Abstract
Background
Identifying how genetic risk interacts with experience to predict psychopathology is an important step toward understanding the etiology of mental health problems. Few studies have examined genetic risk by experience interaction (GxE) in the development of childhood psychopathology.
Methods
We used both co-twin and parent mental health as markers of genetic risk to test whether GxE predicted internalizing problems in a sample of 8-year-old twins. Multi-instrument composites were used to characterize both parent and child psychopathology, and five experiential risk factors (socioeconomic status, single parent upbringing, negative parent-child interactions, number of negative life events, negative impact of negative life events) composed a cumulative risk index.
Results
We found consistent evidence for GxE for child internalizing problems, with significant interaction effects emerging both when genetic risk was indexed by co-twin mental health and when it was based on parent mental health. When co-twin mental health was used to estimate genetic risk, child internalizing problems were more heritable for children at low rather than high experiential risk. When parent mental health was used to estimate genetic risk, the association between genetic risk and internalizing problems was stronger for children at elevated experiential risk. Consideration of the interaction effect sizes helps to reconcile these findings.
Conclusions
Our results suggest that the processes involved in both diathesis-stress and bioecological models of development may operate for child internalizing problems. Effect sizes indicated that the main effects of genetic and experiential risk were much better predictors of child internalizing problems than was their interaction.
Keywords: gene-environment interaction, childhood psychopathology, internalizing problems, parental psychopathology, twins
Depression has been designated as the top cause of disability in the world (World Health Organization, 2001). Given that childhood internalizing problems often precede the onset of depression in adolescence and adulthood (Costello, Foley, & Angold, 2006), understanding the etiology of child internalizing problems has become a top priority (Costello et al., 2002). Heritability estimates ranging from 23–62% (Rice & Thapar, 2009) indicate that both genetic and experiential factors play important roles in child internalizing problems. Both historically (Erlenmeyer-Kimling, 1972) and more recently (Rutter, Moffitt, & Caspi, 2006), scientists have promoted the notion of genetic risk by experience interaction (GxE) as an approach to understanding the etiology of complex psychological patterns, such as childhood internalizing problems. In very basic terms, the GxE approach suggests that the influence of genes on behavior may differ depending on the types of experiences to which the individual has been exposed. Conversely, GxE also indicates that the influence of experience on behavior may differ depending on the genotype of the individual.
As attractive as the idea of GxE is for non-deterministic views of etiology, the paradigm comes bundled with conceptual and statistical difficulties. On the genetic side, it is currently impossible to quantify the full genetic effect in a specific way. We know the identity of only a few genes associated with any given complex human phenotype and thus can only test for interaction of a fraction of the “genotypic risk” with experience. Results using these already-identified genes (the “low-hanging fruit”) may prove non-representative. If willing to sacrifice the specificity that measured genes provide, we can adopt the traditional practice of genetic epidemiology and infer genotypic risk from the phenotypes of genetic relatives. However, this genetic risk assessment is indirect and imprecise. On the environmental side, the chief difficulty lies in conceptualizing risk factors that are fully independent of genetic influence, since many risk factors traditionally thought to be experiential (e.g., socioeconomic status) are heritable to some degree (Plomin & Bergeman, 1991). Given this, genotype by environment correlations and interactions might be as ubiquitous in the construction of human psychological environments as they are thought to be in the development of human psychological phenotypes.
From a strictly statistical perspective, at least three classes of problems plague the field. First is the possibility of selective reporting of positive findings, a problem that looms large with the recent feasibility of testing thousands of genes. In the present study, we emphasize interactions that provide converging evidence across two methods. Second is the well-known scaling problem: observed ordinal interactions can often be eliminated by scale transformations (Cohen, Cohen, West, & Aiken, 2003). The scaling problem is difficult to negotiate when interactions are ordinal, as they are in the present study and in the great majority of prior reports. However, our use of a multi-source outcome composite should at least preclude idiosyncratic scaling properties of any single instrument. Third, and more tentatively, some GxE reported in the literature could represent statistical artifacts rather than describe developmental phenomena (Eaves, 2006). However, Eaves' (2006) cautions apply to measured risk alleles and dichotomous outcomes analyzed with logistic regression, conditions that do not apply to the present study. Previewing our own approach to demonstrating GxE for internalizing problems, we take into account both children's gender and co-occurrence of externalizing symptoms, focus on detailed measurement of the environment and of symptoms, and rely on converging results across methods to provide more convincing evidence of GxE than is typically found in the literature.
Co-twin Mental Health as G-risk
Co-twin psychopathology is an indirect estimate of genetic risk (G-risk). Kendler et al. (1995) first developed a categorical approach to estimating G-risk for a study of GxE in adult depression. G-risk groups were based jointly on zygosity and the mental health status of co-twins. Because monozygotic (MZ) twins share 100% of their genes while dizygotic (DZ) twins share only 50% of their segregating genes on average, the MZ co-twin of an individual with psychiatric problems (“affected”) is at higher G-risk for developing similar problems than the DZ co-twin of an affected individual. Extending this logic, a DZ co-twin of a child without elevated levels of psychiatric problems (unaffected) is at lower G-risk whereas the MZ co-twin of an unaffected child is at the lowest G-risk of all. Using this 4-point ordinal index of G-risk, Kendler et al. (1995) examined whether G (co-twin's lifetime history of major depression) × E (presence/absence of a stressful life event) predicted depression in females. Life events were more strongly associated with depression among women at elevated G-risk. Jaffee et al. (2005) obtained a similar interaction using this approach, finding that maltreatment was more strongly associated with conduct disorder among children at elevated G-risk. Note that although we provide a description of the method developed by Kendler et al. (1995) for historical reference, we do not utilize this specific approach in the current study.
Other studies have used differences in heritability across environments to test for GxE. This approach allows for co-twin psychopathology to be represented as a continuous variable. The heritability of a trait can be estimated by comparing the similarity of MZ co-twins to the similarity of DZ co-twins (Jinks & Fulker, 1970). The first method used in the current study involves testing whether the heritability of a trait differs depending on the level of experiential risk (E-risk). Studies using co-twin mental health as G-risk to test for GxE in the development of childhood psychopathology have yielded mixed results (see Table 1 for selected studies). In one study similar to our own, Lau, Gregory, Goldwin, Pine, and Eley (2007) found that the heritability of child separation anxiety symptoms was higher for children at elevated E-risk (increased negative life events) in comparison to their low E-risk counterparts. Some studies of externalizing problems and antisocial behavior among children and adolescents have yielded interactions in the opposite direction. These studies provide evidence that, in some cases, the heritability of psychopathology may decrease as E-risk increases (Button, Lau, Maughan, & Eley, 2008; Button, Scourfield, Martin, Purcell, & McGuffin, 2005; Tuvblad, Grann, & Lichtenstein, 2006).
Table 1.
