Abstract
Objective
Recent models suggest that generalized anxiety disorder (GAD) symptoms may be maintained by emotional processing avoidance and interpersonal problems.
Method
This is the first randomized controlled trial to test directly whether cognitive-behavioral therapy (CBT) could be augmented with the addition of a module targeting interpersonal problems and emotional processing. Eighty-three primarily White participants (mean age = 37) with a principle diagnosis of GAD were recruited from the community. Participants were assigned randomly to CBT plus supportive listening (n = 40) or to CBT plus interpersonal and emotional processing therapy (n = 43) within a study using an additive design. Doctoral-level psychologists with full-time private practices treated participants in an outpatient clinic. Using blind assessors, participants were assessed at pretreatment, posttreatment, 6-month, 1-year, and 2-year follow-up with a composite of self-report and assessor-rated GAD symptom measures (the Penn State Worry Questionnaire; T. J. Meyer, M. L. Miller, R. L. Metzger, & T. D. Borkovec, 1990; Hamilton Anxiety Rating Scale; M. Hamilton, 1959; assessor severity rating; State–Trait Anxiety Inventory-Trait Version; C. D. Spielberger, R. L. Gorsuch, R. Lushene, P. R. Vagg, & G. A. Jacobs, 1983) as well as with indices of clinically significant change.
Results
Mixed models analysis of all randomized participants showed very large within-treatment effect sizes for both treatments (CI = [-.40, -.28], d = 1.86) with no significant differences at post (CI = [-.09, .07], d = .07) or 2-year follow-up (CI = [-.01, .01]), d = .12). There was also no statistical difference between compared treatments on clinically significant change based on chi-square analysis.
Conclusions
Interpersonal and emotional processing techniques may not augment CBT for all GAD participants.
Keywords: generalized anxiety disorder, emotional processing, emotional avoidance, interpersonal problems, cognitive-behavioral therapy
On the basis of several clinical trials (see Newman & Borkovec, 2002), cognitive-behavioral therapy (CBT) presently stands as the only psychotherapy to meet criteria as an empirically supported treatment for generalized anxiety disorder (GAD; Chambless & Ollendick, 2001). Nonetheless, significant room for improvement exists. A marked percentage of clients continue to experience clinically significant anxious symptoms after treatment (Borkovec & Ruscio, 2001) and fail to demonstrate sustained reduction in GAD symptoms (Westen & Morrison, 2001).
Failure to achieve and/or maintain gains from CBT for GAD might be due to the omission of techniques to address variables that may be maintaining the disorder. Among such variables, both emotional processing avoidance and interpersonal problems are prevalent in people with GAD, and researchers have provided well-developed models for their roles in the maintenance of worry and GAD (e.g., Borkovec, Alcaine, & Behar, 2004; Newman & Erickson, 2010). In one of these models, worry, the central feature of GAD, is hypothesized to be a means to avoid emotional processing (Borkovec et al., 2004). In line with this model, the predominantly verbal-linguistic nature of worrisome thinking (and its lessened concrete imagery) inhibit cardiovascular response to feared material, leading to a dampening of emotional learning and a maintenance of worrisome thinking via negative reinforcement (Borkovec & Hu, 1990; Llera & Newman, 2010). Moreover, people with GAD report using worry as an emotion control tactic (Borkovec & Roemer, 1995) and experience greater perceived threat and discomfort from emotions compared with nonanxious controls (Llera & Newman, 2010; Mennin, Heimberg, Turk, & Fresco, 2005). Unfortunately, attempts to control emotion are not beneficial and may ultimately lead to periods of emotion cue hypervigilence and labile emotionality (Newman, Castonguay, Borkovec, & Molnar, 2004). In support of this idea, people with GAD report heightened intensity of emotions (Mennin, Holaway, Fresco, Moore, & Heimberg, 2007) and are more reactive than nonanxious participants to expressions of negative emotions in others (Erickson & Newman, 2007). The above results suggest that including emotional processing techniques in the treatment of individuals with GAD to help them experience uncomfortable emotions may reduce their chronic worrying.
In addition to difficulty with emotions, individuals with GAD have interpersonal difficulties (e.g., Borkovec, Newman, Pincus, & Lytle, 2002). According to the interpersonal model of GAD (Newman & Erickson, 2010), interpersonal problems arise from nonadaptive attachment relationships (Cassidy, Lichtenstein-Phelps, Sibrava, Thomas, & Borkovec, 2009), leading to biased interpersonal cognitions (Erickson & Newman, 2007; Mogg, Millar, & Bradley, 2000), interpersonal skills deficits, and habitual nonadaptive ways of relating to others (Przeworski, Newman, Pincus, Kasoff, Yamasaki, Castonguay, & Berlin, in press; Salzer, Pincus, Hoyer, Kreische, Leichsenring, & Leibing, 2008). In fact, people with GAD report childhood experiences in which caregivers are inconsistently available (Cassidy et al., 2009), pulling them into a developmentally premature state of needing to take care of the caregiver and/or oneself. In this context, negative interpersonal working models, worry, and nonadaptive social behaviors may be used to cope with a potentially dangerous, unpredictable world lacking consistent support.
Despite evidence that both emotional processing avoidance and interpersonal issues may be central to the maintenance of GAD symptoms, present CBT protocols may be inadequate to address successfully these issues. For example, level of emotional processing was significantly lower in CBT than in a reflective listening condition (Borkovec & Costello, 1993). Standard CBT protocols are also limited in addressing interpersonal issues. For example, Borkovec et al. (2002) found that clients endorsing pretherapy interpersonal problems associated with dominance responded less favorably to CBT than clients without these interpersonal difficulties, and such problems left untreated predicted failure to maintain follow-up gains. Such evidence points to therapy techniques to address interpersonal problems such as attachment difficulties, interpersonal skills deficits, problematic interpersonal behaviors, and ways in which GAD individuals’ interpersonal behaviors fail to elicit the responses from others to meet their needs.
For these reasons, we developed an approach to CBT for GAD that included techniques designed to address emotional processing avoidance and interpersonal problems (Newman et al., 2004). In an initial open trial, our combination of CBT with interpersonal and emotional processing techniques generated promising results (Newman, Castonguay, Borkovec, Fisher, & Nordberg, 2008). Although other studies have used treatments to address emotional processing avoidance in GAD (e.g., Roemer, Orsillo, & Salters-Pedneault, 2008), the present study was the first randomized controlled trial to examine directly whether the addition of techniques purported to address emotional processing avoidance and interpersonal problems would lead to superior outcome compared with standard CBT for GAD. We predicted that CBT plus interpersonal and emotional processing therapy (CBT + I/EP) would lead to better outcomes, particularly at long-term follow-up (due to the entrenched nature of interpersonal problems requiring more time before change would occur) than would CBT plus supportive listening (CBT + SL).
Method
Similar to our open trial (Newman et al., 2008), rather than involve a seamless integration of CBT and I/EP techniques (where any of these techniques could be used at any time), our design, for scientific reasons, involved a separation and sequential combination of two distinct therapeutic segments. Specifically, we compared 50 min of CBT, followed by 50 min of I/EP, with 50 min of CBT, followed by 50 min of supportive listening (SL). Controlling for common factors, such a between-group additive design is not only a method to answer directly whether CBT can be improved upon, but it is also a method to examine whether I/EP causes a significant increment in efficacy beyond CBT (see Behar & Borkovec, 2003).
