Abstract
We performed a percutaneous vertebroplasty at the compressed L2 vertebral body of a 73-year-old female using a left-sided unilateral extrapedicular approach. She complained severe radiating pain and a tingling sensation in her left leg two hours after the vertebroplasty. Spinal computed tomographic scan showed a large retroperitoneal hematoma, and a subsequent spinal angiography revealed a left L2 segmental artery injury. Bleeding was successfully controlled by endovascular embolization. Recently, extrapedicular approaches have been attempted, allowing for the avoidance of facet and pedicle injury with only a unilateral approach. With this approach, however, the needle punctures the vertebral body directly. Therefore, this procedure carries the potential risk of a spinal segmental artery.
Keywords: Compression fractures, Vascular injury, Vertebroplasty
INTRODUCTION
Percutaneous vertebroplasty is a safe and effective minimally invasive procedure used to treat symptomatic osteoporotic vertebral compression fracture, and it is usually performed using a transpedicular approach. Recently, extrapedicular approaches have been attempted, allowing for the avoidance of facet and pedicle injury with only a unilateral approach2,3,5). With this approach, however, the needle punctures the vertebral body directly and, therefore, may injure the nerve root sleeve or the segmental artery2,5). Here, we present a rare case of lumbar segmental artery injury following percutaneous vertebroplasty using the extrapedicular approach.
CASE REPORT
A 73-year-old woman presented with severe back pain after fall. Magnetic resonance imaging and radioisotope images revealed an acute L2 compression fracture. The T-score of her bone marrow densitometry was -3.3. Her back pain did not improve with conservative management, including bed rest and analgesics. We performed a percutaneous vertebroplasty with polymethylmethacrylate using a left-sided unilateral extrapedicular approach at the L2 vertebral body (Fig. 1).
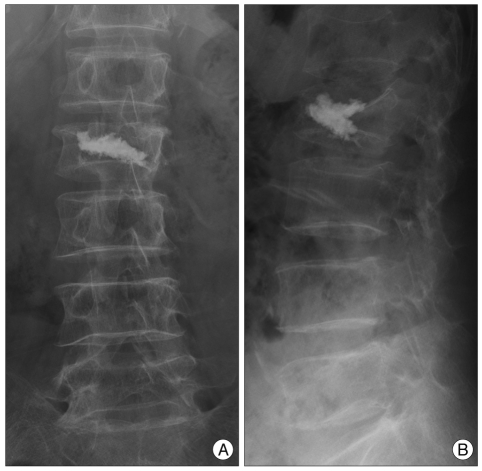
Fig. 1.
Immediate post-vertebroplasty X-ray films. A : Anterior-posterior. B : Lateral.
Her back pain was significantly improved after the vertebroplasty. However, severe radiating pain and a tingling sensation of the left leg developed two hours after vertebroplasty and became refractory to analgesics. Systolic blood pressure decreased from 130 mmHg to 95 mmHg six hours after vertebroplasty and was normalized by intravenous infusion. Computed tomographic (CT) scan one day post-operative showed a large retroperitoneal hematoma (Fig. 2), and we performed a conventional lumbar spinal angiography.
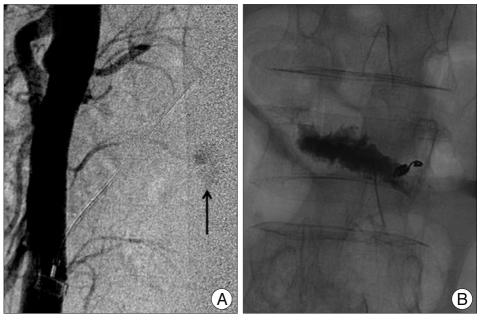
Fig. 2.
Computed tomographic scan showing a large retroperitoneal hematoma (arrows).
Angiogram revealed an extravasation of the distal part of the left L2 segmental artery (Fig. 3A). The injured L2 segmental artery was completely obliterated by endovascular embolization with micro-coil and Gelfoam (Fig. 3B). A subsequent abdominal CT scan taken ten days after the vertebroplasty showed a smaller retroperitoneal hematoma. At 40 days after vertebroplasty, we performed an ultrasound-guided aspiration of the retroperitoneal hematoma. A total of 500 mL of liquefied hematoma was aspirated. She was discharged without any problems.
Fig. 3.
A : Spinal angiography shows extravasation from the distal part of the left L2 segmental artery. B : X-ray film after endovascular embolization with micro-coil and Gelfoam.
DISCUSSION
Recently, percutaneous vertebroplasty or kyphoplasty using an extrapedicular approach has been attempted to treat osteoporotic vertebral compression fractures2,3,5). The extrapedicular approach can be applied to vertebrae with small pedicles, such as those of the upper thoracic levels, and uses a relatively large needle diameter compared to that used in the transpedicular approach. A bone marrow needle would not pass through the pedicle, so we used a larger diameter needle. This procedure allow for the injection of highly viscous filler material under lower pressure, which may prevent complications related to extravasation2,5). The tip of the bone marrow needle used in the extrapedicular approach can easily reach the center of the vertebral body; therefore, the extrapedicular approach may be used to inject sufficient filler material into the center portion of the vertebral body with only one-sided unilateral puncture2,5). Also, the extrapedicular approach can avoid the injury of facet joint and capsule.
