This study provides evidence that decreased expression of the desmosomal cadherin desmocollin-2 enhances intestinal epithelial cell proliferation and promotes tumor formation via an Akt/β-catenin pathway.
Abstract
Desmocollin-2 (Dsc2) and desmoglein-2 (Dsg2) are transmembrane cell adhesion proteins of desmosomes. Reduced expression of Dsc2 has been reported in colorectal carcinomas, suggesting that Dsc2 may play a role in the development and/or progression of colorectal cancer. However, no studies have examined the mechanistic contribution of Dsc2 deficiency to tumorigenesis. Here we report that loss of Dsc2 promotes cell proliferation and enables tumor growth in vivo through the activation of Akt/β-catenin signaling. Inhibition of Akt prevented the increase in β-catenin–dependent transcription and proliferation following Dsc2 knockdown and attenuated the in vivo growth of Dsc2-deficient cells. Taken together, our results provide evidence that loss of Dsc2 contributes to the growth of colorectal cancer cells and highlight a novel mechanism by which the desmosomal cadherins regulate β-catenin signaling.
INTRODUCTION
Colorectal cancer is a leading cause of cancer morbidity and mortality worldwide (Jemal et al., 2008). In the United States alone, 160,000 people are diagnosed with colorectal cancer every year, and close to 60,000 of these patients will die from their disease (Markowitz and Bertagnolli, 2009). Colorectal cancer begins as a benign adenoma and progresses through the adenoma–carcinoma sequence to eventually acquire features of an invasive cancer with metastatic potential (Humphries and Wright, 2008). Numerous genetic changes occur throughout the evolution of the tumor; however, hyperactivation of the Wnt/β-catenin signaling pathway is largely regarded as the initiating event underlying colorectal cancer development, and sustained activation of β-catenin signaling is required for tumor progression (Oving and Clevers, 2002; Gavert and Ben-Ze’ev, 2007; Markowitz and Bertagnolli, 2009).
In the normal adult intestinal epithelium, Wnt/β-catenin signaling preserves the crypt stem cell population and drives epithelial cell proliferation, thereby contributing to epithelial cell renewal and the maintenance of tissue homeostasis (Pinto and Clevers, 2005). Central to the regulation of Wnt/β-catenin signaling is the control of the protein stability of β-catenin, the core effector molecule of this pathway. In the absence of the appropriate Wnt signals, β-catenin is targeted for degradation by a destruction protein complex—containing Axin, glycogen synthase kinase 3β (GSK-3β), and adenomatous polyposis coli (APC)—which binds to and phosphorylates the N-terminus of β-catenin, leading to its ubiquitination and degradation by the proteasome (Jin et al., 2008). Inhibition of the destruction complex allows the cytosolic accumulation and nuclear localization of β-catenin, where it cooperates with T-cell factor (TCF)/lymphoid enhancer factor family members to mediate the transcription of proproliferative genes (Clevers, 2006). The most common mutations in colorectal cancer inactivate the gene that encodes APC, leading to constitutive activation of Wnt/β-catenin signaling and hyperproliferation of cells. Other mutations include those in the N-terminal sequence of β-catenin, which interfere with the ability to phosphorylate and degrade the protein (Markowitz and Bertagnolli, 2009). In addition to Wnt signaling and regulation via the destruction complex, Wnt-independent mechanisms also modulate β-catenin–dependent transcription. Notably, regulation of β-catenin by the cadherin family of cell adhesion molecules has received significant attention in the field of tumor biology and, more recently, the PI3K/Akt signaling axis has been shown to promote β-catenin signaling and cell proliferation in mouse models of intestinal carcinogenesis and inflammation (He et al., 2004, 2007; Lee et al., 2010; Nava et al., 2010).
Classical cadherins such as E-cadherin and N-cadherin directly bind β-catenin, and this interaction is essential for their function as cell adhesion proteins (Nelson and Nusse, 2004). In addition, by associating with β-catenin, these proteins sequester β-catenin at the cell membrane and antagonize its transcriptional activity in colon cancer cells (Sadot et al., 1998; Gottardi et al., 2001; Stockinger et al., 2001). Down-regulation of E-cadherin has been shown to promote β-catenin/TCF transcription in a number of cancer cell types (Eger et al., 2000; Kuphal and Behrens, 2006), and this is one general mechanism by which loss of cell adhesion proteins is thought to contribute to tumor progression.
Desmosomal cadherins, consisting of desmocollin (Dsc 1–3) and desmoglein (Dsg 1–4) family members in humans, do not interact with β-catenin (Kowalczyk et al., 1994b; Wahl et al., 2000) but have been proposed to regulate β-catenin signaling through various mechanisms (Chen et al., 2002; Merritt et al., 2002; Hardman et al., 2005). However, in contrast to the extensively studied classical cadherins E- and N-cadherin, very little is known about the regulation of β-catenin signaling by the desmosomal cadherins and whether these proteins have a role in tumorigenesis (Chidgey and Dawson, 2007). In the human intestinal epithelium, only desmocollin-2 (Dsc2) and desmoglein-2 (Dsg2) are expressed (Holthofer et al., 2007). Recently, it has been reported that Dsc2 is down-regulated in colon carcinomas (Khan et al., 2006; Funakoshi et al., 2008), suggesting that loss of Dsc2 may contribute to colorectal cancer development and/or progression. However, complementary mechanistic studies are lacking.
Here we investigated the effect of Dsc2 down-regulation on the behavior of nontumorigenic, transformed colonic epithelial cells. For our studies, we used the colonic adenocarcinoma-derived SK-CO15 cell line (Anzano et al., 1989; Lisanti et al., 1989), which has constitutive activation of β-catenin/TCF signaling due to an APC mutation (Rowan et al., 2000) but retains features of a differentiated intestinal epithelium (growth as a monolayer, apical-basal polarity, and formation of intercellular adhesive junctions, including tight junctions, adherens junctions, and desmosomes) and has the added advantage of being amenable to transfection (Ivanov et al., 2007; Nava et al., 2007). Our results demonstrate that down-regulation of Dsc2 directly contributes to tumor progression and enables tumor cell growth in immunodeficient mice by promoting cell proliferation and transformation through the activation of Akt/β-catenin signaling. Collectively, these results highlight a previously unrecognized contribution of Dsc2 loss to the malignant transformation of intestinal epithelial cells and will help to reevaluate the role of the desmosomal cadherins in tumorigenesis and epithelial homeostasis.
RESULTS
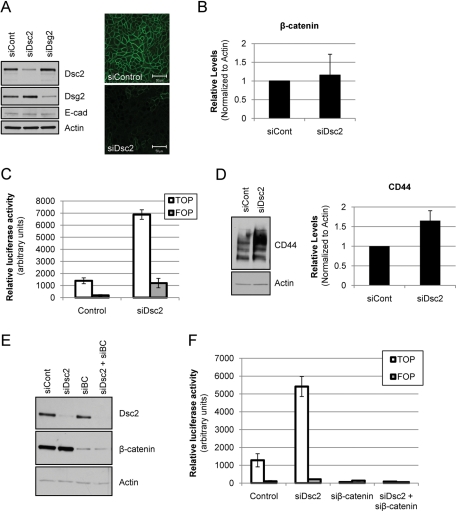
Loss of Dsc2 enhances β-catenin–dependent transcription in transformed colonic epithelial cell lines
Studies in stratified epithelia and cardiac muscle have implicated desmosomal proteins in the regulation of the transcriptional activity of β-catenin (Hardman et al., 2005; Garcia-Gras et al., 2006; Wang et al., 2007). To investigate whether Dsc2 influences β-catenin signaling in colonic epithelial cells, we down-regulated Dsc2 expression in SK-CO15 cells using RNA interference. Dsc2 down-regulation was confirmed by immunoblot analysis and immunofluorescence labeling/confocal microscopy (Figure 1A). Dsc2-specific small interfering RNA (siRNA) did not decrease the total protein levels of other cadherin superfamily members Dsg2 or E-cadherin (E-cad), thus demonstrating the specificity of the siRNA for Dsc2 (Figure 1A). To assess β-catenin following Dsc2 knockdown, we first examined total protein levels of β-catenin by immunoblotting. Dsc2 down-regulation did not significantly alter total levels of β-catenin (Figure 1B). However, because total protein levels of β-catenin do not necessarily correlate with its transcriptional activity, we also used a luciferase-based transcriptional reporter assay (TOP Flash) to measure β-catenin–dependent transcription in cells with decreased Dsc2 expression (Korinek et al., 1997). Cells were cotransfected with control or Dsc2-specific siRNA and the TOP reporter plasmid containing the β-catenin/TCF binding motifs. A parallel set of cotransfections was carried out using the FOP plasmid with mutated binding sites as a negative control. At 72 h after transfection, luciferase activity was assessed in control and Dsc2-deficient cells. As shown in Figure 1C, β-catenin/TCF signaling was significantly increased approximately fivefold in cells with decreased Dsc2 expression. Importantly, down-regulation of Dsc2 enhanced β-catenin transcriptional activity in other epithelial cell types, including the colonic epithelial cell line Caco-2 (Supplemental Figure 1), and in renal epithelial Madin-Darby canine kidney cells (unpublished data), demonstrating that this effect is not specific to the SK-CO15 cell line. To further verify increased β-catenin/TCF transcriptional activity, we analyzed the protein levels of β-catenin/TCF target genes, CD44 and cyclin D1 (Wielenga et al., 1999; Rimerman et al., 2000). In keeping with the reporter assay results, we observed up-regulation of CD44 (Figure 1D) and cyclin D1 (unpublished data). To confirm that the effects we observed in these cells were due to β-catenin, we utilized siRNA to down-regulate the expression of Dsc2, β-catenin, or both proteins (Figure 1E). Indeed, TOP Flash activity following Dsc2 down-regulation was completely inhibited by β-catenin knockdown (Figure 1F). These findings demonstrate that the increased β-catenin activity induced by Dsc2 knockdown was mediated by β-catenin and was not due to TOP Flash reporter activation by another catenin family member.
