A 64-year-old man was evaluated for atypical chest pain that was present during transurethral prostatectomy. He had no risk factors for coronary artery disease (CAD), no prior history of ischaemic heart disease and had not experienced any symptoms of chest pain during exercise before. Computed tomography coronary angiography (CTCA) was performed to exclude CAD.
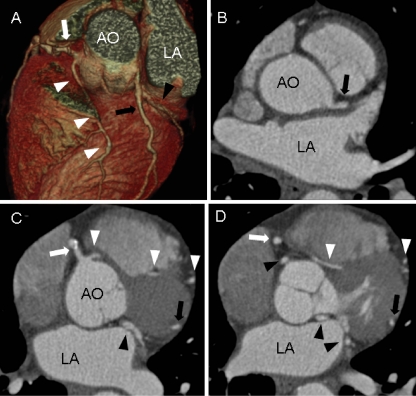
CTCA (Fig. 1) showed a normal right coronary artery (RCA). An aberrant circumflex coronary artery (CX) originated from the right coronary sinus and followed a benign retro-aortic course. A small coronary artery originated from the left coronary sinus and followed an anterolateral course. An anomalous left coronary artery originated from the right coronary sinus and followed an interarterial course between the aortic root and pulmonary trunk to the left ventricular anterior myocardial wall. Nonobstructive calcified atherosclerotic plaque was observed in the proximal RCA and mid CX. These findings were confirmed by invasive coronary angiography.
Fig. 1.
Computed tomography coronary angiography images (Siemens Sensation 64, collimation 64 × 0.6 at 900 mAs and 120 kV). Three-dimensional reconstruction (a) and transverse images (b, c, d) showing a normal right coronary artery (white arrows) and an anomalous circumflex originating from the right coronary sinus and following a retro-aortic course (black arrowheads). A second anomalous coronary artery from the right coronary sinus follows an interarterial course between aorta and pulmonary trunk (white arrowheads). A small coronary artery originates from the left coronary sinus and follows an anterolateral course (black arrows). AO aorta, LA left atrium
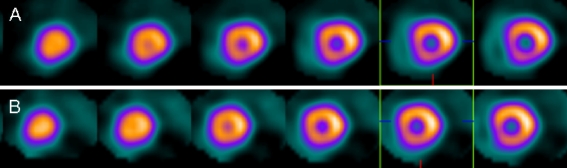
Exercise and rest single-photon emission computed tomography (SPECT) imaging showed normal myocardial perfusion and no significant electrocardiographic changes were observed (Fig. 2). As the patient had never experienced any chest pain before and exercise-induced ischaemia was absent, he was treated conservatively with β-blockers. During a 6-month follow-up, he did not experience any chest pain.
Fig. 2.
Exercise stress (a) and rest (b) single-photon emission computed tomography images showing normal myocardial perfusion in all myocardial segments
Coronary anomalies have a reported overall prevalence of 5.6%. Coronary anomalies originating from the opposite sinus have a reported prevalence of 1.0% [1]. They have a worse prognosis due to torsion or slit-like compression of the proximal parts, vasospasm, exercise-induced compression and ischaemic-induced ventricular arrhythmia.
In contrast to more conventional noninvasive tests for the evaluation of patients with suspected CAD, such as exercise ECG and SPECT, CTCA visualises the coronary anatomy and atherosclerosis accurately [2]. With the increased use of CTCA in clinical practice, coronary anomalies may be detected more frequently. However, still little is known with respect to the appropriate treatment, and evidence is largely based on case reports. Recent expert opinions suggested stress nuclear testing as additional functional test to evaluate the presence of effort-induced ischaemia [1] and stated that older patients (>35 years) without inducible ischaemia may not need surgical therapy [3]. Recently, an ACC/AHA guideline [4] recommended surgical revascularisation of coronary anomalies with an interarterial course and documented ischaemia (class 1). In contrast, surgical revascularisation of the left anterior descending coronary artery with an interarterial course but without documented ischaemia was classified as a 2b indication and might be considered. Thus, CTCA can visualise coronary anomalies accurately; however, functional tests are still warranted to evaluate its haemodynamic relevance [5] and to direct further treatment.
References
- 1.Angelini P. Coronary artery anomalies: an entity in search of an identity. Circulation. 2007;115(10):1296–305. doi: 10.1161/CIRCULATIONAHA.106.618082. [DOI] [PubMed] [Google Scholar]
- 2.Kate GJ, Weustink AC, Feyter PJ. Coronary artery anomalies detected by MSCT-coronary angiography in the adult. Neth Heart J. 2008;16(11):369–75. doi: 10.1007/BF03086181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pelliccia A. Congenital coronary artery anomalies in young patients: new perspectives for timely identification. J Am Coll Cardiol. 2001;37(2):598–600. doi: 10.1016/S0735-1097(00)01122-0. [DOI] [PubMed] [Google Scholar]
- 4.Warnes CA, Williams RG, Bashore TM, et al. ACC/AHA 2008 guidelines for the management of adults with congenital heart disease: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (writing committee to develop guidelines for the management of adults with congenital heart disease) Circulation. 2008;118(23):2395–451. doi: 10.1161/CIRCULATIONAHA.108.190811. [DOI] [PubMed] [Google Scholar]
- 5.Schuijf JD, Wijns W, Jukema JW, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006;48(12):2508–14. doi: 10.1016/j.jacc.2006.05.080. [DOI] [PubMed] [Google Scholar]