Abstract
Background:
Activins and inhibins belong to the TGFβ-superfamily, which controls cell proliferation and differentiation in many organs. Activin A, the dimer of inhibin βA subunit, acts strongly anti-proliferative in hepatocytes. Little is known on the other activin/inhibin subunits in human liver and hepatocellular carcinoma (HCC).
Methods:
We studied the expression of the complete inhibin family α, βA, βB, βC, βE in normal liver, tumour-adjacent and HCC tissue, 12 additional organs and rodent liver. A total of 16 HCC and 10 disease-free livers were analysed. Expression of inhibin subunits was determined by qRT–PCR, normalised to RNA input and by geNorm algorithm, and confirmed by immunohistochemistry.
Results:
Remarkably, βA expression was not decreased in HCC. Similarly, βC and βE exhibited no major changes. In contrast, inhibin α, barely detectable in normal liver, was strongly increased in tumour-adjacent liver and dramatically enhanced in HCC. βB was strongly enhanced in some HCC. At variance with human liver, rodent liver showed higher inhibin α and βC expression, but βA was somewhat, and βB dramatically lower.
Conclusions:
Upregulation of inhibin α – and possibly of βB – may shield HCC cells from anti-proliferative effects of activin A. Dramatic variations between humans and rodents may reflect different functions of some inhibins/activins.
Keywords: inhibin, activin, hepatocellular carcinoma, real-time PCR
Liver cancer is among the leading causes of cancer deaths worldwide. It is characterised by deregulation of proliferation and apoptosis of hepatocytes and usually develops on the basis of chronic tissue inflammation leading to fibrosis and cirrhosis (Grasl-Kraupp et al, 2000; Drucker et al, 2006; Seitz and Stickel, 2006; Herzer et al, 2007). The underlying molecular mechanisms are barely understood (Strand et al, 1996; Laurent-Puig and Zucman-Rossi, 2006; Macheiner et al, 2006). Their elucidation is critical for the development of improved therapies for liver cancer (Schulte-Hermann et al, 1997; Llovet et al, 2003; El-Serag and Rudolph, 2007).
Activin and inhibin proteins are members of the TGFβ superfamily, which controls cell proliferation, apoptosis, inflammation and differentiation in many cell types and organs including the liver (De Bleser et al, 1997; Schulte-Hermann et al, 1997; Rodgarkia-Dara et al, 2006; Deli et al, 2008). The mammalian inhibin family includes one α- (INHA) and four β-genes (INHBA, INHBB, INHBC and INHBE). Gene products dimerise to form inhibin and activin proteins. Inhibins are heterodimers consisting of the α-subunit and one β-subunit, forming inhibin A (α-βA) and inhibin B (α-βB). Activins are homodimers (activin A=βA–βA, activin B, C and E) or heterodimers (e.g., activin AB=βA–βB) of two β-subunits (Grusch et al, 2007). At the mRNA level, INHA is most prominently expressed in ovary, testis, adrenal and pituitary gland but reportedly not detectable in human and rodent liver (Meunier et al, 1988; Tuuri et al, 1994). Expression of INHBA mRNA is usually high and found in many organs including the liver. Similarly, INHBB mRNA has been detected in many organs but in rodent liver low or undetectable levels or only transient appearance on diverse treatments were reported (De Bleser et al, 1997; Kobayashi et al, 2000, 2002; Vejda et al, 2002; Jones et al, 2007). In contrast, INHBC and INHBE expression levels are highest in the liver, much lower in testis, adrenal and pituitary gland and almost undetectable in other organs of rodents (Fang et al, 1997; Vejda et al, 2002; Gold et al, 2004). In human tissues, comparisons of INHBB, INHBC and INHBE expression apparently have not been reported.
The resulting activin proteins may have important functions in the human liver, which are, however, still unknown except for activin A. Activin A is considered a key inhibitor of liver growth (Yasuda et al, 1993; Xu et al, 1995; Zauberman et al, 1997), whereas the so-called liver-specific activin C and activin E were reported to either promote (Wada et al, 2004, 2005) or inhibit hepatocyte proliferation (Chabicovsky et al, 2003; Vejda et al, 2003). After partial hepatectomy in mice nulled for INHBC, or INHBE and or for both no alterations in liver regeneration was observed (Lau et al, 2000). Studies on expression of INHBC and INHBE mRNA during liver regeneration after partial hepatectomy (Esquela et al, 1997; Zhang et al, 1997; Kogure et al, 1998; Lau et al, 2000; Gold et al, 2005; Takamura et al, 2005; Wada et al, 2005), or chemical injury (Kobayashi et al, 2002; Gold et al, 2003; Grusch et al, 2006) in rodents produced conflicting data on possible biological functions as reviewed recently (Grusch et al, 2007). Most of the information available were gathered in rodent liver and rarely confirmed in humans (Tuuri et al, 1994).
Recently, we reported that INHBA and INHBE were downregulated in chemically induced hepatocarcinogenesis in rats (Grusch et al, 2006). However, in patients with cirrhosis and hepatocellular carcinoma (HCC) elevated levels of serum activin A were observed and were suggested as biomarkers of liver disease (Pirisi et al, 2000; Yuen et al, 2002). Similarly, in several other malignancies deregulation of inhibin and activin at the mRNA and protein level is a common event, including tumours of endometrial (Worbs et al, 2007), adrenocortical (Salmenkivi et al, 2001; Hofland et al, 2006, 2007) and gonadal stromal origin (Fuller et al, 1999; Fine and Li, 2003; Ciris et al, 2004).
Consequently, in this study we analysed by qRT–PCR mRNA expression patterns of the inhibin family in human liver, HCC-adjacent fibrotic/cirrhotic tissue, and HCC. For comparison, inhibin expression patterns were also analysed in additional human tissues and in mouse and rat liver. To our knowledge, this is the first analysis of the entire inhibin family in human liver and HCC. To overcome problems resulting from uneven expression of reference genes in normal, tumour-adjacent and malignant tissue, we standardised gene expression by referring to total RNA input and by normalisation with the geNorm protocol. The results provide a distinct molecular expression portrait of the inhibin gene family in disease-free liver, HCC, other organs and rodent liver. Unexpectedly, INHA, barely detectable in disease-free liver, was strongly elevated in most HCC samples. INHBB, extremely low in rat liver, was highly expressed in human liver and further upregulated in most HCC. These results provide important new clues to functions of the inhibin/activin family in liver and HCC.
Materials and methods
Tissue samples
A total of 16 HCC (tumour, T) and tumour-adjacent (non-tumour, NT) liver samples, plus 5 normal (N) liver specimens were obtained from patients of the General Hospital, Vienna, in the Austrian ‘Gen-Au Programme’ (Macheiner et al, 2006; Sagmeister et al, 2008). Patient information's are listed in Table 1. Written informed consent was obtained from each patient. Additionally, 5 RNA samples were purchased, providing overall 10 normal liver specimens.
Table 1. Characteristics of controls and HCC patients.
| Controls (normal liver) | HCC patients | |
|---|---|---|
| Number | 10 | 16 |
| Sex | ||
| Female | 4 | 6 |
| Male | 6 | 10 |
| Age at operation | ||
| Mean±s.d. | 50.5±6.6 | 63.4±12.4 |
| Range | 45–64 | 43-78 |
| HBV infected | 0/10 | 0/16 (0%) |
| HCV infected | 0/10 | 5/16 (31%) |
Abbreviations: HBV=Hepatitis B virus; HCC=hepatocellular carcinoma; HCV=Hepatitis C virus.