Participants
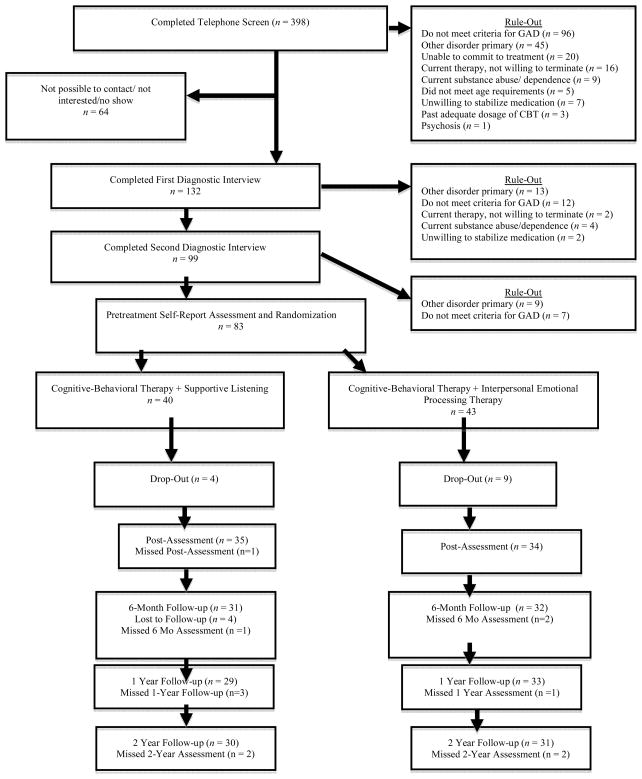
Admission criteria included agreement from two separate diagnostic interviews on the following: a principal diagnosis of Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM–IV) GAD1; a Clinician’s Severity Rating for GAD (part of the Anxiety Disorders Interview Schedule for DSM–IV; Brown, Di Nardo, & Barlow, 1994) of 4 (moderate) or greater; absence of concurrent psychotherapy or past adequate dosage of CBT (at least eight sessions focused on cognitive and behavioral techniques); current stable dose of psychotropic medication (for at least 6 weeks) or medication-free; willingness to maintain stability in medication use during the 14-week therapy period with their physician’s approval (daily diary monitoring of drug use indicated compliance with this request); no medical contributions to the anxiety; absence of substance abuse, psychosis, and organic brain syndrome; and be between 18 and 65 years of age (see Figure 1 for CONSORT flow chart). Thirteen people dropped out at early stages of treatment (four in CBT-SL and nine in CBT-I/EP; χ2(1, N = 83) = 1.87, p = .17. No clients were removed for deteriorating conditions during therapy. No pretreatment client characteristics were significantly different across conditions (see Table 1). Mental health practitioners had referred five; the remainder had responded to media advertisements. All participants consented to the study, and Institutional Review Board approval was attained.
Figure 1.
Flow of Participants Through Each Stage of the Study
Table 1.
Comorbid Diagnoses and Demographic Characteristics of the Sample
| CBT+IEP n = 43 | CBT+SL n = 40 | χ2 | p | d | Total n = 83 | |
|---|---|---|---|---|---|---|
| Major Depression | 25.6% (n=11) | 27.5% (n=11) | 26.5% (n = 22) | |||
| Depressive Disorder NOS | 0% (n = 0) | 2.5% (n = 1) | 1.2% (n = 1) | |||
| Bipolar Disorder | 2.5% (n = 1) | 0% (n = 0) | 1.2% (n = 1) | |||
| Obsessive Compulsive Disorder | 4.7% (n = 2) | 7.5% (n = 3) | 6% (n = 5) | |||
| PTSD | 7% (n = 3) | 5% (n = 2) | 6% (n = 5) | |||
| Social Phobia | 65.1% (n = 28) | 60% (n = 24) | 62.7% (n = 52) | |||
| Specific Phobia | 44.2% (n = 19) | 30% (n = 12) | 37.3% (n = 31) | |||
| Panic Disorder | 18.6% (n = 8) | 17.5 % (n = 7) | 18.1% (n = 15) | |||
| Agoraphobia | 14% (n = 6) | 12.5% (n = 5) | 13.3% (n = 11) | |||
| Dysthymia | 9.3% (n = 4) | 5% (n = 2) | 7.2% (n = 6) | |||
| Pain Disorder | 4.7% (n = 2) | 5% (n = 2) | 4.8% (n = 4) | |||
| Hypochondriasis | 7% (n = 3) | 2.5% (n = 1) | 4.8% (n = 4) | |||
| At least one comorbid Axis I disorder | 86% (n = 37) | 82.5% (n = 33) | 0.20 | .66 | 0.10 | 84.3% (n = 70) |
| Borderline Personality Disorder | 7.1% (n=3) | 2.6% (n=1) | 4.9% (n = 4) | |||
| Narcissistic Personality Disorder | 4.8% (n=2) | 5.1% (n =2) | 4.9% (n = 4) | |||
| Avoidant Personality Disorder | 33.3% (n = 14) | 25.6% (n =10) | 29.6% (n = 24) | |||
| Depressive Personality Disorder | 23.8% (n = 10) | 46.2% (n = 18) | 34.6% (n = 28) | |||
| Dependent Personality Disorder | 2.4% (n = 1) | 7.7% (n = 3) | 4.9% (n = 4) | |||
| Negativistic Personality Disorder | 11.9% (n = 5) | 12.8% (n = 5) | 12.3% (n = 10) | |||
| Obsessive Compulsive Personality Disorder | 33.3% (n =14) | 46.2% (n = 18) | 39.5% (n = 32) | |||
| Paranoid Personality Disorder | 7.1% (n = 3) | 17.9% (n = 7) | 12.3% (n = 10) | |||
| At least one personality disorder | 65% (n = 26) | 71.1% (n = 27) | 0.33 | .57 | 0.13 | 67.9% (n = 53) |
|
| ||||||
| I/EP+CBT n = 43 | CBT+SL n = 40 | χ2 or F value | p | d | Total n = 83 | |
|
| ||||||
| Age | 36.93 | 37.39 | 0.03 | .86 | 0.04 | 37.41 |
| M (SD) | (12.31) | (11.99) | (12.24) | |||
| Duration of GAD in years | 11.26 | 11.51 | 0.01 | .94 | 0.02 | 11.95 |
| M (SD) | (13.56) | (13.97) | (14.94) | |||
| Gender | 0.61 | .44 | 0.17 | |||
| Female | 72.1% (n = 31) | 80% (n = 32) | 75% (n = 63) | |||
| Male | 27.9% (n = 12) | 20% (n = 8) | 25% (n = 21) | |||
| Ethnicity | 0.61 | .53 | 0.17 | |||
| White | 93% (n = 40) | 90% (n = 36) | 91.7% (n = 77) | |||
| African American | 0% (n = 0) | 2.5% (n = 1) | 1.2% (n = 1) | |||
| Asian American | 2.3% (n = 1) | 5% (n = 2) | 3.6% (n = 3) | |||
| Hispanic | 4.7% (n = 2) | 2.5% (n = 1) | 3.6% (n = 3) | |||
| Education | 0.01 | .91 | 0.03 | |||
| High School | 30.2% (n = 13) | 17.5% (n = 7) | 23.8% (n = 20) | |||
| College | 34.9% (n = 15) | 60% (n = 24) | 46.5% (n = 39) | |||
| Masters | 30.2% (n = 13) | 20% (n = 8) | 25% (n = 21) | |||
| Ph.D. | 4.7% (n = 2) | 2.5% (n = 1) | 4.8% (n = 4) | |||
| Marital Status | 3.11 | .38 | 0.37 | |||
| Single | 46.5% (n = 20) | 35% (n = 14) | 40.5% (n = 34) | |||
| Married | 39.5% (n = 17) | 52.5% (n = 21) | 46.4% (n = 39) | |||
| Divorced | 14% (n = 6) | 12.5% (n = 5) | 13.1% (n = 11) | |||
| On Psychotropic Medication | 0.48 | .49 | 0.15 | |||
| Yes | 37.2% (n = 16) | 30% (n = 12) | 34.5% (n = 29) | |||
| No | 62.8% (n = 27) | 70% (n = 28) | 65.5% (n = 55) | |||
Note. CBT = cognitive-behavioral therapy; IEP = interpersonal and emotional processing therapy; SL = supportive listening; NOS = not otherwise specified; PTSD = posttraumatic stress disorder; GAD = generalized anxiety disorder.
Three experienced doctoral-level psychologists conducted the therapy at an outpatient clinic. Assignment to therapist was random within restraints of availability and caseload; however, equal numbers of clients from each condition were assigned to each therapist. All three therapists had received extensive training and 2 years of experience with our treatment and additive design structure in the prior open trial (Newman et al., 2008). The first and third author provided weekly individual supervision of each therapist throughout the project.