Selected Studies of Heritability by Measured E-risk Interaction in Child and Adolescent Psychopathology.
| Publication/Study | Mean Age | Measured E-risk | Outcome | Direction of Interaction |
|---|---|---|---|---|
| Lau et al., 2007 | ||||
| ECHO, U.K. | 8 years, 6 months | Negative Life Events | Separation Anxiety Symptoms | higher h2 as E-risk increases |
| G1219,U.K. | 15 years | Negative Life Events | Panic Anxiety Symptoms | higher h2 as E-risk increases |
|
| ||||
| Button et al., 2008 | Maternal Putative Discipline | Externalizing Problems | lower h2 as E-risk increases | |
| G1219,U.K. | 15 years | Paternal Putative Discipline | Externalizing Problems | higher h2 as E-risk increases |
|
| ||||
| Lau et al., 2008 | Maternal Putative Discipline | Depression Symptoms | higher h2 as E-risk increases | |
| G1219,U.K. | 15 years | Negative Life Events | Depression Symptoms | higher h2 as E-risk increases |
|
| ||||
| Rice et al., 2006 | ||||
| CaStANET, U.K. | 11.2 years | Family Conflict | Depression Symptoms | higher h2 as E-risk increases |
|
| ||||
| Button et al., 2005 | ||||
| CaStA-NET, U.K. | 10.6 years | Family Dysfunction | Antisocial Behavior | lower h2 as E-risk increases |
|
| ||||
| Tuvblad et al., 2006 | ||||
| TCHAD, Sweden | 16–17 years* | Socioeconomic Status | Antisocial Behavior | lower h2 as E-risk increases |
|
| ||||
| Silberg et al., 2001 | Negative Life Events | Depression Symptoms | higher h2 as E-risk increases | |
| VTSABD, U.S.A. | 14–17 years* | Negative Life Events | Anxiety Symptoms | higher h2 as E-risk increases |
|
| ||||
| Miles et al., 2005 | ||||
| VTSABD, U.S.A. | 14.55 years | Parental Closeness | Alcohol Use | higher h2 as E-risk increases |
|
| ||||
| Harden et al., 2008 | ||||
| AddHealth, U.S.A. | 16.1 years | Best Friend Alcohol/Tobacco Use | Alcohol/Tobacco Use | higher h2 as E-risk increases |
|
| ||||
| Antisocial Peer Affiliations | Internalizing Problems | lower h2 as E-risk increases | ||
| Lack of Prosocial Peer Affiliations | Internalizing Problems | lower h2 as E-risk increases | ||
| Hicks et al., 2009a | 17.8 years | Mother-Child Relationship Problems | Internalizing Problems | lower h2 as E-risk increases |
| MTFS, U.S.A. | Father-Child Relationship Problems | Internalizing Problems | lower h2 as E-risk increases | |
| Academic Achievement & Engagement | Internalizing Problems | lower h2 as E-risk increases | ||
| Stressful Life Events | Internalizing Problems | lower h2 as E-risk increases | ||
|
| ||||
| Antisocial Peer Affiliations | Externalizing Problems | higher h2 as E-risk increases | ||
| Lack of Prosocial Peer Affiliations | Externalizing Problems | higher h2 as E-risk increases | ||
| Hicks et al., 2009b | 17.8 years | Mother-Child Relationship Problems | Externalizing Problems | higher h2 as E-risk increases |
| MTFS, U.S.A. | Father-Child Relationship Problems | Externalizing Problems | higher h2 as E-risk increases | |
| Academic Achievement & Engagement | Externalizing Problems | higher h2 as E-risk increases | ||
| Stressful Life Events | Externalizing Problems | higher h2 as E-risk increases | ||
Notes: ECHO = Emotions, Cognitions, Heredity and Outcome; a subsample of TEDS (Twins Early Development Study).
CaStA-NET = Cardiff Study of All Wales and North of England Twins
TCHAD = Twin study of Child and Adolescent Development
VTSABD = Virginia Twin Study of Adolescent Behavioral Development
AddHealth = National Longitudinal Study of Adolescent Health
MTFS = Minnesota Twin Family Study
h2 = heritability
The mean age of this sample was unavailable. Instead an age range was reported.
The studies presented are not comprehensive. We selected recent studies using child and adolescent samples that examined mental health phenotypes. Studies investigating dimensions of E-risk judged to be qualitatively different from our own (e.g. population density, religiosity) were excluded.
Parent Mental Health as G-risk
In the “parent mental health as G-risk” method, G-risk is based on the mental health status of an individual's parents. Hammen, Brennan, and Shih (2004) used parent mental health as G-risk to examine GxE for adolescent depression. They reported an interaction in which G-risk (maternal history of mood disorder) was a stronger predictor among offspring at elevated E-risk (low maternal marital satisfaction). Eley et al. (2004) observed a similar GxE in the prediction of adolescent depressive symptoms. Again, G-risk (based on parental and parental sibling's mental health) was more strongly associated with depressive symptoms among adolescents at high E-risk (low parental education). In contrast, one recent study provides evidence that parental psychopathology may be a better predictor of child behavior in families at low E-risk. Essex et al. (2006) found maternal history of depression to be a significant predictor of childhood psychopathology among low E-risk families (high socioeconomic status [SES]) but not among high E-risk families (low SES).
Although we used parental psychopathology, a heritable phenotype, as a proxy for G-risk in the current study, it is clear that parents with mental health problems are more likely to provide compromised rearing environments (Lovejoy, Graczyk, O'Hare, & Neuman, 2000). Given this tangle of genetic and environmental risk, the parent mental health as G-risk method's main function is to bolster confidence in GxE findings derived from methods using cleaner measures of G-risk (e.g., co-twin psychopathology). This pairing of methods is feasible in any twin study that includes measures of parental mental health.
Aims of the Current Study
The current study addresses three main questions: (1) Does G-risk based on co-twin psychopathology interact with E-risk to predict childhood internalizing problems? (2) Does G-risk based on parental psychopathology interact with E-risk to predict childhood internalizing problems? (3) Are the directions of these interactions consistent across methods?
Innovations of the Study
Studies of GxE typically estimate E-risk using a single indicator for each analysis (e.g., negative life events or SES). However, as the number of E-risk factors a child is exposed to accumulate, risk for psychopathology increases (Rutter, 1979). We accounted for the effects of cumulative adversity by creating an E-risk index from five individual risk factors. Similarly, characterization of parent and child psychopathology often depends on a single measure. We used multi-instrument composites to characterize psychopathology in both parents and children, which should minimize artifacts due to features of specific assessments. Further, we systematically identified twin families from birth records from an entire state before employing a screening process to enrich the sample for childhood psychiatric symptoms (see Lemery-Chalfant, Goldsmith, Schmidt, Arneson, & Van Hulle, 2006, for details). Using this epidemiologically characterized sample should enhance the generalizability of our results. Moreover, our study helps fill a gap in pre-adolescent literature on GxE for internalizing problems. Finally, judging from the limited number of published studies (see Table 1), it appears that the direction of GxE might differ for internalizing vs. externalizing problems. Given this possibility and given the well-established correlation between internalizing and externalizing problems, we have controlled for externalizing problems in our analyses. This procedure, not typically utilized in GxE studies, allows us to determine whether the interaction is impacted by covariation (or in some instances, comorbidity) of internalizing and externalizing problems.