All cancer samples contained at least 80% tumour cells as shown by histology. In all, 6 tumours were classified as stage I, 7 as stage II, 1 as stage III and 2 as stage IV, and histological grading was 2 HCC-1, 13 HCC-2 and 1 HCC-3, according to AJCC/UICC standards and (Edmondson and Steiner, 1954). Hepatocellular carcinoma-adjacent tissue was cirrhotic in seven cases and fibrotic in nine cases. Human RNA from normal liver and 12 additional organs was from BioCat (Heidelberg, Germany), Clontech (Mountain View, CA, USA) and Stratagene/Agilent Genomics (Santa Clara, CA, USA). Liver samples from C57BL/6 mice and Wistar rats were obtained as described (Grusch et al, 2006).
In total, 5 out of 16 samples described above were available for immunhistochemical analyses. In addition, a commercially available HCC tissue array (Biochain, Hayward, CA, USA) was used. This array contains 16 pairs of tumour and adjacent tissue sections (1 stage I and 15 stage II tumours). A human ovarian granulosa cell tumour (Biogenex , Fremont, CA, USA) served as positive control for inhibin α.
RNA isolation
Total RNA was isolated using TRIzol reagent (Invitrogen/Life Technologies, Carlsbad, CA, USA) according to the manufacturer's instructions. Tissue samples were prepared using a homogeniser (Bertin Technologies, Montigny-le-Bretonneux, France). High quality of RNA samples were carefully controlled on GenQuant (Pharmacia/GE Healthcare Life Science, Stockholm, Sweden). All samples of RNA were protein free as indicated by absorbance ratio 260/280 nm of 1.8–2.1. The mean error of triplicate measurements of RNA concentration of all samples (n=42) was 8.0%. The integrity of all RNA samples was confirmed electrophoretically on 1.5% agarose gel (data not shown).
Reverse transcription and quantitative real-time PCR
Two micrograms of total RNA was reverse transcribed with MMLV RevertAid (Fermentas/Thermo Scientific, St Leon-Roth, Germany) resulting in 100 μl cDNA solution. In all, 2 μl cDNA solution was used as template for each PCR. Real-time analysis was performed with TaqMan Universal PCR Master Mix (Applied Biosystems/Life Technologies, Carlsbad, CA, USA) on an ABI Prism 7000 Sequence Detection System (Applied Biosystems/Life Technologies) running the following protocol: initial 50 °C for 2 min and 95 °C for 10 min, and 40 repeats of 95 °C for 15 s, 60 °C for 1 min. Taqman assays used in this study are listed in Supplementary Table 1. All samples were analysed in duplicate and in at least two independent real-time PCR runs. The intra-assay mean error was 0.16% and the inter-assay mean error 1.24%.
Calculation of expression data
Original (raw) cycle threshold values Ct refer to 100 ng of total high quality RNA input (designated ‘normalised to RNA input’). They were transformed by the following procedures. For each gene, the median Ct value of data from normal liver samples (n=10) was used as calibrator. Each single sample Ct value was logarithmically transformed, calculated by the formula 2−(calibrator–sample), and expressed as fold change vs the median of disease-free liver Ct. For normalisation with reference genes, samples were transformed as described (Vandesompele et al, 2002). As expression of standard reference genes in normal and malignant liver showed large variations, we determined the most stable one using geNorm applet. For normalisation, the transformed data of inhibin genes were divided by the respective normalisation factors (NFs). The following genes were used for normalisation: for N samples B2M, ACTB and HPRT, for NT and T samples GAPDH, HPRT and TBP (additional information in Supplementary Figure 1). Subsequently, data from NT and T samples were normalised by using NF. The median of normalised data from disease-free liver samples was used as calibrator and set 1. Two different sets of NF were obtained by either assuming NT and T samples as one group, referred to as ‘NF jointly’, or as separate subgroups NT and T, referred to as ‘NF separately’. Changes in expression levels in NT and T from HCC patient's normalised by geNorm or to RNA input are compared in Table 2.
Table 2. Changes in expression of inhibin genes in tumour-adjacent and HCC samples calculated with different normalisation methods.
|
Normalised to RNA input
|
NF separately
|
NF jointly
|
||||
|---|---|---|---|---|---|---|
| NT | T | NT | T | NT | T | |
| INHA | 9.0±2.9 | 225±148 | 6.2±3.3 | 140±83 | 5.1±2.1 | 357±291 |
| 3.7 | 10.9 | 2.3 | 8.6 | 2.3 | 8.9 | |
| Wmp*, MW–NT*, MW–T** | Wmp**, MW–T* | Wmp**, MW–T* | ||||
| INHBA | 0.61±0.14 | 1.9±0.46 | 0.68±0.17 | 6.3±3.7 | 0.77±0.20 | 3.9±1.4 |
| 0.56 | 0.97 | 0.55 | 2.3 | 0.63 | 1.8 | |
| Wmp* | Wmp** | Wmp** | ||||
| INHBB | 4.0±1.7 | 12±4.0 | 2.5±1.0 | 30±19 | 2.8±1.2 | 16±7.6 |
| 1.23 | 4.3 | 0.64 | 3.5 | 0.72 | 4.3 | |
| Wmp* | Wmp** | Wmp** | ||||
| INHBC | 1.3±0.51 | 1.7±0.52 | 1.1±0.38 | 3.4±1.5 | 1.3±0.43 | 2.2±0.64 |
| 0.73 | 0.98 | 0.71 | 1.3 | 0.81 | 1.4 | |
| — | — | — | ||||
| INHBE | 1.2±0.33 | 3.1±1.6 | 0.80±0.33 | 3.1±1.1 | 0.90±0.37 | 2.0±0.72 |
| 0.94 | 1.7 | 0.40 | 0.76 | 0.46 | 0.65 | |
| Wmp* | Wmp** | — | ||||
Abbreviations: HCC=hepatocellular carcinoma; MW–NT=Mann–Whitney U-test comparing N and NT samples; MW–T=Mann–Whitney U test comparing N and T samples; N=normal; NF=normalisation factor; NT=non-tumour; T=tumour; Wmp, Wilcoxon matched pair test comparing NT and T samples.
*P-value <0.05; **P-value <0.01.
Values are given relative to the median mRNA expression value in normal liver tissue as means±s.e.m. (first row) and medians (second row).
For species and tissue comparisons, Ct values normalised to RNA input were used. The results from the lowest expressing tissues were set 1 after logarithmical transformation. Results from all other samples were expressed as fold change.
Statistical analysis
All statistical analyses were performed using GraphPad Prism 4.0 for Windows (http://www.graphpad.com). Data of all three groups (N, NT and T) were analysed by Kruskal–Wallis test. Significance of differences between medians of non-paired groups (N and NT, N and T) was checked using the non-parametric Mann–Whitney U-tests. Results from paired NT and T samples were analysed by the non-parametric Wilcoxon matched pair test. Correlation between gene expression levels and ratios was checked by the Spearman ranked test. All tests were performed as two-tailed and statistical significance was assumed at P<0.05.
Immunohistochemistry
Histological staining was performed as previously described (Grusch et al, 2006). In brief, tissue samples were fixed in 4% buffered formalin, embedded in paraffin, 2 μm sections were deparaffinised and antigen-retrieval was done by heating in 0.01 M citrate buffer, pH 6.0. Sections were incubated overnight at 4 °C in 0.1% BSA/PBS with primary antibodies against inhibin α-subunit (clone R1, LabVision/Neomarkers/Thermo Scientific, Fremont, CA, USA) diluted 1 : 20 and activin/inhibin βB subunit (R&D Systems, Minneapolis, MN, USA) diluted 1 : 100. Then, sections were washed in PBS with 0.5% Tween 20 and incubated with HRP-coupled secondary anti-mouse antibody (Dako, Glostrup, Denmark) diluted 1 : 200. DAB was used as chromogen to detect peroxidase activity. Sections were counterstained with haematoxylin and mounted in Dako mounting medium (Merck, Darmstadt, Germany).
