Abstract
Background
Smoking is one of well known environmental factors causing endothelial dysfunction and plays important role in the atherosclerosis. We investigated the effect of cilostazol could improve the endothelial dysfunction in smokers with the measurement of flow-mediated dilatation (FMD).
Methods
We enrolled 10 normal healthy male persons and 20 male smokers without any known cardiovascular diseases. After measurement of baseline FMD, the participants were medicated with oral cilostazol 100 mg bid for two weeks. We checked the follow up FMD after two weeks and compared these values between two groups.
Results
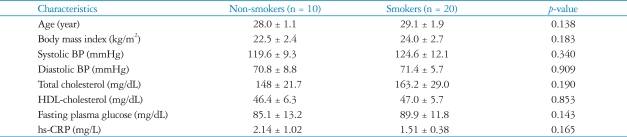
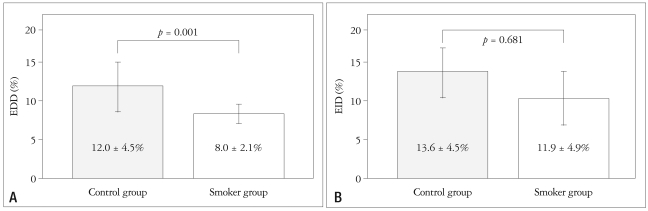
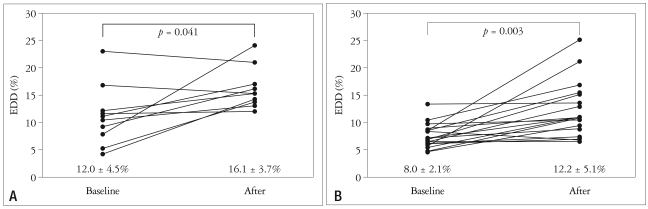
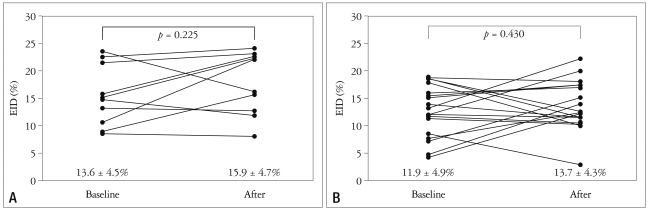
There was no statistical difference of baseline characteristics including age, body mass index, serum cholesterol profiles, serum glucose and high sensitive C-reactive protein between two groups. However, the control group showed significantly higher baseline endothelium-dependent dilatation (EDD) after reactive hyperemia (12.0 ± 4.5% in the control group vs. 8.0 ± 2.1% in the smoker group, p = 0.001). However, endothelium-independent dilatation (EID) after sublingual administration of nitroglycerin was similar between the two groups (13.6 ± 4.5% in the control group vs. 11.9 ± 4.9% in the smoker group, p = 0.681). Two of the smoker group were dropped out due to severe headache. After two weeks of cilostazol therapy, follow-up EDD were significantly increased in two groups (12.0 ± 4.5% to 16.1 ± 3.7%, p = 0.034 in the control group and 8.0 ± 2.1% to 12.2 ± 5.1%, p = 0.003 in the smoker group, respectively). However, follow up EID value was not significantly increased compared with baseline value in both groups (13.6 ± 4.5% to 16.1 ± 3.7%, p = 0.182 in the control group and 11.9 ± 4.9% to 13.7 ± 4.3%, p = 0.430 in the smoker group, respectively).
Conclusion
Oral cilostazol treatment significantly increased the vasodilatory response to reactive hyperemia in two groups. It can be used to improve endothelial function in the patients with endothelial dysfunction caused by cigarette smoking.
