Abstract
Although the adverse health effects of nanoparticles/materials have been proposed and are being clarified, their facilitating effects on preexisting pathological conditions have not been fully established. We provide insights into the environmental immunotoxicity of nanoparticles as an aggravating factor in hypersusceptible subjects, especially those with respiratory disorders, using our in vivo models. We first examined the effects of nanoparticles/materials on lung inflammation induced by bacterial endotoxin (lipopolysaccharide) as a test model against innate immunity, and demonstrated that nanoparticles instilled through both an intratracheal tube and an inhalation system can exacerbate lung inflammation. Secondly, we examined the effects of nanoparticles/materials on allergic pathophysiology, and showed that repetitive pulmonary exposure to nanoparticles has aggravating effects on allergic airway inflammation, including adjuvant effects on Th2-milieu. Taken together, nanoparticle exposure may synergistically facilitate pathological inflammatory conditions in the lung via both innate and adaptive immunological abnormalities.
Keywords: Nanoparticles, Nanomaterials, Lung inflammation, Sensitivity, Asthma
Introduction
Epidemiological studies have demonstrated a correlation between exposure to air pollutant particles at the concentrations currently found in major metropolitan areas and mortality and morbidity [1]. The concentration of particulate matter (PM) with mass median aerodynamic diameter (a density-dependent unit of measure used to describe the diameter of the particle) ≤2.5 μm (PM2.5) is more closely associated with both acute and chronic respiratory effects and subsequent mortality than larger particles of ≤10 μm (PM10) [2]. In addition, one intriguing aspect of the epidemiologic data is that health effects of PM2.5 are primarily seen in subjects with predisposing factors, including pneumonia, asthma, chronic obstructive pulmonary disease, compromised immune systems, and age over 65 years old [3]. Consistent with the epidemiological studies, we have experimentally demonstrated that diesel exhaust particles (DEP), major contributors to environmental PM2.5 in urban areas, exhibit respiratory toxicity with or without predisposing factors in vivo [4–10].
To date, nanoparticles, particles less than 0.1 μm in mass median aerodynamic diameter, have been shown to be increasing in ambient air [11]. Recent measurements indicate that nanoparticle numbers in ambient air range from 2 × 104 to 2 × 105/cm3, with mass concentrations of more than 50 μg/m3 near major highways [12, 13].
Furthermore, nanotechnology is now advancing at an incredible pace, such that it is has created an alternative industrial revolution over the past few years [14]. Consistent with this, use of engineered nanomaterials has been rapidly increasing in commercial applications. As these materials have become more widespread, many questions have arisen regarding the effects they may have on the environment as alternative inhalable toxicants. Due to their size and characteristics, nanoparticles/materials have been implicated in cardiopulmonary system effects [15]. Compared with larger particles, nanoparticles have a higher deposition rate in the peripheral lung, can cross the pulmonary epithelium and reach the interstitium [16], and furthermore, may be systemically distributed in the bloodstream [17]. Nanoparticles have enhanced capacity to produce reactive oxygen species, and, consequently, have widespread toxicity [18–20]. Consistent with these in vitro and in vivo reports, nanoparticle exposure also reportedly influences cardiopulmonary systems with or without predisposing diseases in human studies [21, 22]. On the other hand, development of nanotechnology has increased the risk of types of particles other than combustion-derived particles in the environment, namely engineered nanomaterials [23]. Considering the variety of their sizes and natures, it can be imagined that exposure to nanolevel (<100 nm) materials might also lead to adverse health effects, including cardiorespiratory ones. Indeed, health toxicity induced by nanomaterials is being researched worldwide. In particular, nanomaterial exposure reportedly induces several patterns of lung inflammation [24–28]. Besides their toxic effects on health, therefore, it should be ascertained whether they also aggravate preexisting pathological conditions.
Effects of nanoparticles on acute lung inflammation induced by bacterial endotoxin
A glycolipid of Gram-negative bacteria known as endotoxin or lipopolysaccharide (LPS) stimulates host cells via innate immunity [29]. In animal models, intratracheal administration of LPS causes lung cytokine production, neutrophil recruitment, and lung injury [30]. LPS is found in bronchoalveolar lavage (BAL) fluid of patients with pneumonia [31] and acute respiratory distress syndrome [32], which sometimes results in a fatal outcome. In addition, LPS is a significant constituent of many air pollutant particles and has accordingly been implicated in the adverse effects of PM [33]. In accordance with the close links among LPS, lung inflammation (injury), and PM, we have previously shown that intratracheal administration of DEP and their components facilitates lung inflammation induced by LPS [8, 34] and subsequent systemic inflammation with coagulatory disturbance [9].
