4665–4674. doi: 10.4049/jimmunol.0803628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwartz RH. T cell anergy. Annu Rev Immunol. 2003;21:305–334. doi: 10.1146/annurev.immunol.21.120601.141110. [DOI] [PubMed] [Google Scholar]
- 20.Hughes PD, Belz GT, Fortner KA, Budd RC, Strasser A, Bouillet P. Apoptosis regulators Fas and Bim cooperate in shutdown of chronic immune responses and prevention of autoimmunity. Immunity. 2008;28:197–205. doi: 10.1016/j.immuni.2007.12.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hao Z, Hampel B, Yagita H, Rajewsky K. T cell-specific ablation of Fas leads to Fas ligand-mediated lymphocyte depletion and inflammatory pulmonary fibrosis. J Exp Med. 2004;199:1355–1365. doi: 10.1084/jem.20032196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hildeman D, Jorgensen T, Kappler J, Marrack P. Apoptosis and the homeostatic control of immune responses. Curr Opin Immunol. 2007;19:516–521. doi: 10.1016/j.coi.2007.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wing K, Sakaguchi S. Regulatory T cells exert checks and balances on self tolerance and autoimmunity. Nat Immunol. 2010;11:7–13. doi: 10.1038/ni.1818. [DOI] [PubMed] [Google Scholar]
- 24.Hsieh CS, Zheng Y, Liang Y, Fontenot JD, Rudensky AY. An intersection between the self-reactive regulatory and nonregulatory T cell receptor repertoires. Nat Immunol. 2006;7:401–410. doi: 10.1038/ni1318. [DOI] [PubMed] [Google Scholar]
- 25.Jordan MS, et al. Thymic selection of CD4+CD25+ regulatory T cells induced by an agonist self-peptide. Nat Immunol. 2001;2:301–306. doi: 10.1038/86302. [DOI] [PubMed] [Google Scholar]
- 26.Bluestone JA, Abbas AK. Natural versus adaptive regulatory T cells. Nat Rev Immunol. 2003;3:253–257. doi: 10.1038/nri1032. [DOI] [PubMed] [Google Scholar]
- 27.Bennett CL, et al. The immune dysregulation, polyendocrinopathy, enteropathy, X-linked syndrome (IPEX) is caused by mutations of FOXP3. Nat Genet. 2001;27:20–21. doi: 10.1038/83713. [DOI] [PubMed] [Google Scholar]
- 28.Fontenot JD, Gavin MA, Rudensky AY. Foxp3 programs the development and function of CD4+CD25+ regulatory T cells. Nat Immunol. 2003;4:330–336. doi: 10.1038/ni904. [DOI] [PubMed] [Google Scholar]
- 29.Steinman RM, Hawiger D, Nussenzweig MC. Tolerogenic dendritic cells. Annu Rev Immunol. 2003;21:685–711. doi: 10.1146/annurev.immunol.21.120601.141040. [DOI] [PubMed] [Google Scholar]
- 30.Jenkins MK, Taylor PS, Norton SD, Urdahl KB. CD28 delivers a costimulatory signal involved in antigen-specific IL-2 production by human T cells. J Immunol. 1991;147:2461–2466. [PubMed] [Google Scholar]
- 31.Bromley SK, et al. The immunological synapse and CD28-CD80 interactions. Nat Immunol. 2001;2:1159–1166. doi: 10.1038/ni737. [DOI] [PubMed] [Google Scholar]
- 32.Tuosto L, Acuto O. CD28 affects the earliest signaling events generated by TCR engagement. Eur J Immunol. 1998;28:2131–2142. doi: 10.1002/(SICI)1521-4141(199807)28:07<2131::AID-IMMU2131>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 33.Viola A, Schroeder S, Sakakibara Y, Lanzavecchia A. T lymphocyte costimulation mediated by reorganization of membrane microdomains. Science. 1999;283:680–682. doi: 10.1126/science.283.5402.680. [DOI] [PubMed] [Google Scholar]
- 34.Viola A, Lanzavecchia A. T cell activation determined by T cell receptor number and tunable thresholds. Science. 1996;273:104–106. doi: 10.1126/science.273.5271.104. [DOI] [PubMed] [Google Scholar]
- 35.Yokosuka T, Saito T. Dynamic regulation of T-cell costimulation through TCR-CD28 microclusters. Immunol Rev. 2009;229:27–40. doi: 10.1111/j.1600-065X.2009.00779.x. [DOI] [PubMed] [Google Scholar]
- 36.Frauwirth KA, et al. The CD28 signaling pathway regulates glucose metabolism. Immunity. 2002;16:769–777. doi: 10.1016/s1074-7613(02)00323-0. [DOI] [PubMed] [Google Scholar]
- 37.Rowell EA, Walsh MC, Wells AD. Opposing roles for the cyclin-dependent kinase inhibitor p27kip1 in the control of CD4+ T cell proliferation and effector function. J Immunol. 2005;174:3359–3368. doi: 10.4049/jimmunol.174.6.3359. [DOI] [PubMed] [Google Scholar]
- 38.Appleman LJ, Berezovskaya A, Grass I, Boussiotis VA. CD28 costimulation mediates T cell expansion via IL-2-independent and IL-2-dependent regulation of cell cycle progression. J Immunol. 2000;164:144–151. doi: 10.4049/jimmunol.164.1.144. [DOI] [PubMed] [Google Scholar]
- 39.Boonen GJ, van Dijk AM, Verdonck LF, van Lier RA, Rijksen G, Medema RH. CD28 induces cell cycle progression by IL-2-independent down-regulation of p27kip1 expression in human peripheral T lymphocytes. Eur J Immunol. 1999;29:789–798. doi: 10.1002/(SICI)1521-4141(199903)29:03<789::AID-IMMU789>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 40.Wu LX, et al. CD28 regulates the translation of Bcl-xL via the phosphatidylinositol 3-kinase/mammalian target of rapamycin pathway. J Immunol. 2005;174:180–194. doi: 10.4049/jimmunol.174.1.180. [DOI] [PubMed] [Google Scholar]
- 41.Boise LH, et al. CD28 costimulation can promote T cell survival by enhancing the expression of Bcl-XL. Immunity. 1995;3:87–98. [PubMed] [Google Scholar]
- 42.Howland KC, Ausubel LJ, London CA, Abbas AK. The roles of CD28 and CD40 ligand in T cell activation and tolerance. J Immunol. 2000;164:4465–4470. doi: 10.4049/jimmunol.164.9.4465. [DOI] [PubMed] [Google Scholar]
- 43.Sperling AI, Auger JA, Ehst BD, Rulifson IC, Thompson CB, Bluestone JA. CD28/B7 interactions deliver a unique signal to naive T cells that regulates cell survival but not early proliferation. J Immunol. 1996;157:3909–3917. [PubMed] [Google Scholar]
- 44.Burr JS, et al. Cutting edge: distinct motifs within CD28 regulate T cell proliferation and induction of Bcl-XL. J Immunol. 2001;166:5331–5335. doi: 10.4049/jimmunol.166.9.5331. [DOI] [PubMed] [Google Scholar]
- 45.Okkenhaug K, et al. A point mutation in CD28 distinguishes proliferative signals from survival signals. Nat Immunol. 2001;2:325–332. doi: 10.1038/86327. [DOI] [PubMed] [Google Scholar]
- 46.Croft M, Bradley LM, Swain SL. Naive versus memory CD4 T cell response to antigen. Memory cells are less dependent on accessory cell costimulation and can respond to many antigen-presenting cell types including resting B cells. J Immunol. 1994;152:2675–2685. [PubMed] [Google Scholar]
- 47.London CA, Lodge MP, Abbas AK. Functional responses and costimulator dependence of memory CD4+ T cells. J Immunol. 2000;164:265–272. doi: 10.4049/jimmunol.164.1.265. [DOI] [PubMed] [Google Scholar]
- 48.Ndejembi MP, et al. Control of memory CD4 T cell recall by the CD28/B7 costimulatory pathway. J Immunol. 2006;177:7698–7706. doi: 10.4049/jimmunol.177.11.7698. [DOI] [PubMed] [Google Scholar]
- 49.Borowski AB, et al. Memory CD8+ T cells require CD28 costimulation. J Immunol. 2007;179:6494–6503. doi: 10.4049/jimmunol.179.10.6494. [DOI] [PubMed] [Google Scholar]
- 50.Wells AD, et al. Requirement for T-cell apoptosis in the induction of peripheral transplantation tolerance. Nat Med. 1999;5:1303–1307. doi: 10.1038/15260. [DOI] [PubMed] [Google Scholar]
- 51.Dai Z, Konieczny BT, Baddoura FK, Lakkis FG. Impaired alloantigen-mediated T cell apoptosis and failure to induce long-term allograft survival in IL-2-deficient mice. J Immunol. 1998;161:1659–1663. [PubMed] [Google Scholar]
- 52.Lenschow DJ, et al. Long-term survival of xenogeneic pancreatic islet grafts induced by CTLA4lg. Science. 1992;257:789. doi: 10.1126/science.1323143. [DOI] [PubMed] [Google Scholar]