Rabbit polyclonal activin/inhibin βE subunit antibody was kindly provided by W Schneider (Grusch et al, 2006). Staining for activin/inhibin βE (primary antibody, dilution 1 : 500) and activin/inhibin βA (Serotec, Duesseldorf, Sweden, mouse monoclonal, dilution 1 : 50) was performed as described above except that biotinylated instead of HRP-coupled secondary antibodies were used and sections subsequently incubated with streptavidin–HRP conjugates.
For staining of the tissue arrays, fixed in 10% formalin, the more sensitive Ultravision Detection System (LabVision/Thermo Scientific) was used. Antigen retrieval and the concentration of the primary antibodies were the same as described above. Activin/inhibin βC immunocytochemistry was not studied because of the lack of reliable antibodies. All available antibodies gave a positive response in INHBC knockout mice suggesting cross reactivity with other protein(s) (unpublished).
Results
Expression of the inhibin family in normal and tumour-adjacent liver and in HCC
We have previously studied INHBA and INHBE expression in 11 samples of human HCC and two disease-free livers (Grusch et al, 2006). We now extended our analysis to all inhibin family members and to tumour-adjacent (fibrotic or cirrhotic) tissue, and increased sample numbers (16 HCC, 10 normal liver specimens). PCR results are displayed in Figure 1. B2M is included here, as it was used as reference gene in the previous study.
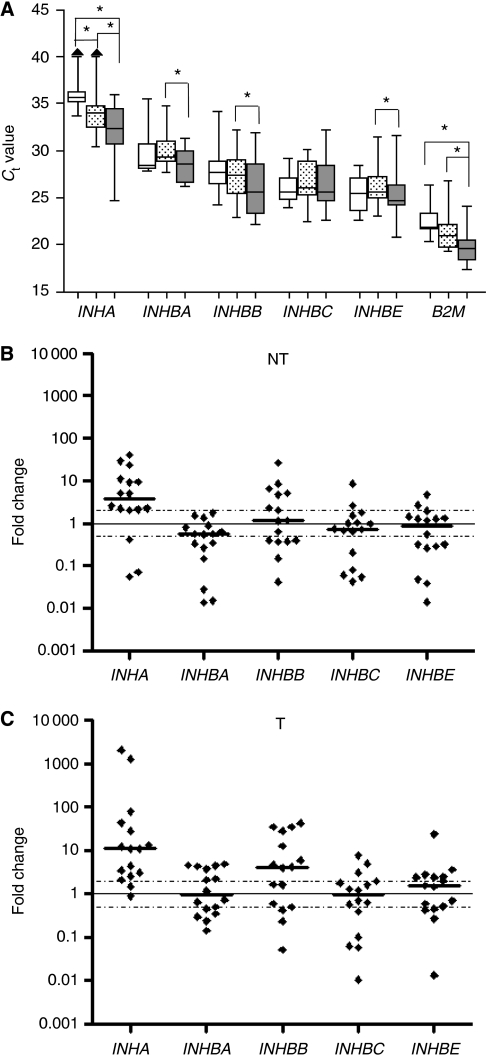
Figure 1.
mRNA expression of inhibin genes in disease-free (N), and tumour-adjacent (NT) liver and in HCC (T). (A) Real-time PCR cycle threshold (Ct) values normalised to RNA input are given. Ct values for B2M are shown for comparison. Boxes (blank, N; dotted, NT; grey; T) represent the lower and upper quartiles with medians; whiskers illustrate the 10–90 percentiles of the samples. Significant changes (P<0.05) are marked with brackets and asterisk. (B and C) Expression changes of individual NT or T samples related to the median of normal liver (N). Log transformed Ct values were used. Dotted lines indicate expression changes to >2-fold or <0.5-fold, considered as thresholds of biological relevance. INHA levels in three N and one NT samples were undetectable and for calculations were set at the detection limit (Ct 40).
INHA (inhibin α) mRNA, reportedly undetectable in rat liver (De Bleser et al, 1997), was found in 7 out of 10 normal (N) liver samples, range of Ct values 33.5–36.5, in 15 out of 16 adjacent tissues (NT), Ct 30.5–39.5, and in all HCC (T), Ct 24.5–36 (Figure 1A). Thus, INHA expression was strongly upregulated in NT and even more in T (significant for N–NT and N–T). Expression of the four β subunits was detected in all samples, Ct 20.5–35.5. No significant changes vs N were seen in NT or T. However, T vs NT in paired samples showed significant upregulation of INHBA, INHBB and INHBE, whereas INHBC expression remained unaltered.
Expression changes in individual NT and T samples vs the median of normal liver are shown in Figures 1B and C, respectively. INHA expression varied considerably, particularly in HCC. Overall, it was increased in all but three NT samples, and in all but two T samples, resulting in mean 9- and 225-fold increases in NT and T, respectively (Table 2, left columns). Similarly, INHBB was upregulated in a fraction of the HCC, resulting in an overall mean 12-fold increase, while other HCC exhibited no change or even decreases. Expression of INHBA, INHBC and INHBE was increased in some and decreased in other HCC, overall no significant changes were noted. Expressions in paired NT and T samples from individual patients are displayed in Supplementary Figure 2. The strong upregulation in HCC of INHA and the weaker increases of INHB genes except INHBC are clearly seen (compare Figure 1A). The increase in INHBE was significant with only two normalisation methods, see below (Table 2).
Expression of INHBB and INHBC was correlated in NT (r=0.897, P=3 × 10−6) and in T (r=0.924, P=6 × 10−7). INHA and INHBA expression was correlated in NT samples (r=0.782, P=0.0006), but not in T. Overall, obvious correlations between expression levels of the genes studied clinical parameters such as gender, age, tumour staging, tumour grading, viral and fibrotic/cirrhotic status were not detected.
The present data showing no significant change in expression of INHBA and INHBE in HCC seem to vary with our previous study in which decreases for these two genes were reported (Grusch et al, 2006). These variations are most likely due to a difference in normalisation which was performed here to RNA input, but previously to B2M. When normalising the present results with B2M, downregulation from N to T appeared again, obviously a consequence of the pronounced increase in B2M expression in HCC. We conclude that a single reference gene may be unsuitable for normalisation of RNA expression data in human HCC.
Normalisation by geNorm
In Figure 1, we display RNA data normalised to RNA input or data derived therefrom by logarithmical transformation according to (Tricarico et al, 2002). In addition, we applied a normalisation protocol based on combinations of reference genes determined by geNorm (Vandesompele et al, 2002), as developed for HCC (Supplementary Figure 1).
As five of the six chosen reference genes are significantly upregulated even in non-tumourous tissue from HCC patients (data not shown), the use of one combination of reference genes for N, NT and T samples together would lead to an general overestimation of gene expression level in the disease-free liver samples. Normalisation within a subgroup, like N, with an optimised reference gene combination (Supplementary Figures 1A and B for NT samples) results in reduced statistical spread of expression of inhibin genes, rather than in shift of the median expression, which varied between 0.86 and 1.22 only after normalisation for N samples (Supplementary Figure 1C). For NT and T samples, the same three reference genes were found as the most stable ones (data not shown). The stability values S calculated for NT samples alone was far below the recommended threshold of 1 (Hellemans et al, 2007). However, when T samples were included into the calculation S-value increase dramatically, reflecting deregulation of reference gene expression (data not shown). Consequently, we used two different sets of normalisation factors, ‘NF jointly’ and ‘NF separately’, compared the results with those obtained by normalisation to RNA input. Overall, results varied in a reasonable range, indicating the reliability of the three normalisation methods used. Specifically, the strongest increase in median expression was consistently found in tumour samples for INHA ranging from 8.6- to 10.9-fold. Significant expression changes between NT and T were observed with INHBA and INHBB, and in part for INHBE (Table 2).
