Abstract
The concept of treatment of hypertension has gone through wide swings over the years. From ignoring blood pressure (BP) treatment initially, to aggressive BP control recently. As newer and more effective drugs were developed, it was possible to lower BP to very low levels. However, recent studies have shown that aggressive BP control might not be in the best interest of the patient. Low levels of diastolic BP (DBP) have been associated with increased cardiovascular events, a situation known as the J-curve effect. This has been seen mostly with low DBP, since the coronary arteries are perfused during the diastolic phase of the cardiac cycle. Due to an autoregulatory mechanism, the heart is protected against wide fluctuations of BP. However, the presence of coronary heart disease, hypertension, especially with left ventricular hypertrophy, shift the curve to higher BP levels and makes the heart more liable to DBP fluctuations. The J-Curve effect has been reported by most investigators, but not by others. Recently, a J-Curve effect has been observed with systolic BP (SBP), as well. In contrast to the heart, the brain is very infrequently subjected to J-curve effect, and in contrast to the heart, the brain’s blood flow autoregulation depends mostly on the SBP. A Medline search of the English literature on this subject was conducted between 1992 and 2010 and 11 pertinent articles were selected. These articles with collateral literature will be discussed in this concise review.
Keywords: Hypertension, Treatment, J-curve, Coronary heart disease, Stroke
INTRODUCTION
The concept of hypertension treatment has gone through severe extremes over the years. The basic premise for these was the original concept that hypertension is an essential condition and therefore should not be treated. The term “essentielle hypertonie”, i.e. essential hypertension, was first quoted by the German physician Frank E in 1911 and continues to be used today[1]. Because of this concept, treatment of hypertension was resisted and several prominent academic physicians admonished primary care physicians who attempted to treat hypertension[2-4]. Statements such as, “The greatest danger to anyone with high blood pressure (BP) lies in its discovery, because then some fool is certain to try to reduce it” by Hay[2] in England, and “For mild benign hypertension, or BP below 200/100 mmHg, there is no indication for use of hypertensive drugs” by Friedberg[4] in the US, were not unusual. However, as time progressed, and more effective treatments for hypertension were available, physicians began to treat the condition. The great impetus for treatment were the pivotal Veterans Administration studies conducted under Ed Freis which showed that lowering the BP reduced strokes, heart failure and kidney failure[5]. Subsequent studies showed the benefits of BP lowering with respect to stroke, kidney and cardiovascular disease complications which led to National and International guidelines recommending reduction of BP to < 140/90 mmHg for uncomplicated hypertension or < 130/80 mmHg for subjects with concomitant diabetes mellitus, coronary heart disease (CHD) or chronic kidney disease[6-8]. However, recent large outcomes trials have found that more aggressive control of BP may cause a J-curve effect, especially in patients with preexisting CHD and lead to increased cardiovascular morbidity and mortality[9,10]. For this review, a Medline search of the English literature was conducted from 1992 to 2010 and 11 pertinent articles were selected. These articles with collateral literature will be discussed in this concise review, as they pertain to aggressive BP control and the incidence of cardiovascular and stroke complications.