- 53.Wells AD, Liu QH, Hondowicz B, Zhang J, Turka LA, Freedman BD. Regulation of T cell activation and tolerance by phospholipase C gamma-1-dependent integrin avidity modulation. J Immunol. 2003;170:4127–4133. doi: 10.4049/jimmunol.170.8.4127. [DOI] [PubMed] [Google Scholar]
- 54.Rowell EA, Wang L, Hancock WW, Wells AD. The cyclin-dependent kinase inhibitor p27kip1 is required for transplantation tolerance induced by costimulatory blockade. J Immunol. 2006;177:5169–5176. doi: 10.4049/jimmunol.177.8.5169. [DOI] [PubMed] [Google Scholar]
- 55.Li L, Iwamoto Y, Berezovskaya A, Boussiotis VA. A pathway regulated by cell cycle inhibitor p27Kip1 and checkpoint inhibitor Smad3 is involved in the induction of T cell tolerance. Nat Immunol. 2006;7:1157–1165. doi: 10.1038/ni1398. [DOI] [PubMed] [Google Scholar]
- 56.Wells AD, Walsh MC, Bluestone JA, Turka LA. Signaling through CD28 and CTLA-4 controls two distinct forms of T cell anergy. J Clin Invest. 2001;108:895–903. doi: 10.1172/JCI13220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Wells AD, Walsh MC, Sankaran D, Turka LA. T cell effector function and anergy avoidance are quantitatively linked to cell division. J Immunol. 2000;165:2432–2443. doi: 10.4049/jimmunol.165.5.2432. [DOI] [PubMed] [Google Scholar]
- 58.Bour-Jordan H, Grogan JL, Tang Q, Auger JA, Locksley RM, Bluestone JA. CTLA-4 regulates the requirement for cytokine-induced signals in T(H)2 lineage commitment. Nat Immunol. 2003;4:182–188. doi: 10.1038/ni884. [DOI] [PubMed] [Google Scholar]
- 59.Khattri R, Auger JA, Griffin MD, Sharpe AH, Bluestone JA. Lymphoproliferative disorder in CTLA-4 knockout mice is characterized by CD28-regulated activation of Th2 responses. J Immunol. 1999;162:5784–5791. [PubMed] [Google Scholar]
- 60.Rulifson IC, Sperling AI, Fields PE, Fitch FW, Bluestone JA. CD28 costimulation promotes the production of Th2 cytokines. J Immunol. 1997;158:658–665. [PubMed] [Google Scholar]
- 61.Krinzman SJ, et al. Inhibition of T cell costimulation abrogates airway hyperresponsiveness in a murine model. J Clin Invest. 1996;98:2693–2699. doi: 10.1172/JCI119093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Finck BK, Linsley PS, Wofsy D. Treatment of murine lupus with CTLA4Ig. Science. 1994;265:1225–1227. doi: 10.1126/science.7520604. [DOI] [PubMed] [Google Scholar]
- 63.Arreaza GA, et al. Neonatal activation of CD28 signaling overcomes T cell anergy and prevents autoimmune diabetes by an IL-4-dependent mechanism. J Clin Invest. 1997;100:2243–2253. doi: 10.1172/JCI119762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lenschow DJ, et al. CD28/B7 regulation of Th1 and Th2 subsets in the development of autoimmune diabetes. Immunity. 1996;5:285–293. doi: 10.1016/s1074-7613(00)80323-4. [DOI] [PubMed] [Google Scholar]
- 65.Bour-Jordan H, Blueston JA. CD28 function: a balance of costimulatory and regulatory signals. J Clin Immunol. 2002;22:1–7. doi: 10.1023/a:1014256417651. [DOI] [PubMed] [Google Scholar]
- 66.Ying H, et al. Cutting edge: CTLA-4--B7 interaction suppresses Th17 cell differentiation. J Immunol. 2010;185:1375–1378. doi: 10.4049/jimmunol.0903369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Bouguermouh S, Fortin G, Baba N, Rubio M, Sarfati M. CD28 co-stimulation down regulates Th17 development. PLoS ONE. 2009;4:e5087. doi: 10.1371/journal.pone.0005087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Purvis HA, et al. Low-strength T-cell activation promotes Th17 responses. Blood. 116:4829–4837. doi: 10.1182/blood-2010-03-272153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rudd CE, Taylor A, Schneider H. CD28 and CTLA-4 coreceptor expression and signal transduction. Immunol Rev. 2009;229:12–26. doi: 10.1111/j.1600-065X.2009.00770.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Pages F, et al. Binding of phosphatidylinositol-3-OH kinase to CD28 is required for T-cell signalling. Nature. 1994;369:327–329. doi: 10.1038/369327a0. [DOI] [PubMed] [Google Scholar]
- 71.Songyang Z, et al. SH2 domains recognize specific phosphopeptide sequences. Cell. 1993;72:767–778. doi: 10.1016/0092-8674(93)90404-e. [DOI] [PubMed] [Google Scholar]
- 72.Ellis JH, Ashman C, Burden MN, Kilpatrick KE, Morse MA, Hamblin PA. GRID: a novel Grb-2-related adapter protein that interacts with the activated T cell costimulatory receptor CD28. J Immunol. 2000;164:5805–5814. doi: 10.4049/jimmunol.164.11.5805. [DOI] [PubMed] [Google Scholar]
- 73.Holdorf AD, et al. Proline residues in CD28 and the Src homology (SH)3 domain of Lck are required for T cell costimulation. J Exp Med. 1999;190:375–384. doi: 10.1084/jem.190.3.375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.King PD, et al. Analysis of CD28 cytoplasmic tail tyrosine residues as regulators and substrates for the protein tyrosine kinases, EMT and LCK. J Immunol. 1997;158:580–590. [PubMed] [Google Scholar]
- 75.Marengere LE, et al. The SH3 domain of Itk/Emt binds to proline-rich sequences in the cytoplasmic domain of the T cell costimulatory receptor CD28. J Immunol. 1997;159:3220–3229. [PubMed] [Google Scholar]
- 76.Sasaki T, et al. Function of PI3Kgamma in thymocyte development, T cell activation, and neutrophil migration. Science. 2000;287:1040–1046. doi: 10.1126/science.287.5455.1040. [DOI] [PubMed] [Google Scholar]
- 77.Kane LP, Andres PG, Howland KC, Abbas AK, Weiss A. Akt provides the CD28 costimulatory signal for up-regulation of IL-2 and IFN-gamma but not TH2 cytokines. Nat Immunol. 2001;2:37–44. doi: 10.1038/83144. [DOI] [PubMed] [Google Scholar]
- 78.Yokosuka T, et al. Spatiotemporal regulation of T cell costimulation by TCR-CD28 microclusters and protein kinase C theta translocation. Immunity. 2008;29:589–601. doi: 10.1016/j.immuni.2008.08.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Bjorgo E, Tasken K. Novel mechanism of signaling by CD28. Immunol Lett. 2010;129:1–6. doi: 10.1016/j.imlet.2010.01.007. [DOI] [PubMed] [Google Scholar]
- 80.Bustelo XR. Regulatory and signaling properties of the Vav family. Mol Cell Biol. 2000;20:1461–1477. doi: 10.1128/mcb.20.5.1461-1477.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Rudd CE, Schneider H. Unifying concepts in CD28, ICOS and CTLA4 co-receptor signalling. Nat Rev Immunol. 2003;3:544–556. doi: 10.1038/nri1131. [DOI] [PubMed] [Google Scholar]
- 82.Takeda K, et al. CD28 stimulation triggers NF-kappaB activation through the CARMA1-PKCtheta-Grb2/Gads axis. Int Immunol. 2008;20:1507–1515. doi: 10.1093/intimm/dxn108. [DOI] [PubMed] [Google Scholar]
- 83.Marinari B, et al. Vav cooperates with CD28 to induce NF-kappaB activation via a pathway involving Rac-1 and mitogen-activated kinase kinase 1. Eur J Immunol. 2002;32:447–456. doi: 10.1002/1521-4141(200202)32:2<447::AID-IMMU447>3.0.CO;2-5. [DOI] [PubMed] [Google Scholar]
- 84.Su B, Jacinto E, Hibi M, Kallunki T, Karin M, Ben-Neriah Y. JNK is involved in signal integration during costimulation of T lymphocytes. Cell. 1994;77:727–736. doi: 10.1016/0092-8674(94)90056-6. [DOI] [PubMed] [Google Scholar]
- 85.Tavano R, et al. CD28 interaction with filamin-A controls lipid raft accumulation at the T-cell immunological synapse. Nat Cell Biol. 2006;8:1270–1276. doi: 10.1038/ncb1492. [DOI] [PubMed] [Google Scholar]