METHODS
Participants and Procedure
The sample includes 431 twin pairs and their parents (83% of fathers) who participated in the Wisconsin Twin Project. Participants were recruited via telephone using contact information included in statewide birth records. Participants' informed consent was obtained following appropriate ethical guidelines. Children (50.9% female) had a mean age of 8.15 (SD = .96) years and 94.7% were White. We screened the sample to enrich it for childhood psychopathology. Mothers completed the MacArthur Health and Behavior Questionnaire (HBQ; Essex et al., 2002) for each twin. The HBQ yields scores of impulsivity, aggression, conduct disorder, oppositional defiant disorder, inattention, depression, separation anxiety, and overanxiousness. A population-based sample of 1,931 twin pairs was screened, and children were considered at least mildly at-risk for psychopathology if they scored 1.5 SD above the mean on at least one subscale. In addition to at-risk children, we also selected a low-risk control sample consisting of children whose scores were below the mean on all scales; this was not an extreme no-symptom group. All co-twins were also assessed. Together, the use of a non-symptomatic control sample and low-symptom co-twins of at-risk twins reduced the skewness that would have been apparent in an “at-risk only” sample and made normal distribution-based statistics appropriate for use with the study sample. The distribution characteristics for the three HBQ symptom scales used to select the study sample and also included in our overall internalizing problem composite score were similar for the study sample and the pre-screening sample (N = 3,862). Skewness statistics for the study vs. the unselected, pre-screening samples were 1.14 vs. 1 for overanxiousness, 1.6 vs. 1.94 for depression, and 1.29 vs. 1.27 for separation anxiety respectively. Skewness of the overall internalizing problem composite score described below was 1.72. Of the 862 participating children, 331 were considered at-risk for psychopathology based on screening data, 243 were low-risk controls, and 288 were non-grouped co-twins. Zygosity was determined using the 32-item Zygosity Questionnaire for Young Twins (Goldsmith, 1991). Agreement of this questionnaire with genotyping is estimated at 95–96% (Forget-Dubois et al., 2003; Price et al., 2000). When zygosity could not be determined from mother-report on this questionnaire, photographs and medical records regarding the placenta(e) were consulted and in some cases formal genotyping of DNA samples was performed. Zygosity remained uncertain for 4 twin pairs who were excluded from the co-twin mental health as G-risk analyses. Of the 427 twin pairs of known zygosity, 161 pairs were MZ, 151 pairs were same-sex DZ, and 115 pairs were opposite-sex DZ. Questionnaires and interviews were administered to parents over the telephone and during a 4 hour home visit, while children engaged in emotion-eliciting tasks, structured social interactions, and interviews.
Construction of the Experiential Risk (E-risk) Index
Five risk factors, empirically and theoretically linked to childhood internalizing problems, composed the E-risk index. Although some specificity could be lost by combining multiple E-risk factors into a single index, recent findings suggest that different types of stressors impact internalizing problems through a general mechanism (Hicks, DiRago, Iacono, & McGue, 2009). Thus, it was appropriate to combine E-risk factors in order to better estimate overall stress level.
Low Socioeconomic Status (SES)
SES was based on parental education and family income. Mothers had a mean of 14.55 years of formal education (SD = 2.19); fathers had a mean of 14.33 years (SD = 2.41). 3.6% of annual family incomes were between $0–$20,000, 5.6% between $20,001–$30,000, 27.1% between $30,001–$50,000, 26.2% between $50,001–$70,000, 22.2% between $70,001–$90,000, and 15.3% above $90,001. Family income and years of parental education were converted to z scores and averaged to create a composite score for SES; membership in the lowest quartile counted toward the risk index.
Marital status
Children in single-parent homes (10.6%) were considered positive for this risk factor.
Number of negative family life events
Past year life events were reported on the Life Experiences Survey (Sarason, Johnson, & Siegel, 1978). Nineteen events judged likely to impact children (e.g., change of residence, serious illness or injury of close family member) were selected for inclusion. Children were considered at-risk if their families experienced two or more events (20.7%). Care was taken to select life events judged less likely to be elicited by child behavior.
Mother's perceived negative impact of family life events
Mother ratings of the negative impact of 57 family life events were summed to create a negative impact score. This risk factor reflects the severity of life events, and the cut-off for risk was 1 SD below the mean (13.4%).
Observed maternal negativity
Two observers rated dimensions of parent-child interaction based on activities during the home visit. The four dimensions were connectedness (interest and involvement) between mother and children, anger and hostility in mother-child interactions, maternal intrusiveness, and mother's ability to read child cues and respond appropriately. Individual item ratings from the two observers were averaged, and then the mean of the four averaged ratings was used (α = .76 for the 8 items; i.e., 4 items each rated by 2 observers). The individual intraclass correlations derived for each of the four items were averaged to arrive at .43. This rather low correlation may be partially due to the fact that the two observers made ratings based on different but overlapping periods of observations. Because the two observers were often in different parts of the home during the visit, they each witnessed some mother-child interactions that the other observer did not (this point is also relevant to observer ratings of child internalizing problems discussed below). A more encouraging perspective on reliability is that the average raw agreement between raters, allowing for a discrepancy of only 1 interval to be counted as an agreement, was 89%. A child whose mother scored 1 SD above the mean on maternal negativity was considered positive for this risk factor (14.4%).
Following a conventional approach to constructing cumulative risk indices (Beck & Shaw, 2005; Rutter, 1979), children were assigned a score of 1 (risk factor present) or 0 (risk factor absent) for each E-risk factor, and individual scores were summed into an overall E-risk score. Then, we dichotomized E-risk scores to form high and low risk groups1. Children with scores of 1 or less were designated as low risk (73.8%) while children with scores greater than 1 were considered high risk (26.2%). We used this threshold because Rutter (1979) showed that two adversity factors are necessary to elevate risk. By dichotomizing the index to test for GxE we have accounted for the possibility that there is a threshold level of E-risk beyond which increasing E-risk has little effect on the portion of variance in child internalizing problems accounted for by genetic influences.
Construction of the Child Internalizing Problems Composite
We utilized multiple informants and modalities to create a child internalizing problems composite. Mothers reported child internalizing problems via the HBQ (Essex et al., 2002), the Children's Depression Inventory (CDI; Kovacs, 2003), and an Obsessions and Compulsions Questionnaire (OCQ; Waldman, undated). The HBQ depression (α = .72), overanxiousness (α = .82), and separation anxiety (α = .84) subscales and the OCQ scale (α = .79) measured child internalizing symptoms during the preceding 6 months, whereas the CDI scale (α = .85) assessed depression symptoms during the prior 2 weeks. HBQ, OCQ, and CDI scores were standardized and averaged to represent a mother-report via questionnaire component. Fathers also reported child internalizing problems on the HBQ (α = .63 for the depression scale, .77 for the overanxiousness scale, and .83 for the separation anxiety scale), OCQ (α = .75), and CDI (α = .81), and their scores were treated like those of mothers to form a father-report component. Mothers also reported child internalizing symptoms during the Diagnostic Interview Schedule for Children Version IV (DISC-IV; Shaffer, Fisher, Lucas, Dulcan, & Schwab-Stone, 2000). Past year symptom counts generated by the generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, agoraphobia, separation anxiety disorder, social phobia, specific phobia, and mood disorder modules were used. Module scores were averaged to represent a mother-report via structured interview component. We collected child report using the depression, overanxiousness, and separation anxiety subscales from the Berkeley Puppet Interview Symptomatology Scales (BPI-S; Ablow et al., 1999). Puppets were used to interview children and responses were coded for symptom severity. Coders' kappa statistics averaged .95. BPI-S subscale scores were averaged to form a child-report component. Two observers made global ratings of depression, obsessive-compulsive behavior, general anxiety, separation anxiety, and social phobia (α = .66 for the 10 ratings; 5 ratings made by 2 observers). Each observer rated both children in the twin pair on these items that were modeled after Bayley's (1993) Scales of Infant Development with items re-worded to be age-appropriate. Average inter-rater correlational agreement for the 5 global ratings was .44. Ratings on individual dimensions of psychopathology were averaged across the two observers, and these mean ratings on each of the 5 dimensions were averaged to create an observer rated component. Finally, the five components (mother report on questionnaires, father report, mother report in an interview, child report, observer ratings) were standardized and averaged to form the internalizing problems composite.