Measures
Clinician-Administered Measures
The Anxiety Disorders Interview Schedule for DSM–IV (ADIS-IV; Brown et al., 1994) has well-established reliability (κs ranging from .67 to .72) for most disorders except dysthymia (κ = .22; Brown, Di Nardo, Lehman, & Campbell, 2001). For our interviewers, kappa agreement for GAD was .78 and for comorbid diagnoses ranged from .68 to 1 based on dual interviews. Interviewers assigned a 0 (none) to 8(very severely disturbing/disabling) Clinicians’ Severity Rating (CSR) to reflect degree of distress and impairment associated with each disorder. Reliability of CSRs for GAD using Finn’s r (Whitehurst, 1984), which corrects for a restricted range, was .74. The Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II; First, Gibbon, Spitzer, Williams, & Benjamin, 1997) is an interview for the diagnosis of personality disorders, with interrater agreement ranging from .48 to .98 (Maffei et al., 1997). Interrater agreement for our raters (based on a random selection of audiotapes of 20% of our interviews) was good to excellent across personality disorder diagnoses (κs = .64 –1). The Hamilton Anxiety Rating Scale (HARS; Hamilton, 1959) is a 14-item clinician-administered measure of severity of anxious symptomatology. Internal consistency (α = .77–.81) ranged from adequate to good (Moras, di Nardo, & Barlow, 1992; α = .87 in the present study). Interrater reliability has ranged from an intraclass correlation (ICC) of .74 –.96 (Bruss, Gruenberg, Goldstein, & Barber, 1994; ICC = .89 in the present study). The Hamilton Rating Scale for Depression (HRSD; Hamilton, 1960) is a 13-item scale assessing severity of depressive symptoms. Internal consistency of the HRSD ranges from adequate to good (α = .73–.81; Hamilton, 1960; Moras et al., 1992; α = .78 in the present sample). Interrater reliabilities of the total score range from ICC of .78 –.82 (Moras et al., 1992; ICC = .86 in the present sample).
Self-report outcome measures
The Penn State Worry Questionnaire (PSWQ; Meyer, Miller, Metzger, & Borkovec, 1990) is a 16–item measure of frequency and intensity of worry. It has high internal consistency (Meyer et al., 1990; .84 in the present sample), test–retest reliability ranging from .74 to .93, as well as strong convergent and discriminant validity (Molina & Borkovec, 1994). The State–Trait Anxiety Inventory-Trait Version (STAI-T; Spielberger, Gorsuch, Lushene, Vagg, & Jacobs, 1983) is a 20-item measure of trait anxiety with high internal consistency (.88 in the present sample), good test–retest reliability (high 70s), and strong convergent and discriminant validity (Spielberger et al., 1983). Due to its bifactorial nature (Bieling, Antony, & Swinson, 1998), the anxiety factor was used to measure trait anxiety (α = .72 in this sample). The Reactions to Relaxation and Arousal Questionnaire (RRAQ; Heide & Borkovec, 1983) is a nine-item factor analytically derived measure of fear of relaxation with a Cronbach’s alpha of .85 (α = .79 in the present sample), high test–retest reliability (.83), and strong convergent and discriminant validity (Newman et al., 2002). The Inventory of Interpersonal Problems-Circumplex Scale (IIP-C; Alden, Wiggins, & Pincus, 1990) measured interpersonal functioning. Its eight scales form a circumplex of interpersonal problems around the dimensions of dominance and nurturance with strong test–retest reliability (r = .98) and internal consistency of subscales (α = .82 – .93; Horowitz, Rosenberg, Baer, Ureno, & Vilasenor, 1988; α = .76 – .93 in the present sample). The Expectancy/Credibility scale (Devilly & Borkovec, 2000) was also administered at the end of each hour (following CBT and again following SL or I/EP) of the first therapy session.
Procedure
Selection and assessor outcome ratings
Clients were enrolled over a 5-year period from 1998 to 2003. Follow-up assessments were conducted from 1998 to 2005. Cell size was determined by a power analysis on the basis of between-groups effect sizes (average Cohen’s f = 0.32) from a prior component control investigation (Borkovec & Costello, 1993). Assuming alpha = .05, 25 clients per condition ensured power at .80 for detecting between-group differences (Neter, Wasserman, & Kutner, 1990).
Participants were recruited on the basis of media advertisements and referrals from clinicians. Advanced clinical graduate students trained to reliability in diagnostic interviewing conducted a 30-min phone interview to determine likely diagnostic suitability. This interview included screening for symptoms of GAD and common comorbid disorders, exclusion criteria, and availability for therapy. For those not ruled out during the phone screen, interviewers administered in person the ADIS, which included the HARS, the HRSD, and CSRs. A second ADIS to reduce likelihood of false-positive cases was given within 2 weeks by the therapist who would see the client in therapy upon acceptance into the trial. The second ADIS was administered only to those not ruled out during the first ADIS interview; however, interviewers were not provided with information about comorbid diagnoses made by the first interviewer until after their interview (i.e., if disagreement occurred). Pretreatment diagnoses, both primary and comorbid, were based on consensus between the independent structured interviewers.
At a separate pretreatment interview, assessors administered the SCID-II Personality Disorders Questionnaire followed by the SCID-II (to confirm endorsed diagnoses on the questionnaire), the STAI-T, RRAQ, IIP-C, and the PSWQ. The latter measures were given again at the post-and follow-up ADIS assessments. For postassessment, a briefer version of the ADIS (assessing only those diagnoses identified at pretherapy) was re-administered 10-14 days after the last therapy session and at 6- and 12- month follow-up assessment; the complete ADIS and rating scales were given at 24-month follow-up. Assessors administering preassessments to a client also administered the postassessment to that client; this was the case at follow-up whenever possible. Assessors were uninformed of therapy condition by preventing their access to the client during therapy and to session tape recordings or any other information pertaining to clients’ condition status. Once all baseline interviews and the self-report session had been completed and clients’ eligibility had been confirmed, the first author randomly assigned clients to treatment using a random numbers table. The first author then met with clients for the only time to reveal their treatment assignment and to provide an overview of the treatment.
Therapy
CBT
All clients received CBT during the first 50 min of 14 2-hr sessions (each of two 50-min segments of each session was followed by a 10-min period to complete process measures, which will be the focus of future publications). Targeting intrapersonal aspects of anxious experience, these techniques were part of the CBT protocol previously developed and tested at Pennsylvania State University (Borkovec et al., 2002). As described in detail elsewhere (Newman & Borkovec, 2002), these techniques included self-monitoring of anxiety cues, relaxation methods, self-controlled desensitization, and cognitive restructuring. During CBT, therapists were allowed to address only the learning and application of these methods as they related to intrapersonal anxious experience. For example, when doing cognitive therapy with aspects of client anxiety that related to other people, the therapist and client could work on identifying nonadaptive thoughts and on logical analysis of such cognitions to generate more accurate ways of perceiving. However, the therapist could not work on developmental origins, the deepening of affective experience, analysis of how client behavior may have been contributing to relationship difficulties, behavioral interpersonal skill training, and the like.
Interpersonal/Emotional Processing Segment
This segment was informed by Safran & Segal’s (1990) model of interpersonal schema, which provides a coherent integration of cognitive, interpersonal, and emotional issues in human functioning and therapy change. However, in contrast to Safran’s model, for the purpose of tailoring the treatment to GAD, this segment was specifically designed to address interpersonal problems and to facilitate emotional processing without the direct integration of cognitive techniques. On the basis of research on the nature (verbal linguistic) and function (emotional processing avoidance) of worry in GAD, it was assumed that the examination and challenge of worry as used in our previous CBT trials would interfere with the fostering of emotional processing at the core of I/EP.
