Abstract
Objective
Improvements in clinical pain care have not matched advances in scientific knowledge, and innovations in medical education are needed. Several streams of evidence indicate that pain education needs to address both the affective and cognitive dimensions of pain. Our aim was to design and deliver a new course in pain establishing foundation-level knowledge while comprehensively addressing the emotional development needs in this area.
Setting
118 first year medical students at Johns Hopkins School of Medicine.
Outcome measures
Performance was measured by multiple choice tests of pain knowledge, attendance, reflective pain portfolios and satisfaction measures.
Results
Domains of competence in pain knowledge included central and peripheral pain signaling, pharmacological management of pain with standard analgesic medications, neuromodulating agents and opioids; cancer pain, musculoskeletal pain, nociceptive, inflammatory, neuropathic, geriatric, and pediatric pain. Socio-emotional development (portfolio) work focused on increasing awareness of pain affect in self and others and enhancing the commitment to excellence in pain care. Reflections included observations on a brief pain experience (cold pressor test), the multi-dimensionality of pain, the role of empathy and compassion in medical care, the positive characteristics of pain-care role models, the complex feelings engendered by pain and addiction including frustration and disappointment, and aspirations and commitments in clinical medicine. The students completing feedback expressed high levels of interest in pain medicine as a result of the course.
Discussion
We conclude that a four-day pain course incorporating sessions with pain- specialists, pain medicine knowledge, and design-built elements to strengthen emotional skills is an effective educational approach.
Introduction
“Tell me, and I forget. Teach me, and I remember. Involve me, and I learn.” – Benjamin Franklin
The last three decades have seen an extraordinary expansion of clinical and basic science knowledge about pain and its mechanisms (1). But as many have observed, there has been a lag in translating this knowledge into clinical practice (2–4). Despite the prevalence of pain in clinical practice and a widespread awareness of the need for improvements, educational and training programs for physicians, as a rule, have been very slow to integrate pain as a topic (5–7).
In the realm of medical education, the intrinsic affective quality of pain presents a protean challenge to the design of educational experiences. It is widely accepted that pain is inherently aversive for those who experience it directly, interfering with function, cognition and mood. Accumulating evidence indicates important effects can occur for spouses (8) and primary caregivers (9). The impact of pain affect on healthcare providers (10) is not well understood but our preliminary studies indicate that medical students exhibit ambivalence toward pain for reasons pertaining to the negative emotions associated with pain experience (11). Beyond this, medical trainees are strongly influenced by the attitudes of influential others whom they encounter in the training environment, a phenomenon referred to as the `hidden curriculum' (12;13).
In fact, the affective dimensions of pain are both a challenge and an opportunity. In recent years, there are new ideas about how medical schools can more positively foster the social and emotional development of medical trainees (14;15). Sometimes examined under the rubric of humanism (16), professionalism or empathy (17), there is a growing body of literature that looks to examine the role of emotion in the clinical encounter (18). Certainly, to prevent nearly epidemic levels of burn-out and frustration, there are those who advocate for enhanced approaches to building emotional awareness and skills (19). At present, evidence supporting the use of particular educational methods for medical students' growth is limited (20). It is known that role models play a critical part in formative clinical experiences (21;22) journaling, discussion groups, and structured reflection activities are other approaches that have yielded results (23–26). Unfortunately, there is abundant evidence that current methods of education are having effects that are diametrically opposed of that desired. Students exhibit dramatic decreases in empathy during training (27) and negative attitudes towards patients with pain become deeply entrenched; novel approaches are needed.
Our aim was to create a new course in pain, one that would give students a solid foundation in pain pathophysiology, a glimpse at some of the remarkable new discoveries in pain science, and a basic body of practical knowledge essential for excellence in clinical care. Our greater vision for the course was that we would build opportunities for emotional development (28). We sought out activities that would spur students to more deeply acknowledge the affective consequences of strong pain, begin to recognize their own emotional responses to pain in self and others, and write meaningfully about their ideals and aspirations as emerging physicians. These activities were presented to students in the form of a pain intersession portfolio. The portfolio is a inclusive document that incorporates the students' work in this domain. We believe this approach acknowledges the complexity of pain while guiding students towards a deeper commitment to relieve pain in the course of their professional lives.
The course described here was delivered as an integral part of a newly re-designed medical curriculum at the Johns Hopkins University School of Medicine (29). The purpose of this report is to provide an overview of the course itself and examine some effects of the intervention.
Methods
The course described here was delivered in May 2010 as part of a new medical curriculum at the Johns Hopkins University School of Medicine entitled Genes-to-Society (29). The process of course design and placement in the curriculum began in 2004. This curriculum includes Pain as one of several `horizontal strands', which are cross-cutting topics spanning all four years of medical school. The pain horizontal strand while `anchored' in the curriculum with an 18-hour, four-day `clinical' intersession for first year medical students, also includes pain content delivered both as separate sessions, e.g. `The primary afferent nociceptor' and pain content delivered as learning objectives in other fields, e.g., `Take the medical history of a patient with pain as a presenting complaint'. The pain intersession course itself featured an active-learning educational design that included only four traditional lecture hours. Instead, multiple lab sessions, team-based learning of pain pharmacology, daily small group discussions with pain-expert clinicians, and incorporation, where possible, of literary and artistic depictions of pain, fostered an atmosphere of professionalism and perspective-taking (30). Importantly, the course integrated time for multiple exercises focusing on the affective dimensions of pain (28).
