Introduction
Fasting in Ramadan is obligatory for all healthy Muslim adults. No food or drink may be consumed between dawn and sunset [1]. Strictly speaking, the fast of Ramadan is a period of “intermittent fasting” or daily cycles of “alternating” fasting and feeding periods. The periods of the fasting and feeding vary by the geographical locations and by time of the year. During the month of Ramadan, there are two main meals in most Moslem communities. These are commonly referred to by their Arabic origin, namely the “Iftar” (i.e. break of fast immediately after sunset) and “Sohur or Suhoor” (i.e. pre-dawn meal). As the Islamic calendar year is lunar, Ramadan (the ninth month) therefore starts approximately 10 days earlier each year on the Gregorian calendar. This year, 2007, Ramadan is likely to start between 12th and 14th September.
Certain groups are exempt from fasting temporarily or permanently including the sick, the elderly, the travellers and the expecting and nursing mothers [1]. However, many of those who are exempt may wish to observe the fast [2]. It is the responsibility of the medical professional to empower patients to make an informed choice and, if possible, an evidence-based decision.
There are several studies on the changes observed in clinical, body composition, and biochemical parameters during the fasting month of Ramadan in healthy subjects and in various medical conditions. The EPIDIAR Study was the largest study reported involving 1,070 patients with type 1 diabetes and 11,173 patients with type 2 diabetes [2]. Less than 50% of the whole population changed their treatment and hypoglycaemia was the only observed event. There are also a few studies which evaluated specific management modalities in those patients with diabetes who observed the fast [3–5]. These have been adequately summarised and discussed in previous review articles, expert opinion statements, and conferences proceedings over the last two decades [6–13]. A further detailed summary and critical appraisal of these studies is outside the scope of this article. Our aim here is to present a practical approach to the assessment of diabetic patients before Ramadan and provide a guide on how to adjust the life style and medical management appropriately should the patient wish to observe the fast having deemed it to be reasonably safe.
Management of people with diabetes during Ramadan: Organizational Issues
The management of diabetes during Ramadan fasting should be considered well in advance of the holy month. Diabetes care departments should have comprehensive strategy meetings a few months before Ramadan. Many patients would have developed their own opinions and established their practices of amending their diabetes care management plans from previous personal experience. Patients attending diabetic clinics should be encouraged to seek advice before considering fasting the month of Ramadan [13]. However, poor knowledge about Ramadan and fasting and its management have been described among some health care professionals [14]. For patients, leaflet and booklets containing information and advice about Ramadan fasting for people with diabetes ought to be available in the waiting areas of diabetic clinics at least 3 months before the month starts (Figure 1). Special classes may need to be considered to enhance selfmanagement during this month [15]. Media presenters of health programmes and healthcare journalists should prepare such educational programmes in advance of the month of Ramadan. Expert doctors should take the time to give interviews preferably jointly with Imams to offer clear and authoritative views and respond to all commonly asked questions. In the clinical settings, doctors should have a clear understanding of the religious ruling on fasting to give their advice with confidence.
Figure 1.
Four examples of educational material on diabetes during Ramadan fast from Abu Dhabi, Qatar, Jordon and Morocco.
The pre-Ramadan consultation
Managing the individual patient with diabetes during Ramadan poses a major challenge. Patients and clinicians are confronted with the dilemma whether to fast or not. The caring physicians should approach this issue with great sensitivity. They should be familiar with the religious rulings and cite these appropriately. They should also be very familiar with the rationale of current guidelines on who may be allowed to fast. Doctors should have an up to date working knowledge on practical management of diabetes should fasting be allowed.
There are two questions that need to be answered. Firstly, when to advise against fasting? and secondly what is the optimal therapeutic regimen? Patients with type 1 and type 2 diabetes who are allowed or choose to fast should be given specific information on fasting and recommendations on therapeutic changes. They should be warned against skipping meals, taking medication irregularly or night time gorging. A model content of the consultation is shown in Table 1. This year we started to display Ramadan posters and distribute information leaflets from the end of June (Figure 1).
Table 1.
A proposed model pre-Ramadan consultation for diabetic persons who intend to fast. (modified from references 7 and 10)
Timing of the consultations
|
Objectives of the consultation
|
Contents of the consultation
|
Possible obstacles
|
When to advise against fasting?