Construction of the Child Externalizing Problems Composite
We calculated a child externalizing problem composite using a similar procedure. Mothers reported child externalizing symptoms observed during the past six months via the HBQ conduct (α = .83), inattention (α = .87), impulsivity (α = .87), overt aggression (α = .74), and oppositional defiant (α = .86) subscales. Scale scores were averaged to represent a mother-report via questionnaire component. Fathers also reported child externalizing on the HBQ (α = .82 conduct scale, .86 inattention scale, .86 impulsivity scale, .69 overt aggression scale, .87 oppositional defiant scale), and the average of these scales formed a father-report component. Mothers also reported child externalizing symptoms on the DISC-IV conduct disorder, ADHD, and oppositional defiant disorder modules, which were averaged to represent a mother-report via structured interview component. Children reported on their own externalizing symptoms via the conduct, inattention, impulsivity, aggression, and oppositional defiant subscales of the BPI-S and subscale scores were averaged to form a child-report component. Observers made global ratings of aggression, hyperactivity, inattention, and non-compliance, with inter-rater correlational agreement on these dimensions averaging .70. Ratings on individual dimensions of psychopathology were averaged across the two observers, and these mean ratings on each of the 5 dimensions were averaged to create an observer rated component. Finally, the five components (mother report on questionnaires, father report, mother report in an interview, child report, observer ratings) were converted to z scores and averaged to form the externalizing composite.
Construction of the Parent Internalizing Problems Composite
Five scores derived from three measures composed the parent internalizing problems composite. Two scores were the lifetime symptom counts from the depression and generalized anxiety modules of the Composite International Diagnostic Interview (CIDI, Robins et al., 1988), a structured interview administered by phone. A third component was the Beck Depression Inventory score (BDI; Beck, Ward, Mendelson, Mock, & Erbaugh, 1961), which measured depressive symptoms during the prior two weeks. Alphas were .88 and .79 for mothers and fathers. The fourth and fifth components were scores on the Well-being and Stress Reactivity subscales of the Multidimensional Personality Questionnaire (MPQ; Patrick, Curtin, & Tellegen, 2002; Tellegen, 1985); these scores reflect more typical-range variation in well-being (positive self-view, positive affect, engagement in life) and stress reactivity (negative emotionality, guilt proneness, sleep disturbance). Alphas ranged from .86−.90. The five component scores were converted to z-scores and averaged separately for mothers and fathers. Finally, mother and father internalizing problems scores were averaged to generate the overall mid-parent internalizing problems composite.
Data Analysis: Co-twin mental health as G-risk
We used DeFries-Fulker (DF) regression (Cherny, DeFries, & Fulker, 1992; Cyphers, Phillips, Fulker, & Mrazek, 1990; Rodgers & Kohler, 2005) to test whether heritability differed as a function of measured experiential risk. DF regression requires a double entry data file in which each twin pair is entered twice. We double entered all twin pairs regardless of their risk status at the time of screening. This practice artificially doubled the sample size and thus standard errors were adjusted to match the actual number of degrees of freedom. This was accomplished by multiplying standard errors by ; this square root is in our case (Cherny et al., 1992). Prior to calculating interaction terms, all predictor variables were centered except for zygosity. Zygosity values were entered as 1 for MZ twin pairs and .5 for DZ pairs to reflect their levels of genetic relatedness.
The first step of our DF regression includes variables representing zygosity or relatedness (R), shared environment, heritability, and gender (G). Shared environmental influence is estimated by the extent to which each twin's internalizing problems score (Int2) is predicted by her co-twin's internalizing problems score (Int1). The b1 coefficient in the equation below represents shared environmental effects because it indicates the degree of similarity between co-twins' internalizing problem scores independent of shared genetic effects. The term “shared environment” refers to environmental influences that function to make children similar to one another. Heritability is estimated by the extent to which twin similarity is dependent on genetic relatedness. The partial regression coefficient for the regression of Twin 2 internalizing problems on the interaction between Twin 1 internalizing problems and relatedness (Int1 × R) represents the heritability of internalizing problems (i.e., the b3 value indicates heritability). Thus, the regression equation is
In the second step of the regression, we tested for a main effect of measured experiential risk (E-risk) by entering scores on the E-risk index. In step three, we tested the hypothesis that heritability would vary as a function of measured E-risk by entering the Int1 × R × E-risk index (E-risk) interaction term, which has the b6 coefficient in the equation below. At step 3, the regression equation becomes
In the final step we controlled for child externalizing by adding T2's externalizing score (Ext) to the set of predictors. Since externalizing problems covary with internalizing problems (r = .42, p < .001 in this sample) we examined whether the GxE predicted a portion of internalizing problems variance independent of externalizing covariation. At step 4, the regression equation becomes
To summarize, in this final regression, b1 estimates the shared environmental effect, b3 estimates heritability, and b6 estimates the GxE effect. These estimates are independent of gender (b4) and externalizing (b7) effects.
Data Analysis: Parent Mental Health as G-risk
We also used hierarchical linear regression in the parent mental health as G-risk method. We departed slightly from the practice of previous studies that implemented the parent mental health as G-risk method to take advantage of our multiple offspring data set. We averaged co-twin internalizing problems scores to form a mid-child score and used this value as our outcome, which is a more reliable indicator of offspring status than is the phenotype of a single child. To more closely parallel the co-twin mental health as G-risk method analyses, each twin's internalizing and externalizing problems scores were regressed on gender and zygosity (coded 1 and .5 as in the co-twin mental health as G-risk method) before they were averaged to form mid-child scores. Again, predictor variables were centered before the interaction term was calculated. Parent internalizing problems, and the E-risk index scores were entered in the first step and the interaction between parent internalizing problems and E-risk was entered in the second step. The third step controlled for mid-child externalizing.
RESULTS
Genetic Risk by Experience Correlation
G-risk based on parental and co-twin internalizing symptoms correlated modestly with E-risk (r ranging from .18–.22). Therefore, GxE reported below exist in the presence of modest genetic risk by experience correlations.