Keywords: Endothelial dysfunction, Smoking, Cilostazol
Introduction
Normal endothelial functions include control of platelet adhesion, mediation of coagulation and immune function, and control of volume and electrolyte content of body components.1) Endothelial dysfunction is a pathophysiological condition of abnormal process carried out by the endothelium. It is thought to be a key initial step in the development of atherosclerosis and can be used as a prognostic marker in predicting cardiovascular events including stroke and heart attacks.2),3) Endothelial dysfunction can be resulted from disease processes including hypertension, dyslipidemia, and diabetes as well as from environmental factors such as smoking.1)
Endothelial dysfunction can be characterized as the inability of arteries to dilate fully in response to appropriated stimuli. This can be detected by flow-mediated dilatation (FMD) using temporary arterial occlusion by inflating a blood pressure cuff to high pressures.4) Flow-mediated changes in conduit artery diameter are caused by shear-stress induced generation of endothelia derived vasoactive mediators including nitric oxides.5),6)
Cilostazol (Otsuka Pharmaceutical Co. Tokushima, Japan), 6-[4-(1-cyclohexyl-1H-tetrazol-5-yl)butoxy]-3,4-dihydro-2(1H)-quinolinone, is a 2-oxo-quinoline derivative with anti-thrombotic, vasodilator, antimitogenic and cardiotonic properties.7) The compound is a potent inhibitor of phosphodiesterase (PDE)-3. It may be useful for treating chronic arterial occlusive diseases and symptoms of intermittent claudication.8) Cilostazol inhibits platelet aggregation and has considerable antithrombotic effects in vivo. Also, this compound relaxes vascular smooth muscle and inhibits mitogenesis and migration of vascular smooth muscle cells. In the heart, it has positive inotropic and chronotropic effects.7),8)
This present study investigated the effects of cilostazol that could improve the endothelial dysfunction, especially in young male smokers.
Methods
Subjects
We enrolled 10 healthy male non-smokers and 20 active male smokers, average 6.0 ± 3.3 pack years, with matching age and weight. They were all volunteers without having a past or present history of coronary diseases and the results of clinical laboratory tests showing no signs of hypertension, dyslipidemia or diabetes. They filled up the informed consent. Total 200 mg/day of oral cilostazol was administered divided into morning and evening for two weeks. The levels of smoking in the smoker group were remained constantly during the study period.
Vascular endothelial function test
FMD was measured according to the methods of previously reported article by Celermajer et al.3) Each participants rested for about 20 minutes, and their internal diameter of the brachial artery were measured with a Sequoia 512 (Siemens Medical Solutions, Mountain View, CA) equipped with a 10-MHz linear ultrasound probe.
The diameter of the brachial artery was measured in the response to an increase in blood flow (causing shear-stress) during reactive hyperemia (induced by transient inflation of a blood pressure cuff). This leads to endothelium-dependent dilatation (EDD). Endothelium-independent dilatation (EID) was defined as a proportional increase in the diameter to sub-lingual nitroglycerin, an endothelium-independent dilator. The brachial artery was scanned and the diameter measured during four conditions; at baseline, during reactive hyperemia (induced by transient inflation of a sphygmomanometer cuff), 20 minutes after hyperemia and finally after administration of a sublingual nitroglycerin. After measurement of baseline brachial artery diameter (BD0), a sphygmomanomter cuff was used to apply up to 200 mmHg of pressure for 5 minutes around the upper part of the arm. Follow-up brachial artery diameter (BDh) was measured within 5 minutes after deflation of a blood pressure cuff. Another baseline brachial artery diameter (BD1) was measured after 20 minutes of rest after reactive hyperemia. Vasodilator response was obtained (BDn) within 4 minutes after administration of a single high dose (400 mg) of sublingual nitroglycerin tablet.
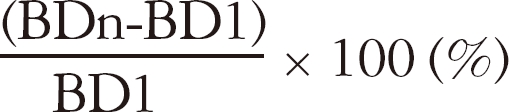
EDD was calculated according to the following formula:
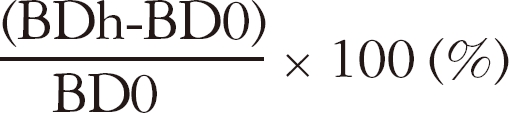
EID was calculated according to the following formula:
Statistical analysis
We used a commercial program, SPSS version 17.0 (SPSS Inc., Chicago, Illinois, USA) for Microsoft Windows, for statistical analysis. Numeric variables are expressed as mean ± SD. The difference of continuous variables between two groups was analyzed using a nonparametric test (Mann-Whitney U test). The difference between the baseline and follow-up data was analyzed using the paired sample t-test.
Intraobserver and interobserver agreements in FMD were tested using the baseline values of 10 participants according to the statistical methods proposed by Bland and Altman.9) All measurements were transformed to an equivalent percentage scale of agreement, according to the following formula;
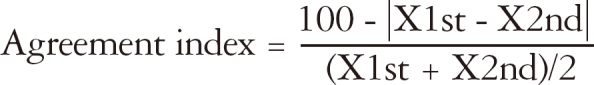
in which X1st and X2nd are measures obtained in twice-repeated evaluation using same technique in the same patient. The measure of reproducibility was 2 SD of the intraobserver and interobserver agreement indexes. Therefore, these coefficient of variations (COV) were equal to 2 SD of 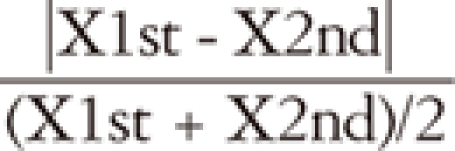 .