FIGURE 1:
Loss of Dsc2 leads to activation of β-catenin/TCF–dependent transcription without inducing accumulation of total β-catenin. (A) SK-CO15 cells were transfected with Dsc2-specific siRNA (siDsc2) in parallel with a nontargeting siRNA control. Knockdown of Dsc2 expression was confirmed by immunoblot (left panel) and immunofluorescence labeling/confocal microscopy (right panel; green, Dsc2; scale bar is 50 μm). Protein levels of other cadherin family members, E-cadherin (E-cad) and Dsg2, are not down-regulated following treatment with Dsc2 siRNA, demonstrating the specificity of the siRNA for Dsc2. (B) Protein extracts from control siRNA and Dsc2-specific, siRNA-transfected SK-CO15 cells were immunoblotted and probed with antibodies against β-catenin and actin and the expression levels quantified by densitometry. The graph represents mean ± SD from three independent experiments. (C) Luciferase-based reporter assay for β-catenin/TCF–dependent transcription (TOP Flash). SK-CO15 cells were cotransfected with control or Dsc2-specific siRNA and the β-catenin luciferase reporter plasmid (TOP) or a negative control plasmid (FOP). At 72 h posttransfection, luciferase activity was assessed. The results are representative of at least five independent experiments. (D) Immunoblot analysis of known β-catenin/TCF target, CD44, using an antibody that detects all variant forms; expression levels were quantified by densitometry. The graph represents mean ± SD from three independent experiments. (E) SK-CO15 cells were transfected with control, Dsc2 (siDsc2), β-catenin (siβ-catenin), or Dsc2 and β-catenin–specific siRNAs. Knockdown was confirmed by immunoblot using Dsc2 and β-catenin–specific antibodies. Actin is included as a loading control. (F) SK-CO15 cells transfected with the indicated siRNAs along with the TOP or FOP luciferase reporter plasmids, as described in (C).
Because Dsc2 down-regulation enhanced the transcriptional activity of β-catenin, we investigated whether β-catenin could be regulated through association with Dsc2 in a protein complex, as has been reported for the classical cadherins. Studies in keratinocytes and coimmunoprecipitation experiments with Dsc and Dsg have shown that β-catenin does not directly associate with desmosomal cadherins, although conflicting results have been reported (Bierkamp et al., 1999; Wahl et al., 2000). To our knowledge, no studies to date have examined the interaction of Dsc2 and β-catenin in intestinal epithelial cells, and to address this possibility, we first determined whether Dsc2 could coimmunoprecipitate with β-catenin in SK-CO15 cells. As shown in Supplemental Figure 2, B and C, coimmunoprecipitation experiments failed to reveal association of these proteins. To further verify this result, we expressed full-length Dsc2 protein in CHO cells, which express β-catenin but lack cadherin family members (Niessen and Gumbiner, 2002; Nava et al., 2007). Consistent with our results in SK-CO15 cells, immunoprecipitation experiments failed to reveal an association between Dsc2 and β-catenin (unpublished data). In contrast, exogenous expression of E-cadherin, which is known to interact directly with β-catenin, coimmunoprecipitated with β-catenin and induced β-catenin membrane localization in CHO cells (unpublished data). Thus these data are in agreement with published reports demonstrating that desmocollin does not associate with β-catenin in a protein complex (Kowalczyk et al., 1994a, 1996).
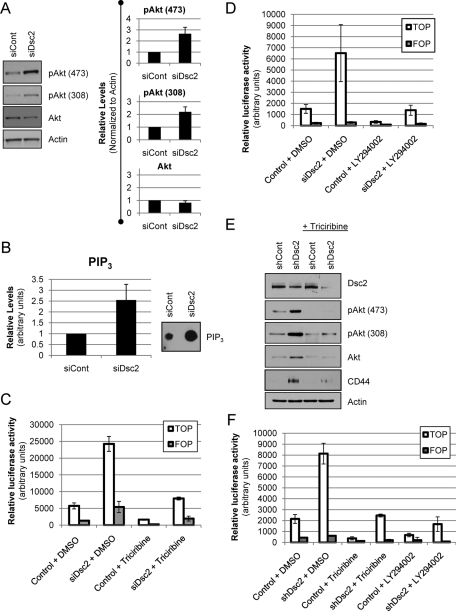
Down-regulation of Dsc2 induces β-catenin signaling through activation of Akt
Because we did not observe an interaction between Dsc2 and β-catenin, we explored other mechanisms by which Dsc2 loss could activate β-catenin signaling. It has been shown that the serine/threonine kinase Akt, also known as protein kinase B, can regulate β-catenin–dependent transcription either by inhibiting GSK-3β or by directly phosphorylating and activating β-catenin (Sharma et al., 2002; He et al., 2004, 2007; Tian et al., 2004; Fang et al., 2007). We therefore investigated whether Akt could mediate the effects of Dsc2 down-regulation on β-catenin signaling. Indeed, in cells with down-regulated Dsc2 expression we observed increased phosphorylation of Akt at Ser-473 and Thr-308, which is consistent with Akt activation (Figure 2A). Because the phosphorylation and activation of Akt depends on the generation of phosphatidylinositol-(3,4,5)-triphosphate (PIP3) in the inner cell membrane, we also examined the levels of PIP3 in control and siDsc2 knockdown cells. As shown in Figure 2B, PIP3 levels are consistently increased in Dsc2-deficient cells, in agreement with the observed increase in Akt activity. To further determine the contribution of Akt activation to increased β-catenin signaling, we utilized a specific Akt inhibitor, triciribine (API-2/Akt inhibitor V), and assessed its effect on β-catenin–dependent transcription (Yang et al., 2004; Koon et al., 2007). As shown in Figure 2C, treatment of cells with triciribine effectively reduced the activation of β-catenin/TCF signaling following Dsc2 down-regulation, as determined by the TOP Flash reporter assay (threefold decrease compared with dimethyl sulfoxide [DMSO] alone). Because active phosphoinositide 3-kinase (PI3K) catalyzes the formation of PIP3 and thereby promotes the activation of Akt, we next investigated the influence of PI3K inhibition on β-catenin–dependent transcription. Analogous to the results obtained with Akt inhibition, we observed that treatment of Dsc2 knockdown cells with a PI3K inhibitor, LY294002 (Vlahos et al., 1994), also reduced β-catenin transcriptional activity (Figure 2D; 4.7-fold decrease compared with DMSO alone). To confirm that Akt mediates the activation of β-catenin signaling in Dsc2-deficient cells, we performed knockdown experiments using specific siRNAs against Dsc2, Akt, or both proteins and examined the effects on β-catenin–dependent transcription (Supplemental Figure 3). Consistent with the results obtained using the Akt and PI3K inhibitors, targeted depletion of Akt also reduces the activation of β-catenin signaling following Dsc2 down-regulation. These results suggest that PI3K/Akt signaling contributes to increased β-catenin–dependent transcription in Dsc2-deficient cells.
FIGURE 2:
Inhibition of PI3K/Akt signaling reduces β-catenin activation following Dsc2 knockdown. (A) Western blot analysis of Akt activation status following Dsc2-specific siRNA treatment. Phospho-specific antibodies against phosphorylated Akt (Ser-473 or Thr-308) and total Akt were used and the expression levels quantified using densitometry. Graphs represent the mean ± standard error of the mean (SEM) from at least three independent experiments. (B) PIP3 content of control vs. siDsc2 knockdown cells. Total cellular PIP3 was isolated as described in Materials and Methods. The graph represents the densitometric quantification of two independent experiments; mean ± SD. (C) SK-CO15 cells were transfected with the indicated siRNAs along with the TOP or FOP luciferase reporter plasmids. At 12 h after transfection, the cells were treated with the Akt inhibitor triciribine or vehicle alone (DMSO). At 72 h posttransfection, luciferase activity was assessed. (D) SK-CO15 cells were transfected with the indicated siRNAs along with the TOP or FOP luciferase reporter plasmids. At 12 h after transfection, the cells were treated with the PI3K inhibitor LY294002 or vehicle alone (DMSO). At 72 h posttransfection, luciferase activity was assessed. (E) Cells stably expressing Dsc2-specific shRNA (shDsc2) or vector-alone control plasmid (control) were grown in the presence of triciribine or vehicle only (DMSO). Protein extracts from each condition were assayed for expression of the indicated proteins by immunoblot. Actin is included as a loading control. (F) Luciferase-based reporter assay for β-catenin/TCF–dependent transcription (TOP Flash) in control and shDsc2 cells. Cells were cotransfected with the β-catenin luciferase reporter plasmid (TOP) or a negative control plasmid (FOP). At 12 h after transfection, the cells were treated with the Akt inhibitor triciribine, PI3K inhibitor LY294002, or vehicle alone (DMSO). At 48 h posttransfection, luciferase activity was assessed.
Sustained down-regulation of Dsc2 activates Akt/β-catenin signaling
Transient down-regulation of Dsc2 allowed the characterization of signaling events and changes in cell behavior at short time periods following Dsc2 loss. To examine the long-term effects of Dsc2 down-regulation, we developed a stable cell line expressing short-hairpin RNA (shRNA) against Dsc2 (Supplemental Figure 4). Consistent with results obtained with transient Dsc2 knockdown, we observed a 3.5-fold increase in the level of β-catenin–dependent transcription, increased CD44 expression, and increased Akt activation (Supplemental Figure 4, C and D) in the stable Dsc2 knockdown cells (shDsc2). In addition, immunofluorescence analysis revealed a prominent nuclear localization of β-catenin in cells with decreased expression of Dsc2, consistent with enhanced activation of β-catenin signaling (Supplemental Figure 5A, arrows). To confirm that the increase in β-catenin signaling was dependent on Akt, we treated control and shDsc2 cells with the Akt inhibitor triciribine. As shown in Figure 2E, treatment with triciribine diminished the activation of Akt, as determined by immunoblot analysis of phosphorylated Akt (Ser-473 and Thr-308), and reduced the expression of the β-catenin/TCF target CD44 (Figure 2E). In addition, Akt inhibition resulted in decreased nuclear localization of β-catenin (Supplemental Figure 5A) and decreased β-catenin/TCF–dependent transcription in shDsc2 cells (Figure 2F). Furthermore, we observed that Akt inhibition enhanced the membrane staining of β-catenin in control cells, an effect that was not seen in shDsc2 knockdown cells (Supplemental Figure 5A). Taken together, these data support the conclusion that PI3K/Akt regulates β-catenin signaling in Dsc2-deficient cells.
Loss of Dsc2 promotes the nuclear localization of p(Ser-552)–β-catenin
Next we examined the mechanism by which Akt enhances the activity of β-catenin in Dsc2-deficient cells. As mentioned above, previous work has shown that Akt promotes β-catenin–dependent transcription by phosphorylating and inhibiting GSK-3β (Ser-9) and/or by activating β-catenin through direct phosphorylation at Ser-552. Therefore we assessed the phosphorylation status of these Akt target residues using phosphorylation site–specific antibodies. As shown in Supplemental Figure 5B, transient down-regulation of Dsc2 promoted the cytosolic and nuclear accumulation of p(Ser-552)–β-catenin. In addition, p(Ser-552)–β-catenin accumulated in the nucleus of stable Dsc2 knockdown cells, and this nuclear localization was inhibited by triciribine (Supplemental Figure 5C). Furthermore, we observed that loss of Dsc2 led to an increase in inactivated GSK-3β (pGSK-3β; Supplemental Figures 4D and 5D), which was reduced by treatment with triciribine. Interestingly, despite the Akt-mediated inhibition of GSK-3β, total levels of β-catenin were decreased in the stable Dsc2 knockdown cells compared with controls (Supplemental Figure 5D). Taken together, these results suggest that Akt enhances β-catenin signaling in Dsc2-deficient cells by promoting the nuclear localization of active β-catenin without inducing accumulation of the total protein level of β-catenin.