The goals of I/EP were (a) identification of interpersonal needs, past and current patterns of interpersonal behavior that attempt to satisfy those needs, and emotional experience that underlies these; (b) generation of more effective interpersonal behavior to better satisfy needs; and (c) identification and processing of avoided emotion associated with all therapeutic content. The interventions were based on the following principles: emphasis on phenomenological experience; therapists’ use of their own emotional experience to identify interpersonal markers; use of the therapeutic relationship to explore affective processes and interpersonal patterns, with therapists’ assuming responsibility for their role in the interactions; promotion of generalization via exploration of between-session events and provision of homework experiments; detection of alliance ruptures and provision of emotionally corrective experiences in their resolution; processing of patient’s affective experiencing in relation to past, current, and in-session interpersonal relationships using emotion-focused techniques (e.g., Greenberg, 2002); and skill training methods to provide more effective interpersonal behaviors to satisfy identified needs.
SL segment
This segment was adopted directly from the SL manual of our prior trials (see Borkovec et al., 2002). Clients were told that this segment involves exploration of important life experiences in a quiet, relaxed atmosphere where therapists’ goals are to facilitate and deepen knowledge about self and anxiety. This segment was presented as an inward journey that might be additionally helpful in changing anxious experience and increasing self-confidence. Therapists’ roles were to provide an opportunity for self-reflection in a safe environment to facilitate change. Clients’ roles were to emphasize their unique efforts to discover new strengths through introspection. Therapists were to facilitate the acceptance of ongoing experience via supportive statements, reflective listening, and empathic communications. Therapists were not allowed to use any methods to deepen clients’ emotional experience. Provision of any direct suggestions, advice, or coping methods was also prohibited.
CBT always preceded SL or I/EP because engaging in specific alliance rupture repair methods described in Safran & Segal (1990) were allowed only in the I/EP segments (as they were considered interpersonal interventions). If signs of a rupture emerged during CBT, therapists could listen and empathize with clients’ expressions and/or intervene using evidence or other techniques allowed within the CBT model. However, for those assigned to CBT + I/EP, additional alliance rupture repair methods could not be used until the next hour. Within SL, therapists were not allowed to use alliance repair techniques beyond listening and empathizing.
Adherence Checks
Trained by the second author, graduate student coders read carefully the treatment manuals and coded several sessions from our previous open trial for calibration purposes before being assigned sessions to rate. They rated every therapist utterance on 100% of three audiotaped sessions randomly selected from early, middle, and late sessions for each client. Ratings were categorical by content of therapists’ verbalizations and classified by checklist representing all techniques from the behavioral, cognitive, interpersonal, emotional processing, and SL treatment protocols. Such ratings were separately obtained from CBT, I/EP, and SL segments of each chosen session. A priori criteria required no more than one nontrivial protocol break (e.g., therapist exploration during CBT of his or her own contribution to an alliance rupture and the impact it has had on a client) for any one client to be included in final data analyses. Of 11,453 checked utterances, zero nontrivial protocol breaches were detected, and only 14 were coded as trivial (e.g., therapist presented some brief psychoeducational information about GAD during an SL segment), two occurring in CBT segments and 12 occurring in SL segments.
Quality Checks
Jeremy Safran rated 100% of two randomly selected sessions (first and second half of sessions) for each client, using (a) our Cognitive Therapy Quality Scale, incorporating Young and Beck’s (1980) Scale into our further-elaborated scale to assess the quality of the first 50-min CBT intervention and (b) our I/EP and SL Scales, developed for this project from the manual sections for these segments and based on items contained in other competency scales (e.g., Safran & Segal, 1990) to assess the quality of the second 50-min intervention (I/EP or SL). All rated sessions met a priori criteria (a score of 3 [“satisfactory”]) or more in CBT and I/EP segments on an overall rating item (0 = poor; 6 = excellent) for this session; an average of 3 or above (based on the same Likert scale) on the four items of the SL reflective listening quality scale (which did not have an “overall” quality rating) for the client to be included in the final analyses. Average ratings were 4.8 for CBT, 4.31 for I/EP, and 4.7 for SL
Results
Statistical Analyses
We created a single outcome variable for symptoms of GAD, using a composite score of CSRs for GAD, the PSWQ, the HARS, and the anxiety scale of the STAI-T. Significant correlations between these measures ranged from .57 to .84. Raw scores were converted to standardized z scores and averaged for each participant. Primary outcome measures were this composite measure, in conjunction with clinically significant change measures. Secondary outcome measures were HRSD, additional treatment seeking, and the IIP-C. As noted earlier, the designated time point of interest was the 2-year follow-up. Unless otherwise noted, we examined group differences using linear mixed-effect models (Raudenbush & Bryk, 2002), which account for nesting inherent in repeated measurement of the same person over time.
Random effects were determined with restricted maximum likelihood estimation and fixed effects with full maximum likelihood estimation. The unit of measurement at Level 1 was time, and at Level 2 was the individual. Models were based on a piecewise analysis of time, as opposed to a single time coefficient. Piecewise analyses allow for the representation of discrete multiple time periods by modeling separate variables (and therefore separate coefficients and slopes) for these periods. The treatment and follow-up periods can be conceptualized as discrete and yet represented within the same model. Piece 1 was the treatment period, from pretreatment to posttreatment. Piece 2 was the posttreatment period including 6-, 12-, and 24-month follow-ups. Piece 1 was coded to allow for the retention of all observation points while holding posttreatment effects constant during the follow-up period. Piece 2 was coded to remove treatment period effects from the analysis of follow-up effects. Random effects for variation at the intercept, and in the slope for Piece 1 and Piece 2 were entered first into each model and were retained when significant. At the second step, we entered fixed effects for Piece 1, Piece 2, condition, and the Piece 1 × Condition and Piece 2 × Condition interactions, into the model.
We examined data for skew and kurtosis and found them to be within normal range at all time points. Because it is a central assumption in the analysis of multilevel data using maximum likelihood estimation, we tested whether relationships between independent and dependent variables were independent of missing data patterns using pattern-mixture models (Gallop & Tasca, 2009). In this analysis, completers with missing data during the follow-up period (Pattern 1, n = 15), and dropouts (pattern 2, n = 13), were compared with completers with no missing data (n = 55). Random effects for Pattern 1 and Pattern 2 were not significant. Random effects for intercept and piecewise time for each model were consistent with those reported below for standard mixed-effect models. Fixed effects for (a) Piece 1 × Condition × Pattern 1, (b) Piece 2 × Condition × Pattern 1, and (c) Condition × Pattern 2 were also nonsignificant in all cases.2 These results indicated that missingness did not meaningfully affect the rate of change by condition for any of the dependent variables and that full information maximum likelihood estimation is an appropriate method of estimation for our data. We therefore retained all participants, including dropouts, using the original raw data.3 As recommended by Dunlap, Cortina, Vaslow, and Burke (1996), we calculated Cohen’s d using the between-groups t-test value: d = t(2/n).
Similar to Borkovec and Costello (1993), we calculated endstate functioning by summing the number of the above four GAD symptom measures plus the RRAQ on which the client either fell within one standard deviation of the mean of nonanxious normative samples and outside of the range of the standard deviation from the mean of the anxious sample or a score that exceeded a face-valid level of meaningful change when norms were not available (a score of 3 or less on the 9-point CSR). Norms from nonanxious participants for the HARS, STAI-T, RRAQ, and PSWQ were based on Butler, Fennell, Robson, and Gelder (1991); , Spielberger et al. (1983), Borkovec and Costello (1993), and Molina and Borkovec (1994), respectively. High endstate functioning was defined as meeting endstate criteria on at least three of the five measures. Responder status was defined as at least 20% change from pretherapy levels on at least three of the five measures. We also examined the impact of our therapy on clinically significant change in the IIP-C. We defined high endstate functioning on this measure as scoring within the normal range on at least six of the eight IIP-C subscales. Norms for this scale from non-anxious participants were based on Horowitz et al. (1988).
Preliminary Analyses
A multivariate analysis of variance found no significant differences between therapy conditions at baseline on the composite outcome measure, F(1,80) = 1.14, p = .29, d = 0.24, HRSD, F(1,80) = .020, p = .89, d = .04, and IIP-C total score, F(1,80) = 2.17, p = .15, d=.33.
