Abstract
Objective
To assess the prevalence of shoulder pain and its association with the use of assistive devices for mobility in persons with chronic spinal cord injury (SCI).
Design
Cross-sectional analysis conducted within a cohort study.
Setting
SCI service in a hospital and the community.
Participants
Between August 2005 and January 2008, 93 participants with chronic SCI completed a standardized health questionnaire and pain questionnaire.
Main Outcome Measures
Shoulder pain in last 6 months elicited by use of the McGill Pain Questionnaire pain diagram.
Results
Of the 93 participants, 65 (69.9%) reported pain at any site in the 6 months before testing. Shoulder pain, reported by 39.8% of participants, was the third most common site of pain after the legs and back. When stratified by the use of assistive mobility devices, shoulder pain was reported by 46.7% of motorized wheelchair users, 35.4% of manual wheelchair users, 47.6% of participants using aids such as crutch(es) or canes, and 33.3% of participants walking without assistance (P = .7 for comparison of 4 groups).
Conclusions
Shoulder pain is highly prevalent in SCI. The authors of previous studies have largely attributed shoulder pain in SCI to manual wheelchair use. However, our results provide evidence for similarly elevated prevalence of shoulder pain among motorized wheelchair users and those patients using crutches or canes. This finding suggests that in addition to overuse injury from cyclic wheelchair propulsion, the assessment of other mechanical and nonmechanical factors that lead to shoulder pain in SCI is an unmet research need that may have treatment implications.
INTRODUCTION
The shoulder is the most common site of upper extremity pain in patients with chronic spinal cord injury (SCI) [1]. Shoulder pain is associated with lower quality-of-life ratings and physical activity in patients with SCI [2]. In able-bodied patients, shoulder pain is the third most common musculoskeletal complaint (after back and knee pain) and results in annual direct expenses of approximately $7 billion in the United States [3,4].
The authors of previous studies [5–9] have reported that the prevalence of shoulder pain in manual wheelchair users with SCI ranges from 38% to 67%. These authors have attributed shoulder pain to overuse injury resulting from the use of a manual wheelchair. In other articles on this topic, authors have reported on the prevalence of shoulder pain stratified by severity of SCI to be 33% to 70% [10,11]. Some authors have provided data on only the overall prevalence of shoulder pain in patients with SCI (33%–63%) [1,12–16]. However, patients with SCI use various modes for ambulation (eg, motorized wheelchairs, cane[s], or crutches and independent mobility) in addition to hand-propelled wheelchairs. The association between modes of ambulation (mobility) and shoulder pain in SCI has not been previously reported. We hypothesized that patients with SCI who use ambulatory devices or modes other than a manual wheelchair also experience significant shoulder pain because of biomechanical muscle imbalance. This cross-sectional analysis was intended to generate hypotheses to be evaluated in subsequent studies that use prospective designs and permit stronger inferences.
MATERIALS AND METHODS
Patient Population
Since 1994 we have been enrolling a chronic SCI cohort recruited from the VA Boston SCI Service and from the Greater Boston area by advertisement, as has been described previously [17]. A recruitment criterion that patients had lived with SCI for more than 1 year was selected to ensure that participants survived acute injury and related complications. Participants requiring mechanical ventilation or tracheostomy were excluded. At study entry, participants had to be free of acute illness. They completed a detailed health questionnaire and underwent a neurological examination.
In August 2005, we introduced a pain questionnaire that was administered to the participants during their study visit. Participants (n = 94) tested between August 2005 and January 2008 were included in our study. One participant with missing data on the pain questionnaire (described in the section “Pain and Mobility Questionnaires”) was excluded. The final dataset for analysis included 93 participants. The study was approved by the Institutional Review Boards at VA Boston Healthcare System, Brigham and Women’s Hospital, and Harvard Medical School, and informed consent was obtained from each participant.
Neurological Examination
The assessment of motor level and completeness of injury was performed at the same time as other questionnaires were administered and based on American Spinal Injury Association (ASIA) Impairment Scale (AIS) [18]. Motor level and completeness of injury was determined by examination. Participants were a priori grouped into 1 of 7 motor injury levels and severity groups. Because complete C5 is the highest level of SCI where the use of a manual wheelchair is possible (although difficult) [19], we classified complete tetraplegia in our study into C3-C4 (few persons were in this group because those on mechanical ventilation were excluded) and C5-C8. Other neurologically complete groups included motor complete T1-T6 and T7-T12. Participants with motor incomplete SCI (AIS C, the majority of key muscles below the neurological level grade <3/5; or AIS D, at least one-half of the key muscles grade ≥3/5) were grouped into cervical AIS C and D; T1-T12 AIS C and D; and lumbar and sacral AIS complete and incomplete.