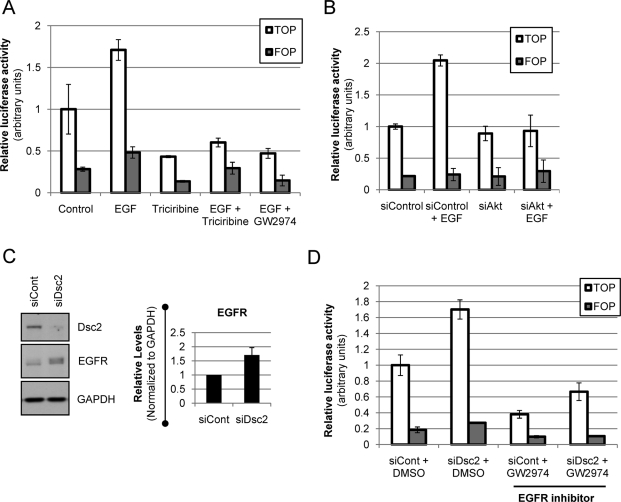
Enhanced activation of the epidermal growth factor receptor promotes Akt/β-catenin signaling in Dsc2-deficient cells
Given the observed effects of Dsc2 loss on the activation of PI3K/Akt signaling, we next sought to elucidate the mechanism by which Dsc2 regulates the activity of Akt. Previous studies have linked the desmosomal cadherins to the regulation of epidermal growth factor receptor (EGFR) signaling (Lorch et al., 2004; Getsios et al., 2009), a well-recognized activator of PI3K/Akt that has been shown to enhance the transcriptional activity of β-catenin (Lu et al., 2003; Hu and Li, 2010). Therefore we hypothesized that activation of EGFR may promote Akt/β-catenin signaling in Dsc2-deficient cells. To first examine whether EGFR activation could induce Akt/β-catenin signaling in SK-CO15 cells, we treated cells with EGF and assessed the effect on β-catenin–dependent transcription. Importantly, β-catenin signaling was increased in EGF-treated cells, an effect that was blocked by inhibition of EGFR using a specific inhibitor (GW2974) (Figure 3A). Importantly, similar results were observed following inhibition of PI3K (unpublished data) or Akt (Figure 3, A and B). Next we assessed the total levels of EGFR in Dsc2-deficient cells by immunoblotting. As shown in Figure 3C, down-regulation of Dsc2 consistently increased the total level of EGFR. Furthermore, inhibition of EGFR diminished the activation of β-catenin following Dsc2 knockdown (Figure 3D), recapitulating the effects of PI3K or Akt inhibition. Taken together, these data suggest that enhanced activation of EGFR promotes Akt/β-catenin signaling in Dsc2-deficient cells.
FIGURE 3:
Loss of Dsc2 induces Akt/β-catenin signaling through activation of the EGFR. (A) SK-CO15 cells were transfected with the TOP or FOP luciferase reporter plasmids. At 12 h after transfection, cells were pretreated with the Akt inhibitor triciribine, the EGFR inhibitor GW2974, or vehicle alone (DMSO) for 8 h before the addition of EGF. Luciferase activity was assessed 4 h post-EGF treatment. The graph is representative of three independent experiments. (B) SK-CO15 cells were transfected with the indicated siRNAs along with the TOP or FOP luciferase reporter plasmids. At 12 h after transfection, cells were treated with EGF, and luciferase activity was assessed 4 h posttreatment. The graph is representative of two independent experiments. (C) Protein extracts from control siRNA and Dsc2-specific siRNA-transfected SK-CO15 cells were immunoblotted and probed with antibodies against Dsc2, EGFR, and GAPDH and the expression levels quantified by densitometry. The graph represents mean ± SEM from three independent experiments. (D) SK-CO15 cells were transfected with the indicated siRNAs along with the TOP or FOP luciferase reporter plasmids. At 12 h after transfection, the cells were treated with the EGFR inhibitor GW2974 or vehicle alone (DMSO). At 48 h posttransfection, luciferase activity was assessed.
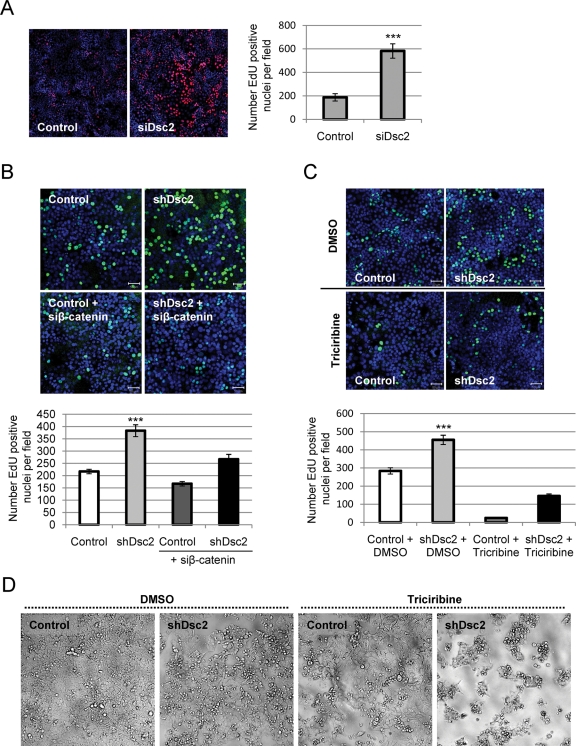
Dsc2 loss enhances cell proliferation through an EGFR/Akt/β-catenin–dependent mechanism
Because enhanced β-catenin activity is known to mediate epithelial proliferation (Hermiston et al., 1996; Wong et al., 1996), we next examined the effect of Dsc2 knockdown on cell proliferation. To assess proliferation, cells were transfected with control or Dsc2-specific siRNA and, 72 h after transfection, pulse-labeled for 1 h with a thymidine analogue 5-ethynyl-2′-deoxyuridine (EdU). As shown in Figure 4A, down-regulation of Dsc2 led to increased incorporation of EdU. This effect was also seen in cells with stable Dsc2 knockdown (unpublished data). Furthermore, simultaneous knockdown of β-catenin and Dsc2 prevented the increase in cell proliferation observed with Dsc2 down-regulation in stable (Figure 4B) and transient knockdowns (Supplemental Figure 6A). These findings further support a role of β-catenin in promoting cell proliferation following Dsc2 down-regulation.
FIGURE 4:
Dsc2 loss enhances cell proliferation through an Akt- and β-catenin–dependent mechanism. (A) SK-CO15 cells were transfected with Dsc2-specific siRNA (siDsc2) in parallel with a nontargeting siRNA control. At 72 h posttransfection, cells were pulse labeled with EdU for 1 h and processed to detect incorporated EdU. Images were obtained using confocal microscopy, and the number of EdU-positive nuclei was scored. The histogram shows the mean ± SEM of EdU-positive nuclei from at least 10 different fields (EdU, red; nuclei, blue) (***p < 0.0002, Student’s t test). (B) Stable shDsc2 knockdown and control cells were transfected with nontargeting or β-catenin–specific siRNA (siβ-catenin) and EdU incorporation assessed 48 h after transfection. Images were obtained using confocal microscopy, and the number of EdU-positive nuclei was scored. The histogram shows the mean ± SEM of the number of EdU-positive nuclei from at least 10 different fields (***p < 0.0001, analysis of variance [ANOVA]). (C) EdU incorporation assay for cells stably expressing Dsc2-specific shRNA (shDsc2) or vector-alone control plasmid (control) and grown in the presence of triciribine or vehicle only (DMSO). The histogram shows the mean ± SEM of EdU-positive nuclei from at least 10 different fields (***p< 0.0001, ANOVA). (D) Images obtained by light microscopy of control and shDsc2 knockdown cells treated for 96 h with triciribine or DMSO. The results are representative of at least three independent experiments.
Because inhibition of either EGFR or Akt signaling reduced the transcriptional activity of β-catenin, we next determined whether the same treatments could also prevent the increase in cell proliferation following Dsc2 knockdown. Control and Dsc2 knockdown cells were cultured for 2 d in the presence of triciribine, GW2974, or vehicle alone (DMSO), and EdU incorporation was used to measure the number of proliferating cells in each condition. Inhibition of either EGFR or Akt prevented the increase in cell proliferation following transient (unpublished data) and stable Dsc2 down-regulation (Akt inhibition, Figure 4C; EGFR inhibition, Supplemental Figure 6B). In addition, when cells were cultured for longer time periods (4–5 d) in the presence of triciribine, we observed that cells with reduced Dsc2 were more sensitive to Akt inhibition than their control counterparts. As shown in Figure 4D, shDsc2 knockdown cells no longer grew as adherent monolayers and large gaps were observed between cell colonies, suggesting that triciribine treatment induced cell detachment and/or death, an effect that was not observed in control cells. Taken together, these results suggest that Dsc2 regulates an EGFR/Akt/β-catenin signaling axis and that, in the absence of Dsc2, cell proliferation and/or survival is dependent on Akt/β-catenin signaling.
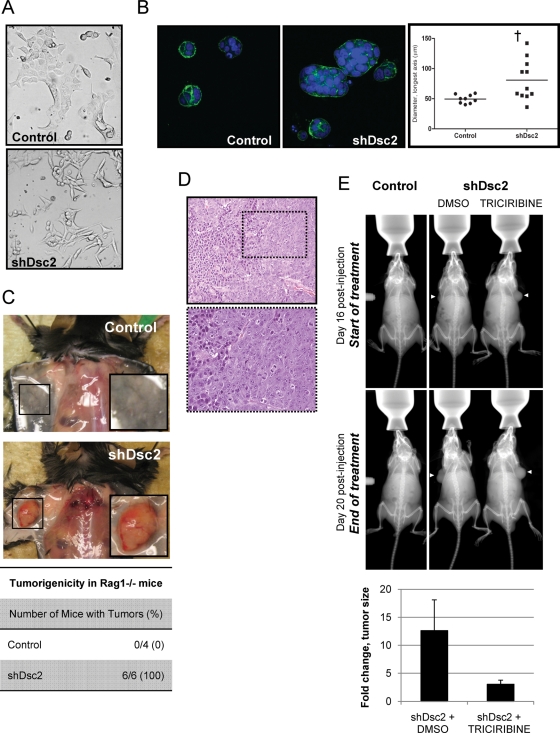
Down-regulation of Dsc2 promotes cell invasion and xenograft tumor formation in mice
In addition to enhancing cell proliferation, aberrant activation of β-catenin signaling is also thought to contribute to the transformation of colonic epithelial cells, enabling cells to eventually acquire an invasive phenotype (Behrens et al., 1993; Birchmeier et al., 1993; Shimizu et al., 1997). Consistent with the notion that Dsc2 loss enhances cell transformation, SK-CO15 cells stably expressing Dsc2 shRNA lacked the classical epithelial phenotype and were less cohesive than their Dsc2-expressing epithelial counterparts (Figure 5A). To analyze the invasive growth potential of cells lacking Dsc2, cells were cultured in a three-dimensional extracellular matrix. As shown in Figure 5B, shDsc2 knockdown cells grew as large cellular aggregates when compared with control cells, suggesting that loss of Dsc2 may confer invasive capabilities to nontumorigenic colonic epithelial cells.