- 86.Freiberg BA, et al. Staging and resetting T cell activation in SMACs. Nat Immunol. 2002;3:911–917. doi: 10.1038/ni836. [DOI] [PubMed] [Google Scholar]
- 87.Dodson LF, et al. Targeted knock-in mice expressing mutations of CD28 reveal an essential pathway for costimulation. Mol Cell Biol. 2009;29:3710–3721. doi: 10.1128/MCB.01869-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Tai X, Cowan M, Feigenbaum L, Singer A. CD28 costimulation of developing thymocytes induces Foxp3 expression and regulatory T cell differentiation independently of interleukin 2. Nat Immunol. 2005;6:152–162. doi: 10.1038/ni1160. [DOI] [PubMed] [Google Scholar]
- 89.Miller J, et al. Two pathways of costimulation through CD28. Immunol Res. 2009 doi: 10.1007/s12026-009-8097-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Marinari B, Costanzo A, Marzano V, Piccolella E, Tuosto L. CD28 delivers a unique signal leading to the selective recruitment of RelA and p52 NF-kappaB subunits on IL-8 and Bcl-xL gene promoters. Proc Natl Acad Sci USA. 2004;101:6098–6103. doi: 10.1073/pnas.0308688101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Sanchez-Valdepenas C, Martin AG, Ramakrishnan P, Wallach D, Fresno M. NF-kappaB-inducing kinase is involved in the activation of the CD28 responsive element through phosphorylation of c-Rel and regulation of its transactivating activity. J Immunol. 2006;176:4666–4674. doi: 10.4049/jimmunol.176.8.4666. [DOI] [PubMed] [Google Scholar]
- 92.Pan M, Winslow MM, Chen L, Kuo A, Felsher D, Crabtree GR. Enhanced NFATc1 nuclear occupancy causes T cell activation independent of CD28 costimulation. J Immunol. 2007;178:4315–4321. doi: 10.4049/jimmunol.178.7.4315. [DOI] [PubMed] [Google Scholar]
- 93.Shapiro VS, Truitt KE, Imboden JB, Weiss A. CD28 mediates transcriptional upregulation of the interleukin-2 (IL-2) promoter through a composite element containing the CD28RE and NF-IL-2B AP-1 sites. Mol Cell Biol. 1997;17:4051–4058. doi: 10.1128/mcb.17.7.4051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Chen CY, et al. Nucleolin and YB-1 are required for JNK-mediated interleukin-2 mRNA stabilization during T-cell activation. Genes Dev. 2000;14:1236–1248. [PMC free article] [PubMed] [Google Scholar]
- 95.Diehn M, et al. Genomic expression programs and the integration of the CD28 costimulatory signal in T cell activation. Proc Natl Acad Sci USA. 2002;99:11796–11801. doi: 10.1073/pnas.092284399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Riley JL, et al. Modulation of TCR-induced transcriptional profiles by ligation of CD28, ICOS, and CTLA-4 receptors. Proc Natl Acad Sci USA. 2002;99:11790–11795. doi: 10.1073/pnas.162359999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Luhder F, et al. Topological requirements and signaling properties of T cell-activating, anti-CD28 antibody superagonists. J Exp Med. 2003;197:955–966. doi: 10.1084/jem.20021024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Tivol EA, Borriello F, Schweitzer AN, Lynch WP, Bluestone JA, Sharpe AH. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 1995;3:541–547. doi: 10.1016/1074-7613(95)90125-6. [DOI] [PubMed] [Google Scholar]
- 99.Walunas TL, Bakker CY, Bluestone JA. CTLA-4 ligation blocks CD28-dependent T cell activation. J Exp Med. 1996;183:2541–2550. doi: 10.1084/jem.183.6.2541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Walunas TL, et al. CTLA-4 can function as a negative regulator of T cell activation. Immunity. 1994;1:405–413. [PubMed] [Google Scholar]
- 101.Griffin MD, et al. Blockade of T cell activation using a surface-linked single-chain antibody to CTLA-4 (CD152). J Immunol. 2000;164:4433–4442. doi: 10.4049/jimmunol.164.9.4433. [DOI] [PubMed] [Google Scholar]
- 102.Fife BT, Griffin MD, Abbas AK, Locksley RM, Bluestone JA. Inhibition of T cell activation and autoimmune diabetes using a B cell surface-linked CTLA-4 agonist. J Clin Invest. 2006;116:2252–2261. doi: 10.1172/JCI27856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Griffin MD, et al. Development and applications of surface-linked single chain antibodies against T-cell antigens. J Immunol Methods. 2001;248:77–90. doi: 10.1016/s0022-1759(00)00344-6. [DOI] [PubMed] [Google Scholar]
- 104.Hwang KW, et al. Cutting edge: targeted ligation of CTLA-4 in vivo by membrane-bound anti-CTLA-4 antibody prevents rejection of allogeneic cells. J Immunol. 2002;169:633–637. doi: 10.4049/jimmunol.169.2.633. [DOI] [PubMed] [Google Scholar]
- 105.Eagar TN, Karandikar NJ, Bluestone JA, Miller SD. The role of CTLA-4 in induction and maintenance of peripheral T cell tolerance. Eur J Immunol. 2002;32:972–981. doi: 10.1002/1521-4141(200204)32:4<972::AID-IMMU972>3.0.CO;2-M. [DOI] [PubMed] [Google Scholar]
- 106.Perez VL, Van Parijs L, Biuckians A, Zheng XX, Strom TB, Abbas AK. Induction of peripheral T cell tolerance in vivo requires CTLA-4 engagement. Immunity. 1997;6:411–417. doi: 10.1016/s1074-7613(00)80284-8. [DOI] [PubMed] [Google Scholar]
- 107.Fife BT, et al. Insulin-induced remission in new-onset NOD mice is maintained by the PD-1-PD-L1 pathway. J Exp Med. 2006;203:2737–2747. doi: 10.1084/jem.20061577. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Egen JG, Allison JP. Cytotoxic T lymphocyte antigen-4 accumulation in the immunological synapse is regulated by TCR signal strength. Immunity. 2002;16:23–35. doi: 10.1016/s1074-7613(01)00259-x. [DOI] [PubMed] [Google Scholar]
- 109.Gozalo-Sanmillan S, McNally JM, Lin MY, Chambers CA, Berg LJ. Cutting edge: two distinct mechanisms lead to impaired T cell homeostasis in Janus kinase 3- and CTLA-4-deficient mice. J Immunol. 2001;166:727–730. doi: 10.4049/jimmunol.166.2.727. [DOI] [PubMed] [Google Scholar]
- 110.Tivol EA, Gorski J. Re-establishing peripheral tolerance in the absence of CTLA-4: complementation by wild-type T cells points to an indirect role for CTLA-4. J Immunol. 2002;169:1852–1858. doi: 10.4049/jimmunol.169.4.1852. [DOI] [PubMed] [Google Scholar]
- 111.Ise W, et al. CTLA-4 suppresses the pathogenicity of self antigen-specific T cells by cell-intrinsic and cell-extrinsic mechanisms. Nat Immunol. 2010;11:129–135. doi: 10.1038/ni.1835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harper K, Balzano C, Rouvier E, Mattei MG, Luciani MF, Golstein P. CTLA-4 and CD28 activated lymphocyte molecules are closely related in both mouse and human as to sequence, message expression, gene structure, and chromosomal location. J Immunol. 1991;147:1037–1044. [PubMed] [Google Scholar]
- 113.Baroja ML, et al. Inhibition of CTLA-4 function by the regulatory subunit of serine/threonine phosphatase 2A. J Immunol. 2002;168:5070–5078. doi: 10.4049/jimmunol.168.10.5070. [DOI] [PubMed] [Google Scholar]
- 114.Balzano C, Buonavista N, Rouvier E, Golstein P. CTLA-4 and CD28: similar proteins, neighbouring genes. Int J Cancer. 1992;7(Suppl):28–32. [PubMed] [Google Scholar]
- 115.Peach RJ, et al. Complementarity determining region 1 (CDR1)- and CDR3-analogous regions in CTLA-4 and CD28 determine the binding to B7-1. J Exp Med. 1994;180:2049–2058. doi: 10.1084/jem.180.6.2049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Pentcheva-Hoang T, Egen JG, Wojnoonski K, Allison JP. B7-1 and B7-2 selectively recruit CTLA-4 and CD28 to the immunological synapse. Immunity. 2004;21:401–413. doi: 10.1016/j.immuni.2004.06.017. [DOI] [PubMed] [Google Scholar]