.
The intraobserver agreement was 90.8% and the COV was 8.9%. The interobserver agreement was 82.8% and the COV was 14.3%. A p value less than 0.05 was considered statistically significant.
Results
There was no significant difference in the clinical characteristics including age, body mass index, blood pressure, serum cholesterol profile, high sensitive C-reactive protein, and serum glucose level between two groups (Table 1). There was no significant side-effect associated with use of oral cilostazol except headache. Though majority subjects with headache were well controlled with oral analgesics, two of 20 smokers dropped out because of uncontrolled severe headache.
Table 1.
Baseline clinical and laboratory characteristics
BP: blood pressure, HDL-cholesterol: high density lipoprotein-cholesterol, hs-CRP: high sensitive C-reactive protein
Baseline EDD was significantly higher in the control group than in the smoker group (12.0 ± 4.5 in the control group vs. 8.0 ± 2.1% in the smoker group, p = 0.002, Fig. 1A). Baseline EID was similar in two groups (13.6 ± 4.5% in the control group vs. 11.9 ± 4.9% in the smoker group, p = 0.681, Fig. 1B). After two weeks of oral cilostazol treatment, follow-up EDD values were significantly increased in both groups (control group: 12.0 ± 4.5 to 16.1 ± 3.7%, p = 0.041, Fig. 2A; smoker group: 8.0 ± 2.1 to 12.2 ± 5.1%, p = 0.003, Fig. 2B). Follow-up EDD in the control group showed higher value than that of control group (16.1 ± 3.7 in the control group vs. 12.2 ± 5.1% in the smoker group, p = 0.018).
Fig. 1.
Comparison of endothelium-dependent dilatation (EDD) (A) and endothelium-independent dilatation (EID) (B) in the control and smoker group. Data are expressed as the mean ± standard deviation.
Fig. 2.
Effect of cilostazol treatment on endothelium-dependent dilatation (EDD) in the control group (A) and smoker group (B). A significant effect of cilostazol treatment on EDD is observed.
However, follow up EID value was not significantly increased compared with baseline value in both groups. (13.6 ± 4.5% to 16.1 ± 3.7%, p = 0.182 in the control group, Fig. 3A; 11.9 ± 4.9% to 13.7 ± 4.3%, p = 0.430 in the smoker group, Fig. 3B).
Fig. 3.
Effect of cilostazol treatment on endothelium-independent dilatation (EID) in the control group (A) and smoker group (B). There is no significant difference between baseline and post-treatment values. Also, there is no statistical significance between post EID values of two groups.
Discussion
In this FMD study with oral cilostazol, we demonstrated decreased baseline EDD level in the smoker group and significant improvement of EDD with administration of oral cilostazol in this group. However, cilostazol did not change the EID in this group.