Co-twin Mental Health as G-risk
Data were available on 420 twin pairs (840 individuals) for the co-twin mental health as G-risk method analyses. Based on our screening procedure, 320 of the individuals were at least mildly at-risk for psychopathology, 237 were controls, and 283 were non-grouped co-twins. Results from step 3 of the DF regression are reported with all SEs corrected as explained above (see Table 2). Genetic influences significantly predicted internalizing problems (b = .486, SE = .180, p < .001), but shared environmental influences did not (b = .126, SE = .127, p = .16). Measured E-risk showed a significant effect (b = .072, SE = .025, p < .001) but neither zygosity (b = −.116, SE = .092, p = .21) nor gender (b = .017, SE = .023, p = .45) were significant predictors. Finally, the GxE was significant (b = .167, SE = .061, p < .001), accounting for 1.3% of internalizing problems variance. DF regressions were run separately for low and high E-risk groups to determine the direction of the heritability by E-risk interaction2. Heritability was elevated for children at low E-risk (.67) in comparison to their high E-risk counterparts (.36). This interaction was evaluated prior to controlling for externalizing problems in order to be more consistent with the literature on the heritability of internalizing problems. After controlling for the highly significant effect of child externalizing problems (b = .232, SE = .034, p < .001) in step 4, genetic influences (b = .460, SE = .169, p < .01) and the GxE remained significant (b = .163, SE = .058, p < .01), but the main effect of E-risk on internalizing problems became non-significant (b = .028, SE = .025, p = .26).
Table 2.
DF Regression Results: Co-twin Mental Health Indexing Genetic Risk
| B(SE) | β | t | R2 | |
|---|---|---|---|---|
| Step 3 | ||||
| relatedness | −.116 (.092) | −.054 | −1.261 | .274*** |
| gender | .017 (.023) | .033 | .752 | |
| h2 (co-twin Int × relatedness) | .486 (.180) | .343 | 2.706** | |
| c2 (co-twin Int) | .126 (.127) | .126 | .992 | |
| experiential risk index | .072 (.025) | .120 | 2.834** | |
| h2 × experiential risk index | .167 (.061) | .116 | 2.783** | |
| Step 4 | ||||
| relatedness | −.134 (.088) | −.062 | −1.530 | .348*** |
| gender | −.027 (.022) | −.052 | −1.227 | |
| h2 (co-twin Int × relatedness) | .460 (.169) | .325 | 2.722** | |
| c2 (co-twin Int) | .073 (.121) | .073 | .603 | |
| experiential risk index | .028 (.025) | .046 | 1.120 | |
| h2 × experiential risk index | .163 (.058) | .113 | 2.815** | |
| co-twin externalizing problems | .232 (.034) | .306 | 6.843** |
Note. h2 = heritability; c2 = shared environmental effects; Int = internalizing problems;
p ≤ .01.
p ≤ .001.
Parent Mental Health as G-risk
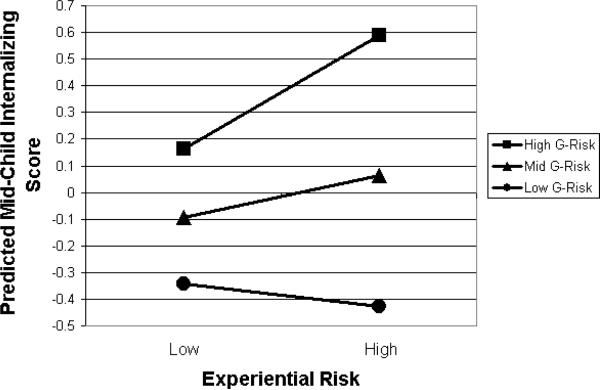
For these analyses, data were available for 357 twin pairs and their parents (a subset of the 431 pairs, with the difference in sample size due mainly to availability of paternal data3). Based on screening data, 260 of these children were at least mildly at-risk for psychopathology, 215 were controls, and 239 were non-grouped co-twins. Parameters from the second step of the regression analysis are presented (see Table 3). G-risk was significantly associated with child internalizing problems (b = .721, SE = .09, p < .001), but E-risk was not (b = .085, SE = .051, p = .10). The GxE was significantly associated with child internalizing problems (b = .241, SE = .09, p = .007), accounting for 1.6% of internalizing problems variance. Figure 1 presents predicted mid-child internalizing problems scores. The association between G-risk and child internalizing problems was stronger among those at elevated E-risk. After controlling for child externalizing (b = .312, SE = .042, p < .001) in step 3, G-risk (b = .567, SE = .086, p < .001) and the GxE remained significant (b = .194, SE = .084, p = .02), while the main effect of E-risk remained non-significant (b = .000, SE = .049, p = .99).
Table 3.
Regression Results: Parent Mental Health Indexing Genetic Risk Mid-child Internalizing Problems Predicted by Genetic Risk, Experiential Risk, and GxE Controlling for Mid-child Externalizing Problems
| B(SE) | β | t | R2 | R2 change | |
|---|---|---|---|---|---|
| Step 1 | |||||
| Genetic Risk | .58 (.07) | .39 | 8.01*** | .19*** | |
| Experiential Risk | .13 (.05) | .13 | 2.63** | ||
| Step 2 | |||||
| Genetic Risk | .72 (.09) | .49 | 8.06*** | .21*** | .016** |
| Experiential Risk | .09 (.05) | .09 | 1.68† | ||
| GxE | .24 (.09) | .16 | 2.70** | ||
| Step 3 | |||||
| Genetic Risk | .57 (.09) | .39 | 6.60*** | 0.32*** | .11*** |
| Experiential Risk | .00 (.05) | .00 | −0.02 | ||
| GxE | 0.19 (.08) | .13 | 2.33* | ||
| Externalizing | 0.31 (.04) | .36 | 7.44*** |
Note. Child internalizing and externalizing problem scores were residualized on gender and zygosity
≤ .10.
≤ .05.
p ≤ .01.
p ≤ .00
Figure 1.
Predicted Mid-Child Internalizing Problems Scores Plotted as a Function of Genetic Risk Based on Parental Internalizing Problems
Notes. Predicted scores plotted at 1 SD above and below the mean genetic risk score.
DISCUSSION
Reconciling results from the two methods
We found evidence for GxE for child internalizing problems using two different methods applied to highly overlapping samples of families, using only twins in one method and twins plus their parents in the other. Can the directions of these interactions be reconciled across methods? Results of the method using parental psychopathology as a proxy for G-risk, support a diathesis-stress model of child internalizing problems. That is, associations between G-risk and internalizing problems were stronger for children at elevated E-risk. Interpretation of results from the method that used co-twin psychopathology to index G-risk, is more complex.
Two theoretical models (typically presented as opposing) describe how GxE should be reflected in heritability at different levels of E-risk (Rutter et al., 2006). A diathesis-stress model predicts that heritability will be higher for those at elevated E-risk when genes interact with the shared environment. That is, some genetic effects are not manifest in the phenotype unless the environment is permissive, allowing for the expression of relevant genes. On the other hand, a bioecological model (Bronfenbrenner & Ceci, 1994, as interpreted by Rutter et al., 2006), predicts that heritability will be higher for those at low E-risk. The notion would be that stressful experiences (in the high range of E-risk) could lead to internalizing problems regardless of the level of G-risk. Correspondingly, genetic variation would be manifest in behavior when the predominant effect of high stress is absent. From this perspective, our co-twin mental health as G-risk method results are consistent with a bioecological model because the heritability of internalizing problems was higher for those at low E-risk.
