Abstract
Elderly, chronically ill patients’ ability to stay at home is dependent on their capacity to perform activities of daily living (ADLs). The Outcome and Assessment Information Set (OASIS) defines ADLs and can be evaluated in various ways. The purpose of this research was to evaluate these approaches and make recommendations for use in research. Several different approaches to the evaluation of functional status were done using ADLs (ambulation, bathing, dressing lower body, dressing upper body, feeding, grooming, toileting, and transferring) scored individually and as indices. Each approach has advantages and disadvantages depending on the research question being asked. The ADL change index score provided the most comprehensive analysis of functional status change although the categorical scores are useful for simple approaches.
Keywords: activities of daily living (ADLs), functional status, home health care
INTRODUCTION
Functional ability is a key indicator of patient ability to stay at home. For progressive chronic diseases like heart failure and chronic obstructive pulmonary disease, it is particularly important to understand functional ability as functional status losses are inevitable. Slowing the decline, then, is the goal for most patients with these diseases and the health care workers caring for them.
Current national initiatives and health care reform activities (i.e. the patient-centered medical home, transitional care from hospitals) have focused attention on home as the site of health care. For older people, in particular, functional status abilities are the key indicators that drive ability to remain at home. Numerous studies have been done on functional status measures among elderly hospital (Boyd et al, 2008; Covinsky et al, 2000) and skilled nursing facility (SNF) patients (Carpenter, Hastie, Morris, Fries, & Ankri, 2006; Jette, Warren, & Wirtalla, 2005). However, much less is known about functional status outcomes among patients with chronic conditions serviced by home health care agencies (Scharpf et al, 2006). Home health care, designed for those for whom it takes considerable and taxing effort to leave the home, measures functional ability through assessments of ability to perform activities of daily living (ADLs) as measured through the standardized data collection instrument, the Outcome and Assessment Information Set (OASIS). However, there are several measurement approaches to the ADL measures within OASIS that can be used for analyzing functional ability in research and it is not clear whether there is an approach that would be more advantageous. Thus the purpose of the present study was to evaluate various measures of functional ability using OASIS.
Keepnews, Capitman, and Rosati (2004) developed an index comprised of eight individual ADLs, seven instrumental activities of daily living (IADLs) and an additional variable that accounted for frequency of pain interfering with functioning. To construct their index, they also rescored each measure on a scale of 0–100 and concluded that overall 78.1% of patients improved, 18.5% declined, and the remainder stayed the same. In another study, OASIS ADLs were evaluated using the raw scores, the Likert corrected scores (described below), and Rasch Partial Credit model scores. The researchers concluded that a corrected Likert approach yielded comparable results to the Rasch approach (Fortinsky, Garcia, Sheehan, Madigan & Tullai-McGuinness, 2003). The research to date using OASIS to evaluate functional ability is limited in scope and uses various approaches to measurement as noted above.
From the perspective of the clinician and the home health care agency, current quality improvement programs focus on individual ADLs items rather than overall ADL performance measures of functional ability. The Centers for Medicare & Medicaid Services, administrator and payer of the Medicare program for aged and disabled Americans, provides home health care agencies with several types of reports based on the OASIS. Internal agency reports identify the number of patients whose conditions improve versus those who declined and stayed the same at the individual ADL item level. There also are public reports, available on the world wide web (www.medicare.gov Home Health Compare), that provide agency level information on the percentage of patients who improve in specific ADL items. While helpful for targeting specific ADL items, a composite score or approach may also be beneficial in agency quality improvement programs to identify trends in patient populations (i.e. higher levels of functional impairment at discharge from home health care may require addressing clinical care differently during and after home health care).
As well, at the individual patient level, clinicians and agency administrators may find a composite score or approach helpful in identifying more generic indications of patient improvement or decline. For example, a clinician whose caseload of patients has a persistent rate of functional status decline from home health care admission to discharge may benefit from focusing care on assessment and interventions to identify frailty.
Since there are multiple approaches to the evaluation of functional status change and no clear guidance from the literature as to the advantages and disadvantages of the various approaches, the purpose of this study was to present several different measures of functional status for home health care patients with heart failure. We present examples using simple demographic measures to demonstrate the advantages and disadvantages of each approach. The focus of the present paper is on patients with heart failure although the results may apply to other progressive chronic diseases among home health care patients as well (e.g. patients with COPD or neuromuscular diseases).