Nitric oxide (NO), also known as the endothelium-derived Nitric oxide (NO), also known as the endothelium-derived relaxing factor (EDRF), is a chemical compound which is an important signaling molecule in the mammalian bodies. It is biosynthesized endogenously from L-arginine and oxygen by various nitric oxide synthase (NOS).10) It contributes to vessel homeostasis by inhibiting platelet aggregation, vascular smooth muscle contraction and growth, and leukocyte adhesion to the endothelium.10) FMD is one of methods to exam endothelial function. Increased shear stress in the arterial wall, usually caused by occlusion of the artery, can open specialized ion channels in the endothelium and influxed calcium ions through these channels stimulate endothelial nitric oxide synthase (eNOS). Increased eNOS activity enhanced NO synthesis and elevated NO evokes vasodilation.3) The vasodilatory effect of NO, EDRF, on the vessel (vasodilation) can be assessed by FMD. Arterial distensibility after reactive hyperemia is influenced by variable factors. FMD can be influenced by a single high-fat meal,11) mental stress,12) cigarette smoking,13) hyperglycemia,14) and changes in electrolytes (sodium and calcium).15) Also, EDD can be decreased by theophylline (adrenoreceptor agonist) or ibuprofen (prostaglandin synthesis inhibitor).16)
Cigarette smoking is one of the well-known risk factors causing endothelial dysfunction and there are strong relationships between cigarette smoking, atherosclerotic burden, and ischemic heart disease.17-19) Cigarette smoking induces initial atherosclerosis and promotes cardiovascular disease through multiple mechanisms including vasomotor, neurohormonal, and hemoatologic dysfunction, and increased oxidative stress19),20) Endothelial dysfunction can be resulted from inhaled cigarette smoke. Smoking as few as 2 cigarettes a day doubles the number of damaged endothelial cells in the blood stream.19-21)
There are several drugs improve endothelial dysfunction including angiotensin converting enzyme inhibitors, angiotensin receptor blockers, and nifedipine in the hypertensive patients, statins, fibrates and omega-3 fatty acid in the dyslipidemic patients, metformin and rosiglitazone in the diabetic patients.22) Few studies have been reported in the improvement of endothelial dysfunction in the smokers. Smoking cessation is one of the well-known methods to restore endothelial dysfunction.23) Guthikonda et al.24) published their study that allopurinol reverses endothelial dysfunction in the heavy smokers. Oida et al.25) presented that oral cilostazol treatment can be associated with improvement of endothelial dysfunction.
Cilostazol, a selective PDE-3 inhibitor, increases cyclic adenosine mono-phosphate (cAMP) in the platelets and inhibits platelet aggregation. Moreover, increased cAMP in the vascular smooth muscle cells activates protein kinase A and decreases intracellular calcium concentration. These effects result in vasodilation.26) Yasuda et al.26) reported that two weeks treatment of oral cilostazol increased tissue blood flow through the pedal vessels through vasodilation in the patients with peripheral arterial occlusive disease. Cilostazol has been approved by the Food and Drug Administration (FDA) in the treatment of peripheral arterial occlusive disease since 1999.27) Recently, triple combination antiplatelet therapy, aspirin, clopidogrel and cilostazol, has been reported to reduce thrombotic complication and recurrence of restenosis after implantation of coronary stent, especially in the diabetic patients.28)
Additional effects of cilostazol on the vascular endothelium have been described. Cilostazol has been associated with increased NO production. Ikeda et al.29) published their study showing cilostazol increased NO production in cultured vascular smooth muscle cells via cAMP pathway. Nakamura et al.30) reported that cilostazol dilated thoracic aorta via released NO from aortic endothelium. Increased NO production with cilostazol treatment can be associated with increased EDD in our study. Our result is similar to that of the previously reported article by Oida et al.25) However, the mean age of the participants was younger (late twenties vs. late thirties) and treated dosage was higher (200 mg per day vs. 150 mg per day) in our study. Because of younger age and shorter duration of smoking, the EDD level in our study may be associated with higher value than that of study by Oida et al.25)
Cilostazol improved reactive hyperemia in these eighteen smokers. This effect can be resulted from the NO production and relaxation of smooth muscle cells in the vessel. Endothelial dysfunction can be resulted from smoking as a result of increased oxidative stresses such as oxygen free radical which disturb normal endothelial functions. Therefore, cilostazol can improve endothelial dysfunctions caused by cigarette smoking.
In this study, most of participants complained headache after cilostazol medication. Most normal participants complained severe headache despite of oral analgesic treatment. Moreover, two of 20 smokers dropped out due to severe headache.
In conclusion, the administration of cilostazol improves the vasodilatory response to reactive hyperemia in the smokers.