These results do not, however, discredit the diathesis-stress model. The co-twin and parent mental health as G-risk methods estimated the proportion of variance attributable to GxE to range from 1.3–1.5% based on the R2 change parameters obtained after adding the GxE terms into the regressions. In the co-twin mental health as G-risk method, however, heritability of internalizing problems was estimated at 67% for children at low E-risk vs. 36% for those at high E-risk. This difference in heritability is much too large to be accounted for by the measured GxE alone. In short, our results are consistent with a net effect that might result from processes predicted by operation of both the diathesis-stress model and the bioecological models. It is important to note that our methods for estimating G-risk differ substantively in the types of genetic influences they account for. The parent mental health as G-risk method marks only additive genetic risk while the co-twin mental health as G-risk method indexes both additive and non-additive G-risk. This raises the possibility that patterns of GxE can differ depending on what type of G-risk is measured. That is, GxE may follow a diathesis-stress pattern for some aspects of G-risk but follow a bioecological pattern for others, even when the outcome and E-risk factors of interest are identical. Our results suggest that it may be overly simplistic to expect all GxEs for a given phenotype to be in the same direction. High levels of psychosocial adversity may reduce the impact of some genes (relative to the genes' impact under less adverse conditions) while simultaneously allowing expression of the other genes that raise the liability internalizing problems. If both types of GxE processes are in fact operative, our results suggest that the overall effect of GxE operating in a diathesis-stress manner is overshadowed by the operation of GxE consistent with the bioecological model. Thus, the directions of the interactions derived from our 2 methods can be conceptually reconciled; together they provide strong evidence that GxE does occur for child internalizing problems4.
Effect sizes
The main effects of genetic and experiential risk accounted for a much larger portion of variance in child internalizing problems than did GxE. When G-risk was based on co-twin mental health status, direct effects of G and E-risk together accounted for 26.1% of internalizing problems variance whereas the GxE accounted for only 1.3%. When G-risk was based on parent mental health, the main effects of G and E-risk accounted for a combined 19.2% of variance whereas the GxE accounted for only 1.6%. It is likely, however, that our GxE effect sizes are underestimated due to difficulties in detecting interaction effects using quasi-experimental designs (McClelland & Judd, 1993). Although GxE are inherently interesting and theoretically important to our understanding of the mechanisms involved in development, main effects of G (at least when inferred from phenotypes and degree of genetic relatedness) and E-risk are far better predictors of child internalizing problems than is their interaction.
Comorbidity
Co-occurrence of internalizing and externalizing symptoms is widely recognized in pediatric epidemiology. Thus, we adjusted internalizing outcomes for the presence of externalizing symptoms in our regression analyses. The evidence for GxE remained; however, the main effect of E-risk became non-significant in the co-twin mental health as G-risk method. This outcome suggests that the direct effect of E-risk on internalizing problems might have been due to co-occurring externalizing symptoms and is consistent with the finding that many family-related stressors tend to be non-specific risk factors (Essex et al., 2006). In any case, controlling for comorbid behavioral problems appears to be crucial for the interpretation of results in this area of research.
Limitations
Rutter et al. (2006) suggested that studies that test for GxE by calculating heritability separately for those at high vs. low E-risk should index E-risk using factors proximal to the child if they hope to adequately test the bioecological model. Although we included proximal factors in our E-risk index (negative life events, negative mother-child interactions), we also included more distal factors (SES, single-parent home). From this perspective, our results may offer only limited support for the bioecological model. In addition, Rutter et al. (2006) assert that researchers should ensure that the effects of E-risk are in fact environmentally mediated. Given that our E-risk factors were measured at the family rather than the child level, we were unable to verify that effects of measured E-risk were environmentally mediated. However, we did show that the E-risk index was only modestly correlated with the G-risk indices.
Our study is limited in two especially important ways because we did not report molecular genetic data. First, although we detected a statistical interaction between E and G-risk, we did not demonstrate that experiences interact with genes at a molecular level (e.g., experiences leading to changes in the methylation or acetylation patterns of DNA and associated proteins). That is, we found evidence for statistical moderation, not for a biological change in DNA or chromatid structure or gene expression dependent on experience. Second, with no biological mechanism proposed to guide hypotheses regarding the direction of interaction, we could not assert a strong prediction in this regard. Instead we relied on the mixed findings reported in the literature to generate research questions and evaluate the plausibility of our results.
As in any study, results should not be generalized to populations with different distributions of environmental risk or internalizing outcomes than our sample. For example, different patterns of GxE might occur in clinical samples or populations with prevalent abuse or neglect. Moreover, generalization to other age groups would also be hazardous, given that child gender becomes a predictor of internalizing symptoms during adolescence (Hyde, Mezulis, & Abramson, 2008).
Implications
Studies of the interaction of genetic and environmental factors for human behavior should move from the current stage of isolated reports to more systematic examinations, which we hope this study helps to initiate. Our results strengthen the case for GxE in the development of childhood anxiety and depression but also highlight the importance of main effects.
Key Points.
The literature shows that heritability estimates for child internalizing problems (i.e., symptoms of depression and anxiety) typically range from 23–62%.
The literature also shows that child internalizing problems are associated with experiential risk factors including low socioeconomic status, single parent upbringing, negative parent-child interactions, and negative life events.
Regression models indicated that genetic influences interact with experiential risk factors to predict child internalizing problems, both when co-twin mental health status indexes genetic risk and when parent symptomology indexes genetic risk.
Results thus suggest that experiential stress can alter associations between genetic influences and child mental health.
Our findings indicate that dominant models of GxE that are typically seen as opposing (i.e. diathesis-stress and bioecological models), may in fact operate simultaneously in the development of child internalizing problems.
Acknowledgements
This work was supported by research grants from the National Institute of Mental Health (R01 MH59785 and R37 MH50560 to Goldsmith), and the Wisconsin Center for Affective Science (P50 MH069315 and P50 MH84051). Infrastructure support was provided by the Waisman Center via a core grant from NICHD (P30 HD03352). Vendlinski was partially supported by NIMH training grant T32 MH18931. We appreciate a suggestion for data analysis from John DeFries and statistical advice from Kristin Javaras.
Abbreviations
- DF
DeFries-Fulker regression
- DZ
dizygotic
- E-risk
experiential risk
- G-risk
genetic risk
- GxE
genetic risk by experience interaction
- MZ
monozygotic
- SES
socioeconomic status
Footnotes
Analyses were also run leaving E-risk as an ordinal variable. Results were similar to those reported for the co-twin mental health as G-risk method. However, in contrast to the results presented, the GxE tested in the parent mental health as G-risk method was not significant. This suggests that when G-risk is estimated using parental psychopathology there is a threshold level of E-risk beyond which increasing E-risk has little effect on the heritability of child internalizing problems.
