Abstract
Objective
To examine spousal associations between functional limitation and depressive symptom trajectories in a national sample of older long-term married couples.
Design
We use 14.5-year longitudinal data on functional limitations and depressive symptoms from 1,704 couples participating in the Study of Asset and Health Dynamics Among the Oldest Old (AHEAD).
Main Outcome Measures
Activities of Daily Living and a short version of the Center for Epidemiologic Studies Depression Scale were used.
Results
Between-person difference findings corroborate previous research by showing that levels and changes in functional limitations and depressive symptoms are closely interrelated among wives and husbands. Importantly, our results further demonstrate sizeable associations in levels and changes in functional limitations and depressive symptoms between spouses. For example, functional limitation levels in one spouse were associated with depressive symptom levels in the respective other spouse. Spousal associations remained after controlling for individual (age, education, cognition) and spousal covariates (marriage duration, number of children) and did not differ between women and men.
Conclusion
Our findings highlight the important role of marital relationships in shaping health trajectories in old age because they show that some of the well-documented between-person differences in functional limitations and depressive symptoms are in fact related to spouses.
Keywords: aging, couples, longitudinal trajectories, unctional limitations, depressive symptoms
Increases in functional limitations represent a common experience in old age (Baltes & Smith, 2003; Manton, Corder, & Stallard, 1997). Past research indicates that functional limitations can impact mental health and are related to increased risk for depression (Everson-Rose et al., 2005; Lenze et al., 2001; Schillerstrom, Royall, & Palmer, 2008; Yang, 2006). Importantly, social contextual factors seem to play a key role in contributing to previously reported associations between functional limitations and depression (Geerlings, Beekman, Deeg, Twisk, & Van Tilburg, 2001; Lenze et al., 2001; Penninx, Leveille, Ferrucci, van Eijk, & Guralnik, 1999; Yang, 2006). To date, most research investigating links between functional limitations and depression in old age considers the individual as the unit of analysis. However, researchers have recently called for an investigation of the spousal dynamics and mutual influences in physical and mental health that uses the couple as the unit of analysis to examine health trajectories based on information from both partners (Berg & Upchurch, 2007; Hoppmann & Gerstorf, 2009; Lam, Lehman, Puterman, & DeLongis, 2009; Siegel, Bradley, Gallo, & Kasl, 2004; Strawbridge, Wallhagen, & Shema, 2007; Townsend, Miller, & Guo, 2001). The present study adopts this approach and extends previous work by examining how functional limitations and depressive symptoms are interrelated in older couples. Specifically, we use 14.5-year longitudinal data from 1,704 couples who participated in the AHEAD study. We simultaneously model longitudinal changes in functional limitations and depressive symptoms to examine how these two domains of functioning are interrelated among wives, among husbands, and between spouses.
In a first step, we review the literature on functional limitation–depressive symptom associations as derived from research on unrelated individuals. We then highlight how adding a dyadic perspective may advance our understanding of the complex interplay between functional limitations and depressive symptoms in old age.
Research using samples of unrelated individuals indicates that functional limitations and depressive symptoms may be associated for a number of different reasons, with the social context representing one key factor (Lenze et al., 2001). For example, functional limitations can restrict opportunities for social engagement and may therefore be associated with increased risks of developing depressive symptoms (Lenze et al., 2001; Roberts, Kaplan, Shema, & Strawbridge, 1997; Rowe & Kahn, 1997; Zeiss, Lewinsohn, Rohde, & Seeley, 1996). Alternatively, depressive symptoms can also lead to reduced social engagement which has been associated with increases in functional limitations (Bruce, Seeman, Merrill, & Blazer, 1994; Cronin-Stubbs et al., 2000; Lenze et al., 2001; Penninx et al., 1999). Hence, functional limitations and depressive symptoms seem to reciprocally influence each other. Regarding individual-level predictions, we therefore expect that increases in functional limitations over time will be accompanied by an increase in depressive symptoms and vice versa in older spouses from the AHEAD.
Recognizing the important role of social contextual factors for the interplay between functional limitations and depressive symptoms in old age requires that attention be paid to the specific characteristics of older adults’ proximal social context, particularly their close relationships such as marriage. The present study therefore moves beyond an investigation of individual-level associations in longitudinal functional limitation–depression trajectories towards an examination of the spousal dynamics that characterize the relationship between these two domains of functioning using longitudinal couple data from older spouses. We argue that older married couples are a unit of primary interest when examining the influence of social contextual factors on health trajectories in old age because older spouses are typically very close to each other, engage in many joint activities, and live in the same environment (Hoppmann, Gerstorf, & Luszcz, 2008; Lang, 2001; Meegan & Berg, 2002). Indeed, previous research using couple samples points to considerable spousal associations across a broad range of physical and mental health measures including chronic conditions, blood pressure, health behaviors, depressive symptoms, and happiness (Bookwala & Schulz, 1996; Hoppmann, Gerstorf, Willis, & Schaie, in press; Peek & Markides, 2003; Sandberg & Harper, 2000; Siegel et al., 2004; Stimpson, Peek, & Markides, 2006; Townsend et al., 2001). Based on previous work, we therefore expect that functional limitations and depressive symptoms are not only associated at a between-persons level among husbands and among wives, but also at a between-spouses level among partners.
Importantly, spousal associations in functional limitations and depressive symptoms can be a double-edged sword (for discussion, Hoppmann & Gerstorf, 2009). On the one hand, spouses may represent an important resource to each other during times of need, thereby compensating for the detrimental effects of functional limitations and depressive symptoms in the affected spouse (Berg & Upchurch, 2007; Berg et al., 2008). On the other hand, spouses can also make each other more vulnerable to the experience of physical and mental health problems (Lam et al., 2009; Townsend et al., 2001). Indeed, spouses are important sources of support when an older adult experiences functional limitations due to illness (Berg & Upchurch, 2007). Importantly, however, providing support to an ill or incapacitated spouse can be stressful and places emotional burdens on the support provider (Lyons, Zarit, Sayer, & Whitlatch, 2002; Schulz & Sherwood, 2008). We therefore expect that increases in functional limitations in one spouse are associated with an increase in depressive symptoms in the respective other spouse over and above the respective other spouse’s own functional limitations.
Alternatively, depressive symptoms in one spouse may also affect the respective other spouse and impact his or her physical health. Specifically, depressive symptoms may be associated with functional limitations of the respective spouse for at least two reasons. First, spousal depressive symptoms may lead to reduced social activity engagement in both members of the couple (Hoppmann et al., 2008). This is insofar important as social engagement (or lack thereof) seems to play a key role in linking depressive symptoms with functional limitations (Lenze et al., 2001). Second, depressed spouses may lack the energy to provide adequate support to their partners during times of need, thereby contributing to increased health problems (Benazon & Coyne, 2000). We therefore expect that increases in depressive symptoms in one spouse are associated with increases in functional limitations in the respective other spouse over and above the effects of the respective other spouse’s own depressive symptoms.