J-CURVE PHENOMENON AND CARDIOVASCULAR COMPLICATIONS
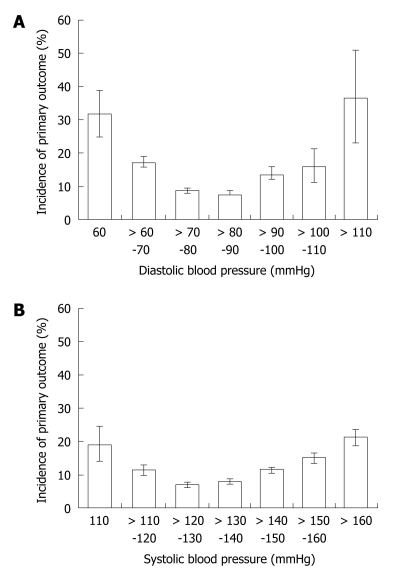
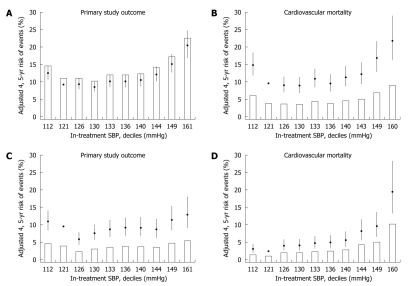
The J-curve phenomenon describes an inverse relationship between low diastolic BP (DBP) and cardiovascular morbidity and mortality. It was originally described by Stewart[11] in 1979 where 169 well matched hypertensive patients were treated and followed for 6.25 years. At the end of the study, the incidence of myocardial infarction was 5 times higher in the patients with DBP < 90 mmHg, compared with those with a DBP 100-109 mmHg (P < 0.01). Similar observations were reported later by Cruickshank et al[12], on 902 hypertensive patients treated with atenolol in combination with other drugs, and were followed for a mean of 6.1 years. They observed a J-curve relationship between a DBP of 85-90 mmHg, and myocardial infarction and death in patients with ischemic heart disease, and the cardiovascular complications rose on either side of the DBP range. Several other investigators followed with similar results[13-25]. In a review by Farnett et al[14], of 13 studies comprising 48 000 hypertensive subjects treated for a minimum of 1 year, they observed a definite J-curve effect between a DBP of 85 mmHg and cardiovascular morbidity and mortality, but not stroke. They also found that the J-curve effect was steeper in patients with preexisting ischemic heart disease and in older hypertensive patients. In most older studies the J-curve effect has been observed with a low DBP. However, 2 recent large clinical outcomes trials have observed a J-curve effect with low SBP besides low DBP, and cardiovascular and stoke complications[9,10]. In these studies, a J-curve effect was observed with SBP ≤ 130 mmHg, and a DBP ≤ 80 mmHg. In the International Verapamil-Trandolapril study (INVEST), 22 576 hypertensive patients with CHD were randomized into 2 treatment regimens, a calcium channel blocker-based regimen (verapamil), or a β-blocker-based regimen (atenolol) and were followed for 24 mo[9]. In this study, the adjusted models for the time of primary outcome (all-cause death, non-fatal myocardial infarction, and non-fatal stroke), the nadir of BP for the J-curve effect was 129/74 mmHg (Figure 1). The incidence of stroke was much less than that of myocardial infarction and correlated with low SBP, whereas the incidence of myocardial infarction was correlated with low DBP. The other study is a sub-analysis of the Ongoing Telmisartan Alone and in Combination with Ramipril Global Endpoint Trial (ONTARGET) Study. In this study, 25 620 high risk patients aged 55 years or older were equally randomized into 3 treatment regimens, telmisartan 80 mg/d, ramipril 10 mg/d, or their combination and were followed for 56 mo[10]. A J-curve effect was observed with a SBP ≤ 130 mmHg for myocardial infarction, but not for stroke (Figure 2). With respect to DBP, the highest risk for myocardial infarction occurred with an average initial DBP of 67 mmHg[10]. All studies showing a J-curve effect are summarized in Table 1.
Figure 1.
The J-curve effect for diastolic and systolic blood pressure and the first occurrence of all cause death, non-fatal myocardial infarction and non-fatal stroke. Adapted and modified with permission[9].
Figure 2.
The J-curve effect for systolic blood pressure and the incidence of the primary outcome, cardiovascular mortality and stoke in treated hypertensive patients. Adapted with permission[10].
Table 1.
Clinical trials demonstrating a J-curve effect for myocardial infarction, but not for stroke
| Author | Subjects | Age (yr) | Follow-up (yr) | Baseline (DBP mmHg) | CAD (present) | J-curve event | ||
| MI | Stroke | DBP (mmHg) | ||||||
| Messerli et al[9] | 22 576 | 66 | 2.7 | 86 | Yes | Yes | No | 76-86 |
| Sleight et al[10] | 25 620 | 55 | 4.7 | 82 | Yes | Yes | No | 75-79 |
| Stewart et al[11] | 169 | 44 | 6.3 | 124 | No | Yes | - | 100-109 |
| Cruickshank et al[12] | 902 | 55 | 6.1 | 109 | Yes | Yes | No | 80-90 |
| Waller et al[13] | 3350 | 50 | 6.5 | 110 | Yes | Yes | - | 91-98 |
| Fletcher et al[18] | 2145 | 51 | 4.0 | 107 | Yes | Yes | No | 86-91 |
| Alderman et al[19] | 1765 | 51 | 4.2 | 102 | Yes | Yes | No | 84-88 |
| Samuelsson et al[20] | 686 | 52 | 12.0 | 106 | Yes | Yes | No | 81 |
| McCloskey et al[21] | 912 | 30-79 | 3-21 | 104 | Yes | Yes | No | 84 |
| Lindblad et al[22] | 2574 | 59 | 7.4 | 92 | Yes | Yes | No | 84 |
| Pastor-Barriuso et al[23] | 7830 | 54 | 15.0 | 82 | No | Yes | No | 80 |
| Protogerou et al[24] | 331 | 85 | 3-4 | - | Yes | Yes | No | < 70 |
| Fagard et al[25] | 4695 | 70 | 1-8 | 85 | Yes | Yes | No | 70-75 |
CAD: Coronary artery disease; DBP: Diastolic blood pressure; MI: Myocardial infarction.