Process Measures
We compared separately expectancy and credibility with reference to the first hour of therapy, wherein participants in both groups received CBT, and measures with reference to the second hour, wherein one group received SL and the other group received I/EP. A one-way multivariate analysis of variance obtained at the end of each segment of the first session yielded no significant differences between conditions, F(4, 63) = 0.996, p = .993, d = 0.24, with moderately high expectancy for the first hour (CBT + SL, M = 67.00%, SD = 19.11 vs. CBT + I/EP, M = 68.18%, SD = 20.07, d = 0.06) and the second hour (CBT + SL, M = 65.86%, SD = 20.67 vs. CBT + I/EP, M = 64.85%, SD = 22.38, d = 0.05) and a high degree of credibility for the first hour (CBT + SL, M = 22.14, SD = 3.9 vs. CBT + I/EP, M = 22.45, SD = 3.13, d = 0.09) and the second hour (CBT + SL, M = 20.70, SD = 5.20 vs. CBT + I/EP, M = 20.67, SD = 5.27, d = 0.01).
Effect of Treatment on GAD Symptom Severity
On the composite primary outcome measure for GAD symptoms, we found significant within-individual variation at the intercept and in the slopes for Piece 1 and Piece 2. Following Step 2, only the main effect for Piece 1 was significant (ß = −.34, SE = .03), t(77) = −11.86, p < .0001, 95% CI = [−.40, −.28], d = 1.86, reflecting a decrease in GAD symptom severity from pre-to posttreatment, irrespective of condition. Main effects for the follow-up period, (ß = .002, SE = .005), t(77) = 0.39, p = .70, 95% CI = [−.01, .01], d = 0.06; condition (ß = −.06, SE = .10), t(77) = −.60, p = .55, 95% CI = [−.26, .14], d = .13, Piece 1 × Condition ( ß = −.01, SE = .04), t(77) = −.31, p= .76, 95% CI = [−.09, .07], d = 0.07, and Piece 2 × Condition (ß = −.004, SE = .007), t(77) = −0.56, p = .58, 95% CI = [−.01, .01], d = .12, were all non-significant. Nonsignificant effects for Piece 2 indicate maintenance of therapeutic gains in both conditions across the 2-year follow-up period. Table 2 lists the means and standard deviations for each time period for each measure.
Table 2.
Means and Standard Deviations for All Outcome Measures Across All Time Points
| Measure and Condition | Pretreatment M (SD) | Posttreatment M (SD) | 6-month M (SD) | 12-month M (SD) | 24-month M (SD) |
|---|---|---|---|---|---|
| Penn State Worry Questionnaire | |||||
| CBT-SL | 67.55 (8.08) | 49.06 (11.13) | 50.67 (11.63) | 50.63 (11.09) | 50.75 (12.7) |
| CBT/IEP | 67.14 (8.18) | 51.00 (11.99) | 50.26 (12.15) | 51.18 (11.35) | 49.16 (13.9) |
| Clinician’s Severity Rating | |||||
| CBT-SL | 6.00 (0.81) | 3.33 (1.56) | 3.06 (1.56) | 3.03 (1.51) | 3.11 (1.65) |
| CBT/IEP | 5.97 (0.77) | 2.83 (1.85) | 2.76 (1.28) | 2.54 (1.51) | 2.53 (1.92) |
| Hamilton Anxiety | |||||
| CBT-SL | 22.34 (7.03) | 11.49 (7.38) | 10.95 (7.35) | 11.72 (7.56) | 11.38 (7.76) |
| CBT/IEP | 22.31 (6.37) | 8.77 (4.90) | 10.15 (6.66) | 10.57 (6.79) | 9.38 (7.57) |
| State Trait Anxiety Inventory (anxiety subscale) | |||||
| CBT-SL | 19.44 (3.36) | 13.3 (2.98) | 14.39 (3.77) | 13.82 (3.94) | 13.37 (3.02) |
| CBT/IEP | 18.93 (3.42) | 13.76 (4.30) | 13.31 (3.06) | 13.30 (3.23) | 13.13 (3.74) |
| Response to Relaxation and Arousal Questionnaire | |||||
| CBT-SL | 31.44 (5.79) | 20.87 (6.41) | 22.15 (6.32) | 22.46 (6.26) | 20.95 (6.83) |
| CBT/IEP | 27.42 (6.56) | 20.74 (6.93) | 20.56 (6.73) | 20.85 (7.60) | 19.19 (7.71) |
| Hamilton Depression Scale | |||||
| CBT-SL | 17.05 (6.23) | 8.44 (7.56) | 7.85 (6.92) | 8.63 (6.66) | 9.09 (8.21) |
| CBT/IEP | 17.30 (7.93) | 6.91 (5.09) | 7.42 (5.75) | 8.59 (6.56) | 7.69 (8.46) |
| Inventory of Interpersonal Problems Total Score | |||||
| CBT-SL | 101.16 (32.99) | 74.93 (36.26) | 83.26 (38.76) | 78.18 (44.08) | 74.80 (36.47) |
| CBT/IEP | 89.85 (35.51) | 73.22 (42.84) | 66.72 (39.15) | 65.61 (36.60) | 59.03 (33.32) |
Note. CBT = cognitive-behavioral therapy; SL = supportive listening; IEP = interpersonal and emotional processing therapy.
Clinically significant change analyses at 2-year follow-up showed that of those receiving CBT + I/EP, 68.8%, 71.9%, 75%, and 83.9% respectively, achieved high endstate functioning, responder status, did not meet GAD criteria, and achieved high endstate functioning on the IIP-C. Of those receiving CBT + SL, 52.9%, 64.7%, 63.6%, and 66.7%, respectively, achieved high endstate functioning on GAD symptoms, responder status, no longer met criteria for GAD, and achieved high endstate functioning on the IIP-C. None of these percentages differed significantly by condition based on chi-square analyses (see Table 3).
Table 3.
Endstate Functioning and Responder Status
| Endstate Functioning based on 3 of 5 measures of GAD | χ2 value | p | d | Responder Status based on 3 of 5 measures of GAD | χ2 value | p | d | |||
|---|---|---|---|---|---|---|---|---|---|---|
| CBT+I/EP | CBT+SL | CBT+I/EP | CBT+SL | |||||||
| Post- | 64.7% (22/34) | 58.3% (21/36) | 0.30 | .58 | 0.13 | 73.5% (25/34) | 69.4% (25/36) | 0.14 | .71 | 0.09 |
| 6-month | 63.6% (21/33) | 41.2% (14/34) | 3.42 | .07 | 0.46 | 81.8% (27/33) | 52.9% (18/34) | 6.51 | .01 | 0.66 |
| 12-month | 55.9% (19/34) | 59.4% (19/32) | 0.08 | .77 | 0.07 | 79.4% (27/34) | 62.5% (20/32) | 2.32 | .13 | 0.38 |
| 24-month | 68.8% (22/32) | 52.9% (18/34) | 1.74 | .19 | 0.33 | 71.9% (23/32) | 64.7% (22/34) | 0.39 | .53 | 0.15 |
|
| ||||||||||
| Endstate Functioning on at least 6 of 8 IIP-C subscales | χ2 value | p | d | Does not meet GAD criteria | χ2 value | p | d | |||
|
| ||||||||||
| CBT+I/EP | CBT+SL | CBT+I/EP | CBT+SL | |||||||
|
| ||||||||||
| Post-treatment | 70.6% (24/34) | 60% (21/35) | 0.86 | 0.36 | 0.22 | 73.5% (25/34) | 55.6% (20/36) | 2.48 | .12 | 0.38 |
| 6-month | 75% (24/32) | 54.8% (17/31) | 2.84 | 0.09 | 0.43 | 72.7% (24/33) | 63.6% (21/33) | 0.63 | .43 | 0.20 |
| 12-month | 75.8% (25/33) | 57.1% (16/28) | 2.39 | 0.12 | 0.40 | 79.4% (27/34) | 65.6% (21/32) | 1.59 | 0.21 | 0.31 |
| 24-month | 83.9% (26/31) | 66.7% (20/30) | 2.47 | 0.12 | 0.41 | 75% (24/32) | 63.6% (21/33) | 0.99 | 0.32 | 0.27 |
Note. CBT = cognitive-behavioral therapy; SL = supportive listening; IEP = interpersonal and emotional processing therapy.