To provide a meaningful interpretation of the proposed spousal associations in functional limitation–depressive symptom trajectories, a number of other factors need to be considered. Specifically, our models account for the effects of individual (age, education, cognition) and spousal factors (length of marriage, number of children; Gerstorf, Hoppmann, Anstey, & Luszcz, 2009; Gerstorf, Hoppmann, Kadlec, & McArdle, 2009; Lenze et al., 2001). Because the two spouses in a given marriage are different from one another and should not be treated as indistinguishable, we use gender-specific models to test if the proposed associations are similar in women and men.
To our knowledge, no studies have addressed spousal associations in functional limitation depressive symptom trajectories in older couples using long-term longitudinal data from a national sample of old and very old spouses. We use latent growth models to examine if functional limitations and depressive symptoms are interrelated among wives, among husbands, and between spouses. We also control for a variety of individual and spousal covariates and explore gender-specific (a)-symmetries in the underlying associations.
Method
We applied a four-variable latent growth model (McArdle, 1988) to eight waves of 14.5-year longitudinal data (1993–2008) from initially 1,704 married couples in the AHEAD study. Below we present details of our study. Further information is published elsewhere (McArdle, Fisher, & Kadlec, 2007; Soldo, Hurd, Rodgers, & Wallace, 1997; Townsend et al., 2001).
Participants and Procedure
The AHEAD study started in 1993 with a probability sample of 8,222 non-institutionalized older adults aged 70 and older (i.e., born before 1924) in the US. If a household included more than one person born 1923 or earlier, one was randomly selected. If that person was married, the spouse was asked to participate as well (overall response rate: 74%). We included the 1,704 couples with data on the variables of interest in 1993 (90 % White). Relative to the remaining AHEAD sample, the couple subsample was younger (M = 74.18 years at baseline, SD = 6.38 vs. M = 78.03 years, SD = 6.69; F [1, 8,218] = 685.8, p < .001), reported fewer depressive symptoms (M = 1.29, SD = 1.77 vs. M = 1.99, SD = 2.13; F [1, 7,379] = 232.8, p < .001) and functional limitations (M = 1.50, SD = 1.86 vs. M = 2.38, SD = 2.34; F [1, 8,219] = 338.7, p < .001). They also had more years of schooling (M = 11.54, SD = 3.51 vs. M = 10.24, SD = 3.83; F [1, 8,218] = 243.0, p < .001), were cognitively fitter (M = 8.32, SD = 3.80 vs. M = 7.18, SD = 3.96; F [1, 7,192] = 153.8, p < .001), were married slightly longer (relative to other married AHEAD participants; M = 44.98, SD = 14.52 vs. M = 43.83, SD = 16.80; F [1, 4,570] = 4.49, p < .01), and had more children (M = 3.02, SD = 2.10 vs. M = 2.60, SD = 2.23; F [1, 8,187] = 79.0, p < .001) than other AHEAD participants.
Participants aged 70 to 79 years were interviewed via telephone and those aged 80+ years were interviewed in person (Herzog & Rodgers, 1988). We use couple data from eight waves spanning 14.5 years where both partners were together and had provided data for depressive symptoms and functional limitations: Baseline in 1993 (T1), 1995 (T2), 1998 (T3), 2000 (T4), 2002 (T5), 2004 (T6), 2006 (T7), and 2008 (T8). T2 occurred on average 1.98 years (SD = 0.29), T3 4.23 years (SD = 0.44), T4 6.31 years (SD = 0.47), T5 8.51 years (SD = 0.50), T6 10.45 years (SD = 0.51), T7 12.46 years (SD = 0.50), and T8 14.45 years (SD = 0.50) after T1. By T2, T3, T4, T5, T6, and T7, 6, 17, 26, 37, 45, and 54% had deceased; these mortality hazards are lower than in the residual sample (12, 27, 39, 51, 60, and 69%).
Measures
Depressive symptoms were indexed by a sum score across responses to eight items from the CES-D scale (Radloff, 1977). Participants indicated whether they had experienced the following eight symptoms “much of the time during the past week” (1) or not (0): Feeling depressed, everything was an effort, restless sleep, was (not) happy, felt lonely, (did not) enjoy life, felt sad, and could not get going. Positively valenced items were reverse coded. At all occasions, internal consistencies were good (α‘s from .73 to .84 for wives and .74 to .84 for husbands; see Townsend et al., 2001; Turvey, Carney, Arndt, Wallace, & Herzog, 1999).
Functional limitations were indexed by a sum score across responses to 10 items asking whether participants had any difficulty with the following instrumental activities of daily living: Using the phone, managing money, taking medications, shopping groceries, preparing hot meals, walking several blocks, climbing one flight of stairs, lifting or carrying 10 lbs of weight, picking up a dime, and pushing or pulling large objects. Internal consistencies were good (α‘s from .73 to .84 for wives and .74 to .83 for husbands; see Fonda & Herzog, 2004).
Covariates
Our models also included individual (age, education, memory) and spousal covariates (length of marriage, number of children) at baseline as time-invariant covariates. Education was measured as the number of school years. For episodic memory, we used a unit-weighted composite of performances on the immediate and delayed free recall tests. Internal consistencies were good (α‘s = 85 for both wives and husbands; see Brandt, Spencer, & Folstein, 1988; Ofstedal, Fisher, & Herzog, 2005).
Data preparation
We standardized the scores for depressive symptoms and physical limitations to a T metric (Mean = 50; SD = 10) using the T1 AHEAD couple sample as the reference (n = 3,408 participants). This transformation ensured a common metric across measures and maintained the psychometric properties of the scores and the longitudinal changes in means and variances. We did not apply any data imputation procedure. The average longitudinal interval was 4.19 years (SD = 4.11). In Table 1, we present means and standard deviations for the study variables, separately for wives and husbands. On average, participants were examined in their mid to late seventies and early eighties with an average 3.5-year age difference between wives and husbands, F (1, 1,703) = 637.6, p < .001. Relative to husbands, wives reported more depressive symptoms, F (1, 1,703) = 34.7, p < .001, and functional limitations, F (1, 1,703) = 12.1, p < .001, fewer school years, F (1, 1,703) = 19.8, p < .001, and performed better on memory, F (1, 1,634) = 174.1, p < .001.
Table 1.