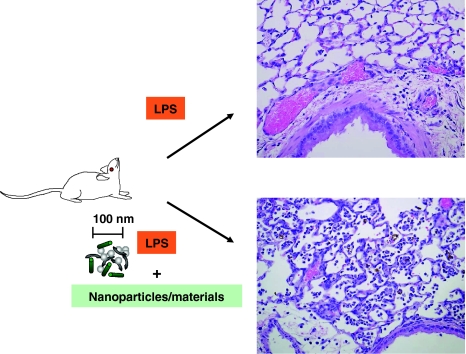
We next examined the effects of pulmonary exposure to nanoparticles (by an intratracheal instillation technique) on lung inflammation related to LPS in mice. Vehicle, two sizes (14 and 56 nm) of carbon black nanoparticles, LPS, or LPS + nanoparticles was administered intratracheally, and parameters of lung inflammation and coagulation were evaluated. Nanoparticles alone induced slight lung inflammation and significant pulmonary edema as compared with vehicle. Fourteen-nanometer nanoparticles intensively aggravated LPS-elicited lung inflammation and pulmonary edema, concomitant with enhanced lung expression of interleukin (IL)-1β, macrophage inflammatory protein (MIP)-1α, macrophage chemoattractant protein (MCP)-1, MIP-2, and keratinocyte chemoattractant (KC) as an overall trend, whereas 56-nm nanoparticles did not show apparent effects. Immunoreactivity for 8-hydroxyguanosine (OHdG), a proper marker for oxidative stress, was more intense in the lung from the LPS + 14 nm nanoparticle group than in that from the LPS group. The circulatory fibrinogen level was higher in the LPS + 14 nm nanoparticle group than in the LPS group. Taken together, nanoparticles can aggravate lung inflammation related to bacterial endotoxin, being more prominent with smaller particles. The enhancing effect may be mediated, at least partly, via increased local expression of proinflammatory cytokines and via oxidative stress. Furthermore, nanoparticles can promote coagulatory disturbance accompanied by lung inflammation [35].
Moreover, we examined the adverse effects of nanomaterials on this pathological model. In brief, ICR male mice were divided into 8 experimental groups that intratracheally received vehicle, three sizes (15, 50, 100 nm) of TiO2 nanomaterials, LPS, or LPS plus nanomaterials. Twenty-four hours after treatment, both nanomaterials exacerbated the lung inflammation and vascular permeability elicited by LPS, with an overall trend for amplified lung expression of cytokines such as IL-1β, MCP-1, and KC. LPS plus nanomaterials, especially of size less than 50 nm, elevated circulatory levels of fibrinogen, IL-1β, MCP-1, and KC, and von Willebrand factor as compared with LPS alone. The enhancement tended overall to be greater with the smaller nanomaterials than with the larger ones. These results suggest that nanomaterials exacerbate lung inflammation related to LPS with systemic inflammation and coagulatory disturbance and that the exacerbation is more prominent with smaller nanomaterials than with larger ones [36]. Additionally, we demonstrated that latex nanoparticles [37] and carbon nanotubes [38] have similar effects on the lung pathophysiology.
Our next study was conducted to determine whether inhaled exposure to diesel-engine-derived nanoparticles also exacerbates the model. ICR mice were exposed for 5 h to clean air or diesel-engine-derived nanoparticles at concentration of 15, 36 or 169 μg/m3 after intratracheal challenge with LPS or vehicle, and were sacrificed for evaluation 24 h after the intratracheal challenge. Exposure to nanoparticles alone did not elicit lung inflammation. Nanoparticle inhalation exaggerated LPS-elicited inflammatory cell recruitment in BAL fluid and lung parenchyma as compared with clean air inhalation in a concentration-dependent manner. Lung homogenates derived from the LPS + nanoparticle groups tended to have increased tumor necrosis factor-α level and chemotaxis activity for polymorphonuclear leukocytes as compared with those from the LPS group or the corresponding nanoparticle groups. Nanoparticle inhalation did not significantly increase lung expression of proinflammatory cytokines or influence systemic inflammation. Isolated alveolar macrophages from nanoparticle-exposed mice showed greater production of IL-1β and KC stimulated with ex vivo LPS challenge than those from clean-air-exposed mice, although the differences did not reach significance. These results suggest that acute exposure to diesel nanoparticles exacerbates lung inflammation induced by LPS [39]. In sum, nanoparticle/material exposure exacerbates acute lung inflammation related to bacterial endotoxin (Fig. 1).