Effect of Treatment on Depressive Symptomatology
For depressive symptomatology (HRSD), there was significant random variation at the intercept and across Piece 1. There was no meaningful within-individual (or random) variation in rate of change over the follow-up period. Following the second step, only the main effect for Piece 1 was significant (ß = −.28, SE = .04), t(77) = −6.77, p < .0001, 95% CI = [−.36, −.20], d = 1.05, showing a decrease in depressive symptoms from pre-to posttreatment, irrespective of condition. Main effects for Piece 2 (ß = .005, SE = .006), t(77) = 0.76, p = .45, 95% CI = [−.007, .02], d = 0.12, condition, (ß = .03, SE = .20), t(77) = 0.16, p = .87, 95% CI = [−.35, .41], d = 0.02; Piece 1 × Condition, (ß = −.03, SE = .06), t(77) = −0.55, p = .58, 95% CI = [−.15, .08], d = 0.08, and Piece 2 × Condition, (ß < −.001, SE = .009), t(77) = −0.005, p > .99, 95% CI = [−.02, .02], d < 0.001, were nonsignificant. Therapeutic gains were maintained in both groups across the 2-year follow-up period.
Effect of Treatment on Interpersonal Distress
On the IIP-C, there were significant random effects for intercept and Piece 1, which were retained within the model. There was no meaningful within-individual variation in rate of change over the follow-up period. Following the second step, only the main effect for Piece 1 was significant (ß = −.20, SE = .06), t(77) = −3.20, p = .002, 95% CI = [−.32, −.08], d = 0.50, demonstrating a decrease in interpersonal distress from pre-to posttreatment, irrespective of condition. Effects for Piece 2 (ß = .005, SE = .010), t(77) = 0.53, p = .60, 95% CI = [−.01, .02], d = 0.08, condition ( ß = −.33, SE = .19), t(77) = −1.70, p = .09, 95% CI = [−.71, .05], d = 0.26,; Piece 1 × Condition ( ß = .04, SE = .04), t(77) = 0.96, p = .34, 95% CI = [−.04, .12], d = 0.15; and Piece 2 × Condition (ß = −.008, SE = .006), t(77) = −1.27, p = .21, 95% CI = [−.02, .004], d = 0.20, were all nonsignificant. Nonsignificant Piece 2 effects showed maintained gains over the 2-year follow-up.
Additional Treatment
At each follow-up interview, clients were asked to list all medications they had taken and/or psychotherapy that had occurred since the previous assessment period. The rate of subsequent psychotherapy was very low at the 6-and 12-month assessments (5.4% and 6.6%, respectively) but increased to 14% by 24 months, but not significantly so as indicated by McNemar’s (1947) change test. We used zero-inflated negative binomial (ZINB) regression models to assess differential seeking of subsequent treatment by condition. ZINB analyses model separate predictors for the source of excess zeros and the independent variable, in which the latter resembles a standard logistic regression. There were no significant differences in subsequent psychotherapy between treatment conditions at any assessment. Of 24 completers on psychotropic medications at pretreatment, 12 (50%), 10 (41.7%), and 11 (45.8%), respectively, were no longer on psychotropic medications at 6- 12- and 24-month assessment with no significant differences between treatments at any assessment. Of 45 clients not on medications at pretreatment, five (11%), five (11%), and six (13.3%), respectively, sought psychotropic medications during 6- 12- and 24-month assessments. At 6- and 12-month assessments, the number of individuals who sought psychotropic medication varied by psychotherapy condition (ß = 13.81, SE = .44), t(54) = 31.50, p < .0001, 95% CI = [12.93, 14.67], d = 4.88 (ß = 13.79, SE = .44); t(59) = 31.25, p < .0001, 95% CI = [12.93, 14.65], d = 4.84, respectively, as all five participants at both time points were in the CBT + SL condition. However, the treatments were no longer significantly different from one another at 24-month assessment (CBT + I/EP = 2; CBT + SL = 4; ß = .80, SE = 1.68), t(55) = 0.48, p = .63, 95% CI = [-2.48, 4.08], d = 0.07.
Discussion
The goal of this study was to test whether the addition of techniques aimed at fostering emotional deepening and improving interpersonal functioning would increase the long-term effect of CBT for GAD. We predicted that CBT + I/EP would lead to better GAD outcomes, particularly at long-term follow-up, than would CBT + SL. Our rationale for predicting effects to be strongest at long-term follow-up was based on our belief that any incremental change coming from the I/EP portion of therapy would occur more slowly because this therapy targets aspects of functioning that are more entrenched in nature. Both treatments led to significant improvement from pre- to posttreatment, as well as maintenance of therapeutic gains from post- to 2-year follow-up. Within-treatment effect sizes were very large for both treatments as well, showing pre- to 2-year follow-up for the HARS of d = 1.51 for CBT + SL and d = 1.9 for CBT + IEP. Both treatments also showed large percentages of participants no longer meeting criteria for GAD symptoms at 2-year follow-up (75% for CBT + IEP and 63.6% for CBT + SL). However, combined CBT + IEP was not significantly superior to CBT + SL on any dependent variable.
A possible explanation for our failure to find differences is that the non-CBT techniques chosen to address emotional and interpersonal deficits in GAD were not sufficient or adequate to abate our clients’ deficits. As such, it is conceivable that including techniques we had not considered adding to the traditional CBT protocol and/or integrating CBT and non-CBT techniques in a more seamless manner (rather than dividing them into separate segments) might have better augmented the impact of CBT.4 However, it is important to note that despite what may seem to be an unnatural division in the way that we conducted psychotherapy, our informal observation of all videotapes of all sessions showed that this division was not experienced as problematic for either clients or therapists. In line with this assertion is that our drop-out rate is comparable to or lower than what has been reported in other studies of treatment for GAD that did not use additive designs (e.g., Barlow, Rapee, & Brown, 1992; Roemer et al., 2008).
It is possible that the techniques added in our combined protocol did have an impact but that their effect was not superior to the supportive interventions that were added to the CBT protocol in order to control for common factors. In line with this interpretation is that our two treatment conditions did not differ in expectancies and credibility (two common factors that have been linked with outcome in treatment of GAD) (Borkovec & Costello, 1993; Newman & Fisher, 2010). Also in line with this interpretation, whereas the present trial showed no deterioration of treatment gains across follow-up, an analysis of data from our most recent CBT trial showed deterioration at 2-year follow-up on a similar composite measure of GAD symptoms (Newman, Przeworski, Fisher, & Borkovec, 2010). It is important to note, however, that with the exception of only one score (endstate functioning for GAD symptoms at 12-month follow-up), all clinically significant change percentages favored CBT + IEP, and some of these percentages showed medium effect sizes. Thus, it is possible that the combined treatment did have a greater impact than the control condition but that the relatively small sample size (despite our power analysis) did not allow for the difference to reach statistical significance.
The combined treatment also may be superior only for some types of clients with GAD. CBT is a potent intervention with significant short- and long-term impacts on a substantial percentage of clients with GAD. As such, the addition of interpersonal and/or experiential interventions might be more beneficial for some individuals, for instance, those who show enough of particular types of interpersonal problems to interfere with their lives, and yet not too severe to be immune to change within a relatively short-term intervention. For clients without significant interpersonal problems, however, the addition of the same interventions might have been at best irrelevant, a possible waste of time and energy, or even a potential detraction from the benefits of the CBT (internally focused and coping oriented) segments they received before every segment of I/EP. Moreover, the exploration of emotional experience may be beneficial only for some clients. These speculations suggest that the addition of I/EP to the CBT protocol may be needed or effective for some clients, while being either no more effective than (or actually inferior to the addition of SL) for others. Future studies with the present data set are planned to investigate such aptitude by treatment interactions. Also planned are process studies to understand how change may or may not have taken place. Whereas adherence and competence ratings suggest that the therapy segments were implemented with a high level of fidelity and satisfactory competence, it is unclear whether the interventions impacted the mechanisms of change that they were aimed at fostering. To use a drug metaphor, although the treatments were adequately delivered, it is unclear whether or not clients absorbed them, and whether or not such absorption was associated with change. As an example, future data analyses will investigate whether the levels of different types of emotion were higher in I/EP than in both CBT and SL, and whether such emotional experience was related to outcome. Such studies may provide clues as to why the combined treatment, as presently designed and implemented, was not superior to CBT on most measures, and may point to modifications of traditional and integrative treatment that can lead to better outcome.