Inhibin protein expression in HCC
To confirm expression of inhibin genes at the protein level, we performed immunohistochemistry on a subset of the NT and T samples used for mRNA expression analysis (indicated in Supplementary Figure 2) and on a HCC tissue array from an independent patient collective. For inhibin α, we choose one HCC with the highest mRNA level and one moderately expressing one, as we expected to work at the detection limit. Moderate staining in almost all carcinoma cells was detected in the highly expressing HCC (Figure 2A (i)), whereas the moderately expressing tumour exhibited very intense staining in a restricted number of carcinoma cells (Figure 2A (iii)). Also in 2 of 16 samples from the tissue array, strong staining in restricted areas was detected (Supplementary Figure 3B). The adjacent tissue samples were either negative for inhibin α or showed a very faint parenchymal staining (Figure 2A, Supplementary Figure 3A, Supplementary Table 2).
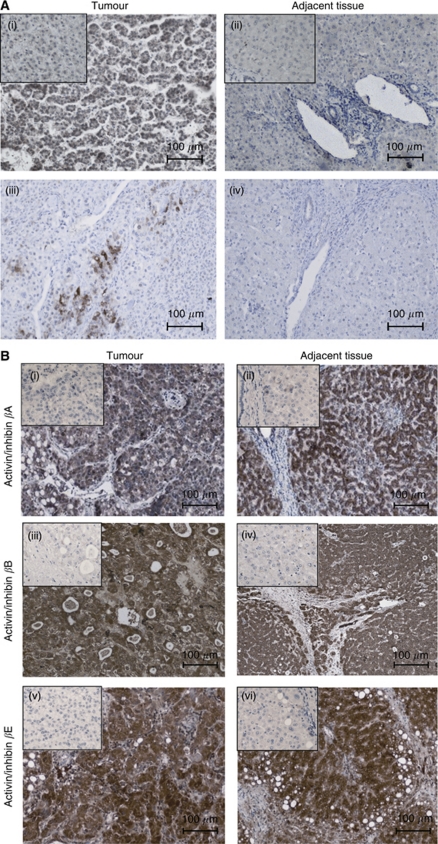
Figure 2.
Immunohistochemical localisation of inhibin/activin proteins in HCC and tumour-adjacent liver. (A) Microphotographs show cytoplasmatic staining of inhibin α in carcinoma cells (i) and (iii), whereas hepatocytes (ii) and (iv) and non-parenchymal cells are negative. (B) Activin/inhibin staining for subunits βA, βB and βE is high in tumour and adjacent parenchymal tissue. Inlets: non-immune serum; scale bars: 100 μm.
For activin/inhibin βB, three representative NT samples expressing high, moderate and low mRNA were stained and the intensity of the staining correlated well with INHBB mRNA levels (Supplementary Figure 3B). In general, activin/inhibin βB staining was intense in cells from parenchymal origin in both, tumour and adjacent tissue. A semi-quantitative analysis of the tissue array data demonstrated upregulation in 7, downregulation in 4 and an unaltered expression in 5 of 16 tumour array samples (Supplementary Table 2), a similar distribution as found for mRNA expression in the independent HCC collective used for RNA analysis (Figure 1C).
Expression of activin/inhibin βA and βE protein subunits was studied in five pairs of T and NT samples. In all specimens, carcinoma cells and the parenchymal cells of the adjacent tissues were clearly positive for both proteins (Figure 2B). For both protein subunits, the staining intensities in the tissue array ranged from negative to very strong staining in tumour as well as adjacent tissues (Supplementary Table 2). With all activin/inhibin subunits, staining was restricted to carcinoma cells, hepatocytes and bile ductular cells; whereas mesenchymal cells were consistently negative. As the antibodies detect inhibin subunits, the composition of the dimeric proteins cannot be deduced.
Inhibin gene family expression in various human tissues
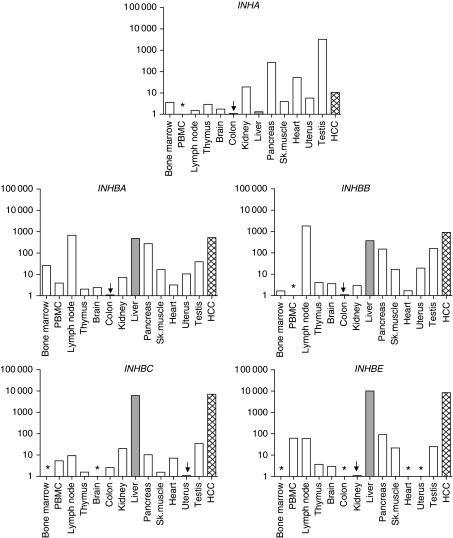
Expression of inhibin family members was analysed in 12 additional human organs and normalised to RNA input. Results including levels in normal liver and HCC are shown in Figure 3. INHA expression was highest in testis, as reported previously (Meunier et al, 1988; Tuuri et al, 1994), exceeding levels in HCC about 250-fold and in normal liver about 2500-fold; lowest levels were measured in colon. All four β subunits were highly expressed in the liver. INHBA and INHBB were detected in almost every tissue sample with a remarkably similar overall pattern. INHBC and INHBE expression were at least 100-fold higher in liver than in any other organ investigated, but nevertheless detected in 11 out of 13 and 9 out of 13 tissues, respectively. Thus, INHBC and INHBE are predominantly, but not specifically expressed in the liver as assumed previously.
Figure 3.
Expression of inhibin subunits in human tissues. Ct values detected in the various tissues ranged from 24.0 to 36.0 for INHA, for INHBA from 27.5 to 37.0, for INHBB from 24.5 to 35.5, for INHBC from 26.0 to 38.5 and for INHBE from 24.5 to 36.5. Expression below detection limits is marked by asterisks. The respective lowest expressing tissue (arrow) was used as calibrator and set 1, the expression levels of the others were depicted as fold increase in logarithmic scale. Disease-free liver is shown in grey, HCC expression levels by gridded bars. PBMC, peripheral blood mononuclear cells.
Inhibin family gene expression differs in human and rodent liver
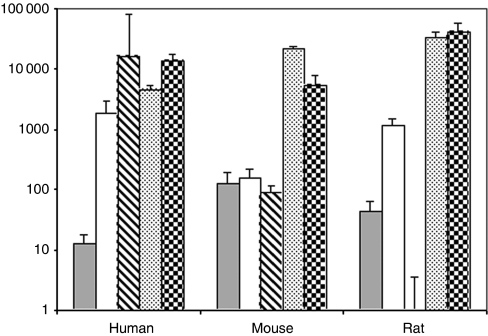
For comparison, expression of the inhibin family was analysed in mouse and rat liver. To test for species differences in qRT-PCR-based Ct values, distinct plasmid dilution series were performed and revealed detectability at similar Ct levels (data not shown). As displayed in Figure 4, INHA expression, overall at a low level, was about 10-fold higher in rodent than in human liver. INHBC and INHBE were highly expressed in all three species, with INHBC levels being about 10-fold higher in rodent than in human liver. In contrast, INHBA and INHBB expression was more pronounced in human than in rodent liver, levels being 10- and 100-fold lower in mice. In rats, INHBA levels were only slightly lower than in humans while INHBB expression was extremely low, detectable only at Ct 37.5. Taken together, there are profound interspecies differences in basal hepatic expression of inhibin genes.
Figure 4.