Curriculum Development Process
The six-step curriculum development process, as described by Kern and Thomas (31), was followed and included: 1) general problem identification, 2) needs assessment of the targeted learners, 3) development of specific learning objectives, 4) integration of educational strategies most appropriate to the desired learning, 5) implementation of the course and 6) evaluation of the curriculum with modifications in response. To begin, an interdisciplinary pain curriculum development team comprised of six pain-expert clinicians and basic scientists was formed in 2005 to address the question: `What should a graduating medical student know about pain?' As part of the needs assessment, a list of major topic headings was generated through a comparison of the existing International Association for the Study of Pain (IASP) pain curriculum (5) with pain courses taught at other medical schools, the European Federation of IASP Chapters (EFIC) pain curriculum and the required topics included in the pain certification exams. These topic headings are shown in Table 1. Within these major topic headings, the team worked to established specific learning objectives. The resulting list of learning objectives was subjected to a modified Delphi-process whereby faculty worked independently to assess the relative importance and appropriateness of each objective (6). Objectives that were not endorsed by most of the group were modified or removed. The original plan for this content, designed to be delivered over 35 hours, was modified so that core content was delivered over 18 hours during four consecutive days. The remaining course objectives were planned for delivery in other parts of the four-year medical school curriculum.
Table 1.
Major topics in Pain Medicine
| pain neurobiology |
| the human and social cost of pain |
| clinical assessment of pain |
| non-pharmacological pain management |
| pharmacological pain management |
| interventional approaches to pain management |
| acute pain |
| chronic pain |
| pediatric pain |
| geriatric pain |
| cancer pain |
| impact of culture and ethnicity on pain |
| medico-legal aspects of pain care |
Course Delivery and Content Definition
The course design was constrained by the expectation of the medical school administration that no more than 60% of the contact time with students would be in the form of lecture. In order to exceed this expectation, only four lectures were planned, these covered the topics of: Introduction to Pain, Peripheral Pathophysiology of Pain, Central Pain Processing and Hyperalgesia, and Clinical Psychology of Pain. Three learning labs were planned. These covered the topics of Pain Psychophysics, Medication Prescription Writing, and Medico-legal Aspects of Pain Care Delivery. The latter consisted of an active learning exercise about risk assessment and documentation standards in the form of a model medical board (peer-review forum). Three team-based learning exercises were prepared on the topics of Over-the-Counter Analgesics and NSAIDs, Neuromodulating Agents for Pain Treatment, and Opioids for Pain. Three small groups were planned, these covered the topics of Pain Assessment, Pain-related Impairment and Disability, and Pain and Substance Abuse. The assessment block, on day four, incorporated a multiple-choice test, a short portfolio for short answer questions and written reflections, a paired-work assignment/test, and a required meet-the-professor session with an expert in pain and addiction.
Design and Implementation of Pain Intersession Portfolio
In order to structure reflection and meaningful effort pertaining to pain affect and emotion, students were required during the intersession to complete a written portfolio. A series of discussions was held by the course design team around the topic of communicating expectations regarding emotional development in the professional context of delivering clinical care in the area of pain. Students were asked to complete portfolio exercises, in 5–10 minute blocks, during class time. The use of in-class time for portfolio work was initially undertaken because of a directive that the course would demand essentially no `homework' of the students. This had the effect of compelling the students to rapidly focus their attention on the questions at hand. Although a couple of students indicated that this process of structured reflection felt forced, the vast majority of students completed the assigned tasks and most were robustly engaged in doing so. The portfolio exercises included: writing a brief pain narrative, describing the pain depicted in a fine-art image, assessing personal responses to the experience of pain during a common psychophysical test (the 30-second cold pressor), drafting personal learning objectives for the intersession, defining the role of empathy and compassion in medicine (28), a description of the relationship between pain and addiction, and a reflection of lessons learned from a pain expert panel and the positive personal qualities exhibited by the pain-expert clinicians of the panel.
Student Assessment and Grading of Reflective Portfolios
Assessment was multi-dimensional. Students were required to complete a multiple-choice exam, a brief assessment portfolio, a paired work assignment, and attend a special lecture on pain and addiction. The multiple choice exam and paired work assignment s were graded for accuracy and completeness. The portfolios were read by a single instructor (BBM) using a four point system with the grades reflecting fair, good, very good or excellent attainment of the tasks of written reflection. Each activity in the portfolio was reviewed and more extensive tasks received a check-mark if excellent, the overall grade reflected a composite of the task-specific check-marks. Assessment of the reflection work in the activities was operationally defined as described here. Excellent reflective work was characterized by multiple positive attributes including: 1) thoughtful appraisal of self or relevant others, 2) correct use of appropriate terms, 3) evidence of proper assessment of the question posed, 4) absence of factual errors, and 5) length of writing adequate to address the points raised. The attribute of primary importance was that of thoughtful appraisal. By contrast, reflective work that did not meet standards was characterized by multiple negative attributes: 1) glib or absent appraisal, 2) incorrect usage of terms, 3) failure to adequately address question posed, 4) factual errors, and 5) excessive brevity. Reflective work that demonstrated a mixture of positive and negative attributes was assigned an intermediate grade. Portfolios were returned to students with comments and where appropriate, a letter of commendation for exceptional effort.