STUDIES WITH NO CLEAR EVIDENCE BETWEEN DBP AND J-CURVE EFFECT
Although the great majority of studies have demonstrated a J-curve effect between cardiovascular complications and DBP, there are several studies where such an effect has not been clearly demonstrated[26-31]. These studies are summarized in Table 2. Coope et al[27] did not observe any increase in cardiovascular complications with decreases in SBP or DBP. In contrast, strokes were decreased by 58%. Similar findings have also been reported by other investigators[26-31]. In the physicians and women’s studies conducted by Glynn et al[31], no J-curve effect was noted. However, most of these studies were observational and were not designed to show whether there was a J-curve effect observed between DBP or SBP and cardiovascular complications.
Table 2.
Clinical trials without clear evidence of J-curve effect
| Author | Subjects | Age (yr) | Follow-up (yr) | Baseline (DBP mmHg) | CAD (present) | J-curve effect MI | Stroke | DBP (mmHg) |
| Wilhelmsen et al[26] | 6569 | 40-60 | 3.9 | 107 | Yes | Yes2 | No | 88-89 |
| Coope et al[27] | 884 | 60-79 | 4.4 | 98 | Yes | Yes1 | No | 80-89 |
| Lubsen et al[29] | 7661 | 63.0 | 4.9 | 85 | Yes | Yes3 | No | 85 |
| Psaty et al[30] | 4702 | 72.6 | 6.7 | 71 | No | No | No | 62 |
| Glynn/PHS[31] | 22 071 | 53.2 | 13.0 | 79 | Yes | No | No | 65 |
| Glynn/WHS[31] | 39 876 | 53.8 | 6.2 | 78 | No | No | No | 70 |
Present in female smokers;
Present for trend;
Present for trend. CAD: Coronary artery disease; DBP: Diastolic blood pressure; MI: Myocardial infarction.
HEMODYNAMIC INTERRELATIONSHIPS BETWEEN BP, CORONARY ARTERY BLOOD FLOW AND J-CURVE EFFECT
Pathophysiologically, there is no argument regarding the occurrence of a J-curve effect and cardiovascular complications, because a BP of 0 mmHg is associated with 100% cardiovascular mortality. The question is at what pathophysiologic BP range the J-curve occurs. Since coronary artery perfusion occurs during the diastolic phase of the cardiac cycle, there should be an association between DBP and coronary artery perfusion. Studies in the dog have shown that the flow to the coronary arteries ceases when the DBP drops to 50 mmHg or lower, depending on the complete vasodilation or not of the coronary vascular bed[32,33]. In patients with hypertension and especially in those with left ventricular hypertrophy (LVH), there is an upward shift of the coronary perfusion pressure to 70 mmHg for hypertensive patients and 80-90 mmHg for those with hypertension and LVH, compared to normotensive controls of 60 mmHg, under maximum vasodilation with intravenous infusion of sodium nitroprusside[34]. Below these pressures the coronary blood flow decreases and the oxygen extraction increases, especially in hypertensive patients with LVH[34]. Studies in dogs with hypertension and LVH showed that the lower range of coronary autoregulation is severely impaired below a perfusion pressure of 40 mmHg for the subendocardial myocardium and predisposes it to severe ischemia or myocardial infarction[35]. The normal epicardial coronary arteries are conductance vessels and do not provide any resistance to blood flow and there is no detectable pressure drop along their entire length[36]. The coronary pressure autoregulation provides a relatively constant perfusion to the myocardium over a fairly wide perfusion pressures ranging from 45-125 mmHg[37]. Consequently, the coronary pressure autoregulation will protect the myocardium over a fairly wide epicardial pressure changes. However, in patients with CHD, the autoregulation will be compromised and a fall in DBP might lower the perfusion pressure distal to the epicardial artery stenosis below a critical level at which the autoregulation is no longer functional and the fractional flow reserve will be compromised and may lead to myocardial ischemia and myocardial infarction. This is further aggravated with the coexistence of hypertension and LVH[34,35]. Therefore, patients with CHD, hypertension and LVH are at a greater risk of manifesting a J-curve effect with low DBP than normal persons.