Species comparison of inhibin family expression in liver tissues. The lowest expressed gene, rat INHBB (Ct 37.5), was used as calibrator and set 1, the expression levels of the other genes were depicted as fold increase in logarithmic scale. Equal sensitivities of the Taqman assays were confirmed by plasmid dilution experiments (not shown). Expression ratios are depicted as following, INHA (grey bars), INHBA (open bars), INHBB (striped bars), INHBC (pointed bars) and INHBE (gridded bars).
Discussion
The involvement of members of the TGFβ superfamily in hepatocellular carcinogenesis is well established (Teicher, 2001; Rodgarkia-Dara et al, 2006), but the individual players and their functions and mechanisms of action are still largely unknown. Here, we analysed the expression of the complete inhibin family in human liver and HCC, other human organs and rodent liver.
Care was taken to assure the validity of comparisons between liver and HCC as well as between different tissues or species. As also reported by several groups the usual reference genes are not stably expressed during stages of cancer development (Blanquicett et al, 2002; Ohl et al, 2005; Waxman and Wurmbach, 2007). The use of a single reference gene for normalisation of RNA data may lead to unreliable or even wrong conclusions. We suggest an adapted normalisation approach especially for comparison of disease-free liver with fibrothic/cirrhotic liver and HCC. Here, we show that these normalisation procedures yield similar results as normalisation to RNA input of carefully controlled quality. This similarity confirms the overall validity of the results. In agreement with other authors (Tricarico et al, 2002; Caradec et al, 2010), we conclude that normalisation to RNA input provides reliable results. However, when studying new systems validity may be rechecked with normalisation protocols such as geNorm.
We also confirmed the validity of interspecies comparison of inhibin expression in the liver (see Results), which is supported by earlier studies reporting weak or undetectable expression of INHA and INHBB in rat liver by northern or RNA protection assays (De Bleser et al, 1997; Kobayashi et al, 2000; Vejda et al, 2002). Overall, our study revealed remarkable interspecies differences in expression levels of some inhibins, in particular INHA, INHBA and INHBB. As these differences may reflect variant roles in human and rodent liver care should be taken when extrapolating results from rodents to humans. This conclusion is supported by recent work (Utoh et al, 2010). In a mouse xenotransplant model, human hepatocytes replaced dying mouse cells excessively resulting in liver growth to three times the normal size, while rat hepatocytes terminated growth at normal liver size. This was explained by failure of human, but not rat hepatocytes to upregulate TGFβ and activin A type II receptors.
Inhibin and activin A were discovered as proteins regulating the release of follicle-stimulating hormone (Ling et al, 1986; Vale et al, 1986). Since then activin A has become the best characterised member of the inhibin/activin family. Besides its function in the pituitary, it is involved in many physiological processes, including embryonic development, erythroid differentiation, fibrosis, inflammation, cell proliferation and apoptosis as reviewed recently (Rodgarkia-Dara et al, 2006). Induction of apoptosis by activin A was described for the first time in rat liver and primary hepatocytes (Schwall et al, 1993). In the following years, several studies revealed a potent growth inhibitory role of activin A in the liver (Yasuda et al, 1993; Hully et al, 1994; Kogure et al, 1995), and activin A and TGFβ turned out as the two dominant hepatic growth inhibitors that counterbalance or terminate growth induction by a large number of stimulating factors.
In this study, somewhat surprisingly the expression of INHBA and also the protein level were not downregulated in the majority of tumour-adjacent and HCC samples studied, but even increased in several HCC. How HCC cells may escape from the proapoptotic and antiproliferative action of activin A? Activin A activity is known to be antagonised by several extracellular factors, including follistatin (Esch et al, 1987; Mashima et al, 1995), fstl3 (Tsuchida et al, 2000) and cripto (Gray et al, 2003). We described previously an upregulation of follistatin expression in rat and human liver tumours (Grusch et al, 2006).
Similarly, inhibin A, the heterodimer of INHA and INHBA gene products, antagonises the anti-proliferative action of activin A by competitive binding to cell surface activin type II receptors (ActRIIA/B) and inhibits downstream signalling in liver cells (Xu et al, 1995; Lewis et al, 2000; Massague, 2000). In the inhibin α nulled mouse, activin A serum levels were enhanced more than 10-fold, leading to apoptosis and necrosis in the liver (Matzuk et al, 1994). Our results revealed increases of INHA mRNA in most of the tumour-adjacent and HCC samples studied amounting to 9- and 225-fold increases, respectively, over disease-free liver (Figure 1, Table 2). Inhibin α protein also was clearly detectable, at least in some HCC (Figure 2, Supplementary Figure 3). The pronounced upregulation of INHA may lead to a shift from production of the activin A homodimer to the inhibin A heterodimer. These data suggest that high INHA expression blocks the activin A signal in HCC and also in tumour-adjacent tissue (which may contain cirrhosis, a cancer prestage), and thereby provides for, or contributes to, the growth advantage of tumour cells.
Similarly, the 12-fold mean increase in INHBB expression in HCC compared with normal liver may cause a shift from activin A to activin AB protein, which reportedly was less inhibitory than activin A on rat hepatocyte proliferation (Niimi et al, 2002). In conclusion, the enhanced expression of INHA or INHBB detected in 80% of our HCC patients may serve as alternative or additional regulators besides follistatin, fstl3 and cripto, overriding the antiproliferative and proapoptotic action of activin A.
Expression of INHBB in normal human liver was as high as in testis (Figure 4), one of the organs with known high expression (Roberts, 1997; Vejda et al, 2002). Up to now only few data on βB expression levels in human liver are available. In human fetal liver INHBB was detected by northern assay at similar levels as INHBA, but less expressed than in fetal testis (Tuuri et al, 1994). Sjoholm et al (2006) detected very low levels of INHBB by RT–PCR after normalising to cyclophilin A, whereas in a large-scale expression study on the same samples (Su et al, 2002) liver INHBB levels were higher than in pituitary, but lower than in testis (http://biogps.gnf.org/; INHBB; 3625_at Entrez Gene). So far, because of its low or negligible occurrence in rodent liver the role of INHBB in this organ has not been elucidated.
Interestingly, some extrahepatic tumours also show upregulation of INHA and/or INHBB. INHBB was upregulated in malignant endometrial tissues (Worbs et al, 2007) and in malignant but not in benign pheochromocytomas (Salmenkivi et al, 2001). Overexpression of the INHA subunit is pronounced in gonadal stromal tumours and even used as tumour marker (Fuller et al, 1999; Fine and Li, 2003; Ciris et al, 2004). Similarly, elevated serum levels of the inhibin α peptide were found in granulosa cell tumour patients (Burger et al, 2001). No inhibin α protein was detected in liver (Renshaw and Granter, 1998; Lau et al, 2002), but was reportedly found in 17 out of 19 HCC by immunohistochemistry (McCluggage et al, 1997; Vrettou et al, 2005). However, this finding was not confirmed on 23 HCC and suggested to be a staining artefact caused by endogenous biotin (Iezzoni et al, 1999). Another study classified a INHA positive hepatic adenocarcinoma as cholangiocarcinoma (Vrettou et al, 2005). Our investigation provides strong evidence for expression of INHA in HCC as cross-reactivity with biotin is excluded by using a biotin-free detection system and the specificity of staining was shown by incubation without antibodies or non-immune serum.
In summary, we have shown a pronounced upregulation of INHA and a more moderate increase in INHBB in most of the HCC samples analysed. Furthermore, marked differences in expression of inhibin genes between rodent and human liver were found. These new insights provide important hints to the largely unknown functions of the inhibins and activins in the liver and during hepatocarcinogenesis. Understanding how cancer cells escape from the action of activin A, a major growth inhibitor in the liver, may elucidate key dysfunctions of signalling in HCC and eventually open up new avenues to molecular therapy of this disease.