Several limitations of this study should be noted. First, most clients were recruited via advertisements and thus might not have sought treatment on their own. Also, study participants were mostly White, and a significant majority of the sample had some college education or higher. These factors may limit the generalizability of our findings. In addition, because the second interviewer only interviewed clients when and if the first interviewer decided they had met all study criteria, our estimates of interrater agreement for the presence of GAD are likely inflated. We also failed to calculate the reliability of our adherence raters, and therefore we cannot speak to the possibility of observer drift. Moreover, we used an additive design in the present study. Although this design enhances internal validity, it diminishes the external validity of our treatment, as practitioners may be less likely to use this therapy in the way that we have done. We also did not include an outcome measure that assessed avoidance of emotion. Because the avoidance of emotional processing was specifically targeted by I/EP, one might have predicted that the experimental condition would have led to greater reduction of emotional avoidance. The support (or lack thereof) for this prediction might have shed light on the absence of significant differences in primary outcome measures.
Acknowledgments
We would like to thank Dr. Jeremy Safran for providing quality ratings for both treatments included in this study. This research was supported in part by National Institute of Mental Health Research Grant RO1 MH58593-02.
Footnotes
We included participants who met criteria for a current principal diagnosis of GAD even when GAD symptoms occurred solely during a depressive episode as long as participants indicated that the GAD symptoms caused them more severe distress than did depressive symptoms. This decision was based on data that the DSM hierarchical rules artificially limit comorbidity (Brown, Campbell, Lehman, Grisham, & Mancill, 2001)
Table of results of this analysis is available from Michelle G. Newman upon request.
Data were also analyzed using missing data replacement with multiple imputed data with maximum likelihood imputation procedures. Findings were the same as the results with missingness intact.
At the conclusion of our study, Rezvan, Baghban, Bahrami, and Abedi (2008) began a partial conceptual replication comparing CBT and CBT plus interpersonal therapy (IPT) for GAD in an undergraduate sample. Although their therapy elements were not identical to ours (including an absence of emotional processing therapy), their sample size was relatively small, and they did not include adherence or quality checks, they did find that a fully integrated version of CBT + IPT was significantly superior to CBT alone on their two main outcome measures (the PSWQ and Oxford Happiness Inventory; Argyle, Martin, & Crossland, 1989) at their 1-year follow-up assessment.
Trial Registry name: Clinical Trials.gov, Identifier: NCT00951652
References
- Alden LE, Wiggins JS, Pincus AL. Construction of circumplex scales for the Inventory of Interpersonal Problems. Journal of Personality Assessment. 1990;55:521–536. doi: 10.1207/s15327752jpa5503&4_10. [DOI] [PubMed] [Google Scholar]
- American Psychiatric Association. Diagnostic and statistical manual of mental disorders. 1. Washington, DC: American Psychiatric Association; 1952. [Google Scholar]
- Barlow DH, Rapee RM, Brown TA. Behavioral treatment of generalized anxiety disorder. Behavior Therapy. 1992;23:551–570. doi: 10.1016/S0005-7894(05)80221-7. [DOI] [Google Scholar]
- Bieling PJ, Antony MM, Swinson RP. The Stait-Trait Anxiety Inventory, Trait version: Structure and content re-examined. Behaviour Research and Therapy. 1998;36(7-8):777–788. doi: 10.1016/s0005-7967(98)00023-0. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Hu S. The effect of worry on cardiovascular response to phobic imagery. Behaviour Research and Therapy. 1990;28:69–73. doi: 10.1016/0005-7967(90)90056-O. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Costello E. Efficacy of applied relaxation and cognitive-behavioral therapy in the treatment of generalized anxiety disorder. Journal of Consulting and Clinical Psychology. 1993;61:611–619. doi: 10.1037/0022-006X.61.4.611. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Roemer L. Perceived functions of worry among generalized anxiety disorder subjects: Distraction from more emotionally distressing topics? Journal of Behavior Therapy and Experimental Psychiatry. 1995;26:25–30. doi: 10.1016/0005-7916(94)00064-s. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Ruscio AM. Psychotherapy for generalized anxiety disorder. Journal of Clinical Psychiatry. 2001;62(Suppl. 11):37–45. [PubMed] [Google Scholar]
- Borkovec TD, Newman MG, Pincus AL, Lytle R. A component analysis of cognitive-behavioral therapy for generalized anxiety disorder and the role of interpersonal problems. Journal of Consulting and Clinical Psychology. 2002;70:288–298. doi: 10.1037/0022-006X.70.2.288. [DOI] [PubMed] [Google Scholar]
- Borkovec TD, Alcaine O, Behar ES. Avoidance theory of worry and generalized anxiety disorder. In: Heimberg R, Mennin D, Turk C, editors. Generalized anxiety disorder: Advances in research and practice. New York: Guilford; 2004. pp. 77–108. [Google Scholar]
- Brown TA, Di Nardo PA, Barlow DH. Anxiety Disorders Interview Schedule for DSM-IV. New York: Oxford University Press; 1994. [Google Scholar]
- Brown TA, Campbell LA, Lehman CL, Grisham JR, Mancill RB. Current and lifetime comorbidity of the DSM-IV anxiety and mood disorders in a large clinical sample. Journal of Abnormal Psychology. 2001;110:585–599. doi: 10.1037//0021-843X.110.4.585. [DOI] [PubMed] [Google Scholar]
- Brown TA, Di Nardo PA, Lehman CL, Campbell LA. Reliability of DSM-IV anxiety and mood disorders: Implications for the classification of emotional disorders. Journal of Abnormal Psychology. 2001;110:49–58. doi: 10.1037//0021-843X.110.1.49. [DOI] [PubMed] [Google Scholar]
- Bruss GS, Gruenberg AM, Goldstein RD, Barber JP. Hamilton Anxiety Rating Scale Interview Guide: Joint interview and test-retest methods for interrater reliability. Psychiatry Research. 1994;53:191–202. doi: 10.1016/0165-1781(94)90110-4. [DOI] [PubMed] [Google Scholar]
- Cassidy J, Lichtenstein-Phelps J, Sibrava NJ, Thomas CL, Borkovec TD. Generalized anxiety disorder: Connections with self-reported attachment. Behavior Therapy. 2009;40:23–38. doi: 10.1016/j.beth.2007.12.004. [DOI] [PubMed] [Google Scholar]
- Castonguay LG, Goldfried MR, Wiser S, Raue PJ, Hayes AM. Predicting the effect of cognitive therapy for depression: A study of unique and common factors. Journal of Consulting and Clinical Psychology. 1996;64:497–504. doi: 10.1037//0022-006X.64.3.497. [DOI] [PubMed] [Google Scholar]
- Chambless DL, Ollendick TH. Empirically supported psychological interventions: Controversies and evidence. Annual Review of Psychology. 2001;52:685–716. doi: 10.1146/annurev.psych.52.1.685. [DOI] [PubMed] [Google Scholar]
- Devilly GJ, Borkovec TD. Psychometric properties of the credibility/expectancy questionnaire. Journal of Behavior Therapy and Experimental Psychiatry. 2000;31:73–86. doi: 10.1016/S0005-7916(00)00012-4. [DOI] [PubMed] [Google Scholar]
- Dunlap WP, Cortina JM, Vaslow JB, Burke MJ. Meta-analysis of experiments with matched groups or repeated measures designs. Psychological Methods. 1996;1:170–177. doi: 10.1037/1082-989x.1.2.170. [DOI] [Google Scholar]
- Erickson TM, Newman MG. Interpersonal and emotional processes in generalized anxiety disorder analogues during social interaction tasks. Behavior Therapy. 2007;38:364–377. doi: 10.1016/j.beth.2006.10.005. [DOI] [PubMed] [Google Scholar]