Interactions detected using DF regression are sometimes probed by taking B for the h2 term and adding it to B for the interaction term multiplied by the measured environmental variable. This method is inappropriate in this case because we did not include all 2-way interactions (i.e., relatedness × E-risk and c2 × E-risk) in our regression.
Children of fathers who did not participate had significantly higher mean levels of internalizing and externalizing problems. These differences, although significant in our large sample, are relatively small in magnitude. For instance, the more highly significant difference (for internalizing problems) was estimated at d =.23. To determine whether excluding children without father data impacted parameter estimates, we ran parent mental health as G-risk method analyses for all children included in the co-twin mental health as G-risk method analyses. For families without father data, mother internalizing problem scores were used in place of mid-parent internalizing problem scores. Results using the full sample in this way did not differ substantively from the parent mental health as G-risk method results presented.
As mentioned in the Introduction, selective reporting of positive GxE findings in the literature may lead to biases. To counteract such biases we note that similar analyses were conducted to test for GxE for childhood externalizing problems. No evidence for interaction was detected. Results for these analyses are available from the first author upon request.
References
- Ablow JC, Measelle JR, Kraemer HC, Harrington R, Luby J, Smider N, Dierker L, Clark V, Dubicka B, Heffelfinger A, Essex MJ, Kupfer DJ. The MacArthur three-city outcome study: Evaluating multi-informant measures of young children's symptomatology. Journal of the American Academy of Child and Adolescent Psychiatry. 1999;38:1580–1590. doi: 10.1097/00004583-199912000-00020. [DOI] [PubMed] [Google Scholar]
- Bayley N. Bayley Scales of Infant Development: Birth to two years. Psychological Corporation; San Antonio, TX: 1993. [Google Scholar]
- Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Archives of General Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- Beck JE, Shaw DS. The influence of perinatal complications and environmental adversity on boys' antisocial behavior. Journal of Child Psychology and Psychiatry. 2005;46:35–46. doi: 10.1111/j.1469-7610.2004.00336.x. [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner U, Ceci SJ. Nature-nurture reconceptualized in developmental perspective: A bioecological model. Psychological Review. 1994;101:568–586. doi: 10.1037/0033-295x.101.4.568. [DOI] [PubMed] [Google Scholar]
- Button TM, Lau JYF, Maughan B, Eley TC. Parental punitive discipline, negative life events and gene-environment interplay in the development of externalizing behavior. Psychological Medicine. 2008;38:29–39. doi: 10.1017/S0033291707001328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Button TM, Scourfield J, Martin N, Purcell S, McGuffin P. Family dysfunction interacts with genes in the causation of antisocial symptoms. Behavior Genetics. 2005;35:115–120. doi: 10.1007/s10519-004-0826-y. [DOI] [PubMed] [Google Scholar]
- Cherny SS, DeFries JC, Fulker DW. Multiple regression of twin data: A model fitting approach. Behavior Genetics. 1992;22:489–497. doi: 10.1007/BF01066617. [DOI] [PubMed] [Google Scholar]
- Cohen J, Cohen P, West SG, Aiken LS. Applied Multiple Regression / Correlation Analysis for the Behavioral Sciences. 3rd ed. Erlbaum; Mahwah, New Jersey: 2003. [Google Scholar]
- Costello EJ, Foley DL, Angold A. 10-Year research update review: The epidemiology of child and adolescent psychiatric disorders: II. Developmental epidemiology. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:8–25. doi: 10.1097/01.chi.0000184929.41423.c0. [DOI] [PubMed] [Google Scholar]
- Costello EJ, Pine DS, Hammen C, March JS, Plotsky PM, Weissman MM, Biederman J, Goldsmith HH, Kaufman J, Lewinsohn PM, Hellander M, Hoagwood K, Koretz DS, Nelson CA, Leckman JF. Development and natural history of mood disorders. Biological Psychiatry. 2002;52:529–542. doi: 10.1016/s0006-3223(02)01372-0. [DOI] [PubMed] [Google Scholar]
- Cyphers LA, Phillips K, Fulker DW, Mrazek DA. Twin temperament during the transition from infancy to early childhood. Journal of the American Academy of Child and Adolescent Psychiatry. 1990;29:393–397. doi: 10.1097/00004583-199005000-00010. [DOI] [PubMed] [Google Scholar]
- Eaves LJ. Genotype × environment interaction in psychopathology: fact or artifact? Twin Research and Human Genetics. 2006;9:1–8. doi: 10.1375/183242706776403073. [DOI] [PubMed] [Google Scholar]
- Eley TC, Liang H, Plomin R, Sham P, Sterne A, Williamson R, Purcell S. Parental familial vulnerability, family environment, and their interactions as predictors of depressive symptoms in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:298–306. doi: 10.1097/00004583-200403000-00011. [DOI] [PubMed] [Google Scholar]
- Erlenmeyer-Kimling L. Gene-environment interactions and the variability of behavior. In: Ehrman L, Omenn GS, Caspari E, editors. Genetics, environment, and behavior. Academic Press; New York: 1972. pp. 181–208. [Google Scholar]
- Essex MJ, Kraemer HC, Armstrong JM, Boyce WT, Goldsmith HH, Klein MH, Woodward H, Kupfer DJ. Exploring risk factors for the emergence of children's mental health problems. Archives of General Psychiatry. 2006;63:1246–1256. doi: 10.1001/archpsyc.63.11.1246. [DOI] [PubMed] [Google Scholar]
- Essex MJ, Boyce WT, Goldstein LH, Armstrong JM, Kraemer HC, Kupfer DJ. The confluence of mental, physical, social, and academic difficulties in middle childhood. II: Developing the MacArthur Health and Behavior Questionnaire. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:588–603. doi: 10.1097/00004583-200205000-00017. [DOI] [PubMed] [Google Scholar]
- Forget-Dubois N, Perusse D, Turecki G, Girard A, Billette JM, Rouleau G, Boivin M, Malo J, Tremblay RE. Diagnosing zygosity in infant twins: physical similarity, genotyping, and chorionicity. Twin Research. 2003;6:479–485. doi: 10.1375/136905203322686464. [DOI] [PubMed] [Google Scholar]
- Goldsmith HH. A zygosity questionnaire for young twins: A research note. Behavior Genetics. 1991;21:257–269. doi: 10.1007/BF01065819. [DOI] [PubMed] [Google Scholar]
- Hammen C, Brennan PA, Shih JH. Family discord and stress predictors of depression and other disorders in adolescent children of depressed and nondepressed women. Journal of the American Academy of Child and Adolescent Psychiatry. 2004;43:994–999. doi: 10.1097/01.chi.0000127588.57468.f6. [DOI] [PubMed] [Google Scholar]