However, the extrapedicular approach may result in an injury to a nerve root sleeve or a spinal segmental artery (Fig. 4). Nerve root injury can be easily monitored during vertebroplasty because percutaneous vertebroplasty is usually performed under local anesthesia and any neural irritation would present with radiating radicular pain. Therefore, a nerve root injury may be prevented during the procedure. However, we suggest that injury to the spinal segmental artery may be difficult to monitor and to detect during vertebroplasty. A lumbar segmental artery injury results in a retroperitoneal hematoma, which can induce irritation of the nerve root and may potentially lead to systemic hypovolemic shock1).
Fig. 4.
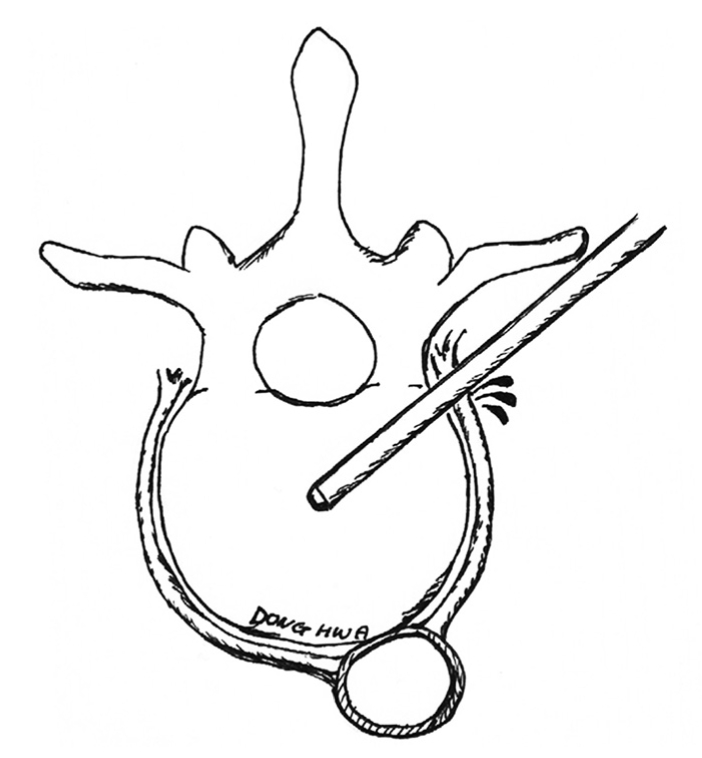
Schematic illustration of the possible mechanism of segmental artery injury during vertebroplasty using the extrapedicular approach.
This case involved a woman with severe radicular pain, a tingling sensation of the left leg, and hypotension. Such a presentation may be secondary to an injury of the segmental artery, and retroperitoneal hematoma should be thought be a possible cause. After vertebroplasty or kyphoplasty using an extrapedicular approach, we strongly suggest serial neurologic examinations along with vital sign monitoring. When such complication has occurred, early endovascular embolization and delayed aspiration of the liquefied hematoma are recommended. In such as case, if the systemic hypovolemic shock status is not corrected by intravenous infusion or endovascular embolization, direct surgical vessel ligation may be another treatment option. We believe that the determination of treatment modality, such as direct surgical vessel ligation, endovascular embolization, surgical removal of the hematoma, or needle aspiration of the hematoma, may be decided according to the patient's presentation1,4).
Recently, we have carried out a spinal CT angiography using intravenous injection of contrast media before vertebroplasty or kyphoplasty using the extrapedicular approach. In our experience, spinal CT angiography can clearly visualize the spinal segmental arteries, and most of the segmental arteries pass below midline of pedicle. Therefore, we believe that the safe puncture zone of extrapedicular vertebroplasty of lumbar vertebral bodies is slightly above the midline of pedicle. We suggest that three-dimensional reconstruction CT images of the spinal segmental artery may help in deciding the needle puncture site and also may help to avoid injury to the segmental artery during the procedure (Fig. 5).
Fig. 5.