Acknowledgments
This study was supported by generous grants of Biopharm, Heidelberg, Germany, to RSH and the Herzfelder‘sche Familienstiftung, Vienna, Austria, to MG and CRD. We thank A Brachner for human tissue RNAs and for carefully reading the paper, R Horvat for support with ovarian carcinoma pathology, M Filipits for support and advice in histology and J Vandesompele and colleagues for running the geNorm communication platform.
Footnotes
Supplementary Information accompanies the paper on British Journal of Cancer website (http://www.nature.com/bjc)
Supplementary Material
References
- Blanquicett C, Johnson MR, Heslin M, Diasio RB (2002) Housekeeping gene variability in normal and carcinomatous colorectal and liver tissues: applications in pharmacogenomic gene expression studies. Anal Biochem 303: 209–214 [DOI] [PubMed] [Google Scholar]
- Burger HG, Fuller PJ, Chu S, Mamers P, Drummond A, Susil B, Neva P, Robertson DM (2001) The inhibins and ovarian cancer. Mol Cell Endocrinol 180: 145–148 [DOI] [PubMed] [Google Scholar]
- Caradec J, Sirab N, Keumeugni C, Moutereau S, Chimingqi M, Matar C, Revaud D, Bah M, Manivet P, Conti M, Loric S (2010) ‘Desperate house genes’: the dramatic example of hypoxia. Br J Cancer 102: 1037–1043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chabicovsky M, Herkner K, Rossmanith W (2003) Overexpression of activin beta(C) or activin beta(E) in the mouse liver inhibits regenerative deoxyribonucleic acid synthesis of hepatic cells. Endocrinology 144: 3497–3504 [DOI] [PubMed] [Google Scholar]
- Ciris M, Erhan Y, Zekioglu O, Bayramoglu H (2004) Inhibin alpha and beta expression in ovarian stromal tumors and their histological equivalences. Acta Obstet Gynecol Scand 83: 491–496 [DOI] [PubMed] [Google Scholar]
- De Bleser PJ, Niki T, Xu G, Rogiers V, Geerts A (1997) Localization and cellular sources of activins in normal and fibrotic rat liver. Hepatology 26: 905–912 [DOI] [PubMed] [Google Scholar]
- Deli A, Kreidl E, Santifaller S, Trotter B, Seir K, Berger W, Schulte-Hermann R, Rodgarkia-Dara C, Grusch M (2008) Activins and activin antagonists in hepatocellular carcinoma. World J Gastroenterol 14: 1699–1709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Drucker C, Parzefall W, Teufelhofer O, Grusch M, Ellinger A, Schulte-Hermann R, Grasl-Kraupp B (2006) Non-parenchymal liver cells support the growth advantage in the first stages of hepatocarcinogenesis. Carcinogenesis 27: 152–161 [DOI] [PubMed] [Google Scholar]
- Edmondson HA, Steiner PE (1954) Primary carcinoma of the liver: a study of 100 cases among 48,900 necropsies. Cancer 7: 462–503 [DOI] [PubMed] [Google Scholar]
- El-Serag HB, Rudolph KL (2007) Hepatocellular carcinoma: epidemiology and molecular carcinogenesis. Gastroenterology 132: 2557–2576 [DOI] [PubMed] [Google Scholar]
- Esch FS, Shimasaki S, Mercado M, Cooksey K, Ling N, Ying S, Ueno N, Guillemin R (1987) Structural characterization of follistatin: a novel follicle-stimulating hormone release-inhibiting polypeptide from the gonad. Mol Endocrinol 1: 849–855 [DOI] [PubMed] [Google Scholar]
- Esquela AF, Zimmers TA, Koniaris LG, Sitzmann JV, Lee SJ (1997) Transient down-regulation of inhibin-betaC expression following partial hepatectomy. Biochem Biophys Res Commun 235: 553–556 [DOI] [PubMed] [Google Scholar]
- Fang J, Wang SQ, Smiley E, Bonadio J (1997) Genes coding for mouse activin beta C and beta E are closely linked and exhibit a liver-specific expression pattern in adult tissues. Biochem Biophys Res Commun 231: 655–661 [DOI] [PubMed] [Google Scholar]
- Fine SW, Li M (2003) Expression of calretinin and the alpha-subunit of inhibin in granular cell tumors. Am J Clin Pathol 119: 259–264 [DOI] [PubMed] [Google Scholar]
- Fuller PJ, Chu S, Jobling T, Mamers P, Healy DL, Burger HG (1999) Inhibin subunit gene expression in ovarian cancer. Gynecol Oncol 73: 273–279 [DOI] [PubMed] [Google Scholar]
- Gold EJ, Francis RJ, Zimmermann A, Mellor SL, Cranfield M, Risbridger GP, Groome NP, Wheatley AM, Fleming JS (2003) Changes in activin and activin receptor subunit expression in rat liver during the development of CCl4-induced cirrhosis. Mol Cell Endocrinol 201: 143–153 [DOI] [PubMed] [Google Scholar]
- Gold EJ, O’Bryan MK, Mellor SL, Cranfield M, Risbridger GP, Groome NP, Fleming JS (2004) Cell-specific expression of betaC-activin in the rat reproductive tract, adrenal and liver. Mol Cell Endocrinol 222: 61–69 [DOI] [PubMed] [Google Scholar]
- Gold EJ, Zhang X, Wheatley AM, Mellor SL, Cranfield M, Risbridger GP, Groome NP, Fleming JS (2005) betaA- and betaC-activin, follistatin, activin receptor mRNA and betaC-activin peptide expression during rat liver regeneration. J Mol Endocrinol 34: 505–515 [DOI] [PubMed] [Google Scholar]
- Grasl-Kraupp B, Luebeck G, Wagner A, Low-Baselli A, de Gunst M, Waldhor T, Moolgavkar S, Schulte-Hermann R (2000) Quantitative analysis of tumor initiation in rat liver: role of cell replication and cell death (apoptosis). Carcinogenesis 21: 1411–1421 [PubMed] [Google Scholar]
- Gray PC, Harrison CA, Vale W (2003) Cripto forms a complex with activin and type II activin receptors and can block activin signaling. Proc Natl Acad Sci USA 100: 5193–5198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grusch M, Drucker C, Peter-Vorosmarty B, Erlach N, Lackner A, Losert A, Macheiner D, Schneider WJ, Hermann M, Groome NP, Parzefall W, Berger W, Grasl-Kraupp B, Schulte-Hermann R (2006) Deregulation of the activin/follistatin system in hepatocarcinogenesis. J Hepatol 45: 673–680 [DOI] [PubMed] [Google Scholar]
- Grusch M, Rodgarkia-Dara C, Bursch W, Schulte-Hermann R (2007) Activins and the Liver – Transforming Growth Factor-β in Cancer Therapy, Vol. 1. Humana Press: New York [Google Scholar]
- Hellemans J, Mortier G, De Paepe A, Speleman F, Vandesompele J (2007) qBase relative quantification framework and software for management and automated analysis of real-time quantitative PCR data. Genome Biol 8: R19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herzer K, Sprinzl MF, Galle PR (2007) Hepatitis viruses: live and let die. Liver Int 27: 293–301 [DOI] [PubMed] [Google Scholar]
- Hofland J, Timmerman MA, de Herder WW, van Schaik RH, de Krijger RR, de Jong FH (2006) Expression of activin and inhibin subunits, receptors and binding proteins in human adrenocortical neoplasms. Clin Endocrinol (Oxf) 65: 792–799 [DOI] [PubMed] [Google Scholar]