Pain and Mobility Questionnaires
To assess mobility, participants were asked “how you usually get around” and given the following options: motorized wheelchair more than half the time; hand-propelled wheelchair more than half the time; walk with aid more than half the time; and walk without assistance more than half the time.
To assess pain, participants were asked whether they experienced pain in the last 6 months. They were then asked to indicate the site of their pain from one of the following: head, neck, shoulders, hands, chest, abdomen, genitals, back, buttocks, thighs, legs, and feet. These sites were based on the pain diagram in the McGill Pain Questionnaire [20].
Statistical Analysis
We examined the prevalence of pain at various sites in participants with SCI and stratified prevalence of shoulder pain by mobility. We compared the prevalence of shoulder pain across mobility groups and level and severity of SCI by using the χ2 test. Logistic regression was used to assess whether mobility was associated with shoulder pain, with an adjustment for age and gender. We considered a P value of <.05 to be statistically significant. We performed statistical analysis by using SAS for Windows (version 9.2) from SAS Institute Inc. (Cary, NC).
RESULTS
The mean age of participants in our study was 53.6 ± 15.1 years (Table 1). Because this cohort comprised mostly veterans, most participants (93.6%) were men. Incomplete tetraplegia formed the largest group of participants in our study (31.2%). Twelve (12.9%) participants had complete tetraplegia.
Table 1.
Baseline characteristics of 93 participants with SCI
| Characteristics | |
|---|---|
| Age in years, mean ± SD | 53.6 ± 15.1 |
| Gender | |
| Male, n (%) | 87 (93.6) |
| Motor level and severity of SCI*† | |
| C3-C4 AIS complete | 3 (3.2) |
| C5-C8 AIS complete | 9 (9.7) |
| T1-T6 AIS complete | 8 (8.6) |
| T7-T12 AIS complete | 10 (10.8) |
| Cervical AIS C and D | 29 (31.2) |
| Thoracic AIS C and D | 22 (23.7) |
| Lumbar and sacral AIS complete and incomplete | 12 (12.9) |
AIS = ASIA Impairment Scale; SCI = spinal cord injury.
As per American Spinal Injury Association Impairment Scale (AIS)
Expressed as n (%).
Of the 93 participants, 65 (69.9%) reported pain at one of the sites in the 6 months before testing. The most common sites of musculoskeletal pain in our study included legs (47%), back (45%), shoulder (40%), feet (39%), and hands (30%) (Figure 1; Table 2). No differentiation between neuropathic and musculoskeletal pain was made.
Figure 1.
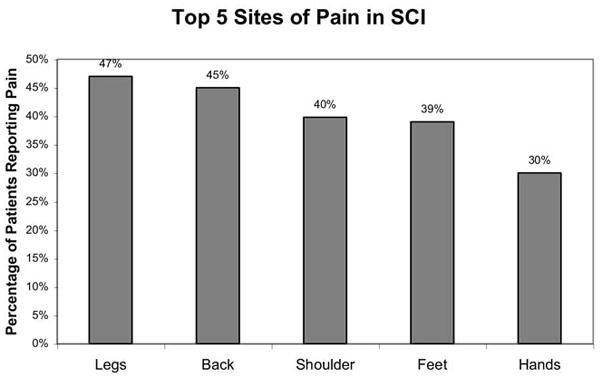
Pain sites in participants with SCI in 6 months before interview. SCI = spinal cord injury.
Table 2.
Musculoskeletal pain sites in 93 participants with SCI
| Pain Sites | Mobility Device* |
|||
|---|---|---|---|---|
| Motorized Wheelchair† (n = 15) | Manual Wheelchair† (n = 48) | Crutch or Cane† (n = 21) | No Device† (n = 9) | |
| Neck | 6 (40) | 12 (25) | 8 (38) | 2 (22) |
| Shoulder | 7 (46.7)† | 17 (35.4)† | 10 (47.6)† | 3 (33.3)† |
| Arms | 5 (33) | 13 (27) | 8 (38) | 2 (22) |
| Hands | 7 (47) | 13 (27) | 7 (33) | 2 (22) |
| Back | 6 (40) | 18 (38) | 13 (62) | 5 (56) |
| Buttocks | 4 (27) | 11 (23) | 4 (19) | 1 (11) |
| Thighs | 6 (40) | 11 (23) | 9 (43) | 1 (11) |
| Legs | 6 (40) | 18 (38) | 14 (67) | 6 (67) |
| Feet | 4 (27) | 16 (33) | 12 (57) | 4 (44) |
SCI = spinal cord injury.