DESIGN AND METHODS
DATA SOURCE
The data come from the Outcomes and Assessment Information Set (OASIS) from 2005. After IRB approval and completion of a Data Use Agreement with CMS, OASIS data for patients with a primary diagnosis of heart failure were obtained from the CMS Chronic Conditions Warehouse (CCW). The CCW is a CMS resource available to researchers that provides the ability to more easily link CMS data sources from claims, clinical data like OASIS, and other files that describe Medicare beneficiaries. CCW uses a unique identifier that does not include name, Medicare number, Social Security number and provides increased privacy protections. Data from the CCW for the study included only patients with a primary diagnosis of heart failure in OASIS, defined by the ICD 9 code of 428 and associated sub-codes.
DESCRIPTION OF THE OUTCOMES AND ASSESSMENT INFORMATION SET
Implemented by the Centers for Medicare & Medicaid Services (CMS) in 1999, the OASIS survey instrument is used by all home health care agencies receiving payment for services through Medicare and/or Medicaid. OASIS was designed as a clinical assessment tool for home health care agencies. Additionally, it is used for reimbursement, quality reporting, and Medicare survey and certification purposes. OASIS data are collected on home health care admission, upon resumption of care following a hospital stay, discharge, when a patient dies or is transferred to the hospital or at least every 60 days if home health services continue (recertification). The most comprehensive time points for OASIS data collection are admission and discharge while the other time points have abridged versions of the OASIS assessment.
There are several domains within the OASIS including demographic information, evaluation of living arrangements and caregiving assistance, clinical information (e.g. wound status, cognitive functioning), basic mental health indicators (e.g. presence of anxiety, presence of depressive symptoms), and functional status assessment at the individual item level.
Reliability and validity of OASIS data
OASIS has been evaluated for internal consistency using Cronbach’s coefficient alpha. The coefficient alpha for baseline and discharge ADL scores were consistently 0.88 and higher, considerably higher than the acceptable value of 0.70 (Nunnally & Bernstein, 1978). Less information is reported on the validity of the OASIS. Researchers who have compared domains of the OASIS with existing instruments to examine concurrent validity (n = 150) find that the functional status items correlate highly with the Katz Index of Activities of Daily Living.(Tullai-McGuinness, Madigan, & Fortinsky, 2009) while depressive symptoms are under-represented in OASIS compared to the Center for Epidemiologic Studies-Depression instrument. The limited evidence on concurrent validity raises concerns that the OASIS measures may not sufficiently capture the intent of some of the measures. This may be of less concern for clinical practice but may limit OASIS usability for research for areas like depressive symptoms for which there is not sufficient concurrent validity.
Measures of functional status within OASIS
Within the OASIS, there are individual items that assess different aspects of functional performance. The ADL items include grooming, dressing upper body, dressing lower body, bathing, toileting, transferring, ambulation/locomotion, and feeding/eating. The individual items have different levels of scoring—for example, ambulation/locomotion ranges from 0 (independent) to 5 (bedfast, unable to ambulate) while dressing upper body ranges from 0 (independent) to 3 (requires total assistance to dress upper body). For all the ADLs, a value of 0 indicates complete independence and is the best score possible. Table 1 describes each individual ADL.
Table 1.