Age at Assessment and Descriptive Statistics for Measures Used in the Present Study, Separately for Husbands and Wives
| Wives |
Husbands |
Spouses |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Age | Mean | SD | N | Age | Mean | SD | N | Mean | SD | |
| Functional Limitations | |||||||||||
| T1 | 1,704 | 72.40 | 50.54 | 9.99 | 1,704 | 75.96 | 49.46 | 9.98 | |||
| T2 | 1,283 | 73.94 | 52.01 | 10.78 | 1,283 | 77.45 | 50.64 | 10.63 | |||
| T3 | 933 | 75.69 | 52.67 | 11.51 | 933 | 78.94 | 51.24 | 11.18 | |||
| T4 | 711 | 76.95 | 52.77 | 11.32 | 711 | 80.48 | 51.75 | 11.28 | |||
| T5 | 500 | 78.76 | 53.31 | 11.87 | 500 | 82.25 | 52.03 | 11.25 | |||
| T6 | 372 | 80.38 | 53.86 | 11.90 | 372 | 83.80 | 54.15 | 12.35 | |||
| T7 | 259 | 81.96 | 56.07 | 12.32 | 259 | 85.15 | 55.42 | 13.93 | |||
| T8 | 180 | 83.66 | 56.82 | 11.96 | 180 | 86.95 | 54.60 | 13.23 | |||
| Depressive Symptoms | |||||||||||
| T1 | 1,704 | 72.40 | 50.89 | 10.66 | 1,704 | 75.96 | 49.11 | 9.21 | |||
| T2 | 1,283 | 73.94 | 49.97 | 10.39 | 1,283 | 77.45 | 48.21 | 8.76 | |||
| T3 | 933 | 75.69 | 52.09 | 10.60 | 933 | 78.94 | 50.06 | 9.32 | |||
| T4 | 711 | 76.95 | 51.80 | 11.06 | 711 | 80.48 | 49.63 | 8.80 | |||
| T5 | 500 | 78.76 | 51.74 | 10.51 | 500 | 82.25 | 49.45 | 9.37 | |||
| T6 | 372 | 80.38 | 50.77 | 10.10 | 372 | 83.80 | 49.84 | 9.32 | |||
| T7 | 259 | 81.96 | 51.25 | 10.32 | 259 | 85.15 | 49.64 | 10.13 | |||
| T8 | 180 | 83.66 | 51.10 | 10.35 | 180 | 86.95 | 48.78 | 8.11 | |||
| Individual covariates | |||||||||||
| Education T1 | 1,704 | 72.40 | 11.70 | 3.14 | 1,704 | 75.96 | 11.37 | 3.84 | |||
| Memory T1 | 1,704 | 72.40 | 4.55 | 1.93 | 1,704 | 75.96 | 3.80 | 1.78 | |||
| Spousal covariates | |||||||||||
| Length of marriage T1 | 1,682 | 44.98 | 14.52 | ||||||||
| Number children T1 | 1,704 | 3.02 | 2.10 | ||||||||
Note. Scores for functional limitations and depressive symptoms standardized to the T metric using the T1 AHEAD couple sample as the reference (n = 3,408 participants), Mean = 50, SD = 10.
Over and above mean-level changes, both variables also exhibited comparable stability over time at the level of between-person differences. Specifically, averaged autocorrelation coefficients between adjacent waves (calculated using Fisher’s z transformation) were r = .53 (range from r = .46 to r = .58) for depressive symptoms of wives and r = .54 (range from r = .47 to r = .70) for husbands, r = .70 (range from r = .62 to r = .75) for functional limitations of wives and r = .66 (range from r = .61 to r = .69, all p’s < .001) for husbands. At a given wave, average correlations between depressive symptoms and functional limitations were comparable across spouses, with r = .36 (range from r = .20 to r = .42) for wives and r = .40 (range from r = .34 to r = .48) for husbands. Spousal similarities at a given wave tended to be stronger for depressive symptoms (average correlation r = .26) as compared with functional limitations (average correlation r = .16), all p’s < .001.
Statistical Procedures
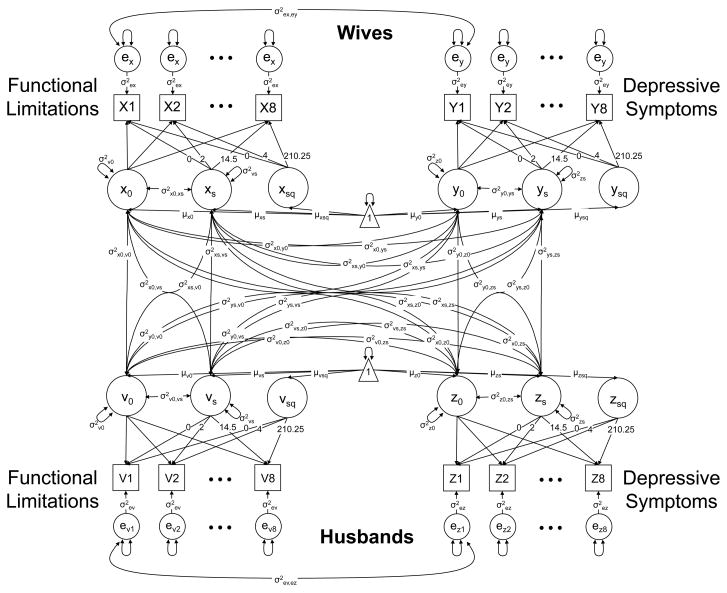
We used a four-variable latent growth curve model (LGM; (J. J. McArdle, 1988). As a straightforward extension of a univariate LGM, a four-variable LGM estimates fixed effects (average levels, linear slopes, and quadratic slopes) and random effects (between-person differences in levels and linear slopes). Figure 1 provides a graphical representation of the model. The repeated measures of wives and husbands have three sources: (a) the latent intercepts with loadings of 1 (x0, y0, v0, z0); (b) the latent slopes with linear loadings (xs, ys, vs, zs) and quadratic loadings (xsq, ysq, vsq, zsq); and (c) the residual terms (ex, ey, ev, ez). Intercepts, linear slopes, and quadratic slopes are estimated at the population level and both intercepts and linear slopes are allowed to vary and covary. Deviations for the quadratic slopeswere examined, but were not significant and thus not included in the final models. The residuals are assumed to be normally distributed with a mean of zero and a time-invariant variance, and are allowed to covary between measures from the same partner within time but not across time (ρex,ey).1
Figure 1.
A four-variable Latent Growth Curve Model (McArdle, 1988) as applied to 14.5-year longitudinal data from 1,704 couples in the Study of Asset and Health Dynamics Among the Oldest Old (AHEAD). Observed variables are presented by squares, latent variables by circles, regression weights by one-headed arrows, and (co-)variances by two-headed arrows. The triangle represents a constant indicating the means and intercepts. Unlabeled paths are set to 1.