- 117.Collins AV, et al. The interaction properties of costimulatory molecules revisited. Immunity. 2002;17:201–210. doi: 10.1016/s1074-7613(02)00362-x. [DOI] [PubMed] [Google Scholar]
- 118.Morton PA, et al. Differential effects of CTLA-4 substitutions on the binding of human CD80 (B7-1) and CD86 (B7-2). J Immunol. 1996;156:1047–1054. [PubMed] [Google Scholar]
- 119.Yokosuka T, et al. Spatiotemporal basis of CTLA-4 costimulatory molecule-mediated negative regulation of T cell activation. Immunity. 2010;33:326–339. doi: 10.1016/j.immuni.2010.09.006. [DOI] [PubMed] [Google Scholar]
- 120.Schwartz JC, Zhang X, Fedorov AA, Nathenson SG, Almo SC. Structural basis for co-stimulation by the human CTLA-4/B7-2 complex. Nature. 2001;410:604–608. doi: 10.1038/35069112. [DOI] [PubMed] [Google Scholar]
- 121.Stamper CC, et al. Crystal structure of the B7-1/CTLA-4 complex that inhibits human immune responses. Nature. 2001;410:608–611. doi: 10.1038/35069118. [DOI] [PubMed] [Google Scholar]
- 122.Zhang X, Schwartz JC, Almo SC, Nathenson SG. Crystal structure of the receptor-binding domain of human B7-2: insights into organization and signaling. Proc Natl Acad Sci USA. 2003;100:2586–2591. doi: 10.1073/pnas.252771499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Chikuma S, Bluestone JA. CTLA-4 and tolerance: the biochemical point of view. Immunol Res. 2003;28:241–253. doi: 10.1385/IR:28:3:241. [DOI] [PubMed] [Google Scholar]
- 124.Chikuma S, Imboden JB, Bluestone JA. Negative regulation of T cell receptor-lipid raft interaction by cytotoxic T lymphocyte-associated antigen 4. J Exp Med. 2003;197:129–135. doi: 10.1084/jem.20021646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Chikuma S, Abbas AK, Bluestone JA. B7-independent inhibition of T cells by CTLA-4. J Immunol. 2005;175:177–181. doi: 10.4049/jimmunol.175.1.177. [DOI] [PubMed] [Google Scholar]
- 126.Valk E, Rudd CE, Schneider H. CTLA-4 trafficking and surface expression. Trends Immunol. 2008;29:272–279. doi: 10.1016/j.it.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Chuang E, Alegre ML, Duckett CS, Noel PJ, Vander Heiden MG, Thompson CB. Interaction of CTLA-4 with the clathrin-associated protein AP50 results in ligand-independent endocytosis that limits cell surface expression. J Immunol. 1997;159:144–151. [PubMed] [Google Scholar]
- 128.Zhang Y, Allison JP. Interaction of CTLA-4 with AP50, a clathrin-coated pit adaptor protein. Proc Natl Acad Sci USA. 1997;94:9273–9278. doi: 10.1073/pnas.94.17.9273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Chuang E, et al. The CD28 and CTLA-4 receptors associate with the serine/threonine phosphatase PP2A. Immunity. 2000;13:313–322. doi: 10.1016/s1074-7613(00)00031-5. [DOI] [PubMed] [Google Scholar]
- 130.Linsley PS, Bradshaw J, Greene J, Peach R, Bennett KL, Mittler RS. Intracellular trafficking of CTLA-4 and focal localization towards sites of TCR engagement. Immunity. 1996;4:535–543. doi: 10.1016/s1074-7613(00)80480-x. [DOI] [PubMed] [Google Scholar]
- 131.Schneider H, Prasad KV, Shoelson SE, Rudd CE. CTLA-4 binding to the lipid kinase phosphatidylinositol 3-kinase in T cells. J Exp Med. 1995;181:351–355. doi: 10.1084/jem.181.1.351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Schneider H, Rudd CE. Tyrosine phosphatase SHP-2 binding to CTLA-4: absence of direct YVKM/YFIP motif recognition. Biochem Biophys Res Commun. 2000;269:279–283. doi: 10.1006/bbrc.2000.2234. [DOI] [PubMed] [Google Scholar]
- 133.Schneider H, Valk E, Leung R, Rudd CE. CTLA-4 activation of phosphatidylinositol 3-kinase (PI 3-K) and protein kinase B (PKB/AKT) sustains T-cell anergy without cell death. PLoS One. 2008;3:e3842. doi: 10.1371/journal.pone.0003842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Deane JA, Fruman DA. Phosphoinositide 3-kinase: diverse roles in immune cell activation. Annu Rev Immunol. 2004;22:563–598. doi: 10.1146/annurev.immunol.22.012703.104721. [DOI] [PubMed] [Google Scholar]
- 135.Teft WA, Kirchhof MG, Madrenas J. A molecular perspective of CTLA-4 function. Annu Rev Immunol. 2006;24:65–97. doi: 10.1146/annurev.immunol.24.021605.090535. [DOI] [PubMed] [Google Scholar]
- 136.Guntermann C, Alexander DR. CTLA-4 suppresses proximal TCR signaling in resting human CD4(+) T cells by inhibiting ZAP-70 Tyr(319) phosphorylation: a potential role for tyrosine phosphatases. J Immunol. 2002;168:4420–4429. doi: 10.4049/jimmunol.168.9.4420. [DOI] [PubMed] [Google Scholar]
- 137.Lee KM, et al. Molecular basis of T cell inactivation by CTLA-4. Science. 1998;282:2263–2266. doi: 10.1126/science.282.5397.2263. [DOI] [PubMed] [Google Scholar]
- 138.Calvo CR, Amsen D, Kruisbeek AM. Cytotoxic T lymphocyte antigen 4 (CTLA-4) interferes with extracellular signal-regulated kinase (ERK) and Jun NH2-terminal kinase (JNK) activation, but does not affect phosphorylation of T cell receptor zeta and ZAP70. J Exp Med. 1997;186:1645–1653. doi: 10.1084/jem.186.10.1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Masteller EL, Chuang E, Mullen AC, Reiner SL, Thompson CB. Structural analysis of CTLA-4 function in vivo. J Immunol. 2000;164:5319–5327. doi: 10.4049/jimmunol.164.10.5319. [DOI] [PubMed] [Google Scholar]
- 140.Yi LA, Hajialiasgar S, Chuang E. Tyrosine-mediated inhibitory signals contribute to CTLA-4 function in vivo. Int Immunol. 2004;16:539–547. doi: 10.1093/intimm/dxh055. [DOI] [PubMed] [Google Scholar]
- 141.Shiratori T, et al. Tyrosine phosphorylation controls internalization of CTLA-4 by regulating its interaction with clathrin-associated adaptor complex AP-2. Immunity. 1997;6:583–589. doi: 10.1016/s1074-7613(00)80346-5. [DOI] [PubMed] [Google Scholar]
- 142.Scalapino KJ, Daikh DI. CTLA-4: a key regulatory point in the control of autoimmune disease. Immunol Rev. 2008;223:143–155. doi: 10.1111/j.1600-065X.2008.00639.x. [DOI] [PubMed] [Google Scholar]
- 143.Oaks MK, Hallett KM. Cutting edge: a soluble form of CTLA-4 in patients with autoimmune thyroid disease. J Immunol. 2000;164:5015–5018. doi: 10.4049/jimmunol.164.10.5015. [DOI] [PubMed] [Google Scholar]
- 144.Ueda H, et al. Association of the T-cell regulatory gene CTLA4 with susceptibility to autoimmune disease. Nature. 2003;423:506–511. doi: 10.1038/nature01621. [DOI] [PubMed] [Google Scholar]
- 145.Vijayakrishnan L, et al. An autoimmune disease-associated CTLA-4 splice variant lacking the B7 binding domain signals negatively in T cells. Immunity. 2004;20:563–575. doi: 10.1016/s1074-7613(04)00110-4. [DOI] [PubMed] [Google Scholar]
- 146.Liu MF, Wang CR, Chen PC, Fung LL. Increased expression of soluble cytotoxic T-lymphocyte-associated antigen-4 molecule in patients with systemic lupus erythematosus. Scand J Immunol. 2003;57:568–572. doi: 10.1046/j.1365-3083.2003.01232.x. [DOI] [PubMed] [Google Scholar]
- 147.Gough SC, Walker LS, Sansom DM. CTLA4 gene polymorphism and autoimmunity. Immunol Rev. 2005;204:102–115. doi: 10.1111/j.0105-2896.2005.00249.x. [DOI] [PubMed] [Google Scholar]
- 148.Holmberg D, Cilio CM, Lundholm M, Motta V. CTLA-4 (CD152) and its involvement in autoimmune disease. Autoimmunity. 2005;38:225–233. doi: 10.1080/08916930500050210. [DOI] [PubMed] [Google Scholar]