- Harden KP, Hill JE, Turkheimer E, Emery RE. Gene-Environment correlation and interaction in peer effects on adolescent alcohol and tobacco use. Behavior Genetics. 2008;38:339–347. doi: 10.1007/s10519-008-9202-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, DiRago AC, Iacono WG, McGue M. Gene-environment interplay in internalizing disorders: consistent findings across six environmental risk factors. Journal of Child Psychology and Psychiatry. 2009a;50:1309–1317. doi: 10.1111/j.1469-7610.2009.02100.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hicks BM, South SC, DiRago AC, Iacono WG, McGue M. Environmental adversity and increasing genetic risk for externalizing disorders. Archives of General Psychiatry. 2009b;66:640–648. doi: 10.1001/archgenpsychiatry.2008.554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hyde JS, Mezulis AH, Abramson LY. The ABCs of depression: Integrating affective, biological, and cognitive models to explain the emergence of the gender difference in depression. Psychological Review. 2008;115:291–313. doi: 10.1037/0033-295X.115.2.291. [DOI] [PubMed] [Google Scholar]
- Jaffee SR, Caspi A, Moffitt TE, Dodge KA, Rutter M, Taylor A, Tully LA. Nature X nurture: Genetic vulnerabilities interact with physical maltreatment to promote conduct problems. Development and Psychopathology. 2005;17:67–84. doi: 10.1017/s0954579405050042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jinks JL, Fulker DW. Comparison of the biometrical genetical, MAVA, and classical approaches to the analysis of human behavior. Psychological Bulletin. 1970;73:311–349. doi: 10.1037/h0029135. [DOI] [PubMed] [Google Scholar]
- Kendler K, Kessler RC, Walters EE, MacLean C, Neale MC, Eaves LJ. Stressful life events, genetic liability, and onset of an episode of major depression in women. The American Journal of Psychiatry. 1995;152:833–842. doi: 10.1176/ajp.152.6.833. [DOI] [PubMed] [Google Scholar]
- Kovacs M. Children's depression inventory: Technical manual update. Multi-Health Systems, Inc; North Tonawanda, NY: 2003. [Google Scholar]
- Lau JYF, Eley TC. Disentangling gene-environment correlations and interactions on adolescent depressive symptoms. Journal of Child Psychology and Psychiatry. 2008;49:142–150. doi: 10.1111/j.1469-7610.2007.01803.x. [DOI] [PubMed] [Google Scholar]
- Lau JYF, Gregory AM, Goldwin MA, Pine DS, Eley TC. Assessing gene-environment interactions on anxiety symptom subtypes across childhood and adolescence. Development and Psychopathology. 2007;19:1129–1146. doi: 10.1017/S0954579407000582. [DOI] [PubMed] [Google Scholar]
- Lemery-Chalfant K, Goldsmith HH, Schmidt NL, Arneson CL, Van Hulle CA. Wisconsin Twin Panel: Current directions and findings. Twin Research and Human Genetics. 2006;9:1038–1042. doi: 10.1375/183242706779462363. [DOI] [PubMed] [Google Scholar]
- Lovejoy MC, Graczyk PA, O'Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytic review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- McClelland GH, Judd CM. Statistical difficulties of detecting interactions and moderator effects. Psychological Bulletin. 1993;114:376–390. doi: 10.1037/0033-2909.114.2.376. [DOI] [PubMed] [Google Scholar]
- Miles DR, Silberg JL, Pickens RW, Eaves LJ. Familial influences on alcohol use in adolescent female twins: Testing for genetic and environmental interactions. Journal of Studies on Alcohol. 2005;66:445–451. doi: 10.15288/jsa.2005.66.445. [DOI] [PubMed] [Google Scholar]
- Patrick CJ, Curtin JJ, Tellegen A. Development and validation of a brief form of the Multidimensional Personality Questionnaire. Psychological Assessment. 2002;14:150–163. doi: 10.1037//1040-3590.14.2.150. [DOI] [PubMed] [Google Scholar]
- Plomin R, Bergeman CS. The nature of nurture: Genetic influence on `environmental' measures. Behavioral and Brain Sciences. 1991;14:373–427. [Google Scholar]
- Price TS, Freeman B, Craig I, Petrill SA, Ebersole L, Plomin R. Infant zygosity can be assigned by parental report questionnaire data. Twin Research. 2000;3:129–133. doi: 10.1375/136905200320565391. [DOI] [PubMed] [Google Scholar]
- Rice F, Harold GT, Shelton KH, Thapar A. Family conflict interacts with genetic liability in predicting childhood and adolescent depression. Journal of the American Academy of Child and Adolescent Psychiatry. 2006;45:841–848. doi: 10.1097/01.chi.0000219834.08602.44. [DOI] [PubMed] [Google Scholar]
- Rice F, Thapar A. Depression and anxiety in childhood and adolescence: Developmental pathways, genes and environment. In: Kim Y-K, editor. Handbook of Behavior Genetics. Springer; New York: 2009. p. 385. [Google Scholar]
- Robins LN, Wing J, Wittchen HU, Helzer JE, Babor TF, Burke J, Farmer A, Jablenski A, Pickens R, Regier DA. The composite international diagnostic interview: An epidemiological instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of_General Psychiatry. 1988;45:1069–1077. doi: 10.1001/archpsyc.1988.01800360017003. [DOI] [PubMed] [Google Scholar]
- Rodgers JL, Kohler H. Reformulating and simplifying the DF analysis model. Behavior Genetics. 2005;35:211–217. doi: 10.1007/s10519-004-1020-y. [DOI] [PubMed] [Google Scholar]
- Rutter M. Protective factors in children's responses to stress and disadvantage. In: Kent M, Rolf J, editors. Primary Prevention of Psychopathology. University Press of New England; Hanover, New Hampshire: 1979. pp. 49–74. [Google Scholar]
- Rutter M, Moffitt TE, Caspi A. Gene-environment interplay and psychopathology: multiple varieties but real effects. Journal of Child Psychology and Psychiatry. 2006;47:226–261. doi: 10.1111/j.1469-7610.2005.01557.x. [DOI] [PubMed] [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: Development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology. 1978;46:932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Shaffer D, Fisher P, Lucas CP, Dulcan MK, Schwab-Stone ME. NIMH Diagnostic Interview Schedule for Children Version IV (NIMH DISC-IV): Description, differences from previous versions and reliability of some common diagnoses. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39:28–38. doi: 10.1097/00004583-200001000-00014. [DOI] [PubMed] [Google Scholar]
- Silberg J, Rutter M, Neale M, Eaves L. Genetic moderation of environmental risk for depression and anxiety in adolescent girls. British Journal of Psychiatry. 2001;179:116–121. doi: 10.1192/bjp.179.2.116. [DOI] [PubMed] [Google Scholar]
- Tellegen A. Structures of mood and personality and their relevance to assessing anxiety, with an emphasis on self-report. In: Tuma AH, Maser JD, editors. Anxiety and the anxiety disorders. Erlbaum; Hillsdale, NJ: 1985. pp. 681–706. [Google Scholar]
- Tuvblad C, Grann M, Lichtenstein P. Heritability for adolescent antisocial behavior differs with socioeconomic status: gene-environment interaction. Journal of Child Psychology and Psychiatry. 2006;47:734–743. doi: 10.1111/j.1469-7610.2005.01552.x. [DOI] [PubMed] [Google Scholar]
- Waldman ID. Obsessions and Compulsions Questionnaire. Department of Psychology, Emory University; Atlanta, GA: undated. Unpublished questionnaire. [Google Scholar]
- World Health Organization . The world health report 2001: Mental health: New understanding, new hope. World Health Organization; Geneva: 2001. [Google Scholar]