Fig. 1.
Proposed schema for enhancement of acute lung injury by nanoparticles/materials
Effects of nanoparticles on allergic airway inflammation
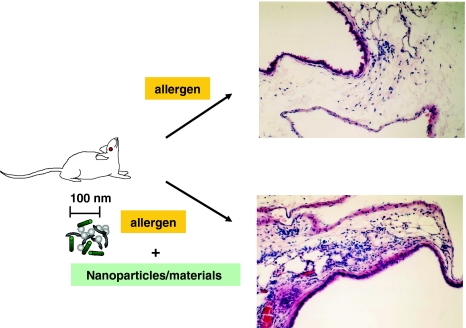
Bronchial asthma has been recognized as chronic airway inflammation with hyperresponsiveness that is characterized by an increase in the number of activated lymphocytes and eosinophils. A number of studies have shown that various particles including carbon black can enhance allergic sensitization [40–42], which is referred to as “adjuvant effect.” Carbon black has been demonstrated to enhance the proliferation of antibody-forming cells and both IgE and IgG levels [43, 44]. Ultrafine particles (PM and carbon black) reportedly exaggerate allergic airway inflammation in vivo [45, 46]. However, all studies have failed to examine the size of particles they used. Therefore, no research has addressed the size effects of particles or nanoparticles on airway biology in the presence or absence of allergen in vivo. Given the hypothesis, we investigated the effects of carbon black nanoparticles with a diameter of 14 or 56 nm on allergen-related airway inflammation. ICR mice were divided into six experimental groups. Vehicle, two sizes of carbon nanoparticles, ovalbumin (OVA), and OVA + nanoparticles were administered intratracheally. The cellular profile of BAL fluid, lung histology, expression of cytokines, chemokines, and 8-OHdG, and immunoglobulin production were studied. Nanoparticles with diameter of 14 or 56 nm aggravated allergen-related airway inflammation characterized by infiltration of eosinophils, neutrophils, and mononuclear cells, and by an increase in the number of goblet cells in bronchial epithelium. Nanoparticles with OVA increased protein levels of IL-5, IL-6, and IL-13, eotaxin, MCP-1, and regulated on activation and normal T cells expressed and secreted (RANTES) in the lung as compared with OVA alone. Formation of 8-OHdG was moderately induced by nanoparticles or allergen alone, and was markedly enhanced by allergen plus nanoparticles as compared with nanoparticles or allergen alone. The aggravation was more prominent with 14-nm nanoparticles than with 56-nm particles in terms of the overall trend. Particles with diameter of 14 nm exhibited adjuvant activity for total IgE and OVA-specific IgG and IgE. Nanoparticles can aggravate allergen-related airway inflammation and immunoglobulin production, being more prominent with smaller particles. The enhancement may be mediated, at least partly, by increased local expression of IL-5 and eotaxin, and also by modulated expression of IL-13, RANTES, MCP-1, and IL-6 [47].
In ongoing reports, nanoparticles alone or OVA alone moderately enhanced cholinergic airway reactivity, as assessed by total respiratory system resistance (R) and Newtonian resistance (Rn). All parameters of lung responsiveness, such as R, compliance, elastance, Rn, tissue damping, and tissue elastance, were worse in the nanoparticle + OVA groups than in the vehicle group, the corresponding nanoparticle groups, or the OVA group. The lung messenger RNA (mRNA) level for Muc5ac was significantly higher in the OVA group than in the vehicle group, and further increased in the nanoparticle + OVA groups than in the OVA or nanoparticle groups. These data suggest that carbon nanoparticles can enhance lung hyperresponsiveness, especially in the presence of allergen. The effects may be mediated, at least partly, through enhanced lung expression of Muc5ac [48].