CEREBRAL BLOOD FLOW AUTOREGULATION
Like the heart, the brain also possesses the intrinsic ability to regulate its blood flow through a wide range of BP levels[38]. Under normal conditions, the cerebral blood flow (CBF) autoregulation typically operates at mean arterial pressures (MAP) in the order of 60-150 mmHg[38]. However, these limits are not entirely fixed, and can be moderated by sympathetic nervous system activity, the vascular renin-angiotensin system and arterial CO2 tension. In contrast to the coronary circulation, which depends on DBP, the cerebral circulation depends mostly on SBP. In a recent study using transcranial Doppler imaging, CBF autoregulation varied between a MAP of 40 and 125 mmHg[39]. These studies show that the CBF is not seriously affected by low DBP and could explain the lack of a J-curve effect regarding strokes at low DBP in contrast with cardiovascular complications. In a pivotal study, Strandgaard et al[40] studied CBF autoregulation in either untreated or ineffectively treated severe hypertensive patients, effectively treated severe hypertensive patients, or normotensive controls, and found that the lower limit of CBF autoregulation was a MAP of 113 ± 17, 96 ± 17 and 73 ± 9 mmHg, respectively, in the 3 groups. He concluded that CBF autoregulation is shifted to higher BP levels in untreated or ineffectively treated hypertensive patients compared with effectively treated hypertensives or normal controls, and also, that effective BP control in previously severe hypertensive patients, adjusts the CBF autoregulation towards normotensive controls[40].
DISCUSSION
The treatment of hypertension has gone through major extremes over the years, from the early advice of prominent cardiologists not to attempt to treat the disease[2-4], to recent national and international guidelines to treat hypertension aggressively and the “lower the better”[6-8]. Initially hypertension was considered an essential condition for survival and the term “essentielle hypertonie” was coined by the German physician Frank in 1911[1], which continues to be used today. The French used to refer to hypertension as “fièvre essentielle”, which literally means essential condition, or an ailment of life that strives to delay death[41]. However, as more effective and safe drugs were developed the treatment of hypertension was successful and led to significant reductions in cardiovascular complications and strokes. This success eventually led to more aggressive BP control. This aggressive BP control has resulted in a higher incidence of cardiovascular complications and strokes in recent large clinical outcomes trials[9,10]. First, Stewart[11] and later Cruickshank et al[12] noted an increase in cardiovascular complications after lowering the DBP below a certain level and coined the term “J-curve effect”. This effect was subsequently noted by several investigators[13-25], but not by others[26-31]. What has transpired from these studies is that the heart is more vulnerable to BP changes, but not the brain, which has a much wider BP autoregulatory range. The coronary arteries are perfused during the diastolic phase of the cardiac cycle and are more vulnerable to low DBP and this situation is aggravated with the coexistence of CHD, hypertension and LVH where the coronary artery reserve is decreased[34-37]. The question here is not whether there is a J-curve effect with low DBP, but what is a safe DBP that will provide benefits instead of increasing the risk of the treated patient. Regarding the guidelines advocating reduction of BP to < 140/90 mmHg for uncomplicated hypertensive patients and to < 130/80 mmHg for those who have coexisting CHD, diabetes or chronic kidney disease, there is no hard evidence for these recommendations as discussed by Zanchetti et al[41,42], and these recommendations were mostly based on wisdom, and not facts. In addition, most clinical trials that have produced benefits from the treatment of hypertension, the BP was seldom lowered to below 