Pairwise structuring of the data allowed us to treat the couple as the unit of analysis. In total, the model estimated 53 free parameters (four times seven parameters within each of the four time series, plus eight cross-variable intercorrelations among wives and among husbands, 16 cross-variable intercorrelations between wives and husbands, and one covariance of time-invariant residuals between measures from the same partner) as well as a total of 108 parameters for the eight covariates. We used all data points available using the full information maximum likelihood estimation algorithm, which allowed accommodating incomplete data under the missing at random assumption (Little & Rubin, 1987). We used the Mplus program version 4 (Muthén & Muthén, 1998–2006). We report results from a four-variable LGM with a particular focus on two sets of model parameters. First, we target between-person differences and examine if levels and changes in depressive symptoms and functional limitations are interrelated among wives and among husbands. Second, we target between-couple differences and explore if levels and changes in functional limitations and depressive symptoms are interrelated between spouses. In follow-up analyses we also examine if such between-person and between-couple differences are (a)-symmetrical between genders. To do so, we use statistically nested model comparisons of models that either freely estimate the respective parameters or set these invariant across spouses.
Results
We first used the intra-class correlation from random intercept-only models to establish between-person and within-person variation in the data. We found that between-person variance in depressive symptoms was .52 for wives and .49 for husbands, with the remainder (wives: 48%; husbands: 51%) being within-person variation. A highly similar pattern was found for functional limitations (within-person variation: 45% for wives and 53% for husbands). Noting that there were indeed substantial between-person differences and within-person changes over time to model, we proceeded to examine how these were structured and interrelated between spouses.
Between-Person Differences in Functional Limitation – Depressive Symptom Associations
Our four-variable LGM provided reasonably good fit to our data, CFI = .938; RMSEA = .025, and model parameters are presented in Table 2. Consistent with previous work (Liang et al., 2008; Mirowski & Ross, 1992), fixed effects indicate that the linear component of change amounted to more than half a standard deviation increase over 10 years for both measures and partners (e.g., depressive symptoms for wives: μs1 = 0.56; functional limitations for husbands: μs1 = 0.88, both p’s < .01). In addition, some curvature characterized the prototypical trajectories of change in functional limitations (e.g., husbands: μs2 = 0.05, p < .01), but not depressive symptoms (e.g., wives: μs2 = 0.01, p > .10). Again in line with extant reports of gender differences (Liang et al., 2008; Piccinelli & Wilkinson, 2000), statistically nested model comparisons revealed that, relative to husbands, wives reported more depressive symptoms (Δχ2/df = 34.6/1, p < .01) and more functional limitations (Δχ2/df = 34.5/1, p < .01). Gender differences in rates of linear change, however, were not reliable (Δχ2/df < 0.2/1, p > .10). Estimated average changes for both wives and husbands were sizeable (depressive symptoms: 0.75+ SD increase; functional limitations: 1.5+ SD increase).
Table 2.
Estimates of a Four-Variable Latent Growth Model for Depressive Symptoms and Functional Limitations of Husbands and Wives: Fixed Effects and Random Effects
| Wives |
Husbands |
|||||||
|---|---|---|---|---|---|---|---|---|
| Functional limitations |
Depressive symptoms |
Functional limitations |
Depressive symptoms |
|||||
| Estimate | SE | Estimate | SE | Estimate | SE | Estimate | SE | |
| Fixed effects | ||||||||
| Level μ0 | 51.72* | 0.27 | 50.94* | 0.28 | 49.51* | 0.27 | 48.98* | 0.25 |
| Linear slope μs1 | 0.87* | 0.08 | 0.56* | 0.08 | 0.88* | 0.08 | 0.58* | 0.07 |
| Quadratic slope μs2 | 0.03* | 0.01 | −0.01 | 0.01 | 0.05* | 0.01 | −0.00 | 0.01 |
| Random effects | ||||||||
| Variance level σ20 | 55.81* | 2.85 | 50.39* | 3.06 | 52.50* | 2.89 | 37.13* | 2.33 |
| Variance linear slope σ2s1 | 0.89* | 0.09 | 0.24* | 0.05 | 1.01* | 0.10 | 0.25* | 0.05 |
| Variance quadratic slope σ2s2 | – | – | – | – | – | – | – | – |
| Residual variance σ2e | 36.40* | 0.92 | 52.47* | 1.26 | 39.60* | 1.00 | 39.40* | 0.96 |
| Estimate | SE | Estimate | SE | |||||
| Residual covariance | 5.51* | 0.52 | 5.51* | 0.52 | ||||
Note. N couples = 1,704. Model includes age, education, and memory functioning of husbands and wives as well as the length of marriage and the number of children as covariates. Intercorrelations of factors are reported in Table 3. Scores for functional limitations and depressive symptoms standardized to the T metric using the T1 AHEAD couple sample as the reference (n = 3,408 participants), Mean = 50, SD = 10. Model fit: χ2 (df) = 1,426 (699); Comparative Fit Index, CFI = .938; root mean square error of approximation, RMSEA = .025.
p < .05 or below.
Of primary interest here, though, was the extent of between-person differences – as indicated by the variance components (random effects). We note that there was substantial variability for both measures and partners in levels (e.g., depressive symptoms for wives: σ20 = 50.39, p < .01) and linear changes (e.g., depressive symptoms for wives: σ2s1 = 0.24, p < .01). These results indicate that, for example, some wives and some husbands showed strong increases in depressive symptoms over time, whereas others showed only minor increases or remained stable. To target our first research question, we were interested in how between-person differences in one variable relate to between-person differences in the other variable.
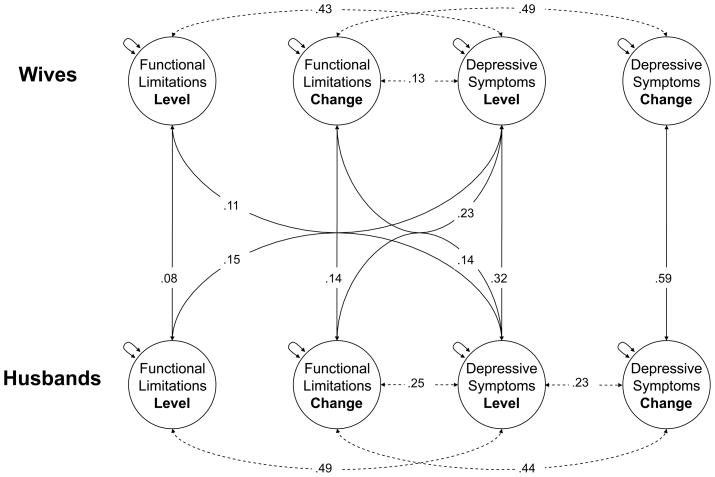
Statistically reliable cross-variable intercorrelations among wives and among husbands are represented by dotted lines in Figure 2. Non-significant intercorrelations at p < .01 were omitted for clarity. We found sizeable intercorrelations at the between-person level. Specifically, more functional limitations at baseline were related with more depressive symptoms at this occasion, both among wives (σ20 = .43) and among husbands (σ20 = .49). In a similar vein, increases in functional limitations over the 14.5 years were accompanied by increases in depressive symptoms among wives (σ20 = .49) and husbands (σ20 = .44). We also found that higher levels of depressive symptoms at baseline were associated with subsequently stronger increases in functional limitations among wives (σ20 = .13) and husbands (σ20 = .25). Nested model comparisons revealed that setting these model parameters invariant across genders did not result in reliable losses of model fit (level associations: Δχ2/df = 0.4/1; change associations:Δχ2/df = 0.1/1; associations between level of depressive symptoms and change in functional limitations: Δχ2/df = 2.3/1, all p’s > .10), indicating that they were similar across genders. In sum, our results corroborate previous between-person difference findings suggesting that levels and changes in depressive symptoms and functional limitations are closely intertwined.