Expressed as n (%).
Significant.
Of the 65 participants who reported pain in the 6 months before testing, 37 (56.9%) reported shoulder as one of the sites of pain. Therefore, the overall prevalence of shoulder pain in our cohort was 39.8%. Participants using crutch(es) or canes (47.6%; 95% confidence interval [95% CI] 26.3%–69.0%) and patient using motorized wheelchairs (46.7%; 95% CI 21.4%–71.9%) reported the greatest prevalence of shoulder pain. The prevalence of shoulder pain in participants using manual wheelchairs was less and similar to the prevalence of participants ambulating independently (35.4%; 95% CI 6.9%–49.0% versus 33.3%; 95% CI 2.5%–64.1%). The 4 groups were not statistically different (P = .7). The 4 mobility groups were not statistically different when logistic regression was performed and adjusted for age and gender (data not presented because of small sample size, which resulted in wide confidence intervals).
None of the participants with C5 and C6 complete tetraplegia used manual wheelchairs. The highest level that a participant using a manual wheelchair scored in our study was C7 complete tetraplegia. When stratified by motor level and severity, participants with motor complete C5-C8 SCI (55.6%) and incomplete thoracic (50%) had the greatest prevalence of shoulder pain (Table 3).
Table 3.
Shoulder pain by AIS motor level and severity of SCI in 93 participants
| Motor Level and Severity of Injury | Total Number of Participants | Participants with Shoulder Pain* |
|---|---|---|
| C3-C4 AIS complete | 3 | 1 (33.3) |
| C5-C8 AIS complete | 9 | 5 (55.6) |
| T1-T6 AIS complete | 8 | 3 (37.5) |
| T7-T12 AIS complete | 10 | 3 (30.0) |
| Cervical AIS C and D | 29 | 12 (41.4) |
| Thoracic AIS C and D | 22 | 11 (50.0) |
| Lumbar and sacral AIS complete and incomplete | 12 | 2 (16.7) |
P = .5 for comparison of 4 groups.
AIS = ASIA Impairment Scale; SCI = spinal cord injury.
Expressed as n (%).
DISCUSSION
We assessed the prevalence of shoulder pain in SCI and its association with the mode of ambulation including hand-propelled wheelchairs. Shoulder pain was highly prevalent in SCI with an overall prevalence of 39.8%. The authors of most studies did not report on the association between mobility devices and shoulder pain and did not stratify patients who used motorized wheelchairs or manual wheelchairs. We found that shoulder pain in SCI was not limited to patients who used a manual wheelchair.
The authors of previous studies [1,6–12,14,16,21–24] have reported a wide range of prevalence of shoulder pain in SCI (33%–67%). The reasons for these variations include the different definitions of shoulder pain used (acute episode versus chronic occurrence). There were variations in survey methodology, including in-person questionnaires, structured versus unstructured interviews, and mail surveys. The study populations also varied from investigations that were limited to wheelchair athletes [23] to studies that surveyed SCI populations in the community [12]. Our study included persons exhibiting a range of injury levels and severity and with a range of mobility modes.
Brose et al [6] reported a 67% prevalence of shoulder pain in 49 wheelchair users with chronic SCI (28.6% with tetraplegia and 67.3% with paraplegia) who participated in the National Veteran Wheelchair Games. Curtis et al [7] reported on 195 patients with SCI who used manual wheelchairs. Fewer than 15% of participants reported shoulder pain before using wheelchairs, whereas 59% of participants with tetraplegia and 42% with paraplegia reported current shoulder pain. Gironda et al [12] performed a mail survey among manual and motorized wheelchair users with SCI and reported that 83% of participants had experienced shoulder pain at some point since they began using wheelchairs. Nichols et al [14] reported a 51.4% prevalence of shoulder pain in 708 members of Spinal Cord Injuries Association and associated shoulder pain with wheelchair use and transfers.