FIGURE 5:
Down-regulation of Dsc2 promotes cellular transformation and enhances growth in vitro and in vivo. (A) Images obtained by light microscopy of control and shDsc2 knockdown cells plated at subconfluent densities. Note the altered cell morphology in Dsc2-deficient cells. (B) Control and Dsc2 stable knockdown clones were plated at equal density (10,000 cells per well) in a Matrigel matrix to assess three-dimensional growth. The Matrigel plugs were processed for immunofluorescence microscopy 72 h later. Images were collected from at least 10 fields per condition using a confocal microscope, and the size of each cell cluster was measured (actin, green; nuclei, blue) (†p < 0.05, Student’s t test). The results are representative of at least three independent experiments. (C) In vivo tumor growth for control vs. shDsc2 knockdown cells in Rag−/− mice. Mice were injected subcutaneously with 1 × 106 control or shDsc2 cells. Animals were killed on day 21, and the extent of tumor development was assessed macroscopically. (D) Microscopic analysis of shDsc2-derived tumors by hematoxylin and eosin analysis. (E) The effect of Akt inhibition on tumor growth in vivo. Using in vivo imaging, tumor size was recorded immediately before treatment with triciribine or vehicle alone and compared with final tumor size. The fold change in tumor size was then calculated. The graph represents the mean ± SD. Note the absence of tumors in mice injected with control, Dsc2-expressing cells. Images are representative of baseline and final tumor sizes in each treatment group. White arrows denote tumor location.
Given our in vitro findings that cells lacking Dsc2 exhibited features of invasive cells, we examined the in vivo tumorigenicity of control and shDsc2 knockdown cells using immunodeficient Rag1−/− mice. Mice were injected subcutaneously with 1 × 106 control or shDsc2 cells and monitored for tumor formation. At 3 wk postinjection, the mice were killed and tumor burden was assessed. As expected, mice injected with control cells did not develop tumors (Figure 5C, top). In contrast, large tumors grew in mice injected with cells lacking Dsc2 (Figure 5C, middle). On histologic examination, the shDsc2-derived growths showed evidence of tumor formation with characteristic features of a poorly differentiated carcinoma (Figure 5D). Thus these data support the hypothesis that loss of Dsc2 promotes tumor growth.
Our studies in vitro demonstrated that cells lacking Dsc2 are sensitive to Akt inhibition. To determine whether the in vivo growth of these cells was also dependent on Akt signaling, we assessed the effect of Akt inhibition on tumor growth in Rag1−/− mice. Mice were injected with control or shDsc2 cells (1 × 106) and monitored for tumor formation. At 16 d postinjection, palpable tumors were detected in all mice injected with shDsc2 cells, and no tumors were evident in mice injected with control SK-CO15 cells, supporting the findings highlighted in Figure 5, C and D. Tumor-bearing mice were then treated with the Akt inhibitor triciribine (1 mg/kg) or DMSO. After 5 d treatment, mice were killed and tumor burden and histology analyzed. To assess the effect of Akt inhibition on tumor size, in vivo images documenting tumor size were obtained immediately before treatment (Figure 5E, day 16) and compared with images obtained at the end of treatment (Figure 5E, day 20). Fold change in tumor size was then estimated by calculating the total tumor area using ImageJ analysis software. As seen in Figure 5E, Akt inhibition markedly reduced the in vivo growth of tumors derived from shDsc2 SK-CO15 cells. Taken together with the in vitro studies, our findings suggest that the increased proliferation and tumor growth following Dsc2 down-regulation is mediated by activation of Akt/β-catenin signaling.
DISCUSSION
In this study, we report that loss of the desmosomal cadherin Dsc2 confers a tumorigenic phenotype to transformed colonic epithelial cells. Our data demonstrate that decreased expression of Dsc2 enhances β-catenin signaling and promotes proliferation of colonic epithelial cells. Furthermore, loss of Dsc2 enables cells to grow as tumors in immunodeficient mice, a phenomenon that is not observed in parental cell lines. Importantly, our results also identify activated Akt as a key component driving β-catenin–dependent transcription in Dsc2-deficient cells. Taken together, these data provide the first mechanistic evidence that loss of Dsc2 may contribute to the malignant transformation of intestinal epithelial cells and demonstrate a novel mechanism to explain the regulation of β-catenin signaling by desmosomal cadherin family members.
Dsc2 is the only desmocollin expressed by simple epithelial tissues such as the colon. Dsc2 loss or down-regulation has been observed in sporadic and inflammation-associated colonic adenocarcinomas (Khan et al., 2006) and in highly tumorigenic colonic adenocarcinoma cell lines (Funakoshi et al., 2008). In support of these findings, we also have observed decreased Dsc2 protein expression and/or diffuse membrane localization in moderately and poorly differentiated colonic adenocarcinomas (Supplemental Figure 7). Dsc2 and Dsc3 proteins, which are both expressed in stratified epithelial tissues, are down-regulated or mislocalized in breast, skin, esophageal, and hepatocellular carcinomas (Kurzen et al., 2003; Oshiro et al., 2005; Cao et al., 2007; Fang et al., 2010). Decreased expression of Dsc3 in oral squamous cell carcinomas correlated with poor histological grade, lymph node metastasis, and altered localization of β-catenin (Wang et al., 2007), and Fang et al. (2010) recently reported similar prognostic correlations for Dsc2 loss in esophageal carcinomas. These data suggest that loss of Dsc proteins may contribute to tumor formation and/or progression; however, no study to date has examined whether Dsc has a direct role in tumorigenesis.
Here we report that down-regulation of Dsc2 in a colonic epithelial cell line increased the activation of β-catenin/TCF signaling, enhanced cell proliferation, and conferred tumorigenic capacity to SK-CO15 cells. These findings are in agreement with a large body of evidence that strongly implicates aberrant activation of β-catenin signaling in the development and progression of colorectal cancers (Munemitsu et al., 1995; Korinek et al., 1997; Morin et al., 1997). Importantly, increased activity of β-catenin/TCF transcription has been shown to drive cell proliferation by directly enhancing the expression of proproliferative target genes (Wong et al., 1996; 1998; Tetsu and McCormick, 1999; Rimerman et al., 2000), and activation of this pathway also contributes to cellular transformation and the acquisition of invasive properties (Behrens et al., 1993; Birchmeier et al., 1993; Shimizu et al., 1997). Interestingly, Dsc2-deficient colonic epithelial cells appear to share similar properties to those described for colon cancer stem cells (hyperproliferation, activation of Akt/β-catenin, expression of putative stem cell markers such as CD44, and tumorigenic capability). It is tempting to speculate that loss or low levels of Dsc2 may play an important role in the maintenance of colon cancer stem cells (Vermeulen et al., 2008, 2010).
Germline or acquired somatic mutations in proteins of the Wnt/β-catenin signaling pathway occur in the majority of colorectal cancers and interfere with β-catenin degradation (Fodde and Brabletz, 2007; Markowitz and Bertagnolli, 2009). However, Wnt-independent mechanisms are also known to regulate the activity of the β-catenin/TCF transcriptional complex, including regulation by cell adhesion proteins, such as E-cadherin (Hermiston et al., 1996; Jeanes et al., 2008), as well as regulation by the serine/threonine kinase Akt (He et al., 2004, 2007; Fang et al., 2007), which has recently emerged as an important regulator of β-catenin transcriptional activity in the intestine (Vermeulen et al., 2008; Brown et al., 2010; Lee et al., 2010; Nava et al., 2010).
As opposed to the extensively studied classical cadherin E-cadherin, the mechanism(s) by which the desmosomal cadherins regulate β-catenin signaling remain unclear. Unlike the findings on E-cadherin, our findings reveal that Dsc2 does not associate with β-catenin in colonic epithelial cells, indicating that activation of β-catenin is not due to “release” of this protein from a Dsc/β-catenin complex, as has been proposed for E-cadherin. Furthermore, the amount of β-catenin bound to E-cadherin does not appear to be altered in Dsc2-deficient cells (unpublished data), suggesting that the effects on β-catenin signaling are not due to changes in the interaction between E-cadherin and β-catenin. In addition, we have not detected a change in E-cadherin membrane localization by immunofluorescence/confocal imaging following Dsc2 down-regulation (unpublished data). The total levels of E-cadherin, as assessed by immunoblotting, are unchanged in transient knockdown cells (Figure 1A) and are modestly decreased (by ∼20%) in stable shDsc2-expressing cells (unpublished data), which mirrors the effects we observed for total β-catenin levels. At the present time, it is not clear why there is a difference between transient and stable Dsc2 knockdown cells; however, these results suggest that decreased expression of E-cadherin in SK-CO15 cells may be a longer term consequence of loss of Dsc2.
Studies in the epidermis have suggested that Dsc proteins may regulate β-catenin signaling indirectly through effects on plakoglobin, a catenin family member that interacts with Dscs and may “compete” with and displace β-catenin from E-cadherin when plakoglobin is in excess (Zhurinsky et al., 2000; Miravet et al., 2003; Hardman et al., 2005). However, simultaneous knockdown experiments in which Dsc2 and β-catenin or plakoglobin were down-regulated in SK-CO15 cells demonstrated that β-catenin but not plakoglobin knockdown completely abolished the activation of the β-catenin transcriptional reporter and reversed the proliferation phenotype of Dsc2-deficient cells (Figures 1F and 4B; unpublished data).