Figure 2.
Intercorrelations obtained from a four-variable Latent Growth Curve Model of functional limitations and depressive symptoms of wives and husbands. Fixed effects and random effects are reported in Table 2. Dotted lines represent reliable cross-variable intercorrelations among wives and among husbands (targeting between-person differences). Solid lines represent reliable cross-variable intercorrelations between wives and husbands (targeting between-couple differences). Non-significant intercorrelations at p < .01 were omitted for clarity. Over and above substantial intercorrelations at the between-person level, results indicate considerable spousal associations at the between-couples level.
Between-Couple Differences in Functional Limitation Depressive Symptom Associations
Our second research question asks whether levels and changes in functional limitations and depressive symptoms also show substantial associations at the between-couples level. Figure 2 shows the statistically reliable cross-variable intercorrelations between wives and husbands by solid lines. Non-significant intercorrelations at p < .01 were again omitted for clarity. Results indicate that over and above substantial associations at the between-person level, considerable spousal interrelations emerged at the between-couples level.
Within domains, spousal associations were found for depressive symptoms and functional limitations both in terms of level and overall change. Specifically, reports of depressive symptoms for one partner were accompanied by reports of depressive symptoms for the other partner (σ20 = .32). Analogous though nominally weaker partner associations were found for the experience of functional limitations (σ20 = .08). Similarly, increases in depressive symptoms for one partner were accompanied by increases in depressive symptoms for the other partner (σ20 = .59). Again, analogous but somewhat weaker partner associations were found for the experience of functional limitations (σ20 = .14). Nested model comparisons revealed that spousal associations in levels of functioning were relatively stronger for depressive symptoms than for functional limitations (loss in model fit when setting level correlations to be of equal size: Δχ2/df = 19.8/1, p < .001), but not for time-related changes in functioning (loss in model fit when setting slope correlations to be of equal size: Δχ2/df = 0.1/1, p > .10).
Across-domains, we found a total of four reliable intercorrelations between depressive symptoms of one partner and functional limitations of the other partner. Specifically, more depressive symptoms of one partner were related with more functional limitations of the other partner (σ20 = .11 and σ20 = .15). In addition, more depressive symptoms of either partner related to more pronounced increases in functional limitations in the corresponding partner (σ20 = .23 and σ20 = .14). Nested model comparisons indicated that these associations were of comparable size between partners (Δχ2/df = 0.3/1 and Δχ2/df = 0.2/1, both p’s > .10). Our results illustrate that the spousal interrelations observed are of considerable size and appear to be as important as, if not more than, other domains of functioning at the between-person level. For example, the between-partner correlation between depressive symptom change of wives and that of husbands (σ20 = .59) was of comparable size to the between-person correlation between changes of husbands in depressive symptoms and in functional limitations (σ20 = .44). If anything, then nested model comparisons revealed that the dyadic association tended to be stronger (Δχ2/df = 5.4/1, p < .05).
We note that these models covaried for the effects of individual (age, education, memory) and spousal factors (length of marriage, number of children) 2. Although the covariates did not account for the substantive pattern of intercorrelations, they still contributed significant portions of overall explained variance to the model parameters (wives’ depressive symptoms level: R2 = .204, wives’ depressive symptoms change: R2 = .054, husbands’ depressive symptoms level: R2 = .159, and husbands’ depressive symptoms change: R2 = .171; wives’ functional limitations level: R2 = .197, wives’ functional limitations change: R2 = .226, husbands’ functional limitations level: R2 = .196, and husbands’ functional limitations change: R2 = .308).
Taken together, our analyses point to substantial between-person differences in levels and overall 14.5-year changes in functional limitations and depressive symptoms. Importantly, intercorrelations revealed that these differences were meaningfully interrelated between spouses with sizeable spousal similarities both within domains and across domains.
Discussion
This study extends previous research linking functional limitations and depressive symptoms by investigating if and how these two core domains of functioning are interrelated between spouses in old age. Using 14.5-year longitudinal data from 1,704 couples in the AHEAD study, we first corroborated previously documented associations between functional limitations and depressive symptoms among wives and among husbands. In addition, our findings also provide evidence for significant spousal associations within and across domains of functioning. Within domains, levels and changes over the 14.5-year study period in functional limitations and depressive symptoms were very similar between spouses with particularly strong spousal associations in depressive symptoms. Across domains, our findings indicate that depressive symptom levels in one spouse were positively associated with functional limitations levels and a subsequently stronger increase in functional limitations over time in the respective other spouse. We discuss our findings in the context of the social relationship and health literature and suggest further steps to substantiate our findings.
This study provides evidence that spouses play an important role in shaping functional limitation and depressive symptom trajectories in old age. Our findings suggest that sizeable portions of the well-documented between-person differences in functional limitations and depressive symptoms are in fact related to spouses. As such, this study significantly extends previous research on functional limitation- depressive symptom associations from samples of unrelated individuals (Everson-Rose et al., 2005; Kiecolt-Glaser & Newton, 2001; Lenze et al., 2001; Yang, 2006). Importantly, spouses did not only report similar baseline levels of functional limitations and depressive symptoms, but their functional limitations and depressive symptoms also waxed and waned together. This suggests that the spousal associations are not just a reflection of compositional effects in marriage (Kenny, Manetti, Pierro, Livi, & Kashy, 2002). Instead, they speak to dynamic social-interactive processes that unfold over time as spouses influence each other’s behaviors and feelings or as they are exposed to similar environments (Carstensen, Graff, Levenson, & Gottman, 1996; Kenny et al., 2002). As such, our findings add to a growing literature on spousal interrelations in physical and mental health and point to the need to extend individual-focused models of health and aging towards an inclusion of the social dynamics that characterize close relationships such as marriages (Lam et al., 2009; Siegel et al., 2004; Strawbridge et al., 2007; Townsend et al., 2001).
