Abstract
Compression of the ulnar nerve in Guyon's canal can result from repeated blunt trauma, fracture of the hamate's hook, and arterial thrombosis or aneurysm. In addition, conditions such as ganglia, rheumatoid arthritis and ulnar artery disease can rapidly compress the ulnar nerve in Guyon's canal. A ganglion cyst can acutely protrude or grow, which also might compress the ulnar nerve. So, clinicians should consider a ganglion cyst in Guyon's canal as a possible underlying cause of ulnar nerve compression in patients with a sudden decrease in hand strength. We believe that early decompression with removal of the ganglion is very important to promote complete recovery.
Keywords: Guyon's canal, Ganglion cyst, Compression
INTRODUCTION
Ulnar nerve compression in Guyon's canal is rare, and that caused by a ganglion cyst is extremely rare3). The etiology of compression in Guyon's canal includes repetitive trauma, tumors such as ganglions and lipomas, pisiform instability, and pisotriquentrial arthritis, to name a few3). In case of a sudden decrease of strength or sensory loss in the hand, understanding the possible cause and performing a proper examination are important.
We report herein a patient who rapidly lost strength in her hand as a result of ulnar nerve compression in Guyon's canal caused by a ganglion cyst.
CASE REPORT
The patient was a 54-year-old female who had felt a progressive loss of strength in her left, non-dominant hand for a month. She had no history of trauma but physical examination found that her fifth finger and hypothenar muscle showed atrophy.
According to the examination, her hypothenar muscle was weak (grade 4 power) and she had sensory deficits in the palmar surfaces of her hypothenal eminence and fourth and fifth digits. However, there was no palpable mass.
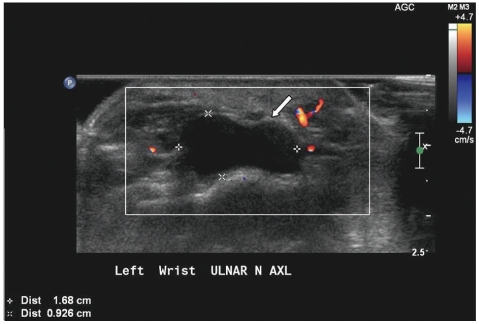
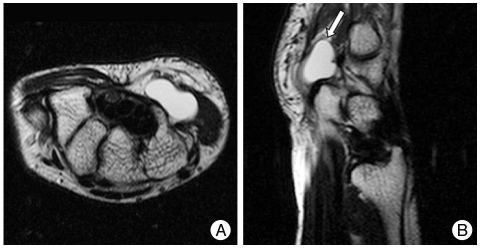
Cervical spine magnetic resonance image (MRI), electromyography (EMG) and nerve conduction velocity (NCV) tests were performed. C-spine MRI showed neither cervical disc protrusion nor nerve canal stenosis, but EMG showed abnormal spontaneous activities in the left first dorsal interossei and abductor digiti minimi muscles. Then, because the motor weakness had progressed rapidly and the lesion was peripheral, we performed wrist sonography, which showed about a 17×13×10 mm ganglion between the ulnar nerve and wrist joint (Fig. 1). To reveal the relationships between the ganglion and other structures, we performed wrist MRI, which showed a ganglion cyst in Guyon's canal between the ulnar nerve and the wrist joint in the volar aspect of the left wrist (Fig. 2).
Fig. 1.
Left wrist ultrasonography shows a ganglion cyst (white arrow).
Fig. 2.
T2-weighted magnetic resonance image reveals a high-intensity mass in Guyon's canal. A : Axial views. B : Sagittal views.
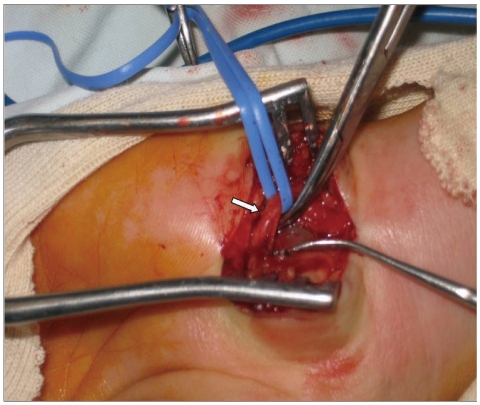
The patient was taken to the operating room and her ulnar nerve was exposed through an incision over Guyon's canal. The ulnar nerve and artery were identified proximally to the wrist. The transverse reticulum was released to expose the volar ganglion, which was compressing the ulnar nerve (Fig. 3). As a result, Guyon's canal was decompressed, and the ganglion was excised during surgery.
Fig. 3.
Intraoperative view of the ganglion cyst compressing the ulnar nerve. The arrow indicates the ulnar nerve.
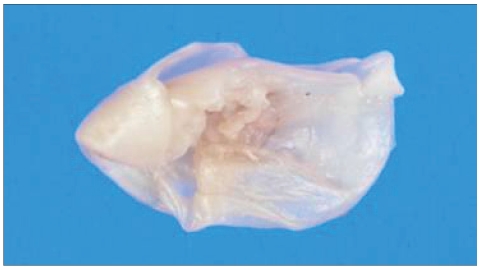
The patient noted prompt recovery with no specific problems during two postoperative weeks. She regained normal strength and function and had no pain. The biopsy showed that the soft tissue removed from her left hand was a ganglion cyst (Fig. 4).
Fig. 4.
Gross finding of ganglion cyst.
DISCUSSION
Ulnar nerve entrapment at the elbow is the second most common nerve entrapment syndrome of the upper extremity. But, ulnar nerve entrapment at the wrist is a rare pathologic condition, because this is only 5% as high as the incidence of ulnar nerve entrapment at the elbow.