Furthermore, we recently demonstrated that (single- and multiwalled) carbon nanotubes promote allergic airway inflammation in mice, which may be partly through enhanced oxidative stress in the airway and inappropriate activation of antigen-presenting cells including dendritic cells (in vitro) [49, 50]. Taken together, nanoparticle/material exposure can exacerbate allergic asthma (Fig. 2).
Fig. 2.
Proposed schema for enhancement of allergic airway inflammation by nanoparticles/materials
Acknowledgments
Special thanks to Prof. Hirohisa Takano, Prof. Takamichi Ichinose, Prof. Masahiko Satoh, Prof. Seishiro Hirano, Dr. Rie Yanagisawa, and Dr. Eiko Koike for greatly contributing to the work in the manuscript. The authors are supported by NIES grants.
References
- 1.Samet JM, Dominici F, Curriero FC, Coursac I, Zeger SL. Fine particulate air pollution and mortality in 20 U.S. cities, 1987–1994. N Engl J Med. 2000;343:1742–1749. doi: 10.1056/NEJM200012143432401. [DOI] [PubMed] [Google Scholar]
- 2.Peters A, Wichmann HE, Tuch T, Heinrich J, Heyder J. Respiratory effects are associated with the number of ultrafine particles. Am J Respir Crit Care Med. 1997;155:1376–1383. doi: 10.1164/ajrccm.155.4.9105082. [DOI] [PubMed] [Google Scholar]
- 3.Dockery DW, Pope CA, 3rd, Xu X, Spengler JD, Ware JH, Fay ME, et al. An association between air pollution and mortality in six U.S. cities. N Engl J Med. 1993;329:1753–1759. doi: 10.1056/NEJM199312093292401. [DOI] [PubMed] [Google Scholar]
- 4.Inoue KI, Takano H, Yanagisawa R, Ichinose T, Shimada A, Yoshikawa T. Pulmonary exposure to diesel exhaust particles induces airway inflammation and cytokine expression in NC/Nga mice. Arch Toxicol. 2005;79(10):595–599. doi: 10.1007/s00204-005-0668-2. [DOI] [PubMed] [Google Scholar]
- 5.Ichinose T, Furuyama A, Sagai M. Biological effects of diesel exhaust particles (DEP). II. Acute toxicity of DEP introduced into lung by intratracheal instillation. Toxicology. 1995;99:153–167. doi: 10.1016/0300-483X(94)03013-R. [DOI] [PubMed] [Google Scholar]
- 6.Ichinose T, Yajima Y, Nagashima M, Takenoshita S, Nagamachi Y, Sagai M. Lung carcinogenesis and formation of 8-hydroxy-deoxyguanosine in mice by diesel exhaust particles. Carcinogenesis. 1997;18:185–192. doi: 10.1093/carcin/18.1.185. [DOI] [PubMed] [Google Scholar]
- 7.Takano H, Yoshikawa T, Ichinose T, Miyabara Y, Imaoka K, Sagai M. Diesel exhaust particles enhance antigen-induced airway inflammation and local cytokine expression in mice. Am J Respir Crit Care Med. 1997;156:36–42. doi: 10.1164/ajrccm.156.1.9610054. [DOI] [PubMed] [Google Scholar]
- 8.Takano H, Yanagisawa R, Ichinose T, Sadakane K, Yoshino S, Yoshikawa T, et al. Diesel exhaust particles enhance lung injury related to bacterial endotoxin through expression of proinflammatory cytokines, chemokines, and intercellular adhesion molecule-1. Am J Respir Crit Care Med. 2002;165:1329–1335. doi: 10.1164/rccm.2108122. [DOI] [PubMed] [Google Scholar]
- 9.Inoue K, Takano H, Sakurai M, Oda T, Tamura H, Yanagisawa R, et al. Pulmonary exposure to diesel exhaust particles enhances coagulatory disturbance with endothelial damage and systemic inflammation related to lung inflammation. Exp Biol Med (Maywood) 2006;231:1626–1632. doi: 10.1177/153537020623101007. [DOI] [PubMed] [Google Scholar]
- 10.Inoue K, Koike E, Takano H, Yanagisawa R, Ichinose T, Yoshikawa T. Effects of diesel exhaust particles on antigen-presenting cells and antigen-specific Th immunity in mice. Exp Biol Med (Maywood) 2009;234:200–209. doi: 10.3181/0809-RM-285. [DOI] [PubMed] [Google Scholar]