Ballinger et al [25] conducted a study of 89 men and reported that among participants with shoulder pain, 3.7% had high tetraplegia (C4 and higher AIS A or AIS B who would not be expected to use a manual wheelchair, and C4 and higher AIS B and C injuries); 48.1% had low tetraplegia (C5 and below AIS A, B, and C injuries), 40.7% had AIS A, B, and C paraplegia; and 7.4% had AIS D injuries as compared with participants without shoulder pain, where 4.8% participants had high tetraplegia, 35.5% had low tetraplegia, 46.8% had paraplegia, and 12.9% had AIS D injuries. Participants with C4 and higher complete injuries would not be expected to use a manual wheelchair. Turner et al [26] conducted a study in 294 participants with SCI and reported that 132 (45%) patients had shoulder pain. When stratified by level of injury, the prevalence of shoulder pain was greater in higher levels and linearly decreased in lower levels of injury. We found that participants with AIS complete and incomplete SCI had a high prevalence of shoulder pain and that differences between groups by level and severity of SCI were not statistically significant.
The prevalence of shoulder pain stratified by mode of ambulation has not been previously reported. We found that shoulder pain was more prevalent in those patient using crutch(es) and canes and those using motorized wheelchairs as compared with those using manual wheelchairs. However, these differences did not reach statistical significance possibly because of our modest sample size. Our study provides data in contradiction to the conventional hypothesis that the primary concern for shoulder disorders and symptomatology in SCI is among manual wheelchair users [5–9]. It is likely that factors other than or in addition to the use of manual wheelchairs, such as the excessive use of the upper extremities for activities of daily living, transfers, ischial pressure relief, and reaching from a seated position in a wheelchair leads to upper extremity injury. It is also likely that biomechanical changes in the musculature as the result of neurologic weakness or muscle plasticity in SCI leads to shoulder pain. It is possible that some patients using motorized wheelchairs in our cohort were prompted to do so because of shoulder pain in the past when using other assistive devices for mobility. Shoulder pain may have existed in the years before the use of a motorized wheelchair, but this possibility was not investigated. Another possibility is that patients with primary neurological disorders are at risk for chronic generalized pain syndromes. However our data did not permit us to address this hypothesis with sufficient rigor.
The investigation of cause of shoulder pain is an unmet need in SCI and will help guide treatment. There are many causes of shoulder pain in SCI related to shoulder pathology, including rotator cuff tears, labral tears, and osteoarthritis of the glenohumeral joint. Shoulder pain may also result from nonshoulder-related pathology such as cervical radiculopathy and heterotopic ossification [27]. A few smaller studies and case series have described the etiology of shoulder pain in SCI. Campbell and Koris [22] studied 13 patients and reported that anterior instability was the cause in 5 patients, multidirectional instability in 3 shoulders, capsular contracture/capsulitis in 3, and other diagnoses comprised the remaining 2 patients. Escobedo et al [28] found evidence for rotator cuff tears on magnetic resonance imaging in 73% of their SCI population. A recent case-control study was conducted between persons with paraplegia who had been using wheelchairs for at least 30 years and able-bodied control patients [21]. It was not specified whether those using motorized wheelchairs were excluded. The authors reported that the prevalence of rotator cuff tears was 4 times greater (63% versus 15%) in patients with paraplegia as compared with the able-bodied control patients.
We did not have imaging and standardized questionnaire and physical examination data that would assist in understanding the etiology of shoulder pain in SCI. These are potential areas of research for future work. Another limitation of our study is a relatively small sample size of 93 participants, including few female patients; therefore, it is an exploratory analysis. Longitudinal studies are needed to strengthen causal inference and exclude bias caused by previous shoulder problems leading to the use of a motorized chair.
CONCLUSION
The overall prevalence of shoulder pain in SCI is high. Most researchers have previously focused on wheelchair propulsion as a cause of shoulder pain in SCI and patients with SCI not using wheelchairs have been excluded from many studies. Although manual wheelchair use may be one of the predisposing factors for shoulder-related pathology in SCI, our data provide evidence that those patients not using manual wheelchairs may be at similar or greater risk for shoulder disorders leading to shoulder pain.
Acknowledgments
Research associated with this article was completed with resources provided within the VA Boston Healthcare System. Supported by the Department of Veterans Affairs, Veterans Health Administration, Rehabilitation Research and Development Service (Merit Review Grant B6618R), and National Institute of Child Health and Human Development (RO1 HD042141).