- 149.Araki M, et al. Genetic evidence that the differential expression of the ligand-independent isoform of CTLA-4 is the molecular basis of the Idd5.1 type 1 diabetes region in nonobese diabetic mice. J Immunol. 2009;183:5146–5157. doi: 10.4049/jimmunol.0802610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Lindsten T, et al. Characterization of CTLA-4 structure and expression on human T cells. J Immunol. 1993;151:3489–3499. [PubMed] [Google Scholar]
- 151.Perkins D, et al. Regulation of CTLA-4 expression during T cell activation. J Immunol. 1996;156:4154–4159. [PubMed] [Google Scholar]
- 152.Salomon B, et al. B7/CD28 costimulation is essential for the homeostasis of the CD4+CD25+ immunoregulatory T cells that control autoimmune diabetes. Immunity. 2000;12:431–440. doi: 10.1016/s1074-7613(00)80195-8. [DOI] [PubMed] [Google Scholar]
- 153.Mandelbrot DA, McAdam AJ, Sharpe AH. B7-1 or B7-2 is required to produce the lymphoproliferative phenotype in mice lacking cytotoxic T lymphocyte-associated antigen 4 (CTLA-4). J Exp Med. 1999;189:435–440. doi: 10.1084/jem.189.2.435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Luhder F, Chambers C, Allison JP, Benoist C, Mathis D. Pinpointing when T cell costimulatory receptor CTLA-4 must be engaged to dampen diabetogenic T cells. Proc Natl Acad Sci USA. 2000;97:12204–12209. doi: 10.1073/pnas.200348397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Francisco LM, Sage PT, Sharpe AH. The PD-1 pathway in tolerance and autoimmunity. Immunol Rev. 2010;236:219–242. doi: 10.1111/j.1600-065X.2010.00923.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Ishida M, et al. Differential expression of PD-L1 and PD-L2, ligands for an inhibitory receptor PD-1, in the cells of lymphohematopoietic tissues. Immunol Lett. 2002;84:57–62. doi: 10.1016/s0165-2478(02)00142-6. [DOI] [PubMed] [Google Scholar]
- 157.Latchman Y, et al. PD-L2 is a second ligand for PD-1 and inhibits T cell activation. Nat Immunol. 2001;2:261–268. doi: 10.1038/85330. [DOI] [PubMed] [Google Scholar]
- 158.Nishimura H, Nose M, Hiai H, Minato N, Honjo T. Development of lupus-like autoimmune diseases by disruption of the PD-1 gene encoding an ITIM motif-carrying immunoreceptor. Immunity. 1999;11:141–151. doi: 10.1016/s1074-7613(00)80089-8. [DOI] [PubMed] [Google Scholar]
- 159.Nishimura H, et al. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science. 2001;291:319–322. doi: 10.1126/science.291.5502.319. [DOI] [PubMed] [Google Scholar]
- 160.Wang J, Yoshida T, Nakaki F, Hiai H, Okazaki T, Honjo T. Establishment of NODPdcd1-/- mice as an efficient animal model of type I diabetes. Proc Natl Acad Sci USA. 2005;102:11823–11828. doi: 10.1073/pnas.0505497102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 161.Kroner A, et al. A PD-1 polymorphism is associated with disease progression in multiple sclerosis. Ann Neurol. 2005;58:50–57. doi: 10.1002/ana.20514. [DOI] [PubMed] [Google Scholar]
- 162.Nielsen C, Hansen D, Husby S, Jacobsen BB, Lillevang ST. Association of a putative regulatory polymorphism in the PD-1 gene with susceptibility to type 1 diabetes. Tissue Antigens. 2003;62:492–497. doi: 10.1046/j.1399-0039.2003.00136.x. [DOI] [PubMed] [Google Scholar]
- 163.Prokunina L, et al. A regulatory polymorphism in PDCD1 is associated with susceptibility to systemic lupus erythematosus in humans. Nat Genet. 2002;32:666–669. doi: 10.1038/ng1020. [DOI] [PubMed] [Google Scholar]
- 164.Liang SC, et al. Regulation of PD-1, PD-L1, and PD-L2 expression during normal and autoimmune responses. Eur J Immunol. 2003;33:2706–2716. doi: 10.1002/eji.200324228. [DOI] [PubMed] [Google Scholar]
- 165.Nishimura H, et al. Developmentally regulated expression of the PD-1 protein on the surface of double-negative (CD4-CD8-) thymocytes. Int Immunol. 1996;8:773–780. doi: 10.1093/intimm/8.5.773. [DOI] [PubMed] [Google Scholar]
- 166.Keir ME, et al. Tissue expression of PD-L1 mediates peripheral T cell tolerance. J Exp Med. 2006;203:883–895. doi: 10.1084/jem.20051776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Salama AD, et al. Critical role of the programmed death-1 (PD-1) pathway in regulation of experimental autoimmune encephalomyelitis. J Exp Med. 2003;198:71–78. doi: 10.1084/jem.20022119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Bour-Jordan H, Salomon BL, Thompson HL, Szot GL, Bernhard MR, Bluestone JA. Costimulation controls diabetes by altering the balance of pathogenic and regulatory T cells. J Clin Invest. 2004;114:979–987. doi: 10.1172/JCI20483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Salomon B, et al. Development of spontaneous autoimmune peripheral polyneuropathy in B7-2- deficient NOD mice. J Exp Med. 2001;194:677–684. doi: 10.1084/jem.194.5.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Habicht A, et al. Striking dichotomy of PD-L1 and PD-L2 pathways in regulating alloreactive CD4(+) and CD8(+) T cells in vivo. Am J Transplant. 2007;7:2683–2692. doi: 10.1111/j.1600-6143.2007.01999.x. [DOI] [PubMed] [Google Scholar]
- 171.Francisco LM, et al. PD-L1 regulates the development, maintenance, and function of induced regulatory T cells. J Exp Med. 2009;206:3015–3029. doi: 10.1084/jem.20090847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Franceschini D, et al. PD-L1 negatively regulates CD4+CD25+Foxp3+ Tregs by limiting STAT-5 phosphorylation in patients chronically infected with HCV. J Clin Invest. 2009;119:551–564. doi: 10.1172/JCI36604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Fife BT, et al. Interactions between PD-1 and PD-L1 promote tolerance by blocking the TCR-induced stop signal. Nat Immunol. 2009;10:1185–1192. doi: 10.1038/ni.1790. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Tang Q, et al. Visualizing regulatory T cell control of autoimmune responses in nonobese diabetic mice. Nat Immunol. 2006;7:83–92. doi: 10.1038/ni1289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Sansom DM, Walker LS. The role of CD28 and cytotoxic T-lymphocyte antigen-4 (CTLA-4) in regulatory T-cell biology. Immunol Rev. 2006;212:131–148. doi: 10.1111/j.0105-2896.2006.00419.x. [DOI] [PubMed] [Google Scholar]
- 176.Tang Q, et al. Cutting edge: CD28 controls peripheral homeostasis of CD4+CD25+ regulatory T cells. J Immunol. 2003;171:3348. doi: 10.4049/jimmunol.171.7.3348. [DOI] [PubMed] [Google Scholar]
- 177.Tang Q, et al. In vitro-expanded antigen-specific regulatory T cells suppress autoimmune diabetes. J Exp Med. 2004;199:1455–1465. doi: 10.1084/jem.20040139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Nazarov-Stoica C, Surls J, Bona C, Casares S, Brumeanu TD. CD28 signaling in T regulatory precursors requires p56lck and rafts integrity to stabilize the Foxp3 message. J Immunol. 2009;182:102–110. doi: 10.4049/jimmunol.182.1.102. [DOI] [PubMed] [Google Scholar]
- 179.Takahashi T, et al. Immunologic self-tolerance maintained by CD25+CD4+ naturally anergic and suppressive T cells: induction of autoimmune disease by breaking their anergic/suppressive state. Int Immunol. 1998;10:1969–1980. doi: 10.1093/intimm/10.12.1969. [DOI] [PubMed] [Google Scholar]