140/90 mmHg. Support for these observations comes from a recent Japanese (JATOS) Study[43]. In this study, 4418 older hypertensive Japanese patients were randomized to either an SBP reduction to < 140 mmHg (n = 2212) or to ≥ 140 mmHg (n = 2206) and followed for 2 years. At the end of the study, there was no difference in the primary endpoint of cardiovascular disease or renal failure between the 2 groups. If anything, a trend for higher cardiovascular complications was noted in the group randomized to SBP < 140 mmHg[43]. Similar observations were recently reported from the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study, which tested the aggressive SBP control in 4733 patients with type 2 diabetes mellitus[44]. In this study the patients were randomized to SBP < 120 mmHg, or < 140 mmHg and were followed for 4.7 years. There was no difference between the aggressively and less aggressively treated groups with respect to cardiovascular events, and the more aggressively treated patients had significantly more side effects than the less aggressively treated patients. However, the incidence of strokes was significantly lower in the aggressively treated patients. Also, a subanalysis of 6400 diabetic patients from the INVEST study, showed that aggressive BP control was not associated with improved cardiovascular outcomes compared with the usual BP control. In addition, in their studies, Messerli et al[9], and Sleight et al[10], observed a J-curve effect for cardiovascular complications, for DBP < 80 mmHg and SBP < 130 mmHg. In a subanalysis of the PROVE IT-TIMI 22 trial[45] in patients with acute coronary syndromes, a J-curve effect was noted for SBP and DBP of < 130 and < 80 mmHg, respectively. Based on the existing recommendations of professional guidelines for aggressive BP control and the recent evidence that aggressive BP control might not be beneficial, the caring physician may reach a quandary regarding decisions as to how aggressively he should treat his hypertensive patients. Since the recent evidence points towards a less aggressive control of BP, moderation should be adapted. The classic Greeks used to say “παν μετρον αριστον” that is, “moderation is the best thing”. Regarding this matter, Mancia et al[46] in a revised statement of the European Society of Hypertension guidelines stated, “On the basis of current data, it may be prudent to recommend lowering SBP/DBP to values within the range of 130-139/80-85 mmHg”. Along the same line of reasoning, Sleight et al[10], proposed that “future trials should be designed to test the value of SBP lowering in high risk patients in the range of 130-150 mmHg”. To this point, Kannel et al[47], caution against aggressive attempts to reduce a stubborn SBP of ≥ 140 mmHg in older individuals, because such attempts will further reduce the DBP, widen the pulse pressure (PP) and increase the cardiovascular complications. Wide PP is considered a significant afterload factor besides SBP in older individuals, causing structural cardiac changes and eventually heart failure. There is no doubt that additional prospective studies are needed to resolve this issue. Hopefully, the Systolic Blood Pressure Intervention Trial, which has similar design with the ACCORD study, with the exception that does not involve diabetic subjects, will provide the needed information when completed[48].
In conclusion, based on the evidence presented, the onset of the J-curve effect with low BP is not uniform across all patients. Older and high risk patients with preexisting CHD, diabetes and hypertension with LVH are more prone to develop the J-curve effect when their BP is decreased below a critical level. On the other hand, younger healthier individuals with uncomplicated hypertension can tolerate much lower BP without developing the J-curve effect. However, when physicians are dealing with older and high risk patients, they should refrain from aggressive BP treatment, and not lower their SBP and DBP < 130 and < 80 mmHg till new evidence becomes available.