Footnotes
N.B.J. Disclosure: nothing to disclose
L.D.H. Disclosure: nothing to disclose
J.N.K. Disclosure: nothing to disclose
E.G. Disclosure: nothing to disclose
This study was presented as an abstract at the American Academy of Physical Medicine and Rehabilitation annual meeting in Austin in 2009.
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the United States government.
Contributor Information
Nitin B. Jain, Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital, 125 Nashua St, Boston, MA 02114; and Orthopedic and Arthritis Center for Outcomes Research, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA.
Laurence D. Higgins, Department of Orthopedic Surgery, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA.
Jeffrey N. Katz, Orthopedic and Arthritis Center for Outcomes Research and Department of Orthopedic Surgery, Brigham and Women’s Hospital and Harvard Medical School, Boston, MA; Division of Rheumatology, Immunology, and Allergy, Brigham and Women’s Hospital.
Eric Garshick, Pulmonary and Critical Care Medicine Section, Medical Service, VA Boston Health-care System; and Channing Laboratory, Department of Medicine, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA.
References
- 1.Dalyan M, Cardenas DD, Gerard B. Upper extremity pain after spinal cord injury. Spinal Cord. 1999;37:191–195. doi: 10.1038/sj.sc.3100802. [DOI] [PubMed] [Google Scholar]
- 2.Gutierrez DD, Thompson L, Kemp B, Mulroy SJ. The relationship of shoulder pain intensity to quality of life, physical activity, and community participation in persons with paraplegia. J Spinal Cord Med. 2007;30:251–255. doi: 10.1080/10790268.2007.11753933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Meislin RJ, Sperling JW, Stitik TP. Persistent shoulder pain: Epidemiology, pathophysiology, and diagnosis. Am J Orthop (Belle Mead NJ) 2005;34:5–9. [PubMed] [Google Scholar]
- 4.Rekola KE, Keinanen-Kiukaanniemi S, Takala J. Use of primary health services in sparsely populated country districts by patients with musculoskeletal symptoms: Consultations with a physician. J Epidemiol Community Health. 1993;47:153–157. doi: 10.1136/jech.47.2.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alm M, Saraste H, Norrbrink C. Shoulder pain in persons with thoracic spinal cord injury: Prevalence and characteristics. J Rehabil Med. 2008;40:277–283. doi: 10.2340/16501977-0173. [DOI] [PubMed] [Google Scholar]
- 6.Brose SW, Boninger ML, Fullerton B, et al. Shoulder ultrasound abnormalities, physical examination findings, and pain in manual wheelchair users with spinal cord injury. Arch Phys Med Rehabil. 2008;89:2086–2093. doi: 10.1016/j.apmr.2008.05.015. [DOI] [PubMed] [Google Scholar]
- 7.Curtis KA, Drysdale GA, Lanza RD, Kolber M, Vitolo RS, West R. Shoulder pain in wheelchair users with tetraplegia and paraplegia. Arch Phys Med Rehabil. 1999;80:453–457. doi: 10.1016/s0003-9993(99)90285-x. [DOI] [PubMed] [Google Scholar]
- 8.Finley MA, Rodgers MM. Prevalence and identification of shoulder pathology in athletic and nonathletic wheelchair users with shoulder pain: A pilot study. J Rehabil Res Dev. 2004;41:395–402. doi: 10.1682/jrrd.2003.02.0022. [DOI] [PubMed] [Google Scholar]
- 9.Samuelsson KA, Tropp H, Gerdle B. Shoulder pain and its consequences in paraplegic spinal cord-injured, wheelchair users. Spinal Cord. 2004;42:41–46. doi: 10.1038/sj.sc.3101490. [DOI] [PubMed] [Google Scholar]
- 10.Salisbury SK, Choy NL, Nitz J. Shoulder pain, range of motion, and functional motor skills after acute tetraplegia. Arch Phys Med Rehabil. 2003;84:1480–1485. doi: 10.1016/s0003-9993(03)00371-x. [DOI] [PubMed] [Google Scholar]