The major concerns associated with fasting in patients with diabetes are shown in Table 2. These concerns need to be considered when the advice in favour of or against fasting is being addressed. There are widely accepted consensus criteria for advising against fasting (Table 3). An alternative approach proposed is a more elaborate stratification system to categorize risk in patients with type 1 or type 2 diabetes who fast during Ramadan into very high, high, moderate and low [11]. Very high risk included those with severe hypoglycaemia within the last 3 months prior to Ramadan, patients with a history of recurrent hypoglycaemia, patients with hypoglycaemia unawareness, patients with sustained poor glycaemic control, ketoacidosis within the last 3 months prior to Ramadan, type 1 diabetes, acute illness, hyperosmolar hyperglycaemic coma within the previous 3 months, patients who perform intense physical labour, pregnancy, and patients on chronic dialysis. High risk patients included those with moderate hyperglycaemia (average blood glucose between 150 and 300 mg/dl, A1C 7.5–9.0%), patients with renal insufficiency, patients with advanced macrovascular complications, people living alone that are treated with insulin or sulfonylureas, patients living alone, patients with comorbid conditions that present additional risk factors, old age with ill health and those on drugs that may affect mentation.
Table 2.
Major risks associated with fasting in patients with diabetes and their potential mechanisms (modified from references 11)*
|
These form the basis for advice against fasting in different clinical scenarios discussed in Table 3
Table 3.
Widely-accepted criteria to advise against fasting in patients with Diabetes. (modified from references 6–10)*
|
Some workers considered these separately for type 1 and type 2 patients and further subdivided them as absolute contraindications or relative contraindications or even more elaborate risk stratification (see text).
Moderate risk was exemplified by the well-controlled patients treated with short-acting insulin secretagogues, whereas well-controlled patients treated with diet alone, metformin, or a Glitazone who are otherwise healthy were deemed to have a low risk [11]. Because of the religious nature of the fast, the use of the terms “indicated” and “contraindicated” were deemed to be inappropriate [11]. These are based on the practical translation of the Quran teaching that “Muslims should not put themselves at risk by fasting” [1]. However, many diabetic subjects choose to fast and the physician should be sympathetic and sensitive to their convictions and try to work out a programme that will minimise the risk. The physician should agree on a strategy when to break the fast and when to terminate it, e.g. if more than one hypoglycaemic episode occurs then no further attempts to fast should be made (Table 3).
Life style modifications
Life style should be re-enforced before and during Ramadan (Table 4). Lack of careful attention to diet during the ‘non-fasting’ night time period with excessive gorging, or compensatory eating of carbohydrates and fatty foods, contributes to poor control and wide excursions in blood glucose and weight gain in the well controlled patient. Therefore, patients should be encouraged to maintain their good dietary habits and to resist any temptation to break their dietary restrictions, as during Ramadan, social functions are frequent and food is a common way of hospitality. Benefits from Ramadan fasting seem to appear only in patients who maintain their appropriate diets. Thus, in order to optimise glycaemic control, individuals with diabetes must be reminded to abstain from the high-calorie foods prepared during this month. Regular light to moderate exercise during Ramadan fasting can be tolerated and is safe in type 2 patients. Therefore, light to moderate exercises may continue throughout the fast either in the morning or at night well after breaking the fast. It is probably prudent to avoid exercise in the final few hours of the fast when the risk of hypoglycaemia is predictably maximal particularly in insulin-treated patients [2].
Table 4.
Example of guidance for self-management for fasting diabetic patients to be included in posters and leaftets to support the consultations (Modified from reference 9)
|
Modification of drug regimens
A. Type 2 diabetes
Patients with type 2 diabetes can be controlled by adhering to similar drug regimens to the pre-fasting period with the morning oral hypoglycaemic given at the break of the fast and the pre-dinner dose is usually reduced by 25–50% and given pre-Sohur. Anecdotally, use of Nateglinides with Iftar may produce less excursions of blood glucoses after Iftar either as a replacement to sulphonylureas or new addition to metformin of Glitazones.
