Abstract
A case of Rickettsia tamurae infection in Japan is reported. A 76-year-old Japanese male had a tick bite which developed to local skin inflammation on his left leg. Anti-rickettsia antibodies were detected in his serum, and R. tamurae DNA was identified in his blood, the lesional skin, and the tick.
Key Words: Rickettsia tamurae infection, Spotted fever group, Amblyomma testudinarium, Local skin inflammation, Human pathogen
Introduction
In recent decades, reports of newly described rickettsioses have increased as a result of improved cell culture isolation technique and extensive use of bacterial detection and identification techniques based on molecular biology. R. tamurae was isolated from the Amblyomma testudinarium tick in 1993 in Japan [1]. Fournier et al. formally identified R. tamurae as a novel species by genetic and phylogenetic analyses in 2006 [2]. Although R. tamurae has often been isolated from A. testudinarium ticks in Japan, the pathogenic role of this rickettsia in humans is yet unknown. We report the first official case of local skin inflammation caused by tick-borne R. tamurae in the Shimane prefecture, the western part of central Japan (fig. 1).
Fig. 1.
Geographical position of Shimane in Japan. Star: location of the present case.
Case Report
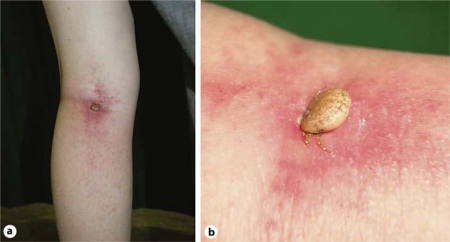
A 76-year-old man visited Shimane University Hospital with a skin nodule in the left popliteal region and pain in the left leg on June 22, 2009. He had a history of multiple cerebral infarction, and had been suffering from insulin-dependent diabetes mellitus for 10 years. He often took a walk to some fields near his house. Three days before visiting our hospital, he had felt some pain in the left leg. One day before the visit, a nodule was found in his left popliteal region and the left leg became swollen (fig. 2a). The nodule measured 15 mm in diameter and was identified as a tick body during a subsequent medical examination (fig. 2b). Although diffuse erythema, mild swelling and mild heat with pain were found in the left sural area, none of the typical clinical signs (e.g. high fever, generalized rash, lymphadenopathy) of spotted fever rickettsiosis was observed. The erythema blanched with pressure. Skin hemorrhages were absent. Hematological examination showed a white blood cell count of 9,070/μl and a C-reactive protein level of 1.30 mg/dl (less than 0.5 mg/dl is considered normal) on June 22, 2009. No abnormal results were found in other blood examinations.
Fig. 2.
Erythema and mild swelling of the left sural area. There was a 15 mm-sized tick in the left popliteal region (a). The engorged tick, which was an Amblyomma testudinarium female, had attached itself to the patient's popliteal region (b).
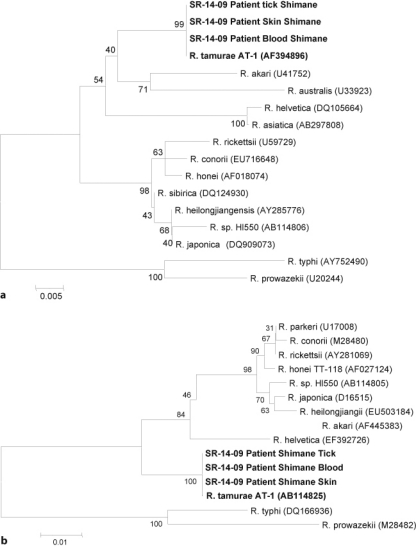
The tick was removed with the attached skin by a scalpel under local anesthesia and identified as a female A. testudinarium based on morphological characteristics [3]. Further detail classification of the tick was performed with a PCR-based amplification technique of tick-associated DNA. DNA was extracted from the patient's blood, the skin biopsy specimen and the infected tick with a QIAamp DNA Mini Kit (QIAGEN, Courtaboeuf, France) according to the manufacturer's instructions. PCR amplification and sequencing reactions were performed using the following primers in accordance with a previously reported method: primers RpCS.877p/RpCS.1258n for the genus Rickettsia which target the citrate synthase-encoding gene (gltA) [4], primers Rr17.61p/Rr17.492n for the 17 kDa genus-common antigen gene [5], primers 10/11 for the 56 kDa outer membrane protein gene of Orientia tsutsugamushi [6] and primers p3761/p4183 for the 44 kDa outer membrane protein gene of Anaplasma sp. (p44 multigene family) [7]. Although the O. tsutsugamushi and genus Anaplasma genes were not detected, all samples were positive for the