Guyon's canal, or the ulnar-carpal canal, is bounded proximally and medially by the pisiform bone and laterally and distally by the hamate's hook. The canal's floor is formed by the transverse carpal ligament and its roof is formed by the volar carpal ligament5). At the distal end of the canal's floor is the pisohamate hiatus, which is bounded superiorly by a concave musculotendinous arch and below by the pisohamate ligament8).
Within Guyon's canal lie the ulnar artery and nerve. The nerve is divided into a superficial branch, which is sensory to the little finger's palmar surface and the ring finger's ulnar side, and is motor to the palmaris brevis muscle, and a deep motor branch, which innervates the hypothenar muscles and then passes through the pisohamate hiatus to innervate the third and fourth lumbricals, the interossei, the adductor pollicis, and the deep head of the flexor pollicis brevis muscles.
Distal ulnar nerve lesions are classified into one of three categories1). Type I syndrome includes motor weakness of all ulnar-innervated muscles in the hand and a sensory deficit in the palmar surfaces of the hypothenar eminence and the fourth and fifth digits. Sensation over the hand's dorsum is unaffected. This syndrome is caused by a lesion in the proximal part of Guyon's canal. Type II syndrome, which is the most common, spares sensation but weakens the muscles innervated by the ulnar nerve's deep branch. The lesion is at the pisohamate hiatus or a more distal location, and the number of muscles involved depends on the compression site along the deep branch. Type III syndrome involves a purely volar sensory deficit without motor findings and is caused by a pathology that affects only the superficial sensory branch in the canal's most distal part. Our case is Type I by this classification.
As mentioned above, repeated blunt trauma, fractures of the hamate's hook, and arterial thrombosis or aneurysm can compress the ulnar nerve in Guyon's canal. Cases of ulnar nerve compression in Guyon's canal caused by an arteriovenous malformation also have been reported4). The presence of ganglion has been cited as the most common cause of this syndrome.
Ganglion cysts in the hand occur most frequently during the second through fourth decades of life, and affect women more often than men. Patients often present with a history of an asymptomatic mass that has been present for a period of months or years6). Many patients report that the mass fluctuates in size, growing after periods of increased activity and shrinking with inactivity. These masses can develop suddenly or gradually, and can disappear as fast as they arise7). A history of trauma is usually absent. Ganglion cysts can rupture or disappear spontaneously6). Many patients seek a physician's advice because of their cyst's cosmetic appearance or because they are concerned about malignant growth possibilities9).
Our patient had suffered from compression in Guyon's canal for a month. Interestingly, she had a sudden onset of symptoms and progressive loss of strength in her hand. There were many other possible causes including ganglia, rheumatoid arthritis, ulnar artery disease, and others. But, it is most likely that acute protrusion or growth of the ganglion cyst, which wrist movements might have provoked, accounted for the compression of her ulnar nerve's branch. Laboratory tests and radiographs enable us to differentiate a ganglion cyst from other possible causes2).
In our patient, cervical MRI, wrist sonography, and EMG/NCV studies were done. Clinical examination and nerve conduction showed the exact location of cyst, and surgical decompression of Guyon's canal led to a complete recovery.
CONCLUSION
Ulnar nerve compression by a ganglion cyst in Guyon's canal with a sudden decrease in hand strength is extremely rare. However in such clinical setting, clinicians should consider a ganglion cyst in Guyon's canal as the possible underlying cause of compression. We believe that early decompression with removal of the ganglion is an important step toward a complete recovery.
References
- 1.Duggal A, Anastakis DJ, Salonen D, Becker E. Compression of the deep palmar branch of the ulnar nerve by a ganglion : a case report. Hand (N Y) 2006;1:98–101. doi: 10.1007/s11552-006-9008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Erkin G, Uysal H, Keleş I, Aybay C, Ozel S. Acute ulnar neuropathy at the wrist : a case report and review of the literature. Rheumatol Int. 2006;27:191–196. doi: 10.1007/s00296-006-0166-8. [DOI] [PubMed] [Google Scholar]
- 3.Inaparthy PK, Anwar F, Botchu R, Jähnich H, Katchburian MV. Compression of the deep branch of the ulnar nerve in Guyon's canal by a ganglion : two cases. Arch Orthop Trauma Surg. 2008;128:641–643. doi: 10.1007/s00402-008-0636-4. [DOI] [PubMed] [Google Scholar]
- 4.Kim SS, Kim JH, Kang HI, Lee SJ. Ulnar nerve compression at Guyon's canal by an arteriovenous malformation. J Korean Neurosurg Soc. 2009;45:57–59. doi: 10.3340/jkns.2009.45.1.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kleinert HE, Hayes JE. The ulnar tunnel syndrome. Plast Reconstr Surg. 1971;47:21–24. doi: 10.1097/00006534-197101000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Nahra ME, Bucchieri JS. Ganglion cysts and other tumor related conditions of the hand and wrist. Hand Clin. 2004;20:249–260. v. doi: 10.1016/j.hcl.2004.03.015. [DOI] [PubMed] [Google Scholar]
- 7.Thommasen HV, Johnston S, Thommasen A. Management of the occasional wrist ganglion. Can J Rural Med. 2006;11:51–52. [PubMed] [Google Scholar]
- 8.Uriburu IJ, Morchio FJ, Marin JC. Compression syndrome of the deep motor branch of the ulnar nerve. (Piso-Hamate Hiatus syndrome) J Bone Joint Surg Am. 1976;58:145–147. [PubMed] [Google Scholar]
- 9.Westbrook AP, Stephen AB, Oni J, Davis TR. Ganglia : the patient's perception. J Hand Surg Br. 2000;25:566–567. doi: 10.1054/jhsb.2000.0504. [DOI] [PubMed] [Google Scholar]