- 11.Cyrys J, Stolzel M, Heinrich J, Kreyling WG, Menzel N, Wittmaack K, et al. Elemental composition and sources of fine and ultrafine ambient particles in Erfurt, Germany. Sci Total Environ. 2003;305:143–156. doi: 10.1016/S0048-9697(02)00494-1. [DOI] [PubMed] [Google Scholar]
- 12.Timonen KL, Hoek G, Heinrich J, Bernard A, Brunekreef B, Hartog J, et al. Daily variation in fine and ultrafine particulate air pollution and urinary concentrations of lung Clara cell protein CC16. Occup Environ Med. 2004;61:908–914. doi: 10.1136/oem.2004.012849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhu Y, Hinds WC, Kim S, Sioutas C. Concentration and size distribution of ultrafine particles near a major highway. J Air Waste Manag Assoc. 2002;52:1032–1042. doi: 10.1080/10473289.2002.10470842. [DOI] [PubMed] [Google Scholar]
- 14.Service RF. Nanotoxicology. Nanotechnology grows up. Science. 2004;304:1732–1734. doi: 10.1126/science.304.5678.1732. [DOI] [PubMed] [Google Scholar]
- 15.Utell MJ, Frampton MW. Acute health effects of ambient air pollution: the ultrafine particle hypothesis. J Aerosol Med. 2000;13:355–359. doi: 10.1089/jam.2000.13.355. [DOI] [PubMed] [Google Scholar]
- 16.Oberdorster G. Pulmonary effects of inhaled ultrafine particles. Int Arch Occup Environ Health. 2001;74:1–8. doi: 10.1007/s004200000185. [DOI] [PubMed] [Google Scholar]
- 17.Seaton A, MacNee W, Donaldson K, Godden D. Particulate air pollution and acute health effects. Lancet. 1995;345:176–178. doi: 10.1016/S0140-6736(95)90173-6. [DOI] [PubMed] [Google Scholar]
- 18.Brown DM, Wilson MR, MacNee W, Stone V, Donaldson K. Size-dependent proinflammatory effects of ultrafine polystyrene particles: a role for surface area and oxidative stress in the enhanced activity of ultrafines. Toxicol Appl Pharmacol. 2001;175:191–199. doi: 10.1006/taap.2001.9240. [DOI] [PubMed] [Google Scholar]
- 19.Dick CA, Brown DM, Donaldson K, Stone V. The role of free radicals in the toxic and inflammatory effects of four different ultrafine particle types. Inhal Toxicol. 2003;15:39–52. doi: 10.1080/08958370304454. [DOI] [PubMed] [Google Scholar]
- 20.Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, et al. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect. 2003;111:455–460. doi: 10.1289/ehp.6000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gong H, Jr, Linn WS, Clark KW, Anderson KR, Sioutas C, Alexis NE, et al. Exposures of healthy and asthmatic volunteers to concentrated ambient ultrafine particles in Los Angeles. Inhal Toxicol. 2008;20:533–545. doi: 10.1080/08958370801911340. [DOI] [PubMed] [Google Scholar]
- 22.Frampton MW, Stewart JC, Oberdorster G, Morrow PE, Chalupa D, Pietropaoli AP, et al. Inhalation of ultrafine particles alters blood leukocyte expression of adhesion molecules in humans. Environ Health Perspect. 2006;114:51–58. doi: 10.1289/ehp.7962. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Oberdorster G, Oberdorster E, Oberdorster J. Nanotoxicology: an emerging discipline evolving from studies of ultrafine particles. Environ Health Perspect. 2005;113:823–839. doi: 10.1289/ehp.7339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warheit DB, Laurence BR, Reed KL, Roach DH, Reynolds GA, Webb TR. Comparative pulmonary toxicity assessment of single-wall carbon nanotubes in rats. Toxicol Sci. 2004;77:117–125. doi: 10.1093/toxsci/kfg228. [DOI] [PubMed] [Google Scholar]
- 25.Warheit DB, Webb TR, Colvin VL, Reed KL, Sayes CM. Pulmonary bioassay studies with nanoscale and fine quartz particles in rats: toxicity is not dependent upon particle size but on surface characteristics. Toxicol Sci. 2007;95(1):270–280. doi: 10.1093/toxsci/kfl128. [DOI] [PubMed] [Google Scholar]