gltA and 17 kDa genus-common antigen genes. The DNA fragments separated by agarose gel electrophoresis were extracted using the QIAEX Gel Extraction Kit (QIAGEN). DNA sequencing was performed using an ABI PRISM® BigDyeTM Terminator v3.1 KIT (Life Technologies, Carlsbad, Calif., USA) on an ABI Prism 3130 Genetic Analyzer (Life Technologies). The nucleotide sequences were compared with the corresponding sequences deposited in the DNA database (GenBank/EMBL/DDBJ) by using the BLAST tool (http://blast.ddbj.nig.ac.jp/top-j.html), and aligned using ClustalW on Biomanager by ANGIS (http://www.angis.org.au) and Mega 4 (version 1.83). A phylogenetic tree was constructed by the neighbor-joining method. The phylogram analysis of spotted fever group (SFG) rickettsiae derived from gltA and 17 kDa genus-common antigen genes revealed 100% nucleotide sequence homology with R. tamurae AT-1 (fig. 3a, b). Histological examination was not performed.
Fig. 3.
Phylogenetic tree of SFG rickettsiae derived from the gltA gene (a) and phylogenetic tree of SFG rickettsiae derived from the 17 kDa genus-common antigen gene (b) by the neighbor-joining method. The numbers at nodes are the bootstrap values obtained from 100 re-samplings. The scale bars represent 0.5% (glt-A gene) and 1% (17 kDa genus-common antigen gene) differences in nucleotide sequences (GenBank accession numbers are shown).
Oral minocycline hydrochloride 200 mg/day was administered, whereupon the leukocytosis and the increased serum C-reactive protein level went back to normal limits within 1 week. The medication was continued for 2 weeks until the skin eruption disappeared. The PCR assay for the gltA gene and the 17 kDa genus-common antigen gene became negative 1 week after administration of minocycline hydrochloride. Neither fever nor lymphadenopathy was observed throughout the clinical course.
Serum IgM and IgG antibody titers against the following rickettsiae were measured in series by indirect immunofluorescence technique [8]: R. tamurae (AT-1 strain), Rickettsia japonica (YH strain), Rickettsia typhi (Wilmington strain), as well as titers against O. tsutsugamushi (Karp, Gilliam, Kuroki, Kawasaki, and Kato strains). The patient showed positive antibody titers against R. tamurae and R. japonica (table 1). The increased R. japonica titers might be serological cross-reactions between R. tamurae and R. japonica.
Table 1.
Serum IgM and IgG antibody titers of the rickettsiae and O. tsutsugamushi measured by the indirect immunofluorescence technique
| Species | June 22, 2009 | June 29, 2009 | July 6, 2009 | July 30, 2009 | August 27, 2009 |
|---|---|---|---|---|---|
| R. tamurae | |||||
| IgG | <20 | <20 | 20 | 160 | 10,240 |
| IgM | 20 | 20 | 40 | 160 | 2,560 |
| R. japonica | |||||
| IgG | <20 | <20 | <20 | 160 | 5,120 |
| IgM | 20 | 20 | 40 | 160 | 640 |
| O. tsutsugamushi | |||||
| IgG | <20 | <20 | <20 | <20 | <20 |
| IgM | <20 | <20 | <20 | <20 | <20 |
| R. typhi | |||||
| IgG | <20 | <20 | <20 | <20 | <20 |
| IgM | <20 | <20 | <20 | <20 | <20 |
Discussion
The clinical features of rickettsiosis can vary in intensity, ranging from the mild symptomatic type, e.g. tick-borne lymphadenopathy [9], or Rickettsia parkeri infection [10] to the severe symptomatic type, e.g. Japanese spotted fever. Although there has been no report of a patient associated with R. tamurae as a human pathogen, this rickettsia has been suspected to have some pathogenic potential. Here we report the first case of local skin inflammation caused by R. tamurae in Japan, which was proved by phylogenetic and serological analysis. There have been several case reports of tick bite due to A. testudinarium describing local symptoms, such as papules or pustules, without general symptoms like Japanese spotted fever [11]. These reports might include cases of R. tamurae infection, because these patients were not examined for rickettsiae.