Footnotes
Peer reviewers: Dr. Shih-Tai Chang, Department of Cardiology, Chiayi Chang Gung Memorial Hospital, 6, Sec. West Chai-Pu Road, Pu-TZ City, Chai Yi Hsien, Taiwan, China; Junichiro Hashimoto, MD, PhD, Associate Professor, Department of Blood Pressure Research, Tohoku University Graduate School of Medicine, 1-1 Seiryo-cho, Aoba-ku, Sendai 980-8574, Japan
S- Editor Cheng JX L- Editor Cant MR E- Editor Zheng XM
References
- 1.Frank E. Deutsches Archiv Fur Klin Medizin. 1911;103:397–412. [Google Scholar]
- 2.Hay J. A British Medical Association Lecture on THE SIGNIFICANCE OF A RAISED BLOOD PRESSURE. Br Med J. 1931;2:43–47. doi: 10.1136/bmj.2.3679.43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.White PD. Heart disease. 2nd ed. New York, NY: MacMillan Co; 1937. [Google Scholar]
- 4.Friedberg CK. Diseases of the heart. Philadelphia, PA: WB Saunders Co; 1949. [Google Scholar]
- 5.Effects of treatment on morbidity in hypertension. Results in patients with diastolic blood pressures averaging 115 through 129 mm Hg. JAMA. 1967;202:1028–1034. [PubMed] [Google Scholar]
- 6.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, Jones DW, Materson BJ, Oparil S, Wright JT Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension. 2003;42:1206–1252. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 7.Japanese Society of Hypertension. Guidelines for the management of hypertension (JSH 2004) Hypertens Res. 2006;29(Suppl):1–106. doi: 10.1291/hypres.29.s1. [DOI] [PubMed] [Google Scholar]
- 8.Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, et al. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC) J Hypertens. 2007;25:1105–1187. doi: 10.1097/HJH.0b013e3281fc975a. [DOI] [PubMed] [Google Scholar]
- 9.Messerli FH, Mancia G, Conti CR, Hewkin AC, Kupfer S, Champion A, Kolloch R, Benetos A, Pepine CJ. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous. Ann Intern Med. 2006;144:884–893. doi: 10.7326/0003-4819-144-12-200606200-00005. [DOI] [PubMed] [Google Scholar]
- 10.Sleight P, Redon J, Verdecchia P, Mancia G, Gao P, Fagard R, Schumacher H, Weber M, Böhm M, Williams B, et al. Prognostic value of blood pressure in patients with high vascular risk in the Ongoing Telmisartan Alone and in combination with Ramipril Global Endpoint Trial study. J Hypertens. 2009;27:1360–1369. doi: 10.1097/HJH.0b013e32832d7370. [DOI] [PubMed] [Google Scholar]
- 11.Stewart IM. Relation of reduction in pressure to first myocardial infarction in patients receiving treatment for severe hypertension. Lancet. 1979;1:861–865. doi: 10.1016/s0140-6736(79)91274-1. [DOI] [PubMed] [Google Scholar]
- 12.Cruickshank JM, Thorp JM, Zacharias FJ. Benefits and potential harm of lowering high blood pressure. Lancet. 1987;1:581–584. doi: 10.1016/s0140-6736(87)90231-5. [DOI] [PubMed] [Google Scholar]
- 13.Waller PC, Isles CG, Lever AF, Murray GD, McInnes GT. Does therapeutic reduction of diastolic blood pressure cause death from coronary heart disease. J Hum Hypertens. 1988;2:7–10. [PubMed] [Google Scholar]
- 14.Farnett L, Mulrow CD, Linn WD, Lucey CR, Tuley MR. The J-curve phenomenon and the treatment of hypertension. Is there a point beyond which pressure reduction is dangerous. JAMA. 1991;265:489–495. [PubMed] [Google Scholar]
- 15.D'Agostino RB, Belanger AJ, Kannel WB, Cruickshank JM. Relation of low diastolic blood pressure to coronary heart disease death in presence of myocardial infarction: the Framingham Study. BMJ. 1991;303:385–389. doi: 10.1136/bmj.303.6799.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hakala SM, Tilvis RS, Strandberg TE. Blood pressure and mortality in an older population. A 5-year follow-up of the Helsinki Ageing Study. Eur Heart J. 1997;18:1019–23. doi: 10.1093/oxfordjournals.eurheartj.a015360. [DOI] [PubMed] [Google Scholar]
- 17.Messerli FH, Panjrath GS. The J-curve between blood pressure and coronary artery disease or essential hypertension: exactly how essential. J Am Coll Cardiol. 2009;54:1827–1834. doi: 10.1016/j.jacc.2009.05.073. [DOI] [PubMed] [Google Scholar]