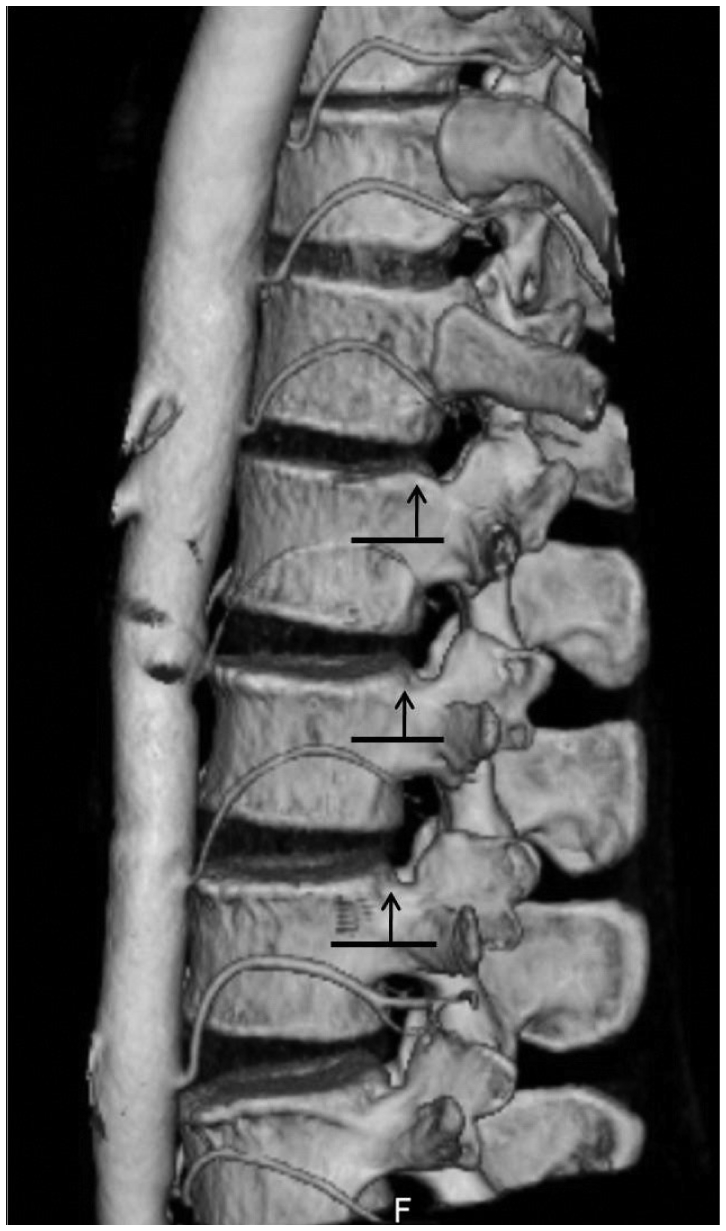
Three-dimensional reconstruction image of spinal segmental arteries using spinal computed tomographic angiography. The safe puncture zone of extrapedicular vertebroplasty of lumbar vertebral bodies is slightly above the midline of pedicle (arrows).
CONCLUSION
Although percutaneous vertebroplasty using an extrapedicular approach has several advantages over the transpedicular approach, this procedure carries the potential risk of a spinal segmental artery injury. Therefore, we suggest that the transpedicular vertebroplasty may be safer than the extrapedicular approach in lumbar area. Symptoms related to this injury include radicular leg pain and systolic hypotension. If injury to the spinal segmental artery is suspected, we recommend immediate evaluation with CT scan to confirm such complication. For the treatment, spinal segmental artery injury may be successfully controlled by endovascular embolization as in this case.
Acknowledgements
This study was supported by BioGreen21 Program (200810FTH010103002 and 200810FTH010102001) of Rural Development Administration.
References
- 1.Ahn Y, Kim JU, Lee BH, Lee SH, Park JD, Hong DH, et al. Postoperative retroperitoneal hematoma following transforaminal percutaneous endoscopic lumbar discectomy. J Neurosurg Spine. 2009;10:595–602. doi: 10.3171/2009.2.SPINE08227. [DOI] [PubMed] [Google Scholar]
- 2.Biafora SJ, Mardjetko SM, Bulter JP, McCarthy PL, Gleason TF. Arterial injury following percutaneous vertebral augmentation : a case report. Spine. 2006;31:E84–E87. doi: 10.1097/01.brs.0000197596.88416.02. [DOI] [PubMed] [Google Scholar]
- 3.Cho YJ, Choi JH, Cho SM. Vertebroplasty utilizing percutaneous vertebral body access (PVBA) technique for osteoporotic vertebral compression fractures in the middle thoracic vertebrae. J Korean Neurosurg Soc. 2007;41:161–165. [Google Scholar]
- 4.Han KR, Kim C, Eun JS, Chung YS. Extrapedicular approach of percutaneous vertebroplasty in the treatment of upper and mid-thoracic verte-bral compression fracture. Acta Radiol. 2005;46:280–287. doi: 10.1080/02841850510021058. [DOI] [PubMed] [Google Scholar]
- 5.Ryu KS, Park CK, Kim MK, Kim DH. Single balloon kyphoplasty using far-lateral extrapedicular approach : technical note and preliminary results. J Spinal Disord Tech. 2007;20:392–398. doi: 10.1097/BSD.0b013e31802da846. [DOI] [PubMed] [Google Scholar]