References
- 1.Celermajer DS. Endothelial dysfunction: does it matter? Is it reversible? J Am Coll Cardiol. 1997;30:325–333. doi: 10.1016/s0735-1097(97)00189-7. [DOI] [PubMed] [Google Scholar]
- 2.Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993;362:801–809. doi: 10.1038/362801a0. [DOI] [PubMed] [Google Scholar]
- 3.Celermajer DS, Sorensen KE, Gooch VM, Spiegelhalter DJ, Miller OI, Sullivan ID, Lloyd JK, Deanfield JE. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115. doi: 10.1016/0140-6736(92)93147-f. [DOI] [PubMed] [Google Scholar]
- 4.Jeong YH, Lee SW, Choi BR, Kim IS, Seo MK, Kwak CH, Hwang JY, Park SW. Randomized comparison of adjunctive cilostazol versus high maintenance dose clopidogrel in patients with high post-treatment platelet reactivity: results of the ACCEL-RESISTANCE (Adjunctive Cilostazol Versus High Maintenance Dose Clopidogrel in Patients With Clopidogrel Resistance) randomized study. J Am Coll Cardiol. 2009;53:1101–1109. doi: 10.1016/j.jacc.2008.12.025. [DOI] [PubMed] [Google Scholar]
- 5.Kelm M. Flow-mediated dilatation in human circulation: diagnostic and therapeutic aspects. Am J Physiol Heart Circ Physiol. 2002;282:H1–H5. doi: 10.1152/ajpheart.2002.282.1.H1. [DOI] [PubMed] [Google Scholar]
- 6.Joannides R, Haefeli WE, Linder L, Richard V, Bakkali EH, Thuillez C, Luscher TF. Nitric oxide is responsible for flow-dependent dilatation of human peripheral conduit arteries in vivo. Circulation. 1995;91:1314–1319. doi: 10.1161/01.cir.91.5.1314. [DOI] [PubMed] [Google Scholar]
- 7.Wang T, Elam MB, Forbes WP, Zhong J, Nakajima K. Reduction of remnant lipoprotein cholesterol concentrations by cilostazol in patients with intermittent claudication. Atherosclerosis. 2003;171:337–342. doi: 10.1016/j.atherosclerosis.2003.08.017. [DOI] [PubMed] [Google Scholar]
- 8.Dawson DL, Cutler BS, Meissner MH, Strandness DE., Jr Cilostazol has beneficial effects in treatment of intermittent claudication: results from a multicenter, randomized, prospective, double-blind trial. Circulation. 1998;98:678–686. doi: 10.1161/01.cir.98.7.678. [DOI] [PubMed] [Google Scholar]
- 9.Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986;1:307–310. [PubMed] [Google Scholar]
- 10.Cooke JP, Tsao PS. Is NO an endogenous antiatherogenic molecule? Arterioscler Thromb. 1994;14:653–655. doi: 10.1161/01.atv.14.5.653. [DOI] [PubMed] [Google Scholar]
- 11.Vogel RA, Corretti MC, Plotnick GD. Effect of a single high-fat meal on endothelial function in healthy subjects. Am J Cardiol. 1997;79:350–354. doi: 10.1016/s0002-9149(96)00760-6. [DOI] [PubMed] [Google Scholar]
- 12.Ghiadoni L, Donald AE, Cropley M, Mullen MJ, Oakley G, Taylor M, O'Connor G, Betteridge J, Klein N, Steptoe A, Deanfield JE. Mental stress induces transient endothelial dysfunction in humans. Circulation. 2000;102:2473–2478. doi: 10.1161/01.cir.102.20.2473. [DOI] [PubMed] [Google Scholar]
- 13.Lekakis J, Papamichael C, Vemmos C, Nanas J, Kontoyannis D, Stamatelopoulos S, Moulopoulos S. Effect of acute cigarette smoking on endothelium-dependent brachial artery dilatation in healthy individuals. Am J Cardiol. 1997;79:529–531. doi: 10.1016/s0002-9149(96)00805-3. [DOI] [PubMed] [Google Scholar]
- 14.Kawano H, Motoyama T, Hirashima O, Hirai N, Miyao Y, Sakamoto T, Kugiyama K, Ogawa H, Yasue H. Hyperglycemia rapidly suppresses flow-mediated endothelium-dependent vasodilation of brachial artery. J Am Coll Cardiol. 1999;34:146–154. doi: 10.1016/s0735-1097(99)00168-0. [DOI] [PubMed] [Google Scholar]
- 15.Bevan JA. Flow regulation of vascular tone. Its sensitivity to changes in sodium and calcium. Hypertension. 1993;22:273–281. doi: 10.1161/01.hyp.22.3.273. [DOI] [PubMed] [Google Scholar]
- 16.Mombouli JV, Vanhoutte PM. Endothelial dysfunction: from physiology to therapy. J Mol Cell Cardiol. 1999;31:61–74. doi: 10.1006/jmcc.1998.0844. [DOI] [PubMed] [Google Scholar]