Instead we observed that loss of Dsc2 induced the activation of serine/threonine kinase Akt, which has been shown to positively regulate β-catenin signaling in a number of cell types, including intestinal epithelial cells. Akt has been proposed to enhance β-catenin–dependent transcription through direct phosphorylation and activation of β-catenin (Ser-552) or through the inhibition of GSK-3β (Ser-9), a signaling component that is shared with the Wnt/β-catenin pathway. In our study, activation of Akt in Dsc2-deficient cells was associated with an increase in the number of cells staining positively for phospho-β-catenin (Ser-552), an Akt phosphorylation site on β-catenin that is associated with enhanced β-catenin transcription (Fang et al., 2007; He et al., 2007). Furthermore, we observed an enrichment of phospho-β-catenin (Ser-552) in the nucleus of mitotic cells (unpublished data), a phenomenon that has been reported previously for β-catenin (Kaplan et al., 2004; Zhang et al., 2010). We also observed an increase in phosphorylation of the inhibitory Ser-9 residue of GSK-3β, which has been proposed to enhance β-catenin signaling by promoting the accumulation of β-catenin protein levels, in a manner analogous to Wnt-mediated GSK-3β inactivation (Desbois-Mouthon et al., 2001; Sharma et al., 2002; Naito et al., 2005; Mulholland et al., 2006). Interestingly, despite the inhibition of GSK-3β, we observed a decrease in the total levels of β-catenin in stable Dsc2 knockdown cells, suggesting that Akt-mediated GSK-3β inhibition may promote the nuclear redistribution of β-catenin and enhance β-catenin–dependent transcription without inducing stabilization of total β-catenin protein levels. These findings are in agreement with a number of reports suggesting that it is the nuclear localization of β-catenin, rather than the total protein levels, that indicates enhanced transcriptional activity of β-catenin (Miller and Moon, 1997; Gottardi and Gumbiner, 2004; Maher et al., 2010) and signify that in addition to GSK-3β, other cellular components (e.g., cell–cell adhesion complexes) likely also influence the total levels of β-catenin in cells. Furthermore, our results also suggest that inhibition of GSK-3β by Akt may enhance β-catenin signaling in a more distinct manner than Wnt-mediated GSK-3β inactivation, even though this component is shared by both Wnt/β-catenin and Akt/β-catenin pathways (see Figure 6). Of note, while numerous reports have demonstrated a clear role for Akt activation in the regulation of β-catenin–dependent transcription, PI3K/Akt does not enhance the transcriptional activity of β-catenin in all cell types, suggesting that Akt/β-catenin signaling may occur in a tissue- and/or context-dependent manner (Ng et al., 2009).
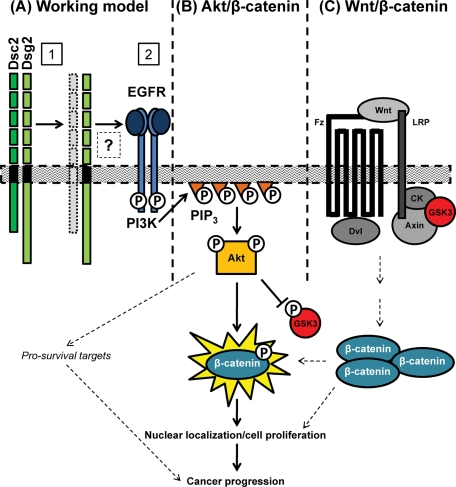
FIGURE 6:
Working model. Loss of Dsc2 promotes cellular transformation and proliferation through activation of the Akt/β-catenin signaling pathway. (A1) Down-regulation of Dsc2 leads to activation of the EGFR (A2) and PI3K/Akt-dependent activation of β-catenin/TCF transcription in colonic epithelial cells. Activation of this pathway leads to enhanced cell proliferation and tumor growth in vitro and in vivo. The contribution of Wnt/β-catenin signaling (C), “solitary” Dsg2, or the additional prosurvival targets of Akt that may enhance tumorigenicity of Dsc2-deficient cells have not been directly investigated in this study. (B) Akt/β-catenin signaling. Akt is recruited to PIP3-rich regions of the plasma membrane via its pleckstrin homology domain, where it is activated by phosphorylation at residues Ser-473 and Thr-308. Active Akt has been shown to enhance β-catenin signaling either by phosphorylation of GSK-3β at Ser-9 or by directly phosphorylating β-catenin at Ser-552. Note that GSK-3 is also part of the β-catenin destruction complex of the Wnt pathway. (C) Wnt/β-catenin signaling. In the absence of a Wnt signal, β-catenin is bound by the destruction complex and targeted for degradation (not depicted). In the presence of Wnt ligands, Wnt binds to the Frizzled (Fz) and LRP coreceptors, leading to the dissociation of the GSK-3–containing destruction complex from β-catenin and thereby promoting accumulation of β-catenin. Abbreviations: CK, casein kinase; Dvl, Dishevelled; EGFR, epidermal growth factor receptor; Fz, Frizzled; GSK-3, glycogen synthase kinase 3; LRP, low-density lipoprotein receptor–related protein.
Our data suggest that loss of Dsc2 may promote Akt/β-catenin signaling through the EGFR, which has been previously shown to regulate β-catenin–dependent transcription (Hu and Li, 2010). We find that EGFR protein levels are increased following Dsc2 down-regulation (Figure 3C) and that inhibition of EGFR diminishes the activation of β-catenin–dependent transcription and cell proliferation following Dsc2 knockdown (Figure 3D; Supplemental Figure 6B). Furthermore, treatment of SK-CO15 cells with EGF enhances β-catenin signaling, an effect that is diminished by treatment with EGFR, PI3K, and Akt inhibitors or by targeted depletion of Akt using siRNA (Figure 3, A and B). Thus EGFR activation by EGF recapitulates the effect of Dsc2 down-regulation on β-catenin–dependent transcription and strongly supports a role for EGFR in the activation of Akt/β-catenin signaling in Dsc2-deficient cells. These findings complement a recent report linking increased desmosomal cadherin expression to the suppression of EGFR signaling in a model of epidermal differentiation (Getsios et al., 2009).
Interestingly, activation of EGFR/Akt/β-catenin signaling appears to be specific to loss of Dsc2 rather than a general response to the disruption of desmosomal adhesion, as down-regulation of the related desmosomal cadherin Dsg2 does not appear to activate the same signaling cascade in SK-CO15 cells (unpublished data).
Finally, the mechanisms by which Dsc2 may be down-regulated in colorectal cancers are not well defined. Funakoshi et al. (2008) reported that loss of the intestine-specific homeobox transcription factor CDX2 correlated with loss of Dsc2 expression in colon cancer cell lines and that reexpression of CDX2 restored Dsc2 expression, suggesting that transcriptional regulation may lead to its down-regulation. In contrast, Khan et al. (2006) noted that loss of Dsc2 protein in colonic adenocarcinomas occurred without changes in mRNA levels, indicating changes in protein stability rather than transcriptional down-regulation. Furthermore, these authors found evidence of “Dsc switching” in colonic adenocarcinoma, as loss of Dsc2 was associated with increased expression of Dsc3. In our study, we found no evidence of Dsc3 protein or mRNA induction following down-regulation of Dsc2, suggesting that loss of Dsc2 is not sufficient to induce Dsc3 expression. Last, others have proposed that enhanced proteolytic cleavage of the extracellular domain of Dsc2 may contribute to its loss in transformed cells (Mathias et al., 2009). While these studies provide important insight, additional work is required to better characterize the mechanisms regulating changes in Dsc expression during tumorigenesis.
Based on the data from the current study, a hypothetical model to explain how loss of Dsc2 contributes to tumor formation and growth can be proposed (Figure 6A). In this model, down-regulation of Dsc2 induces the activation of the EGFR, which stimulates PI3K activity and enhances PIP3 levels. Akt is recruited to the membrane via interactions with PIP3 and is activated by phosphorylation. Activated Akt phosphorylates and inhibits GSK-3β and phosphorylates β-catenin directly, increasing the nuclear localization and transcriptional activity of β-catenin. Interestingly, our data suggest that loss of Dsc2 may lead to activation of Akt/β-catenin signaling through the presence of “solitary” (Schmitt et al., 2007) or excess Dsg2, which has been shown to activate Akt (Brennan et al., 2007; our unpublished data). Although not addressed in the work presented here, in addition to promoting β-catenin signaling and cell proliferation, active Akt also phosphorylates other downstream targets, which are known to promote the survival of tumor cells (dashed arrows). These prosurvival effects of Akt may also contribute to the enhanced tumorigenicity of Dsc2-deficient SK-CO15 cells by allowing the cells to “seed” a tumor in vivo.
In summary, this work defines a mechanistic role for Dsc2 in the progression of colorectal cancer and identifies Akt as a novel link between the desmosomal cadherins and β-catenin signaling.
MATERIALS AND METHODS
Cell culture and antibodies
The transformed human intestinal epithelial cell lines SK-CO15 and Caco-2 were grown in high glucose (4.5 g/l) DMEM supplemented with 10% fetal bovine serum, 100 U/ml penicillin, 100 mg/ml streptomycin, 15 mM HEPES (pH 7.4), 2 mM l-glutamine, and 1% nonessential amino acids as previously described (Ivanov et al., 2007). The following primary polyclonal antibodies (pAb) and monoclonal antibodies (mAb) were used to detect proteins by immunofluorescence labeling and/or Western blotting: anti-desmocollin 2/3 mAb, clone 7G6 (kind gift from K. Green, Northwestern University, Evanston, IL); anti-actin, tubulin, and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) pAbs (Sigma-Aldrich, St. Louis, MO); anti-desmoglein 2 mAb, clone AH12.2 (generated in-house); anti–E-cadherin mAb, clone HECD-1 (hybridoma supernatant; a generous gift from A.S. Yap, University of Queensland, Australia); anti–β-catenin mAb and anti-JAM-A pAb (Zymed Laboratories, South San Francisco, CA); anti-CD44 mAb, clone BBA10 (R&D Systems); pAkt (Ser-473), pAkt (Thr-308), pGSK-3β (Ser-9), and p-β-catenin (Ser-552) pAbs (Cell Signaling, Beverly, MA); anti-PML pAb (Abbiotec, San Diego, CA); anti-EGFR pAb (amino acids 961–972, ECM Biosciences, Versailles, KY); and Alexa 488–conjugated phalloidin (Invitrogen, Carlsbad, CA). Fluorophore-conjugated secondary antibodies were obtained from Invitrogen (Alexa Dye Series). Peroxidase-conjugated secondary antibodies were obtained from Jackson Laboratories (Bar Harbor, ME).
RNA interference reagents, transient transfection, and generation of stable cell lines
siGENOME SMARTpool siRNA for human Dsc2, β-catenin, E-cadherin, and nontargeting control were purchased from Dharmacon RNA Technologies (Lafayette, CO). Akt1- and Akt2-specific siRNAs were purchased from Sigma and shRNA against Dsc2 or empty vector was obtained from Open Biosystems (Huntsville, AL). SK-CO15 cells cultured to 60–70% confluence were transfected with the reagents at a final concentration of 20 nM by using Lipofectamine 2000 (Invitrogen). The cells were incubated for an additional 2–3 d after transfection to allow for sufficient knockdown of the target proteins. To generate stable cell lines, SK-CO15 cells were transfected with control (empty vector with puromycin resistance cassette) or a Dsc2-specific shRNA plasmid (also puromycin resistant) and grown in the presence of puromycin to select for transfected cells. Monoclonal cell populations were isolated by limiting dilution, and clones were chosen for further analysis based on the efficiency of Dsc2 down-regulation by immunoblot analysis. β-Catenin + Dsc2 knockdown was achieved by cotransfecting siRNA targets for β-catenin and Dsc2 together or β-catenin siRNA in the shRNA Dsc2 stable cell line. Akt knockdown studies were performed using a combination of siRNAs targeting both Akt1 and Akt2 isoforms, which are the two major Akt isoforms expressed in colonic epithelial cells, including the SK-CO15 cell line (unpublished observations). Confluent epithelial cultures were analyzed. Each experiment was performed at least three times.