- First MB, Gibbon M, Spitzer RL, Williams JBW, Benjamin LS. Structured Clinical Interview for DSM-IV Axis II Personality Disorders. Washington: American Psychiatric Press; 1997. [Google Scholar]
- Gallop R, Tasca GA. Multilevel modeling of longitudinal data for psychotherapy researchers: II: The complexities. Psychotherapy Research. 2009;19:438–452. doi: 10.1080/10503300902849475. [DOI] [PubMed] [Google Scholar]
- Greenberg LS. Emotion-focused therapy: Coaching clients to work through their feelings. Washington, DC: American Psychological Association; 2002. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. British Journal of Medical Psychology. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hamilton M. A rating scale for depression. Journal of Neurology, Neurosurgery and Psychiatry. 1960;23:56–61. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heide FJ, Borkovec TD. Relaxation-induced anxiety: Paradoxical anxiety enhancement due to relaxation training. Journal of Consulting and Clinical Psychology. 1983;51:171–182. doi: 10.1037/0022-006X.51.2.171. [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Rosenberg SE, Baer BA, Ureno G, Vilasenor VS. Inventory of interpersonal problems: Psychometric properties and clinical applications. Journal of Consulting and Clinical Psychology. 1988;56:885–892. doi: 10.1037//0022-006X.56.6.885. [DOI] [PubMed] [Google Scholar]
- Llera SJ, Newman MG. Effects of worry on physiological and subjective reactivity to emotional stimuli in generalized anxiety disorder and nonanxious control participants. Emotion. 2010;10(5):640–650. doi: 10.1037/a0019351. [DOI] [PubMed] [Google Scholar]
- Maffei C, Fossati A, Agostoni I, Barraco A, Bagnato M, Deborah D, Petrachi M. Interrater reliability and internal consistency of the Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II), version 2.0. Journal of Personality Disorders. 1997;11:279–284. doi: 10.1521/pedi.1997.11.3.279. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Heimberg RG, Turk CL, Fresco DM. Preliminary evidence for an emotion dysregulation model of generalized anxiety disorder. Behaviour Research and Therapy. 2005;43:1281–1310. doi: 10.1016/j.brat.2004.08.008. [DOI] [PubMed] [Google Scholar]
- Mennin DS, Holaway RM, Fresco DM, Moore MT, Heimberg RG. Delineating components of emotion and its dysregulation in anxiety and mood psychopathology. Behavior Therapy. 2007;38:284–302. doi: 10.1016/j.beth.2006.09.001. [DOI] [PubMed] [Google Scholar]
- Meyer TJ, Miller ML, Metzger RL, Borkovec TD. Development and validation of the Penn State Worry Questionnaire. Behaviour Research and Therapy. 1990;28:487–495. doi: 10.1016/0005-7967(90)90135-6. [DOI] [PubMed] [Google Scholar]
- Mogg K, Millar N, Bradley BP. Biases in eye movements to threatening facial expressions in generalized anxiety disorder and depressive disorder. Journal of Abnormal Psychology. 2000;109:695–704. doi: 10.1037//0021-843X.109.4.695. [DOI] [PubMed] [Google Scholar]
- Molina S, Borkovec TD. The Penn State Worry Questionnaire: Psychometric properties and associated characteristics. In: Davey GCL, Tallis F, editors. Worrying: Perspectives on theory, assessment and treatment. Oxford, England: Wiley; 1994. pp. 265–283. [Google Scholar]
- Moras K, di Nardo PA, Barlow DH. Distinguishing anxiety and depression: Reexamination of the reconstructed Hamilton scales. Psychological Assessment. 1992;4:224–227. doi: 10.1037/1040-3590.4.2.224. [DOI] [Google Scholar]
- Neter J, Wasserman W, Kutner MH. Applied linear statistical models. 3. Homewood, IL: Richard D. Irwin, Inc; 1990. [Google Scholar]
- Newman MG, Borkovec TD. Cognitive behavioral therapy for worry and generalized anxiety disorder. In: Simos G, editor. Cognitive behaviour therapy: A guide for the practising clinician. New York: Taylor & Francis; 2002. pp. 150–172. [Google Scholar]
- Newman MG, Zuellig AR, Kachin KE, Constantino MJ, Przeworski A, Erickson T, Cashman-McGrath L. Preliminary reliability and validity of the Generalized Anxiety Disorder Questionnaire-IV: A revised self-report diagnostic measure of generalized anxiety disorder. Behavior Therapy. 2002;33:215–233. doi: 10.1016/S0005-7894(02)80026-0. [DOI] [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Molnar C. Integrative psychotherapy. In: Heimberg RG, Turk CL, Mennin DS, editors. Generalized anxiety disorder: Advances in research and practice. New York, NY: Guilford Press; 2004. pp. 320–350. [Google Scholar]
- Newman MG, Castonguay LG, Borkovec TD, Fisher AJ, Nordberg SS. An open trial of integrative therapy for generalized anxiety disorder. Psychotherapy: Theory, Research, Practice, Training. 2008;45:135–147. doi: 10.1037/0033-3204.45.2.135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Erickson TM. Generalized anxiety disorder. In: Beck JG, editor. Interpersonal processes in the anxiety disorders: Implications for understanding psychopathology and treatment. Washington, DC: American Psychological Association; 2010. pp. 235–259. [Google Scholar]
- Newman MG, Fisher AJ. Expectancy/Credibility change as a mediator of cognitive behavioral therapy for generalized anxiety disorder: Mechanism of action or proxy for symptom change? International Journal of Cognitive Therapy. 2010;3:245–261. doi: 10.1521/ijct.2010.3.3.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newman MG, Przeworski A, Fisher AJ, Borkovec TD. Diagnostic comorbidity in adults with generalized anxiety disorder: impact of comorbidity on psychotherapy outcome and impact of psychotherapy on comorbid diagnoses. Behavior Therapy. 2010;41:59–72. doi: 10.1016/j.beth.2008.12.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Przeworski A, Newman MG, Pincus AL, Kasoff MB, Yamasaki AS, Castonguay LG, Berlin KS. Interpersonal pathoplasticity in individuals with generalized anxiety disorder. Journal of Abnormal Psychology. doi: 10.1037/a0023334. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rezvan S, Baghban I, Bahrami F, Abedi M. A comparison of cognitive-behavior therapy with interpersonal and cognitive behavior therapy in the treatment of generalized anxiety disorder. Counselling Psychology Quarterly. 2008;21:309–321. [Google Scholar]
- Roemer L, Orsillo SM, Salters-Pedneault K. Efficacy of an acceptance-based behavior therapy for generalized anxiety disorder: evaluation in a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2008;76:1083–1089. doi: 10.1037/a0012720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Safran JD, Segal ZV. Interpersonal process in cognitive therapy. New York: Basic Books; 1990. [Google Scholar]
- Salzer S, Pincus AL, Hoyer J, Kreische R, Leichsenring F, Leibing E. Interpersonal subtypes within generalized anxiety disorder. Journal of Personality Assessment. 2008;90:292–299. doi: 10.1080/00223890701885076. [DOI] [PubMed] [Google Scholar]
- Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory STAI (Form Y) Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- Westen D, Morrison K. A multidimensional meta-analysis of treatments for depression, panic, and generalized anxiety disorder: An empirical examination of the status of empirically supported therapies. Journal of Consulting and Clinical Psychology. 2001;69:875–899. doi: 10.1037//0022-006X.69.6.875. [DOI] [PubMed] [Google Scholar]
- Whitehurst GJ. Interrater agreement for journal manuscript reviews. American Psychologist. 1984;39:22–28. doi: 10.1037/0003-066x.39.1.22. [DOI] [Google Scholar]
- Young JE, Beck AT. The development of the Cognitive Therapy Scale. Philadelphia, PA: Center for Cognitive Therapy; 1980. [Google Scholar]