Course assessment and Statistical Analysis
Although all students completed the course assignments, only 48% completed the course assessment survey administered by the office of medical education, this was a typical response rate as compared with similar assessment surveys. Data were analyzed using a commercially available spreadsheet program. No statistical comparisons were made for this observational study.
Results
In all, 118 medical students and one biomedical graduate student completed the pain intersession. The demographic characteristics of the student population are shown in Table 2. All students received a passing grade but performance in the assessment exercise varied as described below. Several students required additional time the day of the examination in order to complete the portfolio work. Attendance was required of all students and was verified by a computerized attendance system.
Table 2.
Student participant characteristics (n = 118)
| Characteristic | |
|---|---|
| Male, number (%) | 63 (53) |
| Age, average ±(stand. dev.) | 23.76 ± (2.26) |
| M.D./Ph.D., number (%) | 14 (12) |
Pain course content and delivery: results of the Six-step curriculum development process
The outline of the course content and delivery, including hours and learning modality, is specified in Table 3. The course material was delivered over three days with additional formative experiences and summative assessment taking place on the fourth day. The three instructional days were organized to progress in complexity. Day One focused on pain in the periphery. The pathophysiology lecture addressed peripheral pain mechanisms, small group discussions focused on pain assessment, the case-learning examples included sports injuries, arthritis and other problems of the limbs, the pharmacology focused on NSAIDs and acetaminophen and the learning lab included painful stimuli applied to the hands and feet. Day Two focused on pain at the peripheral-central junction (e.g. spinal roots, dorsal horn, etc.). Pathophysiology covered mechanisms of hyperalgesia including wind-up, glial activation and neuropathic signaling. Pharmacology covered selected neuromodulating agents, small group discussions focused on pain and impairment, and the case-learning activity addressed injuries of the neck and back. Day Three addressed persistent pain and opioids. Included in this was material about risk assessment for opioid use, conditions that reflect central modulation of pain experience and societal duties of the physician when treating pain. The structure, while originally conceived as having specific disciplines, e.g., pathophysiology, pharmacology, recurring at certain hours of the day, was adjusted to accommodate scheduling needs of faculty and students. The small groups, which occurred in the second hour on Day One, in order to follow the introductory lecture, were held in the first hour on the second and third days. This was very helpful for accommodating the participation of clinician small group leaders, but some students did not report in a timely fashion.
Table 3.
Outline of Pain Course Content
| Session | Format | Hr. | Faculty: student ratio | Topics | Portfolio work |
|---|---|---|---|---|---|
| Introduction to PAIN | Lecture | 1 | 1:120 | Prevalence of pain |
|
| Assessment of pain | |||||
| Interventions for pain | |||||
| Neurobiology (intro) of pain | |||||
|
| |||||
| Pain Assessment | Small group | 1 | 1:10 | Multi-dimensional |
|
| Developing a pain differential diagnosis | |||||
|
| |||||
| Pain Pathophysiology I | Lecture | 1 | 1:120 | Peripheral modes of increased pain |
|
| Inflammatory mediators and pain | |||||
| Muscle pain and joint pain | |||||
|
| |||||
| Pain Pharmacology I | TBL | 1 | 2:60 | Acetaminophen | |
| NSAIDs (OTC and prescription) | |||||
| First aid for pain: RICE-M | |||||
|
| |||||
| Pain Psychophysics | Lab | 1 | 1:60* | Pain Sensitivity questionnaire |
|
| Band-aid removal | |||||
| Cold pressor test (30 seconds) | |||||
| Painful and non-painful pressure | |||||
|
| |||||
| Pain, Impairment and Disability | Small group | 1 | 1:10 | Pain and impact on role functioning |
|
| Physician's role in impairment | |||||
| Pain as a contributing factor to disability | |||||
|
| |||||
| Pain Pathophysiology II | Lecture | 1 | 1:120 | Central mechanisms of increased pain |
|
| Wind-up | |||||
| Hyperalgesia | |||||
| Neuropathic pain – general principles | |||||
|
| |||||
| Pain Pharmacology II | TBL | 1 | 2:60 | Neuromodulating agents |
|
| Anti-depressants | |||||
| Anti-convulsants | |||||
| Local anesthetics | |||||
|
| |||||
| Pain – writing prescriptions | Lab | 1 | 2:60 | General practices |
|
| Techniques for controlled substances | |||||
|
| |||||
| Pain – clinical psychology | Lecture | 1 | 1:120 | Efficacy of non-pharmacological care |
|
| Modalities of behavioral treatment | |||||
| Motivational interviewing and pain | |||||
|
| |||||
| Pain and Addiction I | Small group | 1 | 1:10 | Assessment of risk for substance abuse |
|
| Definitions: dependence, tolerance, aberrant drug-taking behavior | |||||
| Strategies for mitigating risks of abuse | |||||
|
| |||||
| Pain in clinical practice | Pain panel | 1 | 4:120 | Duty of care for patients with pain |
|
| Importance of pain control | |||||
| Personal qualities of pain providers | |||||
| Pain management in oncology | |||||
|
| |||||
| Pain Pharmacology III | TBL | 1 | 1:60 | Opioids |
|
| Clinical decision making and opioids | |||||
| Responsible prescribing | |||||
| Choosing among the options | |||||
|
| |||||
| Pain and the medical board I | Lab (prep) | 1 | 1:60 | Medical documentation |
|
| Ongoing re-assessment of pain | |||||
|
| |||||
| Pain and the medical board I | Lab (present) | 1 | 1:60 | Diligence in medical record-keeping |
|
| Provision of adequate care | |||||
| Interpersonal skillfulness | |||||
| Communication and patient education | |||||
|
| |||||
| Pain – cognitive assessment | Exam | .5 | 1:60 | 37-item test of pain knowledge |
|
|
| |||||
| Pain – portfolio assessment | Exam | .5 | 1:60 | Short answer questions |
|
| Self-assessment scales | |||||
|
| |||||
| Pain – clinical applications | Paired work | 1 | 1:60 | Case based multiple choice questions |
|
| Two short answer synthesis questions | |||||
| Cancer pain | |||||
|
| |||||
| Pain and Addiction II | Q & A | 1 | 1:120 | Meet the professor – visiting faculty |
|
|
| |||||
| Total | 18 | ||||