Importantly, spousal associations were more pronounced for depressive symptoms than for functional limitations. This finding could be due to two different mechanisms: First, the lifespan developmental literature and especially the theory of socio-emotional selectivity suggest that older spouses increasingly focus on the emotional climate in their relationship and become even closer to each other in old age than during earlier life phases (Carstensen et al., 1996; see also Antonucci, 2001; Baltes & Carstensen, 1999). Hence, there may be ample opportunities for emotion transmissions in late-life marriages that result in the observed spousal associations in depressive symptoms. Second, older spouses co-exist in the same environment and often share long relationship histories (Hoppmann & Gerstorf, 2009; Lang, 2001; Meegan & Berg, 2002). Thus, spouses may experience similar stressors (e.g., conflicts with children, financial problems) that impact emotional functioning, which may result in spousal associations in depressive symptoms (Carstensen et al., 1996).
Our findings also point to meaningful although less pronounced spousal associations in functional limitations. Importantly, these results are net of a variety of other potentially confounding factors that are known to be associated with functional limitations such as age or cognitive status. This finding might be interpreted as reflecting the cumulative effects of past health behaviors and lifestyles (e.g. regarding physical activity and eating habits), which tend to be associated between spouses (Stimpson et al., 2006; Weidner, Archer, Healy, & Matarazzo, 1985). In addition, spousal associations in functional limitations may also result from differences in resource status and living environments, such as the ability to afford paid services or the walkability of the neighborhood (Frank, Schmid, Sallis, Chapman, & Saelens, 2005). Future research should test such speculations about the role of lifestyle and environmental factors in moderating or mediating spousal associations in functional limitations.
In addition to within-domain spousal associations, we also found evidence for meaningful across-domain effects. Specifically, depressive symptom levels in one spouse were correlated with functional limitation levels and changes over time in the respective other spouse. One possible interpretation of this finding is that couples where one partner is emotionally challenged or experiences limitations in functional health are less likely to leave the house and engage in social activities, resulting in progressively less favorable physical and mental health in the other partner (Hoppmann et al., 2008; Lenze et al., 2001).
Interestingly, we did not find any gender differences in spousal associations, which contrasts with past findings that women are more emotionally reactive to their husband’s health problems than vice versa (Hagedoorn et al., 2001). We note, however, that we have corroborated well-documented mean-level differences in functional limitations and depressive symptoms between wives and husbands (Piccinelli & Wilkinson, 2000). We can only speculate about possible underlying mechanisms. First, the gender gap in depressive symptoms seems to be closing in very old age (Barefoot, Mortensen, Helms, Avlund, & Schroll, 2001). Gender differences in depressive symptom-associated processes may thus be less pronounced in old age as compared to earlier life phases. Second, in old age both spouses are likely going to experience some functional limitations. This may contribute to an increased awareness of their own vulnerability, thereby making both husbands and wives more vigilant of their partner’s physical health problems (Ilder & Benyamini, 1997). Finally, previously reported gender differences may also be sample-specific, with many studies using convenience samples high in resource status, and not be as evident in a national sample with a broader range of socio-economic backgrounds.
Limitations
Our report is unique in that it uses long-term longitudinal couple data from a national sample of old spouses. Our findings should be interpreted in light of the following potential limitations. Our model inferences are based on strict statistical assumptions (e.g., data missing at random) and need replication and extension using further methodologies (e.g., second-order or mixture models). For example, although this study is unique in providing insights into correlated changes in spousal functioning over time, it does not tell us anything about the directionality of these effects. Specifically, changes in functional limitations may precede changes in depressive symptoms or vice versa. As more waves of data are being collected, applications of “dynamic” modeling techniques (McArdle & Hamagami, 2001) may allow us to address such time-ordered associations in the future. Furthermore, this study did not use clinical assessments of functional limitations and depressive symptoms. Although the self-report measures of this study are widely used and well accepted, they do not provide a clinical diagnosis. We finally note that the couples in this study were married for more than four decades, on average. Hence, they represent the subset of couples who stayed together during good and also not so good times, potentially limiting the generalizability of our findings to younger cohorts.
Conclusions
This study shows that functional limitations and depressive symptoms are meaningfully associated between spouses. Our findings extend previous research by demonstrating the important role of marital relationships for shaping long-term physical and mental health trajectories in old age. Future research may substantiate these findings by going beyond a documentation of spousal associations in individual-level measures towards an examination of the underlying relationship-specific mechanisms. For example, it will be important to ask how spouses actively shape each other’s health trajectories through the setting and pursuit of goals. In addition, it would be intriguing to know how couples cope with chronic disease and how dyadic coping affects their mental and physical health (Berg et al., 2008; DeLongis & Holtzman, 2005). Finally, it would be key to know if spousal associations are specific to long-term married couples and if they generalize to the aging Baby Boomers who enter old age with much more diverse relationship histories (e.g., more often divorced and re-married) than prior cohorts of older adults. Taken together, our findings add to the literature by demonstrating that the social dynamics in marriage play an important role in shaping physical and mental health trajectories in old and very old age.
Acknowledgments
The AHEAD study was supported by a cooperative agreement (Grant No. UO1 AG09740) between the National Institute on Aging (NIA) and the University of Michigan.
Footnotes
In a preliminary step, we tested a series of models utilizing different structures for the residual variances. Relative to a less parsimonious model estimating different residual covariances for husbands and wives, we could set the residual covariances invariant across spouses without a reliable loss in model fit (Δχ2 = 1 per 1 df, p > .10). In another model, we set the covariance between the time series of depressive symptoms and physical limitations to 0; this model provided a worse description of the structure in our data set (Δχ2 = 114 per 1 df, p < .001). Finally, we estimated a non-nested model allowing the residuals be correlated between partners rather than measures; absolute model fit indices were less optimal (CFI = .934, RMSEA = .026) as compared with our model (CFI = .938, RMSEA = .025). Most importantly, these models revealed substantively the same pattern as reported in the main text.
In follow-up analyses, we included an indicator of physical activity of wives and husbands that was available at T2 as an additional covariate into our model. The item read as follows: “On average over the last 12 months have you participated in vigorous physical activity or exercise three times a week or more? By vigorous physical activity, we mean things like, sports, heavy housework, or a job that involves physical labor”. The item was answered as yes or no. The results obtained were virtually identical to those reported, with substantial spousal similarities in levels and changes across physical limitations and depressive symptoms.