- Hofland J, van Nederveen FH, Timmerman MA, Korpershoek E, de Herder WW, Lenders JW, Verhofstad AA, de Krijger RR, de Jong FH (2007) Expression of activin and inhibin subunits, receptors and binding proteins in human pheochromocytomas: a study based on mRNA analysis and immunohistochemistry. Clin Endocrinol (Oxf) 66: 335–340 [DOI] [PubMed] [Google Scholar]
- Hully JR, Chang L, Schwall RH, Widmer HR, Terrell TG, Gillett NA (1994) Induction of apoptosis in the murine liver with recombinant human activin A. Hepatology 20: 854–862 [DOI] [PubMed] [Google Scholar]
- Iezzoni JC, Mills SE, Pelkey TJ, Stoler MH (1999) Inhibin is not an immunohistochemical marker for hepatocellular carcinoma. An example of the potential pitfall in diagnostic immunohistochemistry caused by endogenous biotin. Am J Clin Pathol 111: 229–234 [DOI] [PubMed] [Google Scholar]
- Jones KL, Mansell A, Patella S, Scott BJ, Hedger MP, de Kretser DM, Phillips DJ (2007) Activin A is a critical component of the inflammatory response, and its binding protein, follistatin, reduces mortality in endotoxemia. Proc Natl Acad Sci USA 104: 16239–16244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobayashi T, Niimi S, Fukuoka M, Hayakawa T (2002) Regulation of inhibin beta chains and follistatin mRNA levels during rat hepatocyte growth induced by the peroxisome proliferator di-n-butyl phthalate. Biol Pharm Bull 25: 1214–1216 [DOI] [PubMed] [Google Scholar]
- Kobayashi T, Niimi S, Hashimoto O, Hayakawa T (2000) Expression of inhibin betaA, betaB and follistatin mRNAs in the carbon tetrachloride induced rat liver regeneration model. Biol Pharm Bull 23: 755–757 [DOI] [PubMed] [Google Scholar]
- Kogure K, Omata W, Kanzaki M, Zhang YQ, Yasuda H, Mine T, Kojima I (1995) A single intraportal administration of follistatin accelerates liver regeneration in partially hepatectomized rats. Gastroenterology 108: 1136–1142 [DOI] [PubMed] [Google Scholar]
- Kogure K, Zhang YQ, Shibata H, Kojima I (1998) Immediate onset of DNA synthesis in remnant rat liver after 90% hepatectomy by an administration of follistatin. J Hepatol 29: 977–984 [DOI] [PubMed] [Google Scholar]
- Lau AL, Kumar TR, Nishimori K, Bonadio J, Matzuk MM (2000) Activin betaC and betaE genes are not essential for mouse liver growth, differentiation, and regeneration. Mol Cell Biol 20: 6127–6137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau SK, Prakash S, Geller SA, Alsabeh R (2002) Comparative immunohistochemical profile of hepatocellular carcinoma, cholangiocarcinoma, and metastatic adenocarcinoma. Hum Pathol 33: 1175–1181 [DOI] [PubMed] [Google Scholar]
- Laurent-Puig P, Zucman-Rossi J (2006) Genetics of hepatocellular tumors. Oncogene 25: 3778–3786 [DOI] [PubMed] [Google Scholar]
- Lewis KA, Gray PC, Blount AL, MacConell LA, Wiater E, Bilezikjian LM, Vale W (2000) Betaglycan binds inhibin and can mediate functional antagonism of activin signalling. Nature 404: 411–414 [DOI] [PubMed] [Google Scholar]
- Ling N, Ying SY, Ueno N, Shimasaki S, Esch F, Hotta M, Guillemin R (1986) Pituitary FSH is released by a heterodimer of the beta-subunits from the two forms of inhibin. Nature 321: 779–782 [DOI] [PubMed] [Google Scholar]
- Llovet JM, Burroughs A, Bruix J (2003) Hepatocellular carcinoma. Lancet 362: 1907–1917 [DOI] [PubMed] [Google Scholar]
- Macheiner D, Heller G, Kappel S, Bichler C, Stattner S, Ziegler B, Kandioler D, Wrba F, Schulte-Hermann R, Zochbauer-Muller S, Grasl-Kraupp B (2006) NORE1B, a candidate tumor suppressor, is epigenetically silenced in human hepatocellular carcinoma. J Hepatol 45: 81–89 [DOI] [PubMed] [Google Scholar]
- Mashima H, Kanzaki M, Nobusawa R, Zhang YQ, Suzuki M, Mine T, Kojima I (1995) Derangements in the activin-follistatin system in hepatoma cells. Gastroenterology 108: 834–840 [DOI] [PubMed] [Google Scholar]
- Massague J (2000) How cells read TGF-beta signals. Nat Rev Mol Cell Biol 1: 169–178 [DOI] [PubMed] [Google Scholar]
- Matzuk MM, Finegold MJ, Mather JP, Krummen L, Lu H, Bradley A (1994) Development of cancer cachexia-like syndrome and adrenal tumors in inhibin-deficient mice. Proc Natl Acad Sci USA 91: 8817–8821 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCluggage WG, Maxwell P, Patterson A, Sloan JM (1997) Immunohistochemical staining of hepatocellular carcinoma with monoclonal antibody against inhibin. Histopathology 30: 518–522 [DOI] [PubMed] [Google Scholar]
- Meunier H, Rivier C, Evans RM, Vale W (1988) Gonadal and extragonadal expression of inhibin alpha, beta A, and beta B subunits in various tissues predicts diverse functions. Proc Natl Acad Sci USA 85: 247–251 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niimi S, Horikawa M, Seki T, Ariga T, Kobayashi T, Hayakawa T (2002) Effect of activins AB and B on DNA synthesis stimulated by epidermal growth factor in primary cultured rat hepatocytes. Biol Pharm Bull 25: 437–440 [DOI] [PubMed] [Google Scholar]
- Ohl F, Jung M, Xu C, Stephan C, Rabien A, Burkhardt M, Nitsche A, Kristiansen G, Loening SA, Radonic A, Jung K (2005) Gene expression studies in prostate cancer tissue: which reference gene should be selected for normalization? J Mol Med 83: 1014–1024 [DOI] [PubMed] [Google Scholar]
- Pirisi M, Fabris C, Luisi S, Santuz M, Toniutto P, Vitulli D, Federico E, Del Forno M, Mattiuzzo M, Branca B, Petraglia F (2000) Evaluation of circulating activin-A as a serum marker of hepatocellular carcinoma. Cancer Detect Prev 24: 150–155 [PubMed] [Google Scholar]
- Renshaw AA, Granter SR (1998) A comparison of A103 and inhibin reactivity in adrenal cortical tumors: distinction from hepatocellular carcinoma and renal tumors. Mod Pathol 11: 1160–1164 [PubMed] [Google Scholar]
- Roberts VJ (1997) Tissue-specific expression of inhibin/activin subunit and follistatin mRNAs in mid- to late-gestational age human fetal testis and epididymis. Endocrine 6: 85–90 [DOI] [PubMed] [Google Scholar]
- Rodgarkia-Dara C, Vejda S, Erlach N, Losert A, Bursch W, Berger W, Schulte-Hermann R, Grusch M (2006) The activin axis in liver biology and disease. Mutat Res 613: 123–137 [DOI] [PubMed] [Google Scholar]
- Sagmeister S, Eisenbauer M, Pirker C, Mohr T, Holzmann K, Zwickl H, Bichler C, Kandioler D, Wrba F, Mikulits W, Gerner C, Shehata M, Majdic O, Streubel B, Berger W, Micksche M, Zatloukal K, Schulte-Hermann R, Grasl-Kraupp B (2008) New cellular tools reveal complex epithelial-mesenchymal interactions in hepatocarcinogenesis. Br J Cancer 99: 151–159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmenkivi K, Arola J, Voutilainen R, Ilvesmaki V, Haglund C, Kahri AI, Heikkila P, Liu J (2001) Inhibin/activin betaB-subunit expression in pheochromocytomas favors benign diagnosis. J Clin Endocrinol Metab 86: 2231–2235 [DOI] [PubMed] [Google Scholar]