Abbreviations: Hr. Hours; TBL, team-based learning; OTC, Over-the-counter medications; RICE-M, rest-ice-compression-elevation-medication; prep, preparation time for students; Q & A, Question and Answer session
The educational strategies selected for the course necessitated the participation of a large number of faculty. In all, 24 contributing faculty were involved directly in teaching; the concurrent small group sessions required 12 faculty. The three team-based learning modules were taught twice to groups of 60 students, a task shared by three faculty working in pairs and individually. The pain psychophysics lab required one faculty member and two teaching assistants. The pharmacology lab was taught by two faculty and one teaching assistant. The model board exercise was taught by 1 faculty member and a teaching assistant. The interdisciplinary pain panel consisted of a nurse manager, a surgeon and an oncology fellow. In total, 67 faculty contact hours were committed to the 18 hour course. Preparation of course materials took place over three years. An educational assistant worked on the project full time for a year to accomplish curriculum development and integration. Input from numerous content experts and educational specialists was essential. The faculty director (BBM) was responsible for the final content.
The pain portfolio: socio-emotional development in a professional context
A principal aim of the course was to build awareness of the affective dimensions of pain while fostering positive emotional development in the medical students. For this reason a pain intersession portfolio was developed. The portfolio provided opportunities for students to explore and record their experiences pertaining to the affective impact of pain and begin to examine their own responses to this problem. Details of the portfolio development process are provided in the methods, and results are shown in Table 3. One exercise that was especially meaningful was the cold pressor test (pain psychophysics lab). Many students expressed surprise at the distress associated with the resulting pain, others reflected on the cognitive interference that was evident to them. In another of the portfolio exercises, students were asked to record their impressions of the pain expert panel. They were asked to answer three questions: `What were the most important questions that were asked during this session?', `What were the most important things that you learned in this session (list at least three)?', and `What were the personal qualities of the provider on the panel that you most admired? Please explain'. The question about exemplary personal qualities was especially salient because role models have a profound impact on medical students (21;22). The students' responses were impressive in their perceptiveness and scope. Examples are shown in Table 4. All students completed the intersession portfolios, but three students required additional guidance after the intersession to complete the work. The quality of reflective work by the students was in many cases exceptional.
Table 4.
Sample student portfolio entries following pain-expert clinician panel discussion
| What were the personal qualities of the provider on the panel that you most admired? |
|---|
| I most admired the ability to be self-critical. A lot of times physicians and specialists seem to marginalize other concerns. That isn't wise and it isn't helpful. Acknowledging that doctors need |
| to work with staff, repeatedly check on patients and follow up on the status of pain management is refreshing. |
| The nurse manager from the PACU… was highly knowledgeable …. She seemed personally invested in the care of her patients and consistently advocated sitting down and getting to know your patients…. She also recognized the importance of collaboration in pain management and really came across as a team player. |
| All of the panel members were obviously very compassionate about their care for patients. They really want the best for the patients and a large part of that begins with making them comfortable and managing their pain. |
| Openness – that patients will surprise us in both heartening and disappointing ways, and we should try to keep ourselves open to those possibilities and use our judgment to address things as they come |
| I was very impressed by all three panelists, particularly because of how seriously they take the adequate treatment of pain. They all want to make sure that patients are appropriately treated. |
| I really liked how much emphasis was put on team work, The providers also emphasized the need to treat each patient individually. This point is also incredibly important when it comes to managing pain. The providers also emphasized the need to listen to patients and address their anxiety especially before surgery. |
| The panelists seemed to be very shrewd in their clinical judgments and assessments of patients with pain ….seemed very knowledgeable and well-informed….very passionate about pain treatment…. |
One frequently overlooked aspect of medical education is the importance of communicating expectations to students in advance. As a result of the planning process, it was determined that the students would work towards specific goals in terms of emotional development (28). These included demonstrating emotional strength (e.g., empathy, compassion, caring); emotional intelligence (e.g., awareness of pain's impact on mood, perception of emotion in others); emotional resilience (e.g., capacity for emotional self-repair, ability to tolerate frustration); and emotional regulation (e.g., tolerance of difficulties, sense of professional duty). To make these concepts more appealing and memorable for the students, the `Pain PANDA Program' was developed. The students were given a sheet explaining the ideals of the pain PANDA, these being: Perceptive, Astute, Naturally Nice, Determined to make it right, and Always learning. The students received complimentary PANDA mugs at the start of the course; this generated a high level of excitement. A PANDA logo lanyard was presented to students at the close of the course. The lanyard was designed to create a readily identifiable symbol for those students and faculty who participate in the course and commit to the goals of the PANDA program. It is evident from the reflections on the pain panel experience presented in Table 4, the results of the course feedback, and from other work in the pain portfolios that the students responded well to these efforts.