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
References
- Antonucci . Social Relations- An examination of social networks, social support, and sense of control. In: Birren JE, Schaie KW, editors. Handbook of the Psychology of Aging. Vol. 5. London, UK: Academic Press; 2001. pp. 427–476. [Google Scholar]
- Baltes MM, Carstensen LL. Social-psychological theories and their applications to aging: From individual to collective. Psychological Concepts and Theories. 1999:209–226. [Google Scholar]
- Baltes PB, Smith J. New frontiers in the future of aging: From successful aging in the young old to the dilemmas of the fourth age. Gerontology. 2003;49:123–135. doi: 10.1159/000067946. [DOI] [PubMed] [Google Scholar]
- Barefoot JC, Mortensen EL, Helms MJ, Avlund K, Schroll M. A longitudinal study of gender differences in depressive symptoms from age 50 to 80. Psychology and Aging. 2001;16(2):342–345. doi: 10.1037//0882-7974.16.2.342. [DOI] [PubMed] [Google Scholar]
- Benazon NR, Coyne JC. Living with a depressed spouse. Journal of Family Psychology. 2000;14:71–79. [PubMed] [Google Scholar]
- Berg CA, Upchurch R. A developmental-contextual model of couples coping with chronic illness across the adult life span. Psychological Bulletin. 2007;133(6):920–954. doi: 10.1037/0033-2909.133.6.920. [DOI] [PubMed] [Google Scholar]
- Berg CA, Wiebe DJ, Butner J, Bradstreet C, Hayes J, Nail L, et al. Collaborative coping and daily mood in couples dealing with prostate cancer. Psychology and Aging. 2008;23(3):505–516. doi: 10.1037/a0012687. [DOI] [PubMed] [Google Scholar]
- Bookwala J, Schulz R. Spousal similarity in subjective well-being: The cardiovascular health study. Psychology and Aging. 1996;11(4):582–590. doi: 10.1037//0882-7974.11.4.582. [DOI] [PubMed] [Google Scholar]
- Brandt J, Spencer M, Folstein M. The telephone interview for cognitive status. Neuropsychiatry, Neuropsychology, and Behavioral Neurology. 1988;1:111–117. [Google Scholar]
- Bruce ML, Seeman TE, Merrill SS, Blazer DG. The impact of depressive symptomatology on physical disability: MacArthur Studies of Successful Aging. American Journal of Public Health. 1994;84(11):1796–1799. doi: 10.2105/ajph.84.11.1796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carstensen LL, Graff J, Levenson RW, Gottman JM. Affect in intimate relationships: The developmental course of marriage. In: Magai C, McFadden SH, editors. Handbook of emotion, adult development, and aging. San Diego: Academic Press; 1996. pp. 227–247. [Google Scholar]
- Cronin-Stubbs D, Mendes de Leon CF, Beckett LA, Field TS, Glynn RJ, Evans DA. Six year effect of depressive symptoms on the course of physical disability in community-living older adults. Archives of Internal Medicine. 2000;160:3074–3080. doi: 10.1001/archinte.160.20.3074. [DOI] [PubMed] [Google Scholar]
- DeLongis A, Holtzman S. Coping in context: The role of stress, social support, and personality in coping. Journal of Personality. 2005;73(6):1–24. doi: 10.1111/j.1467-6494.2005.00361.x. [DOI] [PubMed] [Google Scholar]
- Everson-Rose SA, Skarupski KA, Bienias JL, Wilson RS, Evans DA, Mendes de Leon CF. Do depressive symptoms predict declines in physical performance in an elderly, biracial population? Psychosomatic Medicine. 2005;67(4):609–615. doi: 10.1097/01.psy.0000170334.77508.35. [DOI] [PubMed] [Google Scholar]
- Fonda S, Herzog AR. HRS/AHEAD documentation report: Documentation of physical functioning measured in the health and retirement study and the asset and health dynamics among the oldest old study. 2004. [Google Scholar]
- Frank LD, Schmid TL, Sallis JF, Chapman J, Saelens BE. Linking objectively measured physical activity with objectively measured urban form: Findings from SMARTRAQ. American Journal of Preventative Medicine. 2005;28:117–125. doi: 10.1016/j.amepre.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Geerlings SW, Beekman AT, Deeg DJ, Twisk JW, Van Tilburg W. The longitudinal effect of depression on functional limitations and disability in older adults: an eight-wave prospective community-based study. Psychological Medicine. 2001;31(8):1361–1371. doi: 10.1017/s0033291701004639. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Hoppmann C, Anstey K, Luszcz M. Dynamic links of cognitive functioning among married couples: Longitudinal evidence from the Autralian Longitudinal Study of Aging. Psychology & Aging. 2009;24:296–309. doi: 10.1037/a0015069. [DOI] [PubMed] [Google Scholar]
- Gerstorf D, Hoppmann C, Kadlec K, McArdle J. Memory and depressive symptoms are dynamically linked among married couples: Longitudinal evidence from the AHEAD Study. Developmental Psychology. 2009;45:1595–1610. doi: 10.1037/a0016346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hagedoorn M, Sanderman R, Ranchor AV, Brilman EI, Kempen GIJM, Ormel J. Chronic disease in elderly couples: Are women more responsive to their spouses’ health condition than men? Journal of Psychosomatic Research. 2001;51:693–696. doi: 10.1016/s0022-3999(01)00279-3. [DOI] [PubMed] [Google Scholar]
- Herzog AR, Rodgers WL. Interviewing older adults: Mode comparison using data from a face-to-face survey and a telephone survey. Public Opinion Quarterly. 1988;52:84–99. [Google Scholar]
- Hoppmann C, Gerstorf D. Spousal interrelations in old age- A mini review. Gerontology. 2009;55(449):459. doi: 10.1159/000211948. [DOI] [PubMed] [Google Scholar]
- Hoppmann C, Gerstorf D, Willis S, Schaie KW. Spousal interrelations in happiness in the Seattle Longitudinal Study. Developmental Psychology. doi: 10.1037/a0020788. (in press) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoppmann CA, Gerstorf D, Luszcz M. On the interplay between spousal social activity trajectories in the Australian Longitudinal Study on Aging in the context of cognitive, physical, and emotional resources. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2008;63B:41–50. doi: 10.1093/geronb/63.1.p41. [DOI] [PubMed] [Google Scholar]
- Ilder EL, Benyamini Y. Self-rated health and mortality: A review of twenty-seven community studies. Journal of Health and Social Behavior. 1997;38:21–37. [PubMed] [Google Scholar]
- Kenny DA, Manetti L, Pierro A, Livi S, Kashy DA. The statistical analysis of data from small groups. Journal of Personality and Social Psychology. 2002;83:126–137. [PubMed] [Google Scholar]
- Kiecolt-Glaser JK, Newton TL. Marriage and health: His and hers. Psychological Bulletin. 2001;127:472–503. doi: 10.1037/0033-2909.127.4.472. [DOI] [PubMed] [Google Scholar]
- Lam M, Lehman AJ, Puterman E, DeLongis A. Spouse Depression and Disease Course among Persons Living with Rheumatoid Arthritis. Arthritis & Rheumatism. 2009;61:1011–1017. doi: 10.1002/art.24510. [DOI] [PubMed] [Google Scholar]