Metformin could be given post-Iftar and Sohur but some patients may not tolerate the post-Sohur dose because of the gastrointestinal side-effects. If a slow-release preparation of metformin is available, the whole daily dose may be taken altogether after Iftar.
Patients on insulin and sulphonylureas combination should take their basal insulin (Isophane, Glargine or Detimer) about 10 pm to 12 midnight and the oral hypoglycaemic agents taken at Iftar.
Although there are no data on the use of newer anti-diabetic agents during Ramadan, it would seem sensible to take the Glitazones with the evening meal as they are normally taken once daily. Patients on the oral Gliptins would probably be better taking their single daily dose at Iftar. Exenatide injections should be taken twice before Iftar and before Suhor. It is likely that the Gliptins and incretin mimetics will specifically help reduce the post-iftar blood hyperglycaemia. However, evidence is lacking.
B. Type 1 diabetes
If a type 1 diabetic individual chooses to fast, then great care should be taken to monitor and adjust the dose of insulin accordingly.
Those on intensive insulin treatment should receive their long-acting basal insulin (such as Glargine and Detimer) at Iftar or at the usual time of 10 pm- 12 mid night (Isophane Insulin should be given as usual before bedtime). The dose of basal insulin needs to be adjusted according to blood glucose levels between mid-day and Iftar time. The short-acting insulin or rapid-acting insulin analogue at Iftar and Sohur times. The doses of these can be adjusted according to the amount of food consumed; previous experiences and blood glucoses measured 2-3 hours after iftar (conveniently after Isha prayers). For assessment of the pre-Sohur insulin doses, blood glucose can be measured between 11-12 mid day
Those on conventional twice daily insulin regimens should take their usual morning dose before Iftar and their usual evening dose before Sohur. However, the latter needs to be adjusted so that the fast-acting component remains the same and the intermediate acting insulin is cut by 50% or omitted.
Those on pre-mixed insulin such as 30/70 or 25/75 preparations (such Mixtard of Novo Nordisk or Humulin M series from Eli Lilly) should have their morning dose before the Iftar in the same or even greater dose. However the pre-Sohur dose should be reduced or substituted with shorter acting insulin only.
Some patients on insulin pump therapy managed to fast safely by adjusting their basal insulin down during the fasting time.
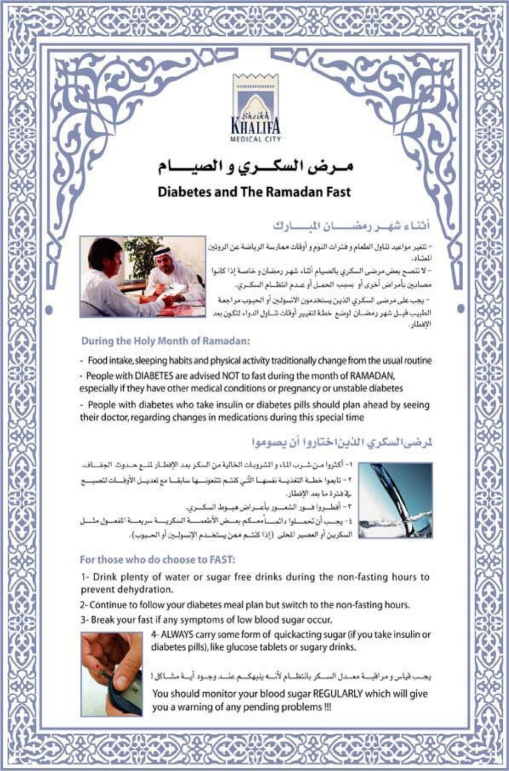
Figure 2.
An example of a blingual poster for Diabetes and Ramadan Fast from Sheikh Khalifa Medical City, Abu Dhabi, UAE. The information is fairly basic and quite appropriate for a poster
Conclusions
In conclusion, the majority of physicians are of the opinion that Ramadan fasting is acceptable for well balanced type 2 patients conscious of their disease and compliant with their diet and drug intake. Islamic rules allow patients not to fast. However, if patients with diabetes wish to fast, it is necessary to advise them to undertake regular monitoring of blood glucose levels several times a day, to reduce the risk of hypoglycemia during daytime fasting or hyperglycemia during the night. Patients with type 1 diabetes who fast during Ramadan may be better managed with fast- acting insulin. Basic knowledge of carbohydrate metabolism in health and disease, of the standard principles of diabetes care and of pharmacology of various anti-diabetic drugs are essential to enable physicians to guide their patients through the month of Ramadan safely. The practical management of these patients is made on an individual basis.