Course outcomes: Assessment and feedback
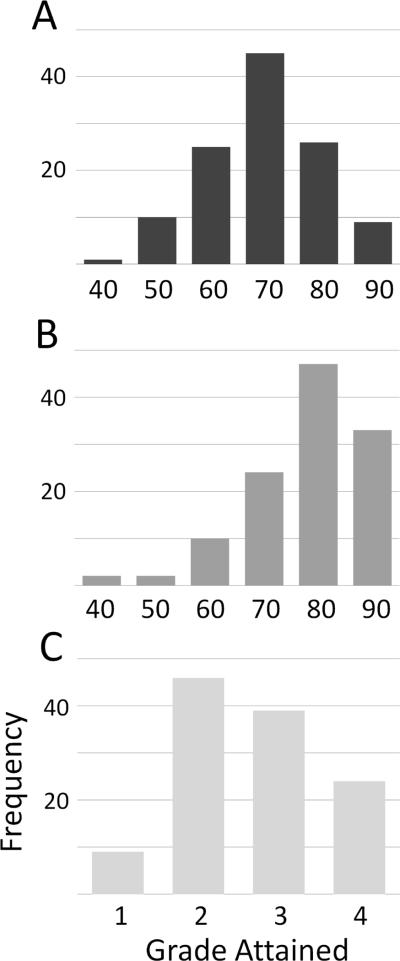
Assessment was multi-dimensional. Students were required to complete a multiple-choice exam, a brief assessment portfolio, a paired work assignment, and attend a special lecture on pain and addiction. The results of the various forms of assessment are illustrated in Figure 1. The multiple-choice exam, Figure 1A, yielded a mean score of 75 with a standard deviation of 11 points. Some students expressed frustration with the difficulty of the exam questions but generally students conveyed new respect for pain as a serious part of medical practice. The paired-work exercise was intentionally designed to prompt students to apply and discuss their working knowledge of pain medicine in order to solve more challenging pain problems. The intent of the exercise was to create a situation where students would need to dialogue about pain and explain their thinking to another in this regard. The results of the multiple choice portion of this exercise are shown in Figure 1B. The mean score (± standard deviation) was 87 (± 12.2). The portfolios were graded using a qualitative scale of fair, good, very good and excellent. The resulting median grade was very good, the modal grade was good. The difficulty of the portfolio work is evident from the grade distribution, shown in Figure 1C, which was shifted to the left relative to the more familiar task of completing a multiple choice exam, Figure 1A. It was evident from reading the portfolios that many of the students were engaged in serious introspection and measured self-appraisal. Examples are shown in Table 4. Some students adopted a glib approach as evidenced by the student who wrote `I am Chuck Norris!' in response to questions about the band-aid removal task. But even this student was highly contemplative when asked about pain and addiction as he wrote movingly about the devastating effects of addiction on a close friend.
Figure 1.
A) Scores for multiple choice exam. Details in text. B) Scores for pair-assessment multiple choice exam. C) Distribution of grades assigned for portfolios.
Students responding to the feedback survey expressed a high degree of satisfaction with the intersession. The small group sessions were especially well-liked. Nearly all students felt that their small group leader was an effective role model for clinical care, capable of `striking a good balance regarding the challenges of caring for patients in pain' and was committed to teaching the subject. In terms of self-assessment, 97% endorsed the statement that they had achieved an appreciation of `key challenges of providing pain care, e.g. assessment, impairment, abuse and addiction'. A more modest number felt they had attained basic knowledge of pain neurobiology and pain interventions, 76%. The overarching goals of the intersession were successfully met as measured by those students responding to the course assessment survey. They indicated agreement with the following: Increased interest in understanding physical pain, 89%; Increased motivation for addressing pain in patients, 91%; More interest in pain as a result of completing the Intersession, 87%.