- 18.Fletcher AE, Beevers DG, Bulpitt CJ, Butler A, Coles EC, Hunt D, Munro-Faure AD, Newson R, O'Riordan PW, Petrie JC. The relationship between a low treated blood pressure and IHD mortality: a report from the DHSS Hypertension Care Computing Project (DHCCP) J Hum Hypertens. 1988;2:11–15. [PubMed] [Google Scholar]
- 19.Alderman MH, Ooi WL, Madhavan S, Cohen H. Treatment-induced blood pressure reduction and the risk of myocardial infarction. JAMA. 1989;262:920–924. [PubMed] [Google Scholar]
- 20.Samuelsson OG, Wilhelmsen LW, Pennert KM, Wedel H, Berglund GL. The J-shaped relationship between coronary heart disease and achieved blood pressure level in treated hypertension: further analyses of 12 years of follow-up of treated hypertensives in the Primary Prevention Trial in Gothenburg, Sweden. J Hypertens. 1990;8:547–555. doi: 10.1097/00004872-199006000-00008. [DOI] [PubMed] [Google Scholar]
- 21.McCloskey LW, Psaty BM, Koepsell TD, Aagaard GN. Level of blood pressure and risk of myocardial infarction among treated hypertensive patients. Arch Intern Med. 1992;152:513–520. [PubMed] [Google Scholar]
- 22.Lindblad U, Råstam L, Rydén L, Ranstam J, Isacsson SO, Berglund G. Control of blood pressure and risk of first acute myocardial infarction: Skaraborg hypertension project. BMJ. 1994;308:681–686. doi: 10.1136/bmj.308.6930.681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Pastor-Barriuso R, Banegas JR, Damián J, Appel LJ, Guallar E. Systolic blood pressure, diastolic blood pressure, and pulse pressure: an evaluation of their joint effect on mortality. Ann Intern Med. 2003;139:731–739. doi: 10.7326/0003-4819-139-9-200311040-00007. [DOI] [PubMed] [Google Scholar]
- 24.Protogerou AD, Safar ME, Iaria P, Safar H, Le Dudal K, Filipovsky J, Henry O, Ducimetière P, Blacher J. Diastolic blood pressure and mortality in the elderly with cardiovascular disease. Hypertension. 2007;50:172–180. doi: 10.1161/HYPERTENSIONAHA.107.089797. [DOI] [PubMed] [Google Scholar]
- 25.Fagard RH, Staessen JA, Thijs L, Celis H, Bulpitt CJ, de Leeuw PW, Leonetti G, Tuomilehto J, Yodfat Y. On-treatment diastolic blood pressure and prognosis in systolic hypertension. Arch Intern Med. 2007;167:1884–1891. doi: 10.1001/archinte.167.17.1884. [DOI] [PubMed] [Google Scholar]
- 26.Wilhelmsen L, Berglund G, Elmfeldt D, Fitzsimons T, Holzgreve H, Hosie J, Hörnkvist PE, Pennert K, Tuomilehto J, Wedel H. Beta-blockers versus diuretics in hypertensive men: main results from the HAPPHY trial. J Hypertens. 1987;5:561–572. doi: 10.1097/00004872-198710000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Coope J, Warrender TS. Randomised trial of treatment of hypertension in elderly patients in primary care. Br Med J (Clin Res Ed) 1986;293:1145–1151. doi: 10.1136/bmj.293.6555.1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hasebe N, Kido S, Ido A, Kenjiro K. Reverse J-curve relation between diastolic blood pressure and severity of coronary artery lesion in hypertensive patients with angina pectoris. Hypertens Res. 2002;25:381–387. doi: 10.1291/hypres.25.381. [DOI] [PubMed] [Google Scholar]
- 29.Lubsen J, Wagener G, Kirwan BA, de Brouwer S, Poole-Wilson PA. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with symptomatic stable angina and hypertension: the ACTION trial. J Hypertens. 2005;23:641–648. doi: 10.1097/01.hjh.0000160223.94220.29. [DOI] [PubMed] [Google Scholar]
- 30.Psaty BM, Furberg CD, Kuller LH, Cushman M, Savage PJ, Levine D, O'Leary DH, Bryan RN, Anderson M, Lumley T. Association between blood pressure level and the risk of myocardial infarction, stroke, and total mortality: the cardiovascular health study. Arch Intern Med. 2001;161:1183–1192. doi: 10.1001/archinte.161.9.1183. [DOI] [PubMed] [Google Scholar]
- 31.Glynn RJ, L'Italien GJ, Sesso HD, Jackson EA, Buring JE. Development of predictive models for long-term cardiovascular risk associated with systolic and diastolic blood pressure. Hypertension. 2002;39:105–110. doi: 10.1161/hy1201.097199. [DOI] [PubMed] [Google Scholar]