Definitions for Individual ADLs:
| ADL | Definition of Values |
|---|---|
| ADL: Grooming | 0 = Able to groom self unaided, with or without use of assistive devices |
| 1 = Grooming utensils must be placed within reach | |
| 2 = Someone must assist the patient to groom self | |
| 3 = Patient depends entirely upon someone else | |
| ADL: Ability to dress upper body | 0 = Able to obtain, put on, and remove clothing |
| 1 = Able to dress upper body without assistance | |
| 2 = Someone must help patient | |
| 3 = Patient depends entirely on someone else | |
| ADL: Ability to dress lower body | 0 = Able to obtain, put on and remove clothing |
| 1 = Able to dress lower body without assistance | |
| 2 = Someone must help the patient | |
| 3 = Patient depends entirely on someone else | |
| ADL: Bathing | 0 = Able to bathe self in shower or tub independently |
| 1 = With the use of devices, is able to bathe | |
| 2 = Able to bathe with the assistance of a person | |
| 3 = Participates in bathing in shower or tub | |
| 4 = Unable to use the shower or tub, but able to assist | |
| 5 = Unable to effectively participate in bathing, totally bathed by another person | |
| ADL: Toileting | 0 = Able to get to and from the toilet independently |
| 1 = When reminded assisted or supervised | |
| 2 = Unable to get to and from toilet; can use bedside commode | |
| 3 = Unable to get to from the toilet or bedside commode; can use a bedpan | |
| 4 = Is totally dependent for toileting | |
| ADL: Transferring | 0 = Able to independently transfer |
| 1 = Transfers with minimal human assistance | |
| 2 = Unable to transfer self but is able to bear weight | |
| 3 = Unable to transfer self and is unable to bear weight | |
| 4 = Bedfast, unable to transfer but is able to turn | |
| 5 = Bedfast, unable to transfer and is unable to turn | |
| ADL: Ambulation/Locomotion | 0 = Able to independently walk |
| 1 = Requires use of a device | |
| 2 = Able to walk only with the supervision | |
| 3 = Chairfast, unable to ambulate but can use wheelchair | |
| 4 = Chairfast, unable to ambulate and or use wheelchair | |
| 5 = Bedfast | |
| ADL: Feeding or eating | 0 = Able to independently feed self |
| 1 = Able to feed self but requires help in setup | |
| 2 = Unable to feed self and requires human assistance | |
| 3 = Able to take in nutrients orally and tube fed | |
| 4 = Unable to take in nutrients orally; tube fed | |
| 5 = Unable to take in nutrients orally or by tube feeding |
Source: OASIS B1 version 1.6 available from CMS.gov (retrieved October 3,2010 from http://www.cms.gov/OASIS/04_DataSpecifications.asp#TopOfPage
Since OASIS was not meant for scale scoring, researchers have evaluated whether a composite score is most appropriate (Fortinsky, Garcia, Sheehan, Madigan, & Tullai-McGuinness, 2003). In the present study, we use the corrected Likert approach where each individual ADL response is divided by the highest value allotted for that ADL. For example, a transferring score of 3 for an individual patient is scored as a 0.6 (since 3/5=0.6). Using the corrected Likert approach puts all of the individual ADLs on the same scale, ranging from zero to one. The total functional status score is then computed by summing the individually adjusted items for a range from zero to eight with eight indicating total dependence in all functional items while zero indicates complete independence.
For ease of interpretation and to insure complete data, we included only those 2005 OASIS patients that had an initial assessment of start of care and a final assessment of discharge since functional status information is collected at home health care admission and discharge but not other assessments (e.g. death, transfer to a hospital). We ended up eliminating almost one-quarter of the patients (23%) since their OASIS episode ended without a discharge. However, there were still substantial numbers of patients available with full sets of data (N=95,948) to provide thorough analyses.
MEASURES
Discharge ADL Individual items and Index Score
In the present study, discharge ADL status was evaluated by looking at each of the eight ADLs individually (grooming, dressing upper body, dressing lower body, toileting, bathing, transferring, ambulation, and feeding/eating) at discharge. Alternatively, a discharge index score was created by calculating the corrected Likert score for each individual ADL and then summing across scores to create an index with a minimum score of zero to a maximum score of eight. A negative score in the ADL discharge index indicates the patient has improved since zero is the best score possible as it defines complete independence.
Change ADL Index
The change score was calculated by subtracting the baseline ADL index score from the discharge ADL index score. In the change score, a zero indicates that there was no change across all eight ADLs (i.e. a patient may have improved two points in one ADL but subsequently declines one point each in two other ADLs for a zero net sum). A negative score in the ADL change score indicates that the patient has exhibited improvements since a higher score indicates worse functional ability. The larger the magnitude of improvement, the smaller the negative number (e.g., a change score of −0.89 indicates more improvement than a change score of −0.32).
Dichotomous Index
The dichotomous ADL score was a measure indicating whether or not a patient experienced a decline in the summed score, coded as yes or no. If a patient’s ADL change score was positive (e.g. any number greater than zero) that patient was defined as having had overall decline (e.g., declines in one or more ADLs). A score of zero (zero net sum) or larger would indicate either no change or improvements and would be defined as ‘no decline’. In this case, we are collapsing those patients with improvements in with those who have no change.
Trichotomous Index
The trichotomous measure was defined much the same way as above except that the patients with improvements were separated from those patients with no overall change in ADL status. The trichotomous ADL measure was defined as a ‘1’ if a patient had declines, a ‘0’ if a patient had net zero sum, and a ‘−1’ if the patient experienced improvements.