Discussion
This report finds that a first-year medical school pain course, integrating cognitive and affective dimensions, is associated with attainment of foundation knowledge, robust engagement in tasks addressing emotional development, and high levels of learner satisfaction. Students and faculty were vigorously engaged in this required pain course, for which active learning methodologies were strongly invoked. The psychometric properties of the assessments were excellent. The multiple choice test of pain knowledge resulted in a normal distribution with a mean that met expectations. The paired-task assessment yielded higher mean scores reflecting the ability of students to aggressively solve problems when working together. The pain portfolio grades were lower on average, consistent with the relative difficulty of this task for many students. Taken as a whole, the course represents a substantial advance towards inclusion of important pain-relevant learning objectives into the medical curriculum of our school.
On a broad scale, the need for improved medical education in pain and pain care is clear, whether in response to the economic burdens associated with the under-treatment of pain, to patient safety concerns, to healthcare utilization pressures, or to the ethical considerations of failing to alleviate human suffering (32). Pain diagnoses and treatments are growing in sophistication and complexity (33). A status quo that demands that physicians address pain without an integrated view of pain neurobiology and clinical care is untenable. It is important to recognize that rectifying this will require consistent long-term advocacy for pain education as a part of modern, patient-centered medicine curriculum.
Strong negative impact on mood is a prominent feature of pain. The significance of this for individuals, as well as for society, depends heavily on the meanings ascribed to pain. Pain meaning and responses to pain affect are often determined by the specifics of societal culture. Virtually nothing is known about how the culture of allopathic medicine has perpetuated the failure of medical schools to more vigorously take up the serious study of pain in an effort to alleviate human suffering. It could be argued that no subject in medicine today offers more opportunity for improving clinical care than does the study of pain.
We sought to address the challenges intrinsic to pain affect by constructing a pain portfolio with activities that directly communicated our expectation that students should engage in active, structured reflection about pain-related experiences and other tasks that would foster emotional development relevant to pain care. We defined reflection as the `measured appraisal of self and others with regards to thoughts, feelings and behaviors' (28). We provided specific guidance to students about our ideals for emotional developmental in a pain-care setting. Candid examination of oneself is not always an integral part of the basic sciences curriculum. As such, the portfolio compelled students to step outside their comfort zone. So although some students commented that reflection felt `forced', the assessment of the portfolios by faculty affirmed that this was an invaluable element of the course. We hope that the students refer back to their portfolios to benchmark professional and personal growth, and spur further progress. One exercise in particular, entitled `My commitment to patients in pain' serves as an important benchmark as students progress in their training. It is worth noting the expressions of gratitude from many students as they picked up their work.
The principal challenge faced by pain-expert medical faculty is resistance to adding material into an already overburdened medical school schedule. There is no simple solution to this problem although many different approaches have been tried (5;34). Regulatory requirements for pain education have been established by JCAHO for healthcare providers (35), however, the educational oversight organizations certifying medical schools do not specify guidelines for pain in medical education. Successful implementation of our pain course required advocacy by local pain champions and the receptiveness of medical school leadership. Consistent participation in the curriculum reform process allowed us to identify institutional needs that could be met through a pain intersession course.
Our colleagues in the allied health professions are making significant progress. The University of Toronto faculty has taught an inter-professional pain course for several years (36). This course was founded by a nurse pain-champion and is now led by a pain-expert physical therapist. The Toronto course brings nursing and medical students together with dentistry, physical therapy, occupational therapy and pharmacy. Inter-professional approaches do require both opportunities in the medical curriculum and alignment with other health professions.
In practical terms, resource requirements were high. The course required several years of planning. The small groups necessitated a large number of faculty be present simultaneously. Compared with a traditional format of the large lecture hall method of content delivery where one faculty member will address a full medical school class for an hour, the need for faculty in small-group teaching was much higher requiring nearly four faculty per content hour on average. Beyond this, a 75-page course workbook, 27-page workbook appendix (fast facts and other content), and a 32-page pain portfolio were created. This was made possible by philanthropic support for the curriculum but necessitated the efforts of multiple faculty and educational experts.
Going forward there are several important lessons learned. 1) Demonstrating the value of pain courses in general and that of pre-clinical courses in particular will demand concerted collaborative effort. 2) Defining the efficacy of specific learning approaches and matching content delivery methods with each learning task requires some pedagogical sophistication. 3) Removing barriers to the adoption of pain into the medical curriculum requires advocacy. 4) Teaching first year students requires a large investment of faculty time and effort. 5) Continued attention must be focused on enhancing students' awareness of and preparation to manage the emotional impacts of pain experiences. The ideal curriculum must concentrate on building reserves of emotional intelligence, strength, resilience and regulation, which can synergize with clinical knowledge in improving pain management. 6) Under the right circumstances, a healthy enthusiasm for improving clinical pain care is almost infectious.
Summary.
Innovations in medical education about pain are needed. Our aim was to design and deliver a new course for medical students addressing both the affective and cognitive dimensions of pain. Combining small-group sessions with pain-specialists, active-learning approaches to pain knowledge, and design-built elements to strengthen emotional skills was highly effective.