- 180.Thornton AM, Shevach EM. CD4+CD25+ immunoregulatory T cells suppress polyclonal T cell activation in vitro by inhibiting interleukin 2 production. J Exp Med. 1998;188:287–296. doi: 10.1084/jem.188.2.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fisson S, et al. Continuous activation of autoreactive CD4+ CD25+ regulatory T cells in the steady state. J Exp Med. 2003;198:737–746. doi: 10.1084/jem.20030686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Walker LS, Chodos A, Eggena M, Dooms H, Abbas AK. Antigen-dependent proliferation of CD4+ CD25+ regulatory T cells in vivo. J Exp Med. 2003;198:249–258. doi: 10.1084/jem.20030315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Hsieh CS, Rudensky AY. The role of TCR specificity in naturally arising CD25+ CD4+ regulatory T cell biology. Curr Top Microbiol Immunol. 2005;293:25–42. doi: 10.1007/3-540-27702-1_2. [DOI] [PubMed] [Google Scholar]
- 184.Sakaguchi S. Naturally arising Foxp3-expressing CD25+CD4+ regulatory T cells in immunological tolerance to self and non-self. Nat Immunol. 2005;6:345–352. doi: 10.1038/ni1178. [DOI] [PubMed] [Google Scholar]
- 185.Samy ET, Parker LA, Sharp CP, Tung KS. Continuous control of autoimmune disease by antigen-dependent polyclonal CD4+CD25+ regulatory T cells in the regional lymph node. J Exp Med. 2005;202:771–781. doi: 10.1084/jem.20041033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Brusko TM, Putnam AL, Bluestone JA. Human regulatory T cells: role in autoimmune disease and therapeutic opportunities. Immunol Rev. 2008;223:371–390. doi: 10.1111/j.1600-065X.2008.00637.x. [DOI] [PubMed] [Google Scholar]
- 187.D'Cruz LM, Klein L. Development and function of agonist-induced CD25+Foxp3+ regulatory T cells in the absence of interleukin 2 signaling. Nat Immunol. 2005;6:1152–1159. doi: 10.1038/ni1264. [DOI] [PubMed] [Google Scholar]
- 188.Malek TR, Yu A, Vincek V, Scibelli P, Kong L. CD4 regulatory T cells prevent lethal autoimmunity in IL-2Rbeta-deficient mice. Implications for the nonredundant function of IL-2. Immunity. 2002;17:167–178. doi: 10.1016/s1074-7613(02)00367-9. [DOI] [PubMed] [Google Scholar]
- 189.Setoguchi R, Hori S, Takahashi T, Sakaguchi S. Homeostatic maintenance of natural Foxp3(+) CD25(+) CD4(+) regulatory T cells by interleukin (IL)-2 and induction of autoimmune disease by IL-2 neutralization. J Exp Med. 2005;201:723–735. doi: 10.1084/jem.20041982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 190.Fontenot JD, Rasmussen JP, Gavin MA, Rudensky AY. A function for interleukin 2 in Foxp3-expressing regulatory T cells. Nat Immunol. 2005;6:1142–1151. doi: 10.1038/ni1263. [DOI] [PubMed] [Google Scholar]
- 191.Hombach AA, Kofler D, Hombach A, Rappl G, Abken H. Effective proliferation of human regulatory T cells requires a strong costimulatory CD28 signal that cannot be substituted by IL-2. J Immunol. 2007;179:7924–7931. doi: 10.4049/jimmunol.179.11.7924. [DOI] [PubMed] [Google Scholar]
- 192.Anderson MS, Bluestone JA. The NOD Mouse: A Model of Immune Dysregulation. Annu Rev Immunol. 2005;23:447–485. doi: 10.1146/annurev.immunol.23.021704.115643. [DOI] [PubMed] [Google Scholar]
- 193.Kundig TM, et al. Duration of TCR stimulation determines costimulatory requirement of T cells. Immunity. 1996;5:41–52. doi: 10.1016/s1074-7613(00)80308-8. [DOI] [PubMed] [Google Scholar]
- 194.Lohr J, Knoechel B, Jiang S, Sharpe AH, Abbas AK. The inhibitory function of B7 costimulators in T cell responses to foreign and self-antigens. Nat Immunol. 2003;4:664–669. doi: 10.1038/ni939. [DOI] [PubMed] [Google Scholar]
- 195.Lohr J, Knoechel B, Kahn EC, Abbas AK. Role of B7 in T cell tolerance. J Immunol. 2004;173:5028–5035. doi: 10.4049/jimmunol.173.8.5028. [DOI] [PubMed] [Google Scholar]
- 196.de Jong YP, et al. Blocking inducible co-stimulator in the absence of CD28 impairs Th1 and CD25+ regulatory T cells in murine colitis. Int Immunol. 2004;16:205–213. doi: 10.1093/intimm/dxh019. [DOI] [PubMed] [Google Scholar]
- 197.Yang J, et al. Paradoxical functions of B7: CD28 costimulation in a MHC class II-mismatched cardiac transplant model. Am J Transplant. 2009;9:2837–2844. doi: 10.1111/j.1600-6143.2009.02839.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Takahashi T, et al. Immunologic self-tolerance maintained by CD25(+)CD4(+) regulatory T cells constitutively expressing cytotoxic T lymphocyte-associated antigen 4. J Exp Med. 2000;192:303–310. doi: 10.1084/jem.192.2.303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199.Deng G, Podack ER. Suppression of apoptosis in a cytotoxic T-cell line by interleukin 2-mediated gene transcription and deregulated expression of the protooncogene bcl-2. Proc Natl Acad Sci USA. 1993;90:2189–2193. doi: 10.1073/pnas.90.6.2189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Dooms H, Kahn E, Knoechel B, Abbas AK. IL-2 induces a competitive survival advantage in T lymphocytes. J Immunol. 2004;172:5973–5979. doi: 10.4049/jimmunol.172.10.5973. [DOI] [PubMed] [Google Scholar]
- 201.Kim HP, Kelly J, Leonard WJ. The basis for IL-2-induced IL-2 receptor alpha chain gene regulation: importance of two widely separated IL-2 response elements. Immunity. 2001;15:159–172. doi: 10.1016/s1074-7613(01)00167-4. [DOI] [PubMed] [Google Scholar]
- 202.Sadlack B, Merz H, Schorle H, Schimpl A, Feller AC, Horak I. Ulcerative colitis-like disease in mice with a disrupted interleukin-2 gene. Cell. 1993;75:253–261. doi: 10.1016/0092-8674(93)80067-o. [DOI] [PubMed] [Google Scholar]
- 203.Suzuki H, et al. Deregulated T cell activation and autoimmunity in mice lacking interleukin-2 receptor beta. Science. 1995;268:1472–1476. doi: 10.1126/science.7770771. [DOI] [PubMed] [Google Scholar]
- 204.Willerford DM, Chen J, Ferry JA, Davidson L, Ma A, Alt FW. Interleukin-2 receptor alpha chain regulates the size and content of the peripheral lymphoid compartment. Immunity. 1995;3:521–530. doi: 10.1016/1074-7613(95)90180-9. [DOI] [PubMed] [Google Scholar]
- 205.Sharfe N, Dadi HK, Shahar M, Roifman CM. Human immune disorder arising from mutation of the alpha chain of the interleukin-2 receptor. Proc Natl Acad Sci USA. 1997;94:3168–3171. doi: 10.1073/pnas.94.7.3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Refaeli Y, Van Parijs L, London CA, Tschopp J, Abbas AK. Biochemical mechanisms of IL-2-regulated Fas-mediated T cell apoptosis. Immunity. 1998;8:615–623. doi: 10.1016/s1074-7613(00)80566-x. [DOI] [PubMed] [Google Scholar]
- 207.Kramer S, Schimpl A, Hunig T. Immunopathology of interleukin (IL) 2-deficient mice: thymus dependence and suppression by thymus-dependent cells with an intact IL-2 gene. J Exp Med. 1995;182:1769–1776. doi: 10.1084/jem.182.6.1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 208.Suzuki H, Zhou YW, Kato M, Mak TW, Nakashima I. Normal regulatory alpha/beta T cells effectively eliminate abnormally activated T cells lacking the interleukin 2 receptor beta in vivo. J Exp Med. 1999;190:1561–1572. doi: 10.1084/jem.190.11.1561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Ono M, et al. Foxp3 controls regulatory T-cell function by interacting with AML1/Runx1. Nature. 2007;446:685–689. doi: 10.1038/nature05673. [DOI] [PubMed] [Google Scholar]
- 210.Boyman O, Kovar M, Rubinstein MP, Surh CD, Sprent J. Selective stimulation of T cell subsets with antibody-cytokine immune complexes. Science. 2006;311:1924–1927. doi: 10.1126/science.1122927. [DOI] [PubMed] [Google Scholar]