- 26.Warheit DB, Webb TR, Sayes CM, Colvin VL, Reed KL. Pulmonary instillation studies with nanoscale TiO2 rods and dots in rats: toxicity is not dependent upon particle size and surface area. Toxicol Sci. 2006;91:227–236. doi: 10.1093/toxsci/kfj140. [DOI] [PubMed] [Google Scholar]
- 27.Chen HW, Su SF, Chien CT, Lin WH, Yu SL, Chou CC, et al. Titanium dioxide nanoparticles induce emphysema-like lung injury in mice. FASEB J. 2006;20:2393–2395. doi: 10.1096/fj.06-6485fje. [DOI] [PubMed] [Google Scholar]
- 28.Shvedova AA, Kisin ER, Mercer R, Murray AR, Johnson VJ, Potapovich AI, et al. Unusual inflammatory and fibrogenic pulmonary responses to single-walled carbon nanotubes in mice. Am J Physiol Lung Cell Mol Physiol. 2005;289:L698–L708. doi: 10.1152/ajplung.00084.2005. [DOI] [PubMed] [Google Scholar]
- 29.Vincenti MP, Burrell TA, Taffet SM. Regulation of NF-kappa B activity in murine macrophages: effect of bacterial lipopolysaccharide and phorbol ester. J Cell Physiol. 1992;150:204–213. doi: 10.1002/jcp.1041500127. [DOI] [PubMed] [Google Scholar]
- 30.Ulich TR, Watson LR, Yin SM, Guo KZ, Wang P, Thang H, et al. The intratracheal administration of endotoxin and cytokines. I. Characterization of LPS-induced IL-1 and TNF mRNA expression and the LPS-, IL-1-, and TNF-induced inflammatory infiltrate. Am J Pathol. 1991;138:1485–1496. [PMC free article] [PubMed] [Google Scholar]
- 31.Flanagan PG, Jackson SK, Findlay G. Diagnosis of gram negative, ventilator associated pneumonia by assaying endotoxin in bronchial lavage fluid. J Clin Pathol. 2001;54:107–110. doi: 10.1136/jcp.54.2.107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Martin TR, Rubenfeld GD, Ruzinski JT, Goodman RB, Steinberg KP, Leturcq DJ, et al. Relationship between soluble CD14, lipopolysaccharide binding protein, and the alveolar inflammatory response in patients with acute respiratory distress syndrome. Am J Respir Crit Care Med. 1997;155:937–944. doi: 10.1164/ajrccm.155.3.9117029. [DOI] [PubMed] [Google Scholar]
- 33.Becker S, Fenton MJ, Soukup JM. Involvement of microbial components and toll-like receptors 2 and 4 in cytokine responses to air pollution particles. Am J Respir Cell Mol Biol. 2002;27:611–618. doi: 10.1165/rcmb.4868. [DOI] [PubMed] [Google Scholar]
- 34.Yanagisawa R, Takano H, Inoue K, Ichinose T, Sadakane K, Yoshino S, et al. Enhancement of acute lung injury related to bacterial endotoxin by components of diesel exhaust particles. Thorax. 2003;58:605–612. doi: 10.1136/thorax.58.7.605. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Inoue K, Takano H, Yanagisawa R, Hirano S, Sakurai M, Shimada A, et al. Effects of airway exposure to nanoparticles on lung inflammation induced by bacterial endotoxin in mice. Environ Health Perspect. 2006;114:1325–1330. doi: 10.1289/ehp.8903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Inoue K, Takano H, Ohnuki M, Yanagisawa R, Sakurai M, Shimada A, et al. Size effects of nanomaterials on lung inflammation and coagulatory disturbance. Int J Immunopathol Pharmacol. 2008;21:197–206. doi: 10.1177/039463200802100122. [DOI] [PubMed] [Google Scholar]
- 37.Inoue K, Takano H, Yanagisawa R, Koike E, Shimada A. Size effects of latex nanomaterials on lung inflammation in mice. Toxicol Appl Pharmacol. 2009;234:68–76. doi: 10.1016/j.taap.2008.09.012. [DOI] [PubMed] [Google Scholar]