References
- 1.The Holy Quran. Sura 2: Verses; pp. 183–185. [Google Scholar]
- 2.Salti I, Benard E, Detournay B, Bianchi-Biscay M, Le Brigand C, Voinet C, et al. EPIDIAR study group, A population based study of diabetes and its characteristics during the fasting month of Ramadan in 13 countries: results of the epidemiology of diabetes and Ramadan 1422/ (EPIDIAR) study. Diabetes Care. 2004;27:2306–2311. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- 3.Belkhadir J, El Ghomari H, Klocker N, et al. Muslims with non-insulin dependent diabetes fasting during Ramadan: treatment with glibenclamide. Brit Med J. 1993;307:292–5. doi: 10.1136/bmj.307.6899.292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kadiri A, Al-Nakhi A, El-Ghazali S, et al. Treatment of type 1 diabetes with insulin lispro during Ramadan. Diabetes Metab. 2001;27:482–486. [PubMed] [Google Scholar]
- 5.Glimepiride in Ramadan (GLIRA) Study Group. The efficacy and safety of glimepiride in the management of type 2 diabetes in Muslim patients during Ramadan. Diabetes Care. 2005;28:421–422. doi: 10.2337/diacare.28.2.421. [DOI] [PubMed] [Google Scholar]
- 6.Sulimani R.A, Famuyiwa F.O, Laajam M.A. Diabetes mellitus and Ramadan fasting: the need for a critical appraisal. Diabetic Medicine. 1988;5:589–591. doi: 10.1111/j.1464-5491.1988.tb01057.x. [DOI] [PubMed] [Google Scholar]
- 7.Azizi F, Siahkolah B. Ramadan fasting and diabetes mellitus. Int. Journal Ramadan Fasting Res. 1998;2:8–17. [Google Scholar]
- 8.Diabetes and Ramadan Advisory Board. International Medical Recommendations for Muslim subjects with diabetes mellitus who fast during the month of Ramadan. Clinical Diabetes (Middle East Edition) 2004;3:143–145. [Google Scholar]
- 9.4. Akbani M.F, Saleem M, Gadit W.U, Ahmed M, Basit A, Malik R.A. Fasting and feasting safely during Ramadan in the diabetic patient. Practical Diabetes Int. 2005;22:100–104. [Google Scholar]
- 10.Beshyah S.A, Sherif I. Diabetes during Ramadan and Haj. In: Lakhdar A. A, Gill GV, editors. Diabetes in The Arab World. Cambridge: FSG. Communications Ltd; 2005. pp. 225–240. [Google Scholar]
- 11.Al-Arouj M, Bouguerra R, Buse J, Hafez S, Hassanein M, Ibrahim M.A, et al. Recommendations for management of diabetes during Ramadan. Diabetes Care. 2005;28:2305–2311. doi: 10.2337/diacare.28.9.2305. [DOI] [PubMed] [Google Scholar]
- 12.Benaji B, Mounib N, Roky R, Aadil N, Houti I.E, Moussamih S, Maliki S, Gressier B, El Ghomari H. Diabetes and Ramadan: Review of the literature. Diabetes Research and Clinical Practice. 2006;73:117–125. doi: 10.1016/j.diabres.2005.10.028. [DOI] [PubMed] [Google Scholar]
- 13.Al-Amoudi A.A, Al-Ulagi N, Bashir M, Bissar L, Al-Ghamdi S.M.G, Elhadd T.A. Education for diabetic patients for fasting of Ramadan: a questionnaire study. Endocrine Abstracts. 2006;11:P277. [Google Scholar]
- 14.Barrow L. Ramadan and diabetes: helping to ensure safe fasting. Journal of Diabetes Nursing. 2004;8(6):227–231. [Google Scholar]
- 15.Chowdhury T.A, Hussain H.A, Hayes H. An educational class on diabetes self-management during Ramadan. Pract Diab Int. 2003;20:306–7. [Google Scholar]