- 211.Webster KE, et al. In vivo expansion of T reg cells with IL-2-mAb complexes: induction of resistance to EAE and long-term acceptance of islet allografts without immunosuppression. J Exp Med. 2009;206:751–760. doi: 10.1084/jem.20082824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.Barron L, et al. Cutting edge: mechanisms of IL-2-dependent maintenance of functional regulatory T cells. J Immunol. 2010;185:6426–6430. doi: 10.4049/jimmunol.0903940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.O'Gorman WE, et al. The initial phase of an immune response functions to activate regulatory T cells. J Immunol. 2009;183:332–339. doi: 10.4049/jimmunol.0900691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Davidson TS, DiPaolo RJ, Andersson J, Shevach EM. Cutting Edge: IL-2 is essential for TGF-beta-mediated induction of Foxp3+ T regulatory cells. J Immunol. 2007;178:4022–4026. doi: 10.4049/jimmunol.178.7.4022. [DOI] [PubMed] [Google Scholar]
- 215.Zheng SG, Wang J, Wang P, Gray JD, Horwitz DA. IL-2 is essential for TGF-beta to convert naive CD4+CD25- cells to CD25+Foxp3+ regulatory T cells and for expansion of these cells. J Immunol. 2007;178:2018–2027. doi: 10.4049/jimmunol.178.4.2018. [DOI] [PubMed] [Google Scholar]
- 216.Thornton AM, et al. Expression of Helios, an Ikaros transcription factor family member, differentiates thymic-derived from peripherally induced Foxp3+ T regulatory cells. J Immunol. 2010;184:3433–3441. doi: 10.4049/jimmunol.0904028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Todd JA, et al. Robust associations of four new chromosome regions from genome-wide analyses of type 1 diabetes. Nat Genet. 2007;39:857–864. doi: 10.1038/ng2068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Vella A, et al. Localization of a type 1 diabetes locus in the IL2RA/CD25 region by use of tag single-nucleotide polymorphisms. Am J Hum Genet. 2005;76:773–779. doi: 10.1086/429843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Bottini N, et al. A functional variant of lymphoid tyrosine phosphatase is associated with type I diabetes. Nat Genet. 2004;36:337–338. doi: 10.1038/ng1323. [DOI] [PubMed] [Google Scholar]
- 220.Wicker LS, Todd JA, Prins JB, Podolin PL, Renjilian RJ, Peterson LB. Resistance alleles at two non-major histocompatibility complex-linked insulin-dependent diabetes loci on chromosome 3, Idd3 and Idd10, protect nonobese diabetic mice from diabetes. J Exp Med. 1994;180:1705–1713. doi: 10.1084/jem.180.5.1705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 221.Lyons PA, et al. Congenic mapping of the type 1 diabetes locus, Idd3, to a 780-kb region of mouse chromosome 3: identification of a candidate segment of ancestral DNA by haplotype mapping. Genome Res. 2000;10:446–453. doi: 10.1101/gr.10.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Yamanouchi J, et al. Interleukin-2 gene variation impairs regulatory T cell function and causes autoimmunity. Nat Genet. 2007;39:329–337. doi: 10.1038/ng1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Tang Q, et al. Central role of defective interleukin-2 production in the triggering of islet autoimmune destruction. Immunity. 2008;28:687. doi: 10.1016/j.immuni.2008.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Grinberg-Bleyer Y, et al. IL-2 reverses established type 1 diabetes in NOD mice by a local effect on pancreatic regulatory T cells. J Exp Med. 2010;207:1871. doi: 10.1084/jem.20100209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 225.Zhou X, et al. Instability of the transcription factor Foxp3 leads to the generation of pathogenic memory T cells in vivo. Nat Immunol. 2009;10:1000–1007. doi: 10.1038/ni.1774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Lazarski CA, Hughson A, Sojka DK, Fowell DJ. Regulating Treg cells at sites of inflammation. Immunity. 2008;29:511. doi: 10.1016/j.immuni.2008.09.012. author reply 512. [DOI] [PubMed] [Google Scholar]
- 227.Bachmann MF, Kohler G, Ecabert B, Mak TW, Kopf M. Cutting edge: lymphoproliferative disease in the absence of CTLA-4 is not T cell autonomous. J Immunol. 1999;163:1128–1131. [PubMed] [Google Scholar]
- 228.Friedline RH, et al. CD4+ regulatory T cells require CTLA-4 for the maintenance of systemic tolerance. J Exp Med. 2009;206:421–434. doi: 10.1084/jem.20081811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 229.Chai JG, Tsang JY, Lechler R, Simpson E, Dyson J, Scott D. CD4+CD25+ T cells as immunoregulatory T cells in vitro. Eur J Immunol. 2002;32:2365–2375. doi: 10.1002/1521-4141(200208)32:8<2365::AID-IMMU2365>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 230.Jonuleit H, Schmitt E, Stassen M, Tuettenberg A, Knop J, Enk AH. Identification and functional characterization of human CD4(+)CD25(+) T cells with regulatory properties isolated from peripheral blood. J Exp Med. 2001;193:1285–1294. doi: 10.1084/jem.193.11.1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 231.Birebent B, et al. Suppressive properties of human CD4+CD25+ regulatory T cells are dependent on CTLA-4 expression. Eur J Immunol. 2004;34:3485–3496. doi: 10.1002/eji.200324632. [DOI] [PubMed] [Google Scholar]
- 232.Tang Q, Boden EK, Henriksen KJ, Bour-Jordan H, Bi M, Bluestone JA. Distinct roles of CTLA-4 and TGF-beta in CD4+CD25+ regulatory T cell function. Eur J Immunol. 2004;34:2996–3005. doi: 10.1002/eji.200425143. [DOI] [PubMed] [Google Scholar]
- 233.Tivol EA, et al. CTLA4Ig prevents lymphoproliferation and fatal multiorgan tissue destruction in CTLA-4-deficient mice. J Immunol. 1997;158:5091–5094. [PubMed] [Google Scholar]
- 234.Read S, et al. Blockade of CTLA-4 on CD4+CD25+ regulatory T cells abrogates their function in vivo. J Immunol. 2006;177:4376–4383. doi: 10.4049/jimmunol.177.7.4376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 235.Peggs KS, Quezada SA, Chambers CA, Korman AJ, Allison JP. Blockade of CTLA-4 on both effector and regulatory T cell compartments contributes to the antitumor activity of anti-CTLA-4 antibodies. J Exp Med. 2009;206:1717–1725. doi: 10.1084/jem.20082492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 236.Schmidt EM, et al. Ctla-4 controls regulatory T cell peripheral homeostasis and is required for suppression of pancreatic islet autoimmunity. J Immunol. 2009;182:274–282. doi: 10.4049/jimmunol.182.1.274. [DOI] [PubMed] [Google Scholar]
- 237.Jain N, Nguyen H, Chambers C, Kang J. Dual function of CTLA-4 in regulatory T cells and conventional T cells to prevent multiorgan autoimmunity. Proc Natl Acad Sci USA. 2010;107:1524–1528. doi: 10.1073/pnas.0910341107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 238.Wing K, et al. CTLA-4 control over Foxp3+ regulatory T cell function. Science. 2008;322:271–275. doi: 10.1126/science.1160062. [DOI] [PubMed] [Google Scholar]
- 239.Kataoka H, et al. CD25(+)CD4(+) regulatory T cells exert in vitro suppressive activity independent of CTLA-4. Int Immunol. 2005;17:421–427. doi: 10.1093/intimm/dxh221. [DOI] [PubMed] [Google Scholar]
- 240.Crellin NK, Garcia RV, Levings MK. Altered activation of AKT is required for the suppressive function of human CD4+CD25+ T regulatory cells. Blood. 2007;109:2014–2022. doi: 10.1182/blood-2006-07-035279. [DOI] [PubMed] [Google Scholar]
- 241.Hickman SP, Yang J, Thomas RM, Wells AD, Turka LA. Defective activation of protein kinase C and Ras-ERK pathways limits IL-2 production and proliferation by CD4+CD25+ regulatory T cells. J Immunol. 2006;177:2186–2194. doi: 10.4049/jimmunol.177.4.2186. [DOI] [PubMed] [Google Scholar]
- 242.Fehervari Z, Sakaguchi S. Control of Foxp3+ CD25+CD4+ regulatory cell activation and function by dendritic cells. Int Immunol. 2004;16:1769–1780. doi: 10.1093/intimm/dxh178. [DOI] [PubMed] [Google Scholar]