- 32.Bellamy RF. Diastolic coronary artery pressure-flow relations in the dog. Circ Res. 1978;43:92–101. doi: 10.1161/01.res.43.1.92. [DOI] [PubMed] [Google Scholar]
- 33.Mosher P, Ross J Jr, McFate PA, Shaw RF. Control of coronary blood flow by an autoregulatory mechanism. Circ Res. 1964;14:250–259. doi: 10.1161/01.res.14.3.250. [DOI] [PubMed] [Google Scholar]
- 34.Polese A, De Cesare N, Montorsi P, Fabbiocchi F, Guazzi M, Loaldi A, Guazzi MD. Upward shift of the lower range of coronary flow autoregulation in hypertensive patients with hypertrophy of the left ventricle. Circulation. 1991;83:845–853. doi: 10.1161/01.cir.83.3.845. [DOI] [PubMed] [Google Scholar]
- 35.Harrison DG, Florentine MS, Brooks LA, Cooper SM, Marcus ML. The effect of hypertension and left ventricular hypertrophy on the lower range of coronary autoregulation. Circulation. 1988;77:1108–1115. doi: 10.1161/01.cir.77.5.1108. [DOI] [PubMed] [Google Scholar]
- 36.Pijls NH, Van Gelder B, Van der Voort P, Peels K, Bracke FA, Bonnier HJ, el Gamal MI. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation. 1995;92:3183–3193. doi: 10.1161/01.cir.92.11.3183. [DOI] [PubMed] [Google Scholar]
- 37.Pijls NHJ, De Bruyne B. Coronary pressure. Dordrecht: Kluwer Academic Publishers; 1997. [Google Scholar]
- 38.Paulson OB, Strandgaard S, Edvinsson L. Cerebral autoregulation. Cerebrovasc Brain Metab Rev. 1990;2:161–192. [PubMed] [Google Scholar]
- 39.Lucas SJ, Tzeng YC, Galvin SD, Thomas KN, Ogoh S, Ainslie PN. Influence of changes in blood pressure on cerebral perfusion and oxygenation. Hypertension. 2010;55:698–705. doi: 10.1161/HYPERTENSIONAHA.109.146290. [DOI] [PubMed] [Google Scholar]
- 40.Strandgaard S. Autoregulation of cerebral blood flow in hypertensive patients. The modifying influence of prolonged antihypertensive treatment on the tolerance to acute, drug-induced hypotension. Circulation. 1976;53:720–727. doi: 10.1161/01.cir.53.4.720. [DOI] [PubMed] [Google Scholar]
- 41.Zanchetti A, Amery A, Berglund G, Cruickshank JM, Hansson L, Lever AF, Sleight P. How much should blood pressure be lowered The problem of the J-shaped curve. J Hypertens Suppl. 1989;7:S338–S348. doi: 10.1097/00004872-198900076-00165. [DOI] [PubMed] [Google Scholar]
- 42.Zanchetti A, Grassi G, Mancia G. When should antihypertensive drug treatment be initiated and to what levels should systolic blood pressure be lowered A critical reappraisal. J Hypertens. 2009;27:923–934. doi: 10.1097/HJH.0b013e32832aa6b5. [DOI] [PubMed] [Google Scholar]
- 43.JATOS Study Group. Principal results of the Japanese trial to assess optimal systolic blood pressure in elderly hypertensive patients (JATOS) Hypertens Res. 2008;31:2115–2127. doi: 10.1291/hypres.31.2115. [DOI] [PubMed] [Google Scholar]
- 44.Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010;362:1575–1585. doi: 10.1056/NEJMoa1001286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Bangalore S, Qin J, Sloan S, Murphy SA, Cannon CP. What is the optimal blood pressure in patients after acute coronary syndromes: Relationship of blood pressure and cardiovascular events in the PRavastatin OR atorVastatin Evaluation and Infection Therapy-Thrombolysis In Myocardial Infarction (PROVE IT-TIMI) 22 trial. Circulation. 2010;122:2142–2151. doi: 10.1161/CIRCULATIONAHA.109.905687. [DOI] [PubMed] [Google Scholar]
- 46.Mancia G, Laurent S, Agabiti-Rosei E, Ambrosioni E, Burnier M, Caulfield MJ, Cifkova R, Clément D, Coca A, Dominiczak A, et al. Reappraisal of European guidelines on hypertension management: a European Society of Hypertension Task Force document. J Hypertens. 2009;27:2121–2158. doi: 10.1097/HJH.0b013e328333146d. [DOI] [PubMed] [Google Scholar]
- 47.Kannel WB, Wilson PW, Nam BH, D'Agostino RB, Li J. A likely explanation for the J-curve of blood pressure cardiovascular risk. Am J Cardiol. 2004;94:380–384. doi: 10.1016/j.amjcard.2004.04.043. [DOI] [PubMed] [Google Scholar]
- 48. Available from: http://clinicaltrials.gov/ct2/show/NCT01206062.