- 11.Silfverskiold J, Waters RL. Shoulder pain and functional disability in spinal cord injury patients. Clin Orthop Relat Res. 1991:141–145. [PubMed] [Google Scholar]
- 12.Gironda RJ, Clark ME, Neugaard B, Nelson A. Upper limb pain in a national sample of veterans with paraplegia. J Spinal Cord Med. 2004;27:120–127. doi: 10.1080/10790268.2004.11753742. [DOI] [PubMed] [Google Scholar]
- 13.Nepomuceno C, Fine PR, Richards JS, et al. Pain in patients with spinal cord injury. Arch Phys Med Rehabil. 1979;60:605–609. [PubMed] [Google Scholar]
- 14.Nichols PJ, Norman PA, Ennis JR. Wheelchair user’s shoulder? Shoulder pain in patients with spinal cord lesions. Scand J Rehabil Med. 1979;11:29–32. [PubMed] [Google Scholar]
- 15.Sie IH, Waters RL, Adkins RH, Gellman H. Upper extremity pain in the postrehabilitation spinal cord injured patient. Arch Phys Med Rehabil. 1992;73:44–48. [PubMed] [Google Scholar]
- 16.Subbarao JV, Klopfstein J, Turpin R. Prevalence and impact of wrist and shoulder pain in patients with spinal cord injury. J Spinal Cord Med. 1995;18:9–13. doi: 10.1080/10790268.1995.11719374. [DOI] [PubMed] [Google Scholar]
- 17.Grandas NF, Jain NB, Denckla JB, et al. Dyspnea during daily activities in chronic spinal cord injury. Arch Phys Med Rehabil. 2005;86:1631–1635. doi: 10.1016/j.apmr.2005.02.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Marino RJ, Barros T, Biering-Sorensen F, et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med. 2003;26(Suppl 1):S50–S56. doi: 10.1080/10790268.2003.11754575. [DOI] [PubMed] [Google Scholar]
- 19.Consortium for Spinal Cord Injury Medicine. Expected outcomes: What you should know. [Accessed May 24, 2010];A guide for people with C5 spinal cord injury. 2010 Available at: http://www.scicpg.org/cpg_cons_pdf/OC5.pdf.
- 20.Melzack R. The short-form McGill Pain Questionnaire. Pain. 1987;30:191–197. doi: 10.1016/0304-3959(87)91074-8. [DOI] [PubMed] [Google Scholar]
- 21.Akbar M, Balean G, Brunner M, et al. Prevalence of rotator cuff tear in paraplegic patients compared with controls. J Bone Joint Surg Am. 2010;92:23–30. doi: 10.2106/JBJS.H.01373. [DOI] [PubMed] [Google Scholar]
- 22.Campbell CC, Koris MJ. Etiologies of shoulder pain in cervical spinal cord injury. Clin Orthop Relat Res. 1996:140–145. [PubMed] [Google Scholar]
- 23.Curtis KA, Black K. Shoulder pain in female wheelchair basketball players. J Orthop Sports Phys Ther. 1999;29:225–231. doi: 10.2519/jospt.1999.29.4.225. [DOI] [PubMed] [Google Scholar]
- 24.Jensen MP, Hoffman AJ, Cardenas DD. Chronic pain in individuals with spinal cord injury: A survey and longitudinal study. Spinal Cord. 2005;43:704–712. doi: 10.1038/sj.sc.3101777. [DOI] [PubMed] [Google Scholar]
- 25.Ballinger DA, Rintala DH, Hart KA. The relation of shoulder pain and range-of-motion problems to functional limitations, disability, and perceived health of men with spinal cord injury: A multifaceted longitudinal study. Arch Phys Med Rehabil. 2000;81:1575–1581. doi: 10.1053/apmr.2000.18216. [DOI] [PubMed] [Google Scholar]
- 26.Turner JA, Cardenas DD, Warms CA, McClellan CB. Chronic pain associated with spinal cord injuries: A community survey. Arch Phys Med Rehabil. 2001;82:501–509. doi: 10.1053/apmr.2001.21855. [DOI] [PubMed] [Google Scholar]
- 27.Kirshblum S. New rehabilitation interventions in spinal cord injury. J Spinal Cord Med. 2004;27:342–350. doi: 10.1080/10790268.2004.11753772. [DOI] [PubMed] [Google Scholar]
- 28.Escobedo EM, Hunter JC, Hollister MC, Patten RM, Goldstein B. MR imaging of rotator cuff tears in individuals with paraplegia. AJR Am J Roentgenol. 1997;168:919–923. doi: 10.2214/ajr.168.4.9124140. [DOI] [PubMed] [Google Scholar]