Unit Change
Finally, we examined change by individual ADLs based on magnitude of change. In short, improvements and declines were evaluated by looking at both frequencies of one unit of change (i.e. change in one point) and two or more units of change. For example, if a patient was admitted as a ‘2’ for grooming and discharged as a ‘0’ they would have a two unit change (i.e. improvement) in grooming.
ANALYSIS
All measures were compiled and all analyses were completed using SAS 9.1. Descriptive measures were evaluated using measures of central tendency and dispersion. Specifically, to further test the appropriateness of using the change ADL score, multivariate analyses were done using SAS 9.1 PROC REG. The analyses evaluated patient factors that best explain changes in ADL status. The OASIS items that were used are noted in parentheses after the variable where applicable whereas items that were categorized do not have this level of detail. For example, age was calculated from date of birth and date of home health care admission. (Further detail on these calculations are available from the authors.) The following clinical information upon admission to home health care were used in the multivariate analysis: age, race (m0140), gender (m0069), admission ADL score, ability to manage oral medications (m0780), cognitive functioning(m0560), dyspnea status (m0490), disease severity of the primary diagnosis (m0230), urinary incontinence (m0520), life expectancy (m0280), living alone status (m0340), any anxiety (m0580), any depressive symptoms (m0590), any problem behaviors (m0610), any high risk behaviors (m0290), overall prognosis (m0260), rehabilitative prognosis (m0270), primary caregiver (m0360), and total number of comorbidities (m0240).
POPULATION DESCRIPTION
The final analytic dataset consists of 95,948 patients. The mean age was 80.9 (SD=9.4) with 62% of the patient population being female. The majority of patients were White (83%, 79,570) with African-Americans comprising the second largest racial category with 13% (N=12,440). There were very few minorities with 2% Hispanic representation and 2% other minorities or unknown. In part, this reflects the OASIS item for ethnicity and race that does not code Hispanic in the same way that other federal systems do.
RESULTS
Of these 95,948 patients, 14% (n=13,572) experienced functional status decline while the remaining 86% either stayed the same or improved. Using the trichotomous measure, among the 86% that did not decline, 70% experienced improvements and the remaining 16% stayed the same (i.e. net sum score of zero).
With very few exceptions, patients consistently improved from admission to discharge across all levels of dependency. (Table 2). The means for the baseline, discharge and change scores were 1.89, 1.17 and −0.73 respectively (Table 2). The mean change score being negative reflects that overall the majority of patients experienced improvement, which is consistent with the dichotomous and trichotomous scores. The median for the change score is quite small (Median=−0.53) because a substantial portion of the patient population (18%) had a discharge score of ‘0’ indicating that they were completely independent at discharge.
Table 2.
Analysis of ADL Index Scores
| Mean | Median | Minimum | Maximum | Std. Dev | |
|---|---|---|---|---|---|
| Baseline ADL | 1.89 | 1.67 | 0.00 | 8.00 | 1.47 |
| Discharge ADL | 1.17 | 0.60 | 0.00 | 8.00 | 1.41 |
| Change Score | −0.73 | −0.53 | −7.20 | 7.20 | 1.11 |
| Discrete Index Scores: | N | % | |||
| Dichotomous | |||||
| Decline (‘Yes’) | 13572 | 14% | |||
| (‘No”) | 82376 | 86% | |||
| Trichotomous | |||||
| Decline | 13572 | 14% | |||
| Stay Same | 15260 | 16% | |||
| Improve | 67116 | 70% | |||
There were significant differences seen by race with Hispanic and other minority patients consistently experiencing larger magnitudes of improvement (i.e., larger negative change scores) as compared to White patients (see Table 3). There were few differences between Black and White patients for the continuous and categorical measures, regardless of how they were measured. For gender, there were some differences by gender using the discharge score but no differences when using the change score. Similarly, the categorical measures showed few differences by gender (see Table 3). By age category, the oldest old (age 85 and older) have the most impairment at baseline and at discharge although all four groups have overall mean improvement. The mean change scores are similar across the four age group categories. The categorical indices (dichotomous and trichotomous) demonstrate more decline among the oldest old group as compared to the three younger categories; these changes are substantially more so than the mean discharge or mean change scores (see Table 3).