- Lang FR. Regulation of social relationships in later adulthood. The Journals of Gerontology. 2001;56B:P321–P326. doi: 10.1093/geronb/56.6.p321. [DOI] [PubMed] [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, et al. The association of late-life depression and anxiety with physical disability: a review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9(2):113–135. [PubMed] [Google Scholar]
- Liang J, Bennett JM, Shaw BA, Quinones AR, Ye W, Xu X, et al. Gender differences in functional status in middle and older age: Are there any age variations? Journal of Gerontology: Social Sciences. 2008;63B:S282–S292. doi: 10.1093/geronb/63.5.s282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical analysis with missing data. New York, NY: Wiley; 1987. [Google Scholar]
- Lyons KS, Zarit SH, Sayer AG, Whitlatch CJ. Caregiving as a dyadic process: Perspectives from caregiver and receiver. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2002;57B:195–204. doi: 10.1093/geronb/57.3.p195. [DOI] [PubMed] [Google Scholar]
- Manton KG, Corder L, Stallard E. Chronic disability trends in elderly United States populations: 1982–1994. Proceedings of the National Academy of Sciences of the United States of America. 1997;94(6):2593–2598. doi: 10.1073/pnas.94.6.2593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McArdle JJ. Dynamic but structural equation modeling of repeated measures data. In: Nesselroade JR, Cattell RB, editors. Handbook of multivariate experimental psychology. Vol. 2. New York: Plenum; 1988. pp. 561–614. [Google Scholar]
- McArdle JJ, Fisher GG, Kadlec KM. Latent variable analyses of age trends of cognition in the Health and Retirement Study, 1992–200. Psychology and Aging. 2007;22:535–545. doi: 10.1037/0882-7974.22.3.525. [DOI] [PubMed] [Google Scholar]
- McArdle JJ, Hamagami F. Linear dynamic analyses of incomplete longitudinal data. In: Collins, Sayer, editors. Methods for the analysis of change. Washington, DC: American Psychological Association; 2001. pp. 139–175. [Google Scholar]
- Meegan SP, Berg CA. Contexts, functions, forms, and processes of collaborative everyday problem solving in older adulthood. International Journal of Behavioral Development. 2002;26:6–15. [Google Scholar]
- Mirowski J, Ross CE. Age and depression. Journal of Health and Social Behavior. 1992;33:187–205. [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles: Muthén & Muthén; 1998–2006. [Google Scholar]
- Ofstedal MB, Fisher GG, Herzog AR. HRS/AHEAD documentation report: Documentation of cognitive functioning measures in the health and retirement study. 2005. [Google Scholar]
- Peek KM, Markides KS. Blood pressure concordance in older married Mexican-American couples. Ethnogeriatrics and special populations. 2003:51. doi: 10.1046/j.1532-5415.2003.51520.x. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Leveille S, Ferrucci L, van Eijk JT, Guralnik JM. Exploring the effect of depression on physical disability: longitudinal evidence from the established populations for epidemiologic studies of the elderly. American Journal of Public Health. 1999;89(9):1346–1352. doi: 10.2105/ajph.89.9.1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piccinelli M, Wilkinson G. Gender differences in depression. British Journal of Psychiatry. 2000;177:486–492. doi: 10.1192/bjp.177.6.486. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Roberts RE, Kaplan GA, Shema SJ, Strawbridge WJ. Does growing old increase the risk for depression? American Journal of Psychiatry. 1997;154(10):1384–1390. doi: 10.1176/ajp.154.10.1384. [DOI] [PubMed] [Google Scholar]
- Rowe JW, Kahn RL. Successful aging. The Gerontologist. 1997;37:433–440. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- Sandberg JG, Harper JM. In search of a marital distress model of depression in older marraiges. Aging and Mental Health. 2000;4(3):210–222. [Google Scholar]
- Schillerstrom JE, Royall DR, Palmer RF. Depression, disability and intermediate pathways: a review of longitudinal studies in elders. Journal of Geriatric Psychiatry & Neurology. 2008;21(3):183–197. doi: 10.1177/0891988708320971. [DOI] [PubMed] [Google Scholar]
- Schulz R, Sherwood PR. Physical and mental health effects of family caregiving. Journal of Nursing Research. 2008;108:23–27. doi: 10.1097/01.NAJ.0000336406.45248.4c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel MJ, Bradley EH, Gallo WT, Kasl SV. The effect of spousal mental and physical health on husbands’ and wives’ depressive symptoms, among older adults: longitudinal evidence from the Health and Retirement Survey. Journal of Aging & Health. 2004;16(3):398–425. doi: 10.1177/0898264304264208. [DOI] [PubMed] [Google Scholar]
- Soldo BJ, Hurd MD, Rodgers WL, Wallace RB. Asset and health dynamics among the oldest old: An overview of the AHEAD study. The Journals of Gerontology. 1997;52:1–20. doi: 10.1093/geronb/52b.special_issue.1. [DOI] [PubMed] [Google Scholar]
- Stimpson JP, Peek MK, Markides KS. Depression and mental health among older Mexican American spouses. Aging & Mental Health. 2006;10:386–393. doi: 10.1080/13607860500410060. [DOI] [PubMed] [Google Scholar]
- Strawbridge WJ, Wallhagen MI, Shema SJ. Impact of spouse vision impairment on partner health and well-being: A longitudinal analysis of couples. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 2007;62B(5):S315–S322. doi: 10.1093/geronb/62.5.s315. [DOI] [PubMed] [Google Scholar]
- Townsend AL, Miller B, Guo S. Depressive symptomatology in middle-aged and older married couples: A dyadic analysis. Journal of Gerontology: Social Sciences. 2001;56B(6):S352–S364. doi: 10.1093/geronb/56.6.s352. [DOI] [PubMed] [Google Scholar]
- Turvey CL, Carney C, Arndt S, Wallace RB, Herzog R. Conjugal loss and syndromal depression in a sample of elders aged 70 years or older. American Psychiatric Association. 1999;156:1596–1601. doi: 10.1176/ajp.156.10.1596. [DOI] [PubMed] [Google Scholar]
- Weidner G, Archer S, Healy B, Matarazzo JD. Family consumption of low fat foods: Stated preference versus actual consumption. Journal of Applied Social Psychology. 1985;15:773–779. [Google Scholar]
- Yang Y. How does functional disability affect depressive symptoms in late life? The role of perceived social support and psychological resources. Journal of Health & Social Behavior. 2006;47(4):355–372. doi: 10.1177/002214650604700404. [DOI] [PubMed] [Google Scholar]
- Zeiss AM, Lewinsohn PM, Rohde P, Seeley JR. Relationship of physical disease and functional impairment to depression in older people. Psychology & Aging. 1996;11(4):572–581. doi: 10.1037//0882-7974.11.4.572. [DOI] [PubMed] [Google Scholar]