- Schulte-Hermann R, Bursch W, Low-Baselli A, Wagner A, Grasl-Kraupp B (1997) Apoptosis in the liver and its role in hepatocarcinogenesis. Cell Biol Toxicol 13: 339–348 [DOI] [PubMed] [Google Scholar]
- Schwall RH, Robbins K, Jardieu P, Chang L, Lai C, Terrell TG (1993) Activin induces cell death in hepatocytes in vivo and in vitro. Hepatology 18: 347–356 [DOI] [PubMed] [Google Scholar]
- Seitz HK, Stickel F (2006) Risk factors and mechanisms of hepatocarcinogenesis with special emphasis on alcohol and oxidative stress. Biol Chem 387: 349–360 [DOI] [PubMed] [Google Scholar]
- Sjoholm K, Palming J, Lystig TC, Jennische E, Woodruff TK, Carlsson B, Carlsson LM (2006) The expression of inhibin beta B is high in human adipocytes, reduced by weight loss, and correlates to factors implicated in metabolic disease. Biochem Biophys Res Commun 344: 1308–1314 [DOI] [PubMed] [Google Scholar]
- Strand S, Hofmann WJ, Hug H, Muller M, Otto G, Strand D, Mariani SM, Stremmel W, Krammer PH, Galle PR (1996) Lymphocyte apoptosis induced by CD95 (APO-1/Fas) ligand-expressing tumor cells – a mechanism of immune evasion? Nat Med 2: 1361–1366 [DOI] [PubMed] [Google Scholar]
- Su AI, Cooke MP, Ching KA, Hakak Y, Walker JR, Wiltshire T, Orth AP, Vega RG, Sapinoso LM, Moqrich A, Patapoutian A, Hampton GM, Schultz PG, Hogenesch JB (2002) Large-scale analysis of the human and mouse transcriptomes. Proc Natl Acad Sci USA 99: 4465–4470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takamura K, Tsuchida K, Miyake H, Tashiro S, Sugino H (2005) Activin and activin receptor expression changes in liver regeneration in rat. J Surg Res 126: 3–11 [DOI] [PubMed] [Google Scholar]
- Teicher BA (2001) Malignant cells, directors of the malignant process: role of transforming growth factor-beta. Cancer Metastasis Rev 20: 133–143 [DOI] [PubMed] [Google Scholar]
- Tricarico C, Pinzani P, Bianchi S, Paglierani M, Distante V, Pazzagli M, Bustin SA, Orlando C (2002) Quantitative real-time reverse transcription polymerase chain reaction: normalization to rRNA or single housekeeping genes is inappropriate for human tissue biopsies. Anal Biochem 309: 293–300 [DOI] [PubMed] [Google Scholar]
- Tsuchida K, Arai KY, Kuramoto Y, Yamakawa N, Hasegawa Y, Sugino H (2000) Identification and characterization of a novel follistatin-like protein as a binding protein for the TGF-beta family. J Biol Chem 275: 40788–40796 [DOI] [PubMed] [Google Scholar]
- Tuuri T, Eramaa M, Hilden K, Ritvos O (1994) The tissue distribution of activin beta A- and beta B-subunit and follistatin messenger ribonucleic acids suggests multiple sites of action for the activin-follistatin system during human development. J Clin Endocrinol Metab 78: 1521–1524 [DOI] [PubMed] [Google Scholar]
- Utoh R, Tateno C, Kataoka M, Tachibana A, Masumoto N, Yamasaki C, Shimada T, Itamoto T, Asahara T, Yoshizato K (2010) Hepatic hyperplasia associated with discordant xenogeneic parenchymal-nonparenchymal interactions in human hepatocyte-repopulated mice. Am J Pathol 177: 654–665 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vale W, Rivier J, Vaughan J, McClintock R, Corrigan A, Woo W, Karr D, Spiess J (1986) Purification and characterization of an FSH releasing protein from porcine ovarian follicular fluid. Nature 321: 776–779 [DOI] [PubMed] [Google Scholar]
- Vandesompele J, De Preter K, Pattyn F, Poppe B, Van Roy N, De Paepe A, Speleman F (2002) Accurate normalization of real-time quantitative RT-PCR data by geometric averaging of multiple internal control genes. Genome Biol 3: RESEARCH0034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vejda S, Cranfield M, Peter B, Mellor SL, Groome N, Schulte-Hermann R, Rossmanith W (2002) Expression and dimerization of the rat activin subunits betaC and betaE: evidence for the formation of novel activin dimers. J Mol Endocrinol 28: 137–148 [DOI] [PubMed] [Google Scholar]
- Vejda S, Erlach N, Peter B, Drucker C, Rossmanith W, Pohl J, Schulte-Hermann R, Grusch M (2003) Expression of activins C and E induces apoptosis in human and rat hepatoma cells. Carcinogenesis 24: 1801–1809 [DOI] [PubMed] [Google Scholar]
- Vrettou E, Hytiroglou P, Sikas N, Soultoyannis I, Goodman ZD (2005) Hepatic adenocarcinoma expressing inhibin in a young patient on oral contraceptives. Virchows Arch 446: 560–565 [DOI] [PubMed] [Google Scholar]
- Wada W, Maeshima A, Zhang YQ, Hasegawa Y, Kuwano H, Kojima I (2004) Assessment of the function of the betaC-subunit of activin in cultured hepatocytes. Am J Physiol Endocrinol Metab 287: E247–E254 [DOI] [PubMed] [Google Scholar]
- Wada W, Medina J, Hasegawa Y, Kuwano H, Kojima I (2005) Adenovirus-mediated overexpression of the activin betaC subunit accelerates liver regeneration in partially hepatectomized rats. J Hepatol 43: 823–828 [DOI] [PubMed] [Google Scholar]
- Waxman S, Wurmbach E (2007) De-regulation of common housekeeping genes in hepatocellular carcinoma. BMC Genomics 8: 243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worbs S, Shabani N, Mayr D, Gingelmaier A, Makrigiannakis A, Kuhn C, Jeschke U, Kupka MS, Friese K, Mylonas I (2007) Expression of the inhibin/activin subunits (-alpha, -betaA and -betaB) in normal and carcinogenic endometrial tissue: possible immunohistochemical differentiation markers. Oncol Rep 17: 97–104 [PubMed] [Google Scholar]
- Xu J, McKeehan K, Matsuzaki K, McKeehan WL (1995) Inhibin antagonizes inhibition of liver cell growth by activin by a dominant-negative mechanism. J Biol Chem 270: 6308–6313 [DOI] [PubMed] [Google Scholar]
- Yasuda H, Mine T, Shibata H, Eto Y, Hasegawa Y, Takeuchi T, Asano S, Kojima I (1993) Activin A: an autocrine inhibitor of initiation of DNA synthesis in rat hepatocytes. J Clin Invest 92: 1491–1496 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yuen MF, Norris S, Evans LW, Langley PG, Hughes RD (2002) Transforming growth factor-beta 1, activin and follistatin in patients with hepatocellular carcinoma and patients with alcoholic cirrhosis. Scand J Gastroenterol 37: 233–238 [DOI] [PubMed] [Google Scholar]
- Zauberman A, Oren M, Zipori D (1997) Involvement of p21(WAF1/Cip1), CDK4 and Rb in activin A mediated signaling leading to hepatoma cell growth inhibition. Oncogene 15: 1705–1711 [DOI] [PubMed] [Google Scholar]
- Zhang YQ, Shibata H, Schrewe H, Kojima I (1997) Reciprocal expression of mRNA for inhibin betaC and betaA subunits in hepatocytes. Endocr J 44: 759–764 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.