Table 3.
Descriptives for ADL index scores by gender, race, and age:
| Baseline | Discharge | Change | Dichotomous | Trichotomous | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Median | Mean (SD) | Median | Mean (SD) | Median | % decline | % no decline | % improve | % same | % decline | |
| Gender: | |||||||||||
| Male | 1.78(1.45) | 1.60 | 1.06(1.37) | 0.60 | −0.72(1.12) | −0.52 | 14 | 86 | 69 | 17 | 14 |
| Female | 1.96(1.48) | 1.80 | 1.23(1.43) | 0.60 | −0.73(1.10) | −0.53 | 14 | 86 | 71 | 15 | 14 |
| Race: | |||||||||||
| White | 1.87(1.45) | 1.67 | 1.15(1.39) | 0.60 | −0.72(1.11) | −0.53 | 14 | 86 | 70 | 16 | 14 |
| Black | 1.94(1.53) | 1.80 | 1.18(1.43) | 0.60 | −0.75(1.09) | −0.53 | 14 | 86 | 69 | 17 | 14 |
| Hisp. | 2.35(1.65) | 2.13 | 1.52(1.62) | 0.93 | −0.82(1.13) | −0.60 | 13 | 87 | 71 | 16 | 13 |
| Other minority | |||||||||||
| 2.25(1.61) | 2.05 | 1.39(1.50) | 0.80 | −0.86(1.15) | −0.67 | 13 | 87 | 73 | 14 | 13 | |
| Age: | |||||||||||
| <65 | 1.56(1.39) | 1.27 | 0.84(1.16) | 0.40 | −0.72(1.02) | −0.40 | 11 | 89 | 66 | 22 | 11 |
| 65–74 | 1.66(1.37) | 1.47 | 0.89(1.21) | 0.40 | −0.77(1.08) | −0.53 | 12 | 88 | 70 | 18 | 12 |
| 75–84 | 1.81(1.41) | 1.60 | 1.05(1.32) | 0.60 | −0.76(1.09) | −0.60 | 13 | 87 | 71 | 15.5 | 13 |
| >=85 | 2.12(1.54) | 1.92 | 1.45(1.55) | 0.80 | −0.68(1.14) | −0.52 | 16.5 | 83.5 | 69 | 14.5 | 16.5 |
Further analysis was done to examine the assumptions for a normal distribution with Figure One providing the histogram for the change score. The change score was the only distribution that approached normality whereas the discharge score was not transformable in this instance, even with several attempts to achieve a normal distribution using various mathematical approaches.
Figure 1.
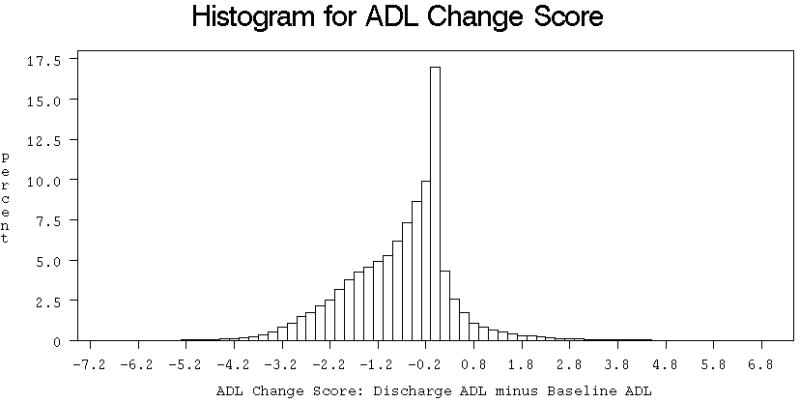
Histogram for ADL Change Score
The individual ADL with the largest magnitudes of improvement was dressing lower body (−.17) followed closely by bathing (−.14), dressing upper body (−.13) and grooming (−.11). See Table 4. Toileting and feeding/eating had the most independent patients (i.e., complete independence baseline score equals ‘0’) at baseline, with mean baseline scores of 0.07 and 0.11 respectively. Likewise, toileting and feeding had substantial independence at discharge (mean discharge scores of 0.4 and 0.6, respectively). The most dependence at baseline was for bathing and dressing lower body (mean baseline scores of 0.44 and 0.37, respectively). It follows then that the individual ADLs that contribute most to the indices were bathing, dressing upper body, and dressing lower body since they comprised the ADLs with the most room for improvement. When examining individual ADLs by the units of change, there were substantially more one unit changes than two unit changes for both improvements and declines indicating that within home health episodes of care, changes in functional status (either improvements or declines) were relatively small in magnitude.