- 17.Lloyd-Jones D, Adams RJ, Brown TM, Carnethon M, Dai S, De Simone G, Ferguson TB, Ford E, Furie K, Gillespie C, Go A, Greenlund K, Haase N, Hailpern S, Ho PM, Howard V, Kissela B, Kittner S, Lackland D, Lisabeth L, Marelli A, McDermott MM, Meigs J, Mozaffarian D, Mussolino M, Nichol G, Roger VL, Rosamond W, Sacco R, Sorlie P, Thom T, Wasserthiel-Smoller S, Wong ND, Wylie-Rosett J. Heart disease and stroke statistics--2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–e215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 18.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years' observations on male British doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ambrose JA, Barua RS. The pathophysiology of cigarette smoking and cardiovascular disease: an update. J Am Coll Cardiol. 2004;43:1731–1737. doi: 10.1016/j.jacc.2003.12.047. [DOI] [PubMed] [Google Scholar]
- 20.Benowitz NL. Cigarette smoking and cardiovascular disease: pathophysiology and implications for treatment. Prog Cardiovasc Dis. 2003;46:91–111. doi: 10.1016/s0033-0620(03)00087-2. [DOI] [PubMed] [Google Scholar]
- 21.Hill JM, Zalos G, Halcox JP, Schenke WH, Waclawiw MA, Quyyumi AA, Finkel T. Circulating endothelial progenitor cells, vascular function, and cardiovascular risk. N Engl J Med. 2003;348:593–600. doi: 10.1056/NEJMoa022287. [DOI] [PubMed] [Google Scholar]
- 22.Hadi HA, Carr CS, Al Suwaidi J. Endothelial dysfunction: cardiovascular risk factors, therapy, and outcome. Vasc Health Risk Manag. 2005;1:183–198. [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson HM, Gossett LK, Piper ME, Aeschlimann SE, Korcarz CE, Baker TB, Fiore MC, Stein JH. Effects of smoking and smoking cessation on endothelial function: 1-year outcomes from a randomized clinical trial. J Am Coll Cardiol. 2010;55:1988–1995. doi: 10.1016/j.jacc.2010.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guthikonda S, Sinkey C, Barenz T, Haynes WG. Xanthine oxidase inhibition reverses endothelial dysfunction in heavy smokers. Circulation. 2003;107:416–421. doi: 10.1161/01.cir.0000046448.26751.58. [DOI] [PubMed] [Google Scholar]
- 25.Oida K, Ebata K, Kanehara H, Suzuki J, Miyamori I. Effect of cilostazol on impaired vasodilatory response of the brachial artery to ischemia in smokers. J Atheroscler Thromb. 2003;10:93–98. doi: 10.5551/jat.10.93. [DOI] [PubMed] [Google Scholar]
- 26.Yasuda K, Sakuma M, Tanabe T. Hemodynamic effect of cilostazol on increasing peripheral blood flow in arteriosclerosis obliterans. Arzneimittelforschung. 1985;35:1198–1200. [PubMed] [Google Scholar]
- 27.Hiatt WR. Medical treatment of peripheral arterial disease and claudication. N Engl J Med. 2001;344:1608–1621. doi: 10.1056/NEJM200105243442108. [DOI] [PubMed] [Google Scholar]
- 28.Lee SW, Park SW, Kim YH, Yun SC, Park DW, Lee CW, Hong MK, Kim HS, Ko JK, Park JH, Lee JH, Choi SW, Seong IW, Cho YH, Lee NH, Kim JH, Chun KJ, Park SJ. Drug-eluting stenting followed by cilostazol treatment reduces late restenosis in patients with diabetes mellitus the DECLARE-DIABETES Trial (A Randomized Comparison of Triple Antiplatelet Therapy with Dual Antiplatelet Therapy After Drug-Eluting Stent Implantation in Diabetic Patients) J Am Coll Cardiol. 2008;51:1181–1187. doi: 10.1016/j.jacc.2007.11.049. [DOI] [PubMed] [Google Scholar]
- 29.Ikeda U, Ikeda M, Kano S, Kanbe T, Shimada K. Effect of cilostazol, a cAMP phosphodiesterase inhibitor, on nitric oxide production by vascular smooth muscle cells. Eur J Pharmacol. 1996;314:197–202. doi: 10.1016/s0014-2999(96)00551-1. [DOI] [PubMed] [Google Scholar]
- 30.Nakamura T, Houchi H, Minami A, Sakamoto S, Tsuchiya K, Niwa Y, Minakuchi K, Nakaya Y. Endothelium-dependent relaxation by cilostazol, a phosphodiesteras III inhibitor, on rat thoracic aorta. Life Sci. 2001;69:1709–1715. doi: 10.1016/s0024-3205(01)01258-9. [DOI] [PubMed] [Google Scholar]