Akt, PI3K, and EGFR inhibitors
AKT inhibition was achieved using the AKT inhibitor (final 10 μM), triciribine (Inhibitor V, 35943-35-2; Calbiochem, Darmstadt, Germany) (Yang et al., 2004; Cheng et al., 2005), or the PI3K inhibitor LY294002 (final 20 μM) (L9908; Sigma-Aldrich). EGFR inhibition was achieved using the specific inhibitor GW2974 (final 2.5 μM) (Sigma-Aldrich). Briefly, after Dsc2 knockdown, medium was replaced with DMEM containing 1% fetal calf serum (FCS) with vehicle alone (DMSO) or the inhibitor and cells were maintained for an additional 12–48 h before processing and analysis.
Immunoblotting
Confluent monolayers were washed two times with Hank’s balanced salt solution+ (HBSS+) on ice and collected in lysis buffer (20 mM Tris, 50 mM NaCl, 2 mM EDTA, 2 mM EGTA, 1% sodium deoxycholate, 1% Triton X-100, and 0.1% SDS, pH 7.4), containing a proteinase inhibitor cocktail (1:100, Sigma). Lysates were then cleared by centrifugation (30 min at 140,000 × g) and immediately boiled in SDS sample buffer. Gel electrophoresis and immunoblotting were conducted by standard methods with 10–20 mg protein per lane.
Immunofluorescence microscopy
Confluent monolayers were fixed/permeabilized in 3.7% paraformaldehyde (10 min at room temperature [RT]) followed by 0.5% Triton X-100 in HBSS+ (30 min at RT) or in ice-cold absolute ethanol (20 min at –20°C). Frozen sections (6 mm) of normal human colonic mucosa were fixed in absolute ethanol. Nonspecific protein binding was blocked in 3% bovine serum albumin in HBSS+ (1 h at RT), incubated with primary antibodies (1 h at RT), washed in HBSS+, and subsequently labeled with secondary antibodies (1 h at RT). Nuclei were stained using To-Pro3-iodide (Invitrogen) in HBSS+ (10 min at RT). Monolayers were mounted in 1:1:0.01 (vol/vol/vol) phosphate-buffered saline (PBS):glycerol:p-phenylenediamine, and they were visualized on a Zeiss LSM 510 Meta Confocal microscope (Carl Zeiss Microimaging, Thornwood, NY).
β-Catenin/TCF transcriptional reporter assay (TOP Flash)
In vitro activation of β-catenin was assessed using the optimized reporter kit for β-catenin/TCF (Upstate Biotechnology, Charlottesville, VA). Briefly, SK-CO15 or Caco-2 cells were trypsinized and plated (60,000 cells/well) in 48-well plates. At 12 h after plating, cells were transfected with the reporter plasmid pTOPGlow (TOP) or the negative control pFOPGlow (FOP) along with TK Renilla (50:1 ratio) as an internal control. After 12 h, media was replaced with DMEM complemented with 1% FCS (time 0). TOP/FOP activities were measured with the Dual Luciferase Reporter Assay System (Promega, Madison, WI) at 48 h after transfection in the GloMax 96 Luminometer (Cat. no. E6511 and E6521) and normalized to Renilla to control for transfection efficiency. For EGF studies, cells were treated with 100 ng/ml EGF (BD Biosciences, MA), and luciferase activity was assessed 4–6 h posttreatment.
PIP3 isolation and detection
PIP3 levels were determined using the commercially available PIP3 Mass Strip Kit from Echelon Biosciences (Salt Lake City, UT).
Nuclear and cytosolic cellular fractionation
Cytosolic and nuclear fractions of SK-CO15 cells were isolated using the commercially available NE-PER Nuclear and Cytoplasmic Extraction Reagents from ThermoScientific (Rockford, IL), following the manufacturer’s protocol.
EdU incorporation assay
Cells were grown to confluence on glass coverslips and pulse labeled with EdU (10 nM) for 1 h. Processing was carried out as described by the manufacturer (Invitrogen, Click-iT EdU). Nuclei were counterstained with TOPRO, mounted in standard mounting media, and imaged by fluorescence microscopy.
3-Dimensional growth in Matrigel invasion assay
Cells were plated at equal density (10,000 per well) in matrix solution (Matrigel; BD Biosciences, Franklin Lakes, NJ) and incubated at 37°C. At 72 h after plating, Matrigel plugs were washed, fixed with 3.7% formaldehyde, and permeabilized with 5% Triton X-100. Plugs were then processed for imaging by immunofluorescent labeling/confocal microscopy.
Tumor formation in Rag1−/− mice
Rag1 homozygous knockout mice were used to assay tumorigenicity in vivo. Control or shDsc2-expressing cells were grown to logarithmic growth phase, harvested, washed, and resuspended in PBS for injection. Each cell line (1 × 106 cells in 150 μl PBS) was injected subcutaneously into the dorsum of Rag1−/− mice. Tumor formation was monitored daily. All mice were killed at 3 wk, and tumors were immediately isolated and analyzed. For Akt inhibition studies, the Akt inhibitor triciribine (1 mg/kg) or DMSO was administered daily via intraperitoneal injection for the indicated time. After treatment, all mice were killed and tumors were isolated and processed for histology. All animal experiments were performed in accordance with protocols approved by the Emory University School of Medicine Institutional Review Board.
In vivo imaging
Images documenting tumor growth were obtained using the Kodak In-Vivo Multispectral System FX.
Statistics
Statistical analysis was carried out using GraphPad PRISM software.
Supplementary Material
Acknowledgments
The authors thank K. Green (Northwestern University) for providing Dsc2 antibody 7G6; S.P. Monga (University of Pittsburgh) for the TOP, FOP, and Renilla plasmids; L. Li (Stowers Institute) for providing phospho-β-catenin (Ser-552) antibody; and S. Voss and P. Goodson (Emory University) for expert technical assistance. This work was supported by a Crohn’s and Colitis Foundation of America Fellowship Award (P.N.), an AGA Foundation for Digestive Health and Nutrition Research Scholar Award (P.N.), and National Institutes of Health grants DK-61739 (C.P.), DK-55679 (A.N.), and DK-59888 (A.N.).
Abbreviations used:
- APC
adenomatous polyposis coli
- DMSO
dimethyl sulfoxide
- Dsc2
desmocollin-2
- Dsg2
desmoglein-2
- EdU
5-ethynyl-2′-deoxyuridine
- EGFR
epidermal growth factor receptor
- FCS
fetal calf serum
- GAPDH
glyceraldehyde-3-phosphate dehydrogenase
- GSK-3β
glycogen synthase kinase 3β
- HBSS
Hank’s balanced salt solution
- mAb
monoclonal antibody
- pAb
polyclonal antibody
- PBS
phosphate-buffered saline
- PI3K
phosphoinositide 3-kinase
- PIP3
phosphatidylinositol-(3,4,5)-triphosphate
- RT
room temperature
- SEM
standard error of the mean
- shRNA
short-hairpin RNA
- siRNA
small interfering RNA
- TCF
T-cell factor
Footnotes
This article was published online ahead of print in MBoC in Press (http://www.molbiolcell.org/cgi/doi/10.1091/mbc.E10-10-0845) on February 16, 2011.
The authors have no competing financial interests in relation to the work described herein.