Table 4.
Descriptives for Baseline, Discharge, and Change Scores and Unit Change Percentages for Individual ADLs:
| Baseline | Discharge | Change | Unit Change(%) Improvements | Unit Change(%) Declines | Unchanged | |||
|---|---|---|---|---|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | One Unit | ≥ Two Units | One Unit | ≥ Two Units | ||
| Ambulation | 0.23(0.20) | 0.17(0.16) | −0.05(0.13) | 27% | 3% | 4.5% | 1% | 64.5% |
| Bathing | 0.44(0.40) | 0.29(0.26) | −0.14(0.25) | 25.5% | 25% | 7% | 3% | 40% |
| Feeding | 0.07(0.00) | 0.04(0.10) | −0.03(0.10) | 17.5% | 0.5% | 5% | 0.5% | 76% |
| Dressing lower | 0.37(0.33) | 0.20(0.31) | −0.17(0.30) | 22% | 17% | 4.5% | 1.5% | 55% |
| Dressing upper | 0.29(0.33) | 0.15(0.27) | −0.13(0.26) | 25.5% | 10% | 4.5% | 1% | 59% |
| Grooming | 0.24(0.00) | 0.13(0.26) | −0.11(0.26) | 22% | 8% | 5% | 1.5% | 63% |
| Toileting | 0.11(0.00) | 0.06(0.18) | −0.05(0.17) | 16% | 4% | 3% | 1% | 76% |
| Transferring | 0.16(0.20) | 0.11(0.15) | −0.05(0.13) | 29.5% | 2% | 6% | 0.5% | 62% |
The multivariate results (Table 5) indicate that the most important patient clinical factors influencing change in ADL status are patients’ ADL score at home health care admission (standardized regression coefficients=−0.56) and patients’ ability to manage oral medications at admission to home health care (standardized regression coefficients=0.08), where negative coefficients indicate improvements from admission to discharge. Additionally, age (standardized regression coefficient=0.07), cognitive functioning (standardized regression coefficient=0.07), urinary incontinence (standardized regression coefficient=0.06), and overall rehabilitation (standardized regression coefficient=−0.06) indicate some impact on functional status change while the remaining factors all had coefficients of 0.05 or less. The model using the change ADL score as the dependent variable performed well in predicting patient clinical factors that are associated with changes in functional status with an R2 =0.23 (F=1655.36, p<.0001). In summary, improvements in ADL change scores were associated with worse ADL scores at admission, better oral medication management at admission, being younger than 85 years of age, having better cognitive functioning at admission, having no urinary incontinence upon admission, and having a worse rehabilitation prognosis at admission to home health care.
Table 5.
Multivariate model results (N=95,948)
| Covariate | Estimate | Standard Error | Standardized Estimate |
|---|---|---|---|
| Intercept | 0.29 | 0.02*** | 0.00 |
| Baseline ADL | −0.42 | 0.003*** | −0.56 |
| Oral med mgmt | 0.12 | 0.006*** | 0.08 |
| Age | 0.15 | 0.007*** | 0.07 |
| Cognitive function | 0.11 | 0.005*** | 0.07 |
| Urinary incontinence | 0.13 | 0.007*** | 0.06 |
| Rehabilitation | −0.15 | 0.01*** | −0.06 |
| Prognosis | −0.15 | 0.01*** | −0.05 |
| HF severity | −0.07 | 0.005*** | −0.04 |
| Lives alone | −0.09 | 0.007*** | −0.04 |
| Total number comorbids | −0.03 | 0.002*** | −0.03 |
| Gender (1=Female) | 0.04 | 0.007*** | 0.02 |
| Race (1=African-American) | 0.05 | 0.01*** | 0.02 |
| Any anxiety | −0.05 | 0.007*** | −0.02 |
| Any problem behaviors | 0.03 | 0.009** | 0.01 |
| Life expectancy | −0.03 | 0.003** | −0.01 |
| Primary caregiver | −0.02 | 0.009* | −0.01 |
| Dyspnea | −0.01 | 0.003*** | −0.01 |
Note: Depressive symptoms and High risk behaviors were not significant (p>.05) and not reported here.