- 38.Inoue K, Takano H, Koike E, Yanagisawa R, Sakurai M, Tasaka S, et al. Effects of pulmonary exposure to carbon nanotubes on lung and systemic inflammation with coagulatory disturbance induced by lipopolysaccharide in mice. Exp Biol Med (Maywood) 2008;233:1583–1590. doi: 10.3181/0805-RM-179. [DOI] [PubMed] [Google Scholar]
- 39.Inoue KI, Takano H, Yanagisawa R, Hirano S, Kobayashi T, Fujitani Y, et al. Effects of inhaled nanoparticles on acute lung injury induced by lipopolysaccharide in mice. Toxicology. 2007;238(2–3):99–110. doi: 10.1016/j.tox.2007.05.022. [DOI] [PubMed] [Google Scholar]
- 40.Maejima K, Tamura K, Taniguchi Y, Nagase S, Tanaka H. Comparison of the effects of various fine particles on IgE antibody production in mice inhaling Japanese cedar pollen allergens. J Toxicol Environ Health. 1997;52:231–248. doi: 10.1080/00984109708984062. [DOI] [PubMed] [Google Scholar]
- 41.Lambert AL, Dong W, Winsett DW, Selgrade MK, Gilmour MI. Residual oil fly ash exposure enhances allergic sensitization to house dust mite. Toxicol Appl Pharmacol. 1999;158:269–277. doi: 10.1006/taap.1999.8709. [DOI] [PubMed] [Google Scholar]
- 42.Lambert AL, Dong W, Selgrade MK, Gilmour MI. Enhanced allergic sensitization by residual oil fly ash particles is mediated by soluble metal constituents. Toxicol Appl Pharmacol. 2000;165:84–93. doi: 10.1006/taap.2000.8932. [DOI] [PubMed] [Google Scholar]
- 43.Lovik M, Hogseth AK, Gaarder PI, Hagemann R, Eide I. Diesel exhaust particles and carbon black have adjuvant activity on the local lymph node response and systemic IgE production to ovalbumin. Toxicology. 1997;121:165–178. doi: 10.1016/S0300-483X(97)00075-9. [DOI] [PubMed] [Google Scholar]
- 44.Zijverden M, Pijl A, Bol M, Pinxteren FA, Haar C, Penninks AH, et al. Diesel exhaust, carbon black, and silica particles display distinct Th1/Th2 modulating activity. Toxicol Appl Pharmacol. 2000;168:131–139. doi: 10.1006/taap.2000.9013. [DOI] [PubMed] [Google Scholar]
- 45.Last JA, Ward R, Temple L, Pinkerton KE, Kenyon NJ. Ovalbumin-induced airway inflammation and fibrosis in mice also exposed to ultrafine particles. Inhal Toxicol. 2004;16:93–102. doi: 10.1080/08958370490265077. [DOI] [PubMed] [Google Scholar]
- 46.Al-Humadi NH, Siegel PD, Lewis DM, Barger MW, Ma JY, Weissman DN, et al. The effect of diesel exhaust particles (DEP) and carbon black (CB) on thiol changes in pulmonary ovalbumin allergic sensitized Brown Norway rats. Exp Lung Res. 2002;28:333–349. doi: 10.1080/01902140290091976. [DOI] [PubMed] [Google Scholar]
- 47.Inoue K, Takano H, Yanagisawa R, Sakurai M, Ichinose T, Sadakane K, et al. Effects of nano particles on antigen-related airway inflammation in mice. Respir Res. 2005;6:106. doi: 10.1186/1465-9921-6-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Inoue K, Takano H, Yanagisawa R, Sakurai M, Abe S, Yoshino S, et al. Effects of nanoparticles on lung physiology in the presence or absence of antigen. Int J Immunopathol Pharmacol. 2007;20:737–744. doi: 10.1177/039463200702000409. [DOI] [PubMed] [Google Scholar]
- 49.Inoue K, Koike E, Yanagisawa R, Hirano S, Nishikawa M, Takano H. Effects of multi-walled carbon nanotubes on a murine allergic airway inflammation model. Toxicol Appl Pharmacol. 2009;237:306–316. doi: 10.1016/j.taap.2009.04.003. [DOI] [PubMed] [Google Scholar]
- 50.Inoue KI, Yanagisawa R, Koike E, Nishikawa M, Takano H. Repeated pulmonary exposure to single-walled carbon nanotubes exacerbates allergic inflammation of the airway: possible role of oxidative stress. Free Radic Biol Med. 2010;48:924–934. doi: 10.1016/j.freeradbiomed.2010.01.013. [DOI] [PubMed] [Google Scholar]