REFERENCES
- Anzano MA, Rieman D, Prichett W, Bowen-Pope DF, Greig R. Growth factor production by human colon carcinoma cell lines. Cancer Res. 1989;49:2898–2904. [PubMed] [Google Scholar]
- Behrens J, Vakaet L, Friis R, Winterhager E, Van Roy F, Mareel MM, Birchmeier W. Loss of epithelial differentiation and gain of invasiveness correlates with tyrosine phosphorylation of the E-cadherin/beta-catenin complex in cells transformed with a temperature-sensitive v-SRC gene. J Cell Biol. 1993;120:757–766. doi: 10.1083/jcb.120.3.757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bierkamp C, Schwarz H, Huber O, Kemler R. Desmosomal localization of beta-catenin in the skin of plakoglobin null-mutant mice. Development. 1999;126:371–381. doi: 10.1242/dev.126.2.371. [DOI] [PubMed] [Google Scholar]
- Birchmeier W, Weidner KM, Behrens J. Molecular mechanisms leading to loss of differentiation and gain of invasiveness in epithelial cells. J Cell Sci Suppl. 1993;17:159–164. doi: 10.1242/jcs.1993.supplement_17.23. [DOI] [PubMed] [Google Scholar]
- Brennan D, Hu Y, Joubeh S, Choi YW, Whitaker-Menezes D, O’Brien T, Uitto J, Rodeck U, Mahoney MG. Suprabasal Dsg2 expression in transgenic mouse skin confers a hyperproliferative and apoptosis-resistant phenotype to keratinocytes. J Cell Sci. 2007;120:758–771. doi: 10.1242/jcs.03392. [DOI] [PubMed] [Google Scholar]
- Brown JB, et al. Mesalamine inhibits epithelial beta-catenin activation in chronic ulcerative colitis. Gastroenterol 138. 2010;605:e1–e3. doi: 10.1053/j.gastro.2009.10.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cao Y, Chang H, Li L, Cheng RC, Fan XN. Alteration of adhesion molecule expression and cellular polarity in hepatocellular carcinoma. Histopathol. 2007;51:528–538. doi: 10.1111/j.1365-2559.2007.02820.x. [DOI] [PubMed] [Google Scholar]
- Chen X, Bonne S, Hatzfeld M, van Roy F, Green KJ. Protein binding and functional characterization of plakophilin 2. Evidence for its diverse roles in desmosomes and beta-catenin signaling. J Biol Chem. 2002;277:10512–10522. doi: 10.1074/jbc.M108765200. [DOI] [PubMed] [Google Scholar]
- Cheng JQ, Lindsley CW, Cheng GZ, Yang H, Nicosia SV. The Akt/PKB pathway: molecular target for cancer drug discovery. Oncogene. 2005;24:7482–7492. doi: 10.1038/sj.onc.1209088. [DOI] [PubMed] [Google Scholar]
- Chidgey M, Dawson C. Desmosomes: a role in cancer? Br J Cancer. 2007;96:1783–1787. doi: 10.1038/sj.bjc.6603808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clevers H. Wnt/beta-catenin signaling in development and disease. Cell. 2006;127:469–480. doi: 10.1016/j.cell.2006.10.018. [DOI] [PubMed] [Google Scholar]
- Desbois-Mouthon C, Cadoret A, Blivet-Van Eggelpoel MJ, Bertrand F, Cherqui G, Perret C, Capeau J. Insulin and IGF-1 stimulate the beta-catenin pathway through two signalling cascades involving GSK-3beta inhibition and Ras activation. Oncogene. 2001;20:252–259. doi: 10.1038/sj.onc.1204064. [DOI] [PubMed] [Google Scholar]
- Eger A, Stockinger A, Schaffhauser B, Beug H, Foisner R. Epithelial mesenchymal transition by c-Fos estrogen receptor activation involves nuclear translocation of beta-catenin and upregulation of beta-catenin/lymphoid enhancer binding factor-1 transcriptional activity. J Cell Biol. 2000;148:173–188. doi: 10.1083/jcb.148.1.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang D, Hawke D, Zheng Y, Xia Y, Meisenhelder J, Nika H, Mills GB, Kobayashi R, Hunter T, Lu Z. Phosphorylation of beta-catenin by AKT promotes beta-catenin transcriptional activity. J Biol Chem. 2007;282:11221–11229. doi: 10.1074/jbc.M611871200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang WK, et al. Reduced membranous and ectopic cytoplasmic expression of DSC2 in esophageal squamous cell carcinoma: an independent prognostic factor. Hum Pathol. 2010;41:1456–1465. doi: 10.1016/j.humpath.2010.04.003. [DOI] [PubMed] [Google Scholar]
- Fodde R, Brabletz T. Wnt/beta-catenin signaling in cancer stemness and malignant behavior. Curr Opin Cell Biol. 2007;19:150–158. doi: 10.1016/j.ceb.2007.02.007. [DOI] [PubMed] [Google Scholar]
- Funakoshi S, Ezaki T, Kong J, Guo RJ, Lynch JP. Repression of the desmocollin 2 gene expression in human colon cancer cells is relieved by the homeodomain transcription factors Cdx1 and Cdx2. Mol Cancer Res. 2008;6:1478–1490. doi: 10.1158/1541-7786.MCR-07-2161. [DOI] [PubMed] [Google Scholar]
- Garcia-Gras E, Lombardi R, Giocondo MJ, Willerson JT, Schneider MD, Khoury DS, Marian AJ. Suppression of canonical Wnt/beta-catenin signaling by nuclear plakoglobin recapitulates phenotype of arrhythmogenic right ventricular cardiomyopathy. J Clin Invest. 2006;116:2012–2021. doi: 10.1172/JCI27751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gavert N, Ben-Ze’ev A. Beta-catenin signaling in biological control and cancer. J Cell Biochem. 2007;102:820–828. doi: 10.1002/jcb.21505. [DOI] [PubMed] [Google Scholar]
- Getsios S, Simpson CL, Kojima S, Harmon R, Sheu LJ, Dusek RL, Cornwell M, Green KJ. Desmoglein 1-dependent suppression of EGFR signaling promotes epidermal differentiation and morphogenesis. J Cell Biol. 2009;185:1243–1258. doi: 10.1083/jcb.200809044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottardi CJ, Gumbiner BM. Distinct molecular forms of beta-catenin are targeted to adhesive or transcriptional complexes. J Cell Biol. 2004;167:339–349. doi: 10.1083/jcb.200402153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gottardi CJ, Wong E, Gumbiner BM. E-cadherin suppresses cellular transformation by inhibiting beta-catenin signaling in an adhesion-independent manner. J Cell Biol. 2001;153:1049–1060. doi: 10.1083/jcb.153.5.1049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hardman MJ, Liu K, Avilion AA, Merritt A, Brennan K, Garrod DR, Byrne C. Desmosomal cadherin misexpression alters beta-catenin stability and epidermal differentiation. Mol Cell Biol. 2005;25:969–978. doi: 10.1128/MCB.25.3.969-978.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He XC, et al. PTEN-deficient intestinal stem cells initiate intestinal polyposis. Nat Genet. 2007;39:189–198. doi: 10.1038/ng1928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- He XC, et al. BMP signaling inhibits intestinal stem cell self-renewal through suppression of Wnt-beta-catenin signaling. Nat Genet. 2004;36:1117–1121. doi: 10.1038/ng1430. [DOI] [PubMed] [Google Scholar]
- Hermiston ML, Wong MH, Gordon JI. Forced expression of E-cadherin in the mouse intestinal epithelium slows cell migration and provides evidence for nonautonomous regulation of cell fate in a self-renewing system. Genes Dev. 1996;10:985–996. doi: 10.1101/gad.10.8.985. [DOI] [PubMed] [Google Scholar]
- Holthofer B, Windoffer R, Troyanovsky S, Leube RE. Structure and function of desmosomes. Int Rev Cytol. 2007;264:65–163. doi: 10.1016/S0074-7696(07)64003-0. [DOI] [PubMed] [Google Scholar]
- Hu T, Li C. Convergence between Wnt-beta-catenin and EGFR signaling in cancer. Mol Cancer. 2010;9:236. doi: 10.1186/1476-4598-9-236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphries A, Wright NA. Colonic crypt organization and tumorigenesis. Nat Rev Cancer. 2008;8:415–424. doi: 10.1038/nrc2392. [DOI] [PubMed] [Google Scholar]
- Ivanov AI, Bachar M, Babbin BA, Adelstein RS, Nusrat A, Parkos CA. A unique role for nonmuscle myosin heavy chain IIA in regulation of epithelial apical junctions. PLoS One. 2007;2:e658. doi: 10.1371/journal.pone.0000658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jeanes A, Gottardi CJ, Yap AS. Cadherins and cancer: how does cadherin dysfunction promote tumor progression? Oncogene. 2008;27:6920–6929. doi: 10.1038/onc.2008.343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ. Cancer statistics. CA Cancer J Clin. 2008;58:71–96. doi: 10.3322/CA.2007.0010. [DOI] [PubMed] [Google Scholar]
- Jin T, George Fantus I, Sun J. Wnt and beyond Wnt: multiple mechanisms control the transcriptional property of beta-catenin. Cell Signal. 2008;20:1697–1704. doi: 10.1016/j.cellsig.2008.04.014. [DOI] [PubMed] [Google Scholar]
- Kaplan DD, Meigs TE, Kelly P, Casey PJ. Identification of a role for beta-catenin in the establishment of a bipolar mitotic spindle. J Biol Chem. 2004;279:10829–10832. doi: 10.1074/jbc.C400035200. [DOI] [PubMed] [Google Scholar]
- Khan K, Hardy R, Haq A, Ogunbiyi O, Morton D, Chidgey M. Desmocollin switching in colorectal cancer. Br J Cancer. 2006;95:1367–1370. doi: 10.1038/sj.bjc.6603453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koon HW, Zhao D, Zhan Y, Moyer MP, Pothoulakis C. Substance P mediates antiapoptotic responses in human colonocytes by Akt activation. Proc Natl Acad Sci USA. 2007;104:2013–2018. doi: 10.1073/pnas.0610664104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korinek V, Barker N, Morin PJ, van Wichen D, de Weger R, Kinzler KW, Vogelstein B, Clevers H. Constitutive transcriptional activation by a beta-catenin-Tcf complex in APC-/- colon carcinoma. Science. 1997;275:1784–1787. doi: 10.1126/science.275.5307.1784. [DOI] [PubMed] [Google Scholar]
- Kowalczyk AP, Borgwardt JE, Green KJ. Analysis of desmosomal cadherin-adhesive function and stoichiometry of desmosomal cadherin-plakoglobin complexes. J Invest Dermatol. 1996;107:293–300. doi: 10.1111/1523-1747.ep12363000. [DOI] [PubMed] [Google Scholar]
- Kowalczyk AP, Palka HL, Luu HH, Nilles LA, Anderson JE, Wheelock MJ, Green KJ. Posttranslational regulation of plakoglobin expression. Influence of the desmosomal cadherins on plakoglobin metabolic stability. J Biol Chem. 1994a;269:31214–31223. [PubMed] [Google Scholar]
- Kowalczyk AP, Stappenbeck TS, Parry DA, Palka HL, Virata ML, Bornslaeger EA, Nilles LA, Green KJ. Structure and function of desmosomal transmembrane core and plaque molecules. Biophys Chem. 1994b;50:97–112. doi: 10.1016/0301-4622(94)85023-2. [DOI] [PubMed] [Google Scholar]
- Kuphal F, Behrens J. E-cadherin modulates Wnt-dependent transcription in colorectal cancer cells but does not alter Wnt-independent gene expression in fibroblasts. Exp Cell Res. 2006;312:457–467. doi: 10.1016/j.yexcr.2005.11.007. [DOI] [PubMed] [Google Scholar]
- Kurzen H, Munzing I, Hartschuh W. Expression of desmosomal proteins in squamous cell carcinomas of the skin. J Cutan Pathol. 2003;30:621–630. doi: 10.1034/j.1600-0560.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- Lee G, et al. Phosphoinositide 3-kinase signaling mediates beta-catenin activation in intestinal epithelial stem and progenitor cells in colitis. Gastroenterol 139. 2010;881:e1–e9. doi: 10.1053/j.gastro.2010.05.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisanti MP, Caras IW, Davitz MA, Rodriguez-Boulan E. A glycophospholipid membrane anchor acts as an apical targeting signal in polarized epithelial cells. J Cell Biol. 1989;109:2145–2156. doi: 10.1083/jcb.109.5.2145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorch JH, Klessner J, Park JK, Getsios S, Wu YL, Stack MS, Green KJ. Epidermal growth factor receptor inhibition promotes desmosome assembly and strengthens intercellular adhesion in squamous cell carcinoma cells. J Biol Chem. 2004;279:37191–37200. doi: 10.1074/jbc.M405123200. [DOI] [PubMed] [Google Scholar]