Adj R-Sq = 0.23, F = 1655.36, p<.0001
p<.001
p<.01
p<.05
DISCUSSION
The results of the present study indicate that most (70%) home health care patients with HF improve during home health care services, although the magnitude of change is small by overall score, regardless of measure, and by individual ADL item. Using the same approach used by Fortinsky, Garcia, Joseph, Madigan, and Tullai-McGuinness (2003) with the corrected Likert score, we were able to determine various measures of functional ability, while adding additional approaches such as the unit change score, which has not been described in the extant literature.
Our multivariate results are comparable to previous research that found prior physical functioning, cognitive functioning, number of comorbidities, and anxiety are all factors associated with functional status decline (Stuck et. al, 1999). Stuck et al. (1999) concluded that functional limitation, whether observed or self-reported, was a predictor of functional decline which is supported in the current study with functional capacity at admission being the largest predictor of functional decline at discharge. Furthermore, these measures may have utility for use in patient populations with progressive diseases other than heart failure, although further testing would be necessary to confirm this.
Additionally, this study is consistent with previous findings from Keepnews, Capitman, and Rosati (2004) who found an association between functional status decline and cognitive impairment, urinary incontinence, and age. In their study advanced age, urinary incontinence, and cognitive impairment at baseline all negatively impacted functional status at discharge which is consistent with our findings that younger age, no urinary incontinence, and better cognitive functioning at admission are associated with overall improvements in functional status at discharge. These findings are consistent even with the difference in OASIS scoring between the two studies.
The various scoring approaches mechanisms show different aspects of patient functional ability. The ADL change score takes into account the baseline score and provides a measure that examines the actual change in status from baseline to discharge. However, the index discharge score finds differences by gender and age category that are not evident when the index change scores is used.
The trichotomous score provided information that was not seen when using the dichotomous score. Notably, there were more patients whose scores stayed the same (16%) than those who declined (14%). Across demographic comparisons, these trends persisted. This may reflect the nature of the chronic, progressive disease where maintaining the same functional status is a positive outcome. The biggest differences were in the age categories where the youngest age categories had the most differences between those who stayed the same (22%) and those who declined (11%). Additionally, the oldest age category (85 and older) had slightly more declines than plateaus.
From a clinical perspective, it may be advantageous to use the individual ADL change scores, particularly the bathing score, since it had the most impact on the indices as well as providing the most change over time. Bathing is a complex task, requiring multiple kinds of movements (transfers, use of upper and lower limbs) and may be a proxy representation of how well these patients with HF can manage their self-care. Additionally, ambulation/locomotion, while more obvious for a measure of functional capacity, is likely to be a driving factor prior to home health care admission where patients with substantial impairment in this item are likely to not return home. Specifically, patients who are very impaired in ambulation/locomotion at the time of hospital discharge may require institutional care prior to a return home because of safety concerns. Use of individual ADL items for clinical evaluation are helpful as home health care agency staff identify the effectiveness of their services and which items patients under their care improve in. In addition, however, the use of a change score may be helpful at the agency level (for quality improvement activities) and at the individual clinician and patient level to give a “snapshot” indicator of overall performance without having to examine each individual ADL item. Because the individual ADL items fluctuate from admission to discharge, an overall change score may be helpful in guiding clinical practice.
Home health care research focused on functional status impairment has not had the same depth of research as in other sites of care, like skilled nursing facilities that have determined “meaningful differences” in magnitudes of change (Carpenter, Hastie, Morris, Fries, & Ankri, 2006). A “meaningful difference” in ADL score for home health care would guide policy and practice decisions for what level of change is possible and attainable. As well, more research in home health care is needed on ADL loss or how ADLs deteriorate among older people as the gerontology literature has identified “late loss” ADLs like feeding and eating (Katz, Ford, Moskowitz, Jackson, & Jaffe, 1963) that influence nursing home placement.
There are a few limitations of this study related to its generalizability. This research applies only to patients with admission and discharge OASIS forms. OASIS data for ADLs are not collected on patients who are transferred to other settings (hospitals, SNFs, hospice, etc.) and therefore, we miss out on over one fifth of the patient population. A second limitation is that this patient population is much more limited than the general population of home health care patients who represent multiple diagnoses and conditions. Although patients with HF constitute a substantial proportion of home health care patients, they do not represent the patients with time-limited conditions like total knee replacements or short-term surgical wounds. Thus the results may not apply to these other types of patients.