The present case exhibited mild local inflammatory signs: swelling, erythema and heat with pain. Although these symptoms were cellulitis-like features and we could not exclude other bacterial infections, increased serum antibody titers against R. tamurae strongly suggested that the patient actually had a R. tamurae infection.
Japanese spotted fever is well known to clinicians; however, most atypical cases of tick bite remain uninvestigated. Serological testing and PCR analysis play a critical role in the diagnosis of rickettsiosis, including R. tamurae infection.
Acknowledgements
We are grateful to Dr. Hiroki Kawabata, National Institute of Infectious Diseases, Tokyo, for reviewing the manuscript.
Footnotes
This is an Open Access article licensed under the terms of the Creative Commons Attribution-NonCommercial-NoDerivs 3.0 License (www.karger.com/OA-license), applicable to the online version of the article only. Distribution for non-commercial purposes only.
References
- 1.Fujita H, Watanabe Y, Ishikura M, Takada N. List of all isolates of spotted fever group rickettsiae from ticks in Japan 1993-1998. Ann Rep Ohara General Hosp. 1999;42:45–50. [Google Scholar]
- 2.Fournier PE, Takada N, Fujita H, Raoult D. Rickettsia tamurae sp. nov., isolated from Amblyomma testudinarium ticks. Int J Syst Evol Microbiol. 2006;56:1673–1675. doi: 10.1099/ijs.0.64134-0. [DOI] [PubMed] [Google Scholar]
- 3.Yamaguchi N, Tipton VJ, Keegan HL, Toshioka S. Ticks of Japan, Korea, and Ryukyu Islands. Brigham Young Univ Bull Biol Ser. 1971;15:25–30. [Google Scholar]
- 4.Regnery RL, Spruill CL, Plikaytis BD. Genotypic identification of Rickettsiae and estimation of intraspecies divergence for portions of two rickettsial genes. J Bacteriol. 1991;173:1576–1589. doi: 10.1128/jb.173.5.1576-1589.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Noda H, Munderloh UG, Kurtti TJ. Endosymbionts of ticks and their relationship to Wolbachia spp. and tick-borne pathogens of humans and animals. Appl Environ Microbiol. 1997;63:3926–3932. doi: 10.1128/aem.63.10.3926-3932.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Furuya Y, Yoshida Y, Katayama T, Kawamori F, Yamamoto S, Ohashi N, Tamura A, Kawamura A., Jr Specific amplification of Rickettsia tsutsugamushi DNA from clinical specimens by polymerase chain reaction. J Clin Microbiol. 1991;29:2628–2630. doi: 10.1128/jcm.29.11.2628-2630.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ohashi N, Inayoshi M, Kitamura K, Kawamori F, Kawaguchi D, Nishimura Y, et al. Anaplasma phagocytophilum-infected ticks, Japan. Emerg Infect Dis. 2005;11:1780–1783. doi: 10.3201/eid1111.050407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Uchida T, Tashiro F, Funato T, Kitamura Y. Immunofluorescence test with Rickettsia Montana for serologic diagnosis of rickettsial infection of the spotted fever group in Shikoku, Japan. Microbiol Immunol. 1986;30:1061–1066. doi: 10.1111/j.1348-0421.1986.tb03035.x. [DOI] [PubMed] [Google Scholar]
- 9.Parola P, Rovery C, Rolain JM, Brouqui P, Davoust B, Raoult D. Rickettsia slovaca and R. raoultii in tick-borne rickettsioses. Emerg Infect Dis. 2009;15:1105–1108. doi: 10.3201/eid1507.081449. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.IA Conti-Díaz, Moraes-Filho J, Pacheco RC, Labruna MB. Serological evidence of Rickettsia parkeri as the etiological agent of rickettsiosis in Uruguay. Rev Inst Med Trop S Paulo. 2009;51:337–339. doi: 10.1590/s0036-46652009000600005. [DOI] [PubMed] [Google Scholar]
- 11.F Nakamura-Uchiyama, Komuro Y, Yoshii A, Nawa Y. Amblyomma testudinarium tick bite: one case of engorged adult and a case of extraordinary number of larval tick infestation. J Dermatol. 2000;27:774–777. doi: 10.1111/j.1346-8138.2000.tb02280.x. [DOI] [PubMed] [Google Scholar]