- 243.Zheng Y, Manzotti CN, Liu M, Burke F, Mead KI, Sansom DM. CD86 and CD80 differentially modulate the suppressive function of human regulatory T cells. J Immunol. 2004;172:2778–2784. doi: 10.4049/jimmunol.172.5.2778. [DOI] [PubMed] [Google Scholar]
- 244.Chikuma S, Bluestone JA. Expression of CTLA-4 and FOXP3 in cis protects from lethal lymphoproliferative disease. Eur J Immunol. 2007;37:1285–1289. doi: 10.1002/eji.200737159. [DOI] [PubMed] [Google Scholar]
- 245.Onishi Y, Fehervari Z, Yamaguchi T, Sakaguchi S. Foxp3+ natural regulatory T cells preferentially form aggregates on dendritic cells in vitro and actively inhibit their maturation. Proc Natl Acad Sci USA. 2008;105:10113–10118. doi: 10.1073/pnas.0711106105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 246.Cederbom L, Hall H, Ivars F. CD4+CD25+ regulatory T cells down-regulate costimulatory molecules on antigen-presenting cells. Eur J Immunol. 2000;30:1538–1543. doi: 10.1002/1521-4141(200006)30:6<1538::AID-IMMU1538>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 247.Oderup C, Cederbom L, Makowska A, Cilio CM, Ivars F. Cytotoxic T lymphocyte antigen-4-dependent down-modulation of costimulatory molecules on dendritic cells in CD4+ CD25+ regulatory T-cell-mediated suppression. Immunology. 2006;118:240–249. doi: 10.1111/j.1365-2567.2006.02362.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 248.DiPaolo RJ, Brinster C, Davidson TS, Andersson J, Glass D, Shevach EM. Autoantigen-specific TGFbeta-induced Foxp3+ regulatory T cells prevent autoimmunity by inhibiting dendritic cells from activating autoreactive T cells. J Immunol. 2007;179:4685–4693. doi: 10.4049/jimmunol.179.7.4685. [DOI] [PubMed] [Google Scholar]
- 249.Misra N, Bayry J, Lacroix-Desmazes S, Kazatchkine MD, Kaveri SV. Cutting edge: human CD4+CD25+ T cells restrain the maturation and antigen-presenting function of dendritic cells. J Immunol. 2004;172:4676–4680. doi: 10.4049/jimmunol.172.8.4676. [DOI] [PubMed] [Google Scholar]
- 250.Grohmann U, et al. CTLA-4-Ig regulates tryptophan catabolism in vivo. Nat Immunol. 2002;3:1097–1101. doi: 10.1038/ni846. [DOI] [PubMed] [Google Scholar]
- 251.Mellor AL, Munn DH. IDO expression by dendritic cells: tolerance and tryptophan catabolism. Nat Rev Immunol. 2004;4:762–774. doi: 10.1038/nri1457. [DOI] [PubMed] [Google Scholar]
- 252.Fallarino F, et al. Modulation of tryptophan catabolism by regulatory T cells. Nat Immunol. 2003;4:1206–1212. doi: 10.1038/ni1003. [DOI] [PubMed] [Google Scholar]
- 253.Fallarino F, et al. CTLA-4-Ig activates forkhead transcription factors and protects dendritic cells from oxidative stress in nonobese diabetic mice. J Exp Med. 2004;200:1051–1062. doi: 10.1084/jem.20040942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 254.Dejean AS, et al. Transcription factor Foxo3 controls the magnitude of T cell immune responses by modulating the function of dendritic cells. Nat Immunol. 2009;10:504–513. doi: 10.1038/ni.1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 255.Teague TK, et al. Activation-induced inhibition of interleukin 6-mediated T cell survival and signal transducer and activator of transcription 1 signaling. J Exp Med. 2000;191:915–926. doi: 10.1084/jem.191.6.915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 256.Peggs KS, Quezada SA, Allison JP. Cell intrinsic mechanisms of T-cell inhibition and application to cancer therapy. Immunol Rev. 2008;224:141–165. doi: 10.1111/j.1600-065X.2008.00649.x. [DOI] [PubMed] [Google Scholar]
- 257.St Clair EW, et al. New reagents on the horizon for immune tolerance. Annu Rev Med. 2007;58:329–346. doi: 10.1146/annurev.med.58.061705.145449. [DOI] [PubMed] [Google Scholar]
- 258.Vincenti F, Luggen M. T cell costimulation: a rational target in the therapeutic armamentarium for autoimmune diseases and transplantation. Annu Rev Med. 2007;58:347–358. doi: 10.1146/annurev.med.58.080205.154004. [DOI] [PubMed] [Google Scholar]
- 259.Turka LA, et al. T-cell activation by the CD28 ligand B7 is required for cardiac allograft rejection in vivo. Proc Natl Acad Sci USA. 1992;89:11102. doi: 10.1073/pnas.89.22.11102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 260.Larsen CP, et al. Rational development of LEA29Y (belatacept), a high-affinity variant of CTLA4-Ig with potent immunosuppressive properties. Am J Transplant. 2005;5:443. doi: 10.1111/j.1600-6143.2005.00749.x. [DOI] [PubMed] [Google Scholar]
- 261.Abrams JR, et al. CTLA4Ig-mediated blockade of T-cell costimulation in patients with psoriasis vulgaris. J Clin Invest. 1999;103:1243. doi: 10.1172/JCI5857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 262.Genovese MC, et al. Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med. 2005;353:1114. doi: 10.1056/NEJMoa050524. [DOI] [PubMed] [Google Scholar]
- 263.Ruperto N, et al. Abatacept in children with juvenile idiopathic arthritis: a randomised, double-blind, placebo-controlled withdrawal trial. Lancet. 2008;372:383. doi: 10.1016/S0140-6736(08)60998-8. [DOI] [PubMed] [Google Scholar]
- 264.Merrill JT, et al. The efficacy and safety of abatacept in patients with non-life-threatening manifestations of systemic lupus erythematosus: results of a twelve-month, multicenter, exploratory, phase IIb, randomized, double-blind, placebo-controlled trial. Arthritis Rheum. 2010;62:3077. doi: 10.1002/art.27601. [DOI] [PubMed] [Google Scholar]
- 265.Vincenti F, et al. Costimulation blockade with belatacept in renal transplantation. N Engl J Med. 2005;353:770. doi: 10.1056/NEJMoa050085. [DOI] [PubMed] [Google Scholar]
- 266.Bluestone JA, et al. The effect of costimulatory and interleukin 2 receptor blockade on regulatory T cells in renal transplantation. Am J Transplant. 2008;8:2086. doi: 10.1111/j.1600-6143.2008.02377.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 267.Nashan B, Moore R, Amlot P, Schmidt AG, Abeywickrama K, Soulillou JP. Randomised trial of basiliximab versus placebo for control of acute cellular rejection in renal allograft recipients. Vol. 350. CHIB 201 International Study Group; Lancet: 1997. p. 1193. [DOI] [PubMed] [Google Scholar]
- 268.Hoyer KK, Dooms H, Barron L, Abbas AK. Interleukin-2 in the development and control of inflammatory disease. Immunol Rev. 2008;226:19. doi: 10.1111/j.1600-065X.2008.00697.x. [DOI] [PubMed] [Google Scholar]
- 269.Hodi FS, et al. Improved survival with ipilimumab in patients with metastatic melanoma. N Engl J Med. 2010;363:711. doi: 10.1056/NEJMoa1003466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 270.Hodi FS, et al. Immunologic and clinical effects of antibody blockade of cytotoxic T lymphocyte-associated antigen 4 in previously vaccinated cancer patients. Proc Natl Acad Sci USA. 2008;105:3005. doi: 10.1073/pnas.0712237105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 271.Beyersdorf N, et al. Selective targeting of regulatory T cells with CD28 superagonists allows effective therapy of experimental autoimmune encephalomyelitis. J Exp Med. 2005;202:445. doi: 10.1084/jem.20051060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 272.Suntharalingam G, et al. Cytokine storm in a phase 1 trial of the anti-CD28 monoclonal antibody TGN1412. N Engl J Med. 2006;355:1018. doi: 10.1056/NEJMoa063842. [DOI] [PubMed] [Google Scholar]