CONCLUSIONS
Measures of functional status in home health care provide opportunities for researchers to use various measures, including individual scores and indices with both continuous and categorical approaches. Based on these findings, we suggest use of the change score as it provides a normal distribution and takes into account the change from baseline home health care status to discharge. For a categorical approach, we recommend the use of the trichotomous approach as there are differences by age that were not evident with the dichotomous measure and it better identifies those with declines and improvements as compared to those whose functional abilities remain the same.
Additionally, we recommend that researchers consider examination of the individual ADL items, particularly bathing, as it seems to represent an important measure for improvement during home health care, likely because of the complexity of the measure for patients with HF.
Acknowledgments
Support for this study was provided through the National Heart Lung and Blood Institute, R01 HL085725, to Elizabeth Madigan, PI.
References
- Boyd CM, Landefeld CS, Counsell SR, Palmer RM, Fortinsky RH, Kresevic D, Burant C, Covinsky KE. Recovery of activities of daily living in older adults after hospitalization for acute medical illness. Journal of the American Geriatric Society. 2008 Dec;56(12):2171–9. doi: 10.1111/j.1532-5415.2008.02023.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter GI, Hastie CL, Morris JN, Fries BE, Ankri J. Measuring change in activities of daily living in nursing home residents with moderate to severe cognitive impairment. BMC Geriatr. 2006 Apr 3;6:7. doi: 10.1186/1471-2318-6-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Covinsky KE, Palmer RM, Counsell SR, Pine ZM, Walter LC, Chren MM. Functional status before hospitalization in acutely ill older adults: validity and clinical importance of retrospective reports. Journal of the American Geriatric Society. 2000 Feb;48(2):164–9. doi: 10.1111/j.1532-5415.2000.tb03907.x. [DOI] [PubMed] [Google Scholar]
- Fortinsky RH, Garcia RI, Joseph ST, Madigan EA, Tullai-McGuinness S. Measuring disability in Medicare home care patients: application of Rasch modeling to the outcome and assessment information set. Med Care. 2003;41:601–615. doi: 10.1097/01.MLR.0000062553.63745.7A. [DOI] [PubMed] [Google Scholar]
- Jette DU, Warren RL, Wirtalla C. Validity of functional independence staging in patients receiving rehabilitation in skilled nursing facilities. Archives of Physical Medicine and Rehabilitation. 2005 Jun;86(6):1095–101. doi: 10.1016/j.apmr.2004.11.035. [DOI] [PubMed] [Google Scholar]
- Katz S, Ford AB, Moskowitz RW, Jackson BA, Jaffe MW. Studies Of Illness In The Aged. The Index Of ADL: A Standardized Measure Of Biological and Psychosocial Function. JAMA. 1963 Sep 21;185:914–9. doi: 10.1001/jama.1963.03060120024016. [DOI] [PubMed] [Google Scholar]
- Keepnews D, Capitman JA, Rosati RJ. Measuring patient-level clinical outcomes of home health care. J Nurs Scholarsh. 2004;36(1):79–85. doi: 10.1111/j.1547-5069.2004.04017.x. [DOI] [PubMed] [Google Scholar]
- Nunnally JC, Bernstein IH. Psychometric Theory. 3. New York: McGraw-Hill; 1994. [Google Scholar]
- Scharpf TP, Colabianchi N, Madigan EA, Neuhauser D, Peng T, Feldman PH, Bridges JF. Functional status decline as a measure of adverse events in home health care: an observational study. BMC Health Serv Res. 2006 Dec 20;6:162. doi: 10.1186/1472-6963-6-162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuck AE, Walther JM, Nikolaus T, Bula CJ, Hohmann C, Beck JC. Risk factors for functional status decline in community-living elderly people: a systematic literature review. Soc Sci Med. 1999 Feb;48(4):445–69. doi: 10.1016/s0277-9536(98)00370-0. [DOI] [PubMed] [Google Scholar]
- Tullai-McGuiness S, Madigan EA, Fortinsky RH. Validity testing the Outcomes and Assessment Information Set (OASIS) Home Health Care Services Quarterly. 2009;28(1):45–57. doi: 10.1080/01621420802716206. [DOI] [PMC free article] [PubMed] [Google Scholar]