Supplementary Material
Acknowledgements
The authors wish to acknowledge the contributions of the following to the development of this curriculum: Drs. Rebecca Pearlman, Aakash Agarwal, Sabine Kost-Byerly and Stuart Grossman; and Members of the Pain Curriculum Development Team: Drs. Myron Yaster, Richard Meyer, Gayle Page, and Albert Wu. The work was supported through grants (to BBM) from the Mayday Fund and the Milbank Foundation for Rehabilitation Research. Dr. Murinson was the recipient of a NINDS Mentored Career Development Award Grant, number NS048146.
References
- (1).Bond MR, Dubner R, Jones LE, Meldrum ML. The History of the IASP: Progress in Pain since 1975. In: Merskey H, Loeser JD, Dubner R, editors. The Paths of Pain 1975–2005. IASP Press; Seattle: 2005. [Google Scholar]
- (2).Loeser JD. Multidisciplinary Pain Management. In: Merskey H, Loeser JD, Dubner R, editors. The Paths of Pain 1975–2005. IASP Press; Seattle: 2005. [Google Scholar]
- (3).Gibbins J, McCoubrie R, Maher J, Forbes K. Incorporating palliative care into undergraduate curricula: lessons for curriculum development. Med Educ. 2009 Aug;43(8):776–83. doi: 10.1111/j.1365-2923.2009.03400.x. [DOI] [PubMed] [Google Scholar]
- (4).Dubois MY, Gallagher RM, Lippe PM. Pain medicine position paper. Pain Med. 2009 Sep;10(6):972–1000. doi: 10.1111/j.1526-4637.2009.00696.x. [DOI] [PubMed] [Google Scholar]
- (5).Pilowsky I. An outline curriculum on pain for medical schools. Pain. 1988 Apr;33(1):1–2. doi: 10.1016/0304-3959(88)90196-0. [DOI] [PubMed] [Google Scholar]
- (6).Turner GH, Weiner DK. Essential components of a medical student curriculum on chronic pain management in older adults: results of a modified delphi process. Pain Med. 2002 Sep;3(3):240–52. doi: 10.1046/j.1526-4637.2002.02030.x. [DOI] [PubMed] [Google Scholar]
- (7).Watt-Watson J, Hunter J, Pennefather P, Librach L, Raman-Wilms L, Schreiber M, et al. An integrated undergraduate pain curriculum, based on IASP curricula, for six health science faculties. Pain. 2004 Jul;110(1–2):140–8. doi: 10.1016/j.pain.2004.03.019. [DOI] [PubMed] [Google Scholar]
- (8).Monin JK, Schulz R, Martire LM, Jennings JR, Lingler JH, Greenberg MS. Spouses' cardiovascular reactivity to their partners' suffering. J Gerontol B Psychol Sci Soc Sci. 2010 Mar;65B(2):195–201. doi: 10.1093/geronb/gbp133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (9).Barakat LP, Patterson CA, Daniel LC, Dampier C. Quality of life among adolescents with sickle cell disease: mediation of pain by internalizing symptoms and parenting stress. Health Qual Life Outcomes. 2008;6:60. doi: 10.1186/1477-7525-6-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (10).Bergstrom L, Richards L, Morse JM, Roberts J. How caregivers manage pain and distress in second-stage labor. J Midwifery Womens Health. 2010 Jan;55(1):38–45. doi: 10.1016/j.jmwh.2009.05.001. [DOI] [PubMed] [Google Scholar]
- (11).Murinson BB, Agarwal AK, Klick b, Haythornthwaite JA. Underestimation of pain by medical students is associated with negative emotional reactions to pain. J.Pain. 2007;8(4):S84. [Google Scholar]
- (12).Olthuis G, Dekkers W. Medical education, palliative care and moral attitude: some objectives and future perspectives. Med Educ. 2003 Oct;37(10):928–33. doi: 10.1046/j.1365-2923.2003.01635.x. [DOI] [PubMed] [Google Scholar]
- (13).Hundert EM, Douglas-Steele D, Bickel J. Context in medical education: the informal ethics curriculum. Med Educ. 1996 Sep;30(5):353–64. doi: 10.1111/j.1365-2923.1996.tb00847.x. [DOI] [PubMed] [Google Scholar]
- (14).Epstein RM, Hundert EM. Defining and assessing professional competence. JAMA. 2002 Jan 9;287(2):226–35. doi: 10.1001/jama.287.2.226. [DOI] [PubMed] [Google Scholar]
- (15).Flowers LK. The missing curriculum: experience with emotional competence education and training for premedical and medical students. J Natl Med Assoc. 2005 Sep;97(9):1280–7. [PMC free article] [PubMed] [Google Scholar]
- (16).Goldberg JL. Humanism or professionalism? The White Coat Ceremony and medical education. Acad Med. 2008 Aug;83(8):715–22. doi: 10.1097/ACM.0b013e31817eba30. [DOI] [PubMed] [Google Scholar]
- (17).Hojat M, Gonnella JS, Mangione S, Nasca TJ, Veloski JJ, Erdmann JB, et al. Empathy in medical students as related to academic performance, clinical competence and gender. Med Educ. 2002 Jun;36(6):522–7. doi: 10.1046/j.1365-2923.2002.01234.x. [DOI] [PubMed] [Google Scholar]