- Lu Z, Ghosh S, Wang Z, Hunter T. Downregulation of caveolin-1 function by EGF leads to the loss of E-cadherin, increased transcriptional activity of beta-catenin, and enhanced tumor cell invasion. Cancer Cell. 2003;4:499–515. doi: 10.1016/s1535-6108(03)00304-0. [DOI] [PubMed] [Google Scholar]
- Maher MT, Mo R, Flozak AS, Peled ON, Gottardi CJ. Beta-catenin phosphorylated at serine 45 is spatially uncoupled from beta-catenin phosphorylated in the GSK3 domain: implications for signaling. PLoS One. 2010;5:e10184. doi: 10.1371/journal.pone.0010184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Markowitz SD, Bertagnolli MM. Molecular origins of cancer: molecular basis of colorectal cancer. N Engl J Med. 2009;361:2449–2460. doi: 10.1056/NEJMra0804588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathias RA, Wang B, Ji H, Kapp EA, Moritz RL, Zhu HJ, Simpson RJ. Secretome-based proteomic profiling of Ras-transformed MDCK cells reveals extracellular modulators of epithelial-mesenchymal transition. J Proteome Res. 2009;8:2827–2837. doi: 10.1021/pr8010974. [DOI] [PubMed] [Google Scholar]
- Merritt AJ, Berika MY, Zhai W, Kirk SE, Ji B, Hardman MJ, Garrod DR. Suprabasal desmoglein 3 expression in the epidermis of transgenic mice results in hyperproliferation and abnormal differentiation. Mol Cell Biol. 2002;22:5846–5858. doi: 10.1128/MCB.22.16.5846-5858.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller JR, Moon RT. Analysis of the signaling activities of localization mutants of beta-catenin during axis specification in Xenopus. J Cell Biol. 1997;139:229–243. doi: 10.1083/jcb.139.1.229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miravet S, Piedra J, Castano J, Raurell I, Franci C, Dunach M, Garc de Herreros A. Tyrosine phosphorylation of plakoglobin causes contrary effects on its association with desmosomes and adherens junction components and modulates beta-catenin-mediated transcription. Mol Cell Biol. 2003;23:7391–7402. doi: 10.1128/MCB.23.20.7391-7402.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morin PJ, Sparks AB, Korinek V, Barker N, Clevers H, Vogelstein B, Kinzler KW. Activation of beta-catenin-Tcf signaling in colon cancer by mutations in beta-catenin or APC. Science. 1997;275:1787–1790. doi: 10.1126/science.275.5307.1787. [DOI] [PubMed] [Google Scholar]
- Mulholland DJ, Dedhar S, Wu H, Nelson CC. PTEN and GSK3beta: key regulators of progression to androgen-independent prostate cancer. Oncogene. 2006;25:329–337. doi: 10.1038/sj.onc.1209020. [DOI] [PubMed] [Google Scholar]
- Munemitsu S, Albert I, Souza B, Rubinfeld B, Polakis P. Regulation of intracellular beta-catenin levels by the adenomatous polyposis coli (APC) tumor-suppressor protein. Proc Natl Acad Sci USA. 1995;92:3046–3050. doi: 10.1073/pnas.92.7.3046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naito AT, Akazawa H, Takano H, Minamino T, Nagai T, Aburatani H, Komuro I. Phosphatidylinositol 3-kinase-Akt pathway plays a critical role in early cardiomyogenesis by regulating canonical Wnt signaling. Circ Res. 2005;97:144–151. doi: 10.1161/01.RES.0000175241.92285.f8. [DOI] [PubMed] [Google Scholar]
- Nava P, et al. Interferon-gamma regulates intestinal epithelial homeostasis through converging beta-catenin signaling pathways. Immunity. 2010;32:392–402. doi: 10.1016/j.immuni.2010.03.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nava P, Laukoetter MG, Hopkins AM, Laur O, Gerner-Smidt K, Green KJ, Parkos CA, Nusrat A. Desmoglein-2: a novel regulator of apoptosis in the intestinal epithelium. Mol Biol Cell. 2007;18:4565–4578. doi: 10.1091/mbc.E07-05-0426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson WJ, Nusse R. Convergence of Wnt, beta-catenin, and cadherin pathways. Science. 2004;303:1483–1487. doi: 10.1126/science.1094291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ng SS, Mahmoudi T, Danenberg E, Bejaoui I, de Lau W, Korswagen HC, Schutte M, Clevers H. Phosphatidylinositol 3-kinase signaling does not activate the Wnt cascade. J Biol Chem. 2009;284:35308–35313. doi: 10.1074/jbc.M109.078261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niessen CM, Gumbiner BM. Cadherin-mediated cell sorting not determined by binding or adhesion specificity. J Cell Biol. 2002;156:389–399. doi: 10.1083/jcb.200108040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oshiro MM, et al. Epigenetic silencing of DSC3 is a common event in human breast cancer. Breast Cancer Res. 2005;7:R669–R680. doi: 10.1186/bcr1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oving IM, Clevers HC. Molecular causes of colon cancer. Eur J Clin Invest. 2002;32:448–457. doi: 10.1046/j.1365-2362.2002.01004.x. [DOI] [PubMed] [Google Scholar]
- Pinto D, Clevers H. Wnt control of stem cells and differentiation in the intestinal epithelium. Exp Cell Res. 2005;306:357–363. doi: 10.1016/j.yexcr.2005.02.022. [DOI] [PubMed] [Google Scholar]
- Rimerman RA, Gellert-Randleman A, Diehl JA. Wnt1 and MEK1 cooperate to promote cyclin D1 accumulation and cellular transformation. J Biol Chem. 2000;275:14736–14742. doi: 10.1074/jbc.m910241199. [DOI] [PubMed] [Google Scholar]
- Rowan AJ, Lamlum H, Ilyas M, Wheeler J, Straub J, Papadopoulou A, Bicknell D, Bodmer WF, Tomlinson IP. APC mutations in sporadic colorectal tumors: a mutational “hotspot” and interdependence of the “two hits”. Proc Natl Acad Sci USA. 2000;97:3352–3357. doi: 10.1073/pnas.97.7.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadot E, Simcha I, Shtutman M, Ben-Ze’ev A, Geiger B. Inhibition of beta-catenin-mediated transactivation by cadherin derivatives. Proc Natl Acad Sci USA. 1998;95:15339–15344. doi: 10.1073/pnas.95.26.15339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmitt CJ, Franke WW, Goerdt S, Falkowska-Hansen B, Rickelt S, Peitsch WK. Homo- and heterotypic cell contacts in malignant melanoma cells and desmoglein 2 as a novel solitary surface glycoprotein. J Invest Dermatol. 2007;127:2191–2206. doi: 10.1038/sj.jid.5700849. [DOI] [PubMed] [Google Scholar]
- Sharma M, Chuang WW, Sun Z. Phosphatidylinositol 3-kinase/Akt stimulates androgen pathway through GSK3beta inhibition and nuclear beta-catenin accumulation. J Biol Chem. 2002;277:30935–30941. doi: 10.1074/jbc.M201919200. [DOI] [PubMed] [Google Scholar]
- Shimizu H, Julius MA, Giarre M, Zheng Z, Brown AM, Kitajewski J. Transformation by Wnt family proteins correlates with regulation of beta-catenin. Cell Growth Differ. 1997;8:1349–1358. [PubMed] [Google Scholar]
- Stockinger A, Eger A, Wolf J, Beug H, Foisner R. E-cadherin regulates cell growth by modulating proliferation-dependent beta-catenin transcriptional activity. J Cell Biol. 2001;154:1185–1196. doi: 10.1083/jcb.200104036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tetsu O, McCormick F. Beta-catenin regulates expression of cyclin D1 in colon carcinoma cells. Nature. 1999;398:422–426. doi: 10.1038/18884. [DOI] [PubMed] [Google Scholar]
- Tian Q, Feetham MC, Tao WA, He XC, Li L, Aebersold R, Hood L. Proteomic analysis identifies that 14-3-3zeta interacts with beta-catenin and facilitates its activation by Akt. Proc Natl Acad Sci USA. 2004;101:15370–15375. doi: 10.1073/pnas.0406499101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeulen L, et al. Wnt activity defines colon cancer stem cells and is regulated by the microenvironment. Nat Cell Biol. 2010;12:468–476. doi: 10.1038/ncb2048. [DOI] [PubMed] [Google Scholar]
- Vermeulen L, Sprick MR, Kemper K, Stassi G, Medema JP. Cancer stem cells–old concepts, new insights. Cell Death Differ. 2008;15:947–958. doi: 10.1038/cdd.2008.20. [DOI] [PubMed] [Google Scholar]
- Vlahos CJ, Matter WF, Hui KY, Brown RF. A specific inhibitor of phosphatidylinositol 3-kinase, 2-(4-morpholinyl)-8-phenyl-4H-1-benzopyran-4-one (LY294002) J Biol Chem. 1994;269:5241–5248. [PubMed] [Google Scholar]
- Wahl JK III, Nieset JE, Sacco-Bubulya PA, Sadler TM, Johnson KR, Wheelock MJ. The amino- and carboxyl-terminal tails of (beta)-catenin reduce its affinity for desmoglein 2. J Cell Sci. 2000;113:1737–1745. doi: 10.1242/jcs.113.10.1737. [DOI] [PubMed] [Google Scholar]
- Wang L, Liu T, Wang Y, Cao L, Nishioka M, Aguirre RL, Ishikawa A, Geng L, Okada N. Altered expression of desmocollin 3, desmoglein 3, and beta-catenin in oral squamous cell carcinoma: correlation with lymph node metastasis and cell proliferation. Virchows Arch. 2007;451:959–966. doi: 10.1007/s00428-007-0485-5. [DOI] [PubMed] [Google Scholar]
- Wielenga VJ, Smits R, Korinek V, Smit L, Kielman M, Fodde R, Clevers H, Pals ST. Expression of CD44 in Apc and Tcf mutant mice implies regulation by the WNT pathway. Am J Pathol. 1999;154:515–523. doi: 10.1016/S0002-9440(10)65297-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MH, Hermiston ML, Syder AJ, Gordon JI. Forced expression of the tumor suppressor adenomatosis polyposis coli protein induces disordered cell migration in the intestinal epithelium. Proc Natl Acad Sci USA. 1996;93:9588–9593. doi: 10.1073/pnas.93.18.9588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong MH, Rubinfeld B, Gordon JI. Effects of forced expression of an NH2-terminal truncated beta-catenin on mouse intestinal epithelial homeostasis. J Cell Biol. 1998;141:765–777. doi: 10.1083/jcb.141.3.765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang L, et al. Akt/protein kinase B signaling inhibitor-2, a selective small molecule inhibitor of Akt signaling with antitumor activity in cancer cells overexpressing Akt. Cancer Res. 2004;64:4394–4399. doi: 10.1158/0008-5472.CAN-04-0343. [DOI] [PubMed] [Google Scholar]
- Zhang J, Woodhead GJ, Swaminathan SK, Noles SR, McQuinn ER, Pisarek AJ, Stocker AM, Mutch CA, Funatsu N, Chenn A. Cortical neural precursors inhibit their own differentiation via N-cadherin maintenance of beta-catenin signaling. Dev Cell. 2010;18:472–479. doi: 10.1016/j.devcel.2009.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhurinsky J, Shtutman M, Ben-Ze’ev A. Differential mechanisms of LEF/TCF family-dependent transcriptional activation by beta-catenin and plakoglobin. Mol Cell Biol. 2000;20:4238–4252. doi: 10.1128/mcb.20.12.4238-4252.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.