- (18).Roter DL, Frankel RM, Hall JA, Sluyter D. The expression of emotion through nonverbal behavior in medical visits. Mechanisms and outcomes. J Gen Intern Med. 2006 Jan;21(Suppl 1):S28–S34. doi: 10.1111/j.1525-1497.2006.00306.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (19).Dobie S. Viewpoint: reflections on a well-traveled path: self-awareness, mindful practice, and relationship-centered care as foundations for medical education. Acad Med. 2007 Apr;82(4):422–7. doi: 10.1097/01.ACM.0000259374.52323.62. [DOI] [PubMed] [Google Scholar]
- (20).Satterfield JM, Hughes E. Emotion skills training for medical students: a systematic review. Med Educ. 2007 Oct;41(10):935–41. doi: 10.1111/j.1365-2923.2007.02835.x. [DOI] [PubMed] [Google Scholar]
- (21).Wright S, Wong A, Newill C. The impact of role models on medical students. J Gen Intern Med. 1997 Jan;12(1):53–6. doi: 10.1046/j.1525-1497.1997.12109.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (22).Murinson BB, klick b, Haythornthwaite JA, Shochet R, Levine RB, Wright SM. Formative Experiences of Emerging Physicians: Gauging the Impact of Events That Occur During Medical School. Acad Med. 2010 Aug;85(8):1331–7. doi: 10.1097/ACM.0b013e3181e5d52a. [DOI] [PubMed] [Google Scholar]
- (23).Pitkala KH, Mantyranta T. Feelings related to first patient experiences in medical school. A qualitative study on students' personal portfolios. Patient Educ Couns. 2004 Aug;54(2):171–7. doi: 10.1016/S0738-3991(03)00209-X. [DOI] [PubMed] [Google Scholar]
- (24).Blasco PG, Moreto G, Levites MR. Teaching humanities through opera: leading medical students to reflective attitudes. Fam Med. 2005 Jan;37(1):18–20. [PubMed] [Google Scholar]
- (25).Levine RB, Kern DE, Wright SM. The impact of prompted narrative writing during internship on reflective practice: a qualitative study. Adv Health Sci Educ Theory Pract. 2008 Dec;13(5):723–33. doi: 10.1007/s10459-007-9079-x. [DOI] [PubMed] [Google Scholar]
- (26).Torppa MA, Makkonen E, Martenson C, Pitkala KH. A qualitative analysis of student Balint groups in medical education: contexts and triggers of case presentations and discussion themes. Patient Educ Couns. 2008 Jul;72(1):5–11. doi: 10.1016/j.pec.2008.01.012. [DOI] [PubMed] [Google Scholar]
- (27).Bellini LM, Shea JA. Mood change and empathy decline persist during three years of internal medicine training. Acad Med. 2005 Feb;80(2):164–7. doi: 10.1097/00001888-200502000-00013. [DOI] [PubMed] [Google Scholar]
- (28).Murinson BB, Agarwal AK, Haythornthwaite JA. Cognitive expertise, emotional development, and reflective capacity: clinical skills for improved pain care. J Pain. 2008 Nov;9(11):975–83. doi: 10.1016/j.jpain.2008.07.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (29).Wiener CM, Thomas PA, Goodspeed E, Valle D, Nichols DG. “Genes to society”--the logic and process of the new curriculum for the Johns Hopkins University School of Medicine. Acad Med. 2010 Mar;85(3):498–506. doi: 10.1097/ACM.0b013e3181ccbebf. [DOI] [PubMed] [Google Scholar]
- (30).Murinson BB. Pain and the Humanities: Exploring the Meaning of Pain in Medicine Through Drama, Literature, Fine Arts and Philosophy. MedEdPORTAL 2010 July 27Available from: URL: http://services.aamc.org/30/mededportal/servlet/s/segment/mededportal/?subid=8129.
- (31).Kern DE, Thomas PA, Howard DM, Bass EB. Curriculum Development for medical education: A six-step approach. 1 ed. Johns Hopkins University Press; Baltimore: 1998. [Google Scholar]
- (32).Giordano J. Moral agency in pain medicine: philosophy, practice and virtue. Pain Physician. 2006 Jan;9(1):41–6. [PubMed] [Google Scholar]
- (33).Sullivan MD, Edlund MJ, Fan MY, Devries A, Brennan BJ, Martin BC. Trends in use of opioids for non-cancer pain conditions 2000–2005 in commercial and Medicaid insurance plans: the TROUP study. Pain. 2008 Aug 31;138(2):440–9. doi: 10.1016/j.pain.2008.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- (34).Chang HM. Educating medical students in pain medicine and palliative care. Pain Med. 2002 Sep;3(3):194–5. doi: 10.1046/j.1526-4637.2002.02040.x. [DOI] [PubMed] [Google Scholar]
- (35).JCAHO . Improving the Quality of Pain Management Through Measurement and Action. Joint Commission on Accreditation of Healthcare Organizations; Oakbrook Terrace, Illinois: 2003. [Google Scholar]
- (36).Hunter J, Watt-Watson J, McGillion M, Raman-Wilms L, Cockburn L, Lax L, et al. An interfaculty pain curriculum: lessons learned from six years experience. Pain. 2008 Nov 15;140(1):74–86. doi: 10.1016/j.pain.2008.07.010. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.