Abstract
Background and Objectives
Transradial coronary angiography and intervention are increasing in frequency due to lower major vascular access site complications and the potential for early mobilization. However, the small size of the radial artery (RA) is a major limitation of this technique. A sheathless guiding catheter (GC) has recently been introduced that has a 1-2 French smaller diameter compared with the corresponding introducer sheath. This catheter also has a hydrophilic coating along its entire length. We evaluated the feasibility of using a sheathless GC in patients who have small radial arteries.
Subjects and Methods
The procedural results were evaluated in patients with small radial arteries (diameter <2.3 mm) who underwent transradial coronary intervention using a sheathless GC.
Results
A total of 25 (male: 9) patients with 29 lesions were enrolled. The mean RA diameter was 1.81±0.26 mm. 44% of the patients had stable angina and 50.0% had acute coronary syndrome. The procedural success rate was 93.1%. Two patients (6.9%) had chronic total occlusive lesions that could not be crossed with a guide-wire despite good guiding support. An intravascular ultrasound could be used for all of the treated lesions. Multi-vessel intervention was performed in 29.2% of the patients. Two bifurcated lesions were treated with a kissing balloon technique, and one with a modified T-stenting technique. No catheter related complications were reported.
Conclusion
The use of a sheathless GC is feasible in patients with small radial arteries without catheter related complications.
Keywords: Coronary intervention, Radial artery, Vascular access
Introduction
The use of transradial coronary angiography and intervention (TRI) is increasing because of its low rates of major vascular access-related complications and the potential for early mobilization.1),2) A large-bore guiding catheter (GC) with a large-bore introducer sheath is needed in patients with complex lesions, but they cannot be used in patients with a small radial artery (RA) because they can cause forearm discomfort and RA spasm and occlusion,3) which are significant limitations to the transradial approach. To conquer this limitation, GC that does not require an introducer sheath has been developed.
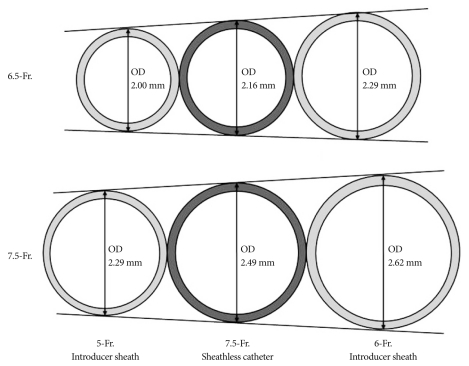
The sheathless GC system (Sheathless Eaucath, Asahi Intecc®, Japan) consists of a hydrophilic GC and a central dilator. This system can be used to insert the GC into the RA without the use of an introducer sheath. The outer diameter of the 6.5 French (Fr.) sheathless GC (2.16 mm) is smaller than a 5 Fr. introducer sheath (2.29 mm). The outer diameter of the 7.5 Fr. sheathless GC (2.49 mm) is also less than that of a 6 Fr. introducer sheath (2.62 mm) (Fig. 1). With this feature, the sheathless GC system enables performance of TRI even in patients with small RAs. Furthermore, the hydrophilic coating that is present along the entire length of the GC may be helpful in reducing radial pain and RA spasm.
Fig. 1.
Comparison of outer diameter (OD) between introducer sheath and sheathless guiding catheter (GC) (illustrated by author referred to SheathLess Eaucath® information brochure).
Here, we evaluated the feasibility of coronary intervention using the sheathless GC in patients with small RAs.
Subjects and Methods
Study population
A total of 36 patients with 60 lesions were enrolled in this study. The patients underwent TRI using a 6.5 or 7.5 Fr. sheathless GC at Wonju Christian Hospital from January 2009 to December 2009. All patients underwent diagnostic coronary angiography using a 5 Fr. conventional catheter through a 5 Fr. introducer sheath. Patients who required primary percutaneous coronary intervention (PCI) were excluded because preparation of a sheathless GC that is composed of two pieces (a catheter and a central dilator) requires more time than a conventional one-piece GC. All procedures were performed in the left RA unless the patient had a history of previous angiography through the right RA. All patients signed informed consent forms for participation in this study.
Antiplatelet and anticoagulation therapy
A loading dose of 600 mg clopidogrel and 300 mg aspirin was given to all patients at least three hours before the procedure. We administered 5,000 units of heparin through the RA after insertion of the 5 Fr. introducer sheath. An additional dose of 5,000 units heparin was given through the same route before PCI. Glycoprotein IIb/IIIa inhibitor was used at the operator discretion.
Radial artery puncture and radial artery diameter measurement
The RA was punctured using a 20-G venous needle at a point 5-10 mm proximal to the styloid process after subcutaneous infiltration with 0.6 mL of 2% lidocaine. A 5 Fr. introducer sheath (Terumo Company, Japan) was inserted into the RA. Normal saline (10 mL) with 200 µg of nitroglycerine was injected into the RA through the introducer sheath to prevent RA spasm. Angiography of the RA was performed after injection of normal saline (10 mL) with 200 µg of nitroglycerine. A 30- to 40-mm long segment of RA from the tip of the introducer sheath was selected for the determination of the mean diameter. The mean of the maximal and minimal diameter of the selected segment of RA was used to determine the size of the RA using a computer-assisted quantification method (GE®, US). Because the outer diameter of the 5 Fr. introducer sheath was approximately 2.3 mm in diameter, a small RA was defined as a diameter ≤2.3 mm.
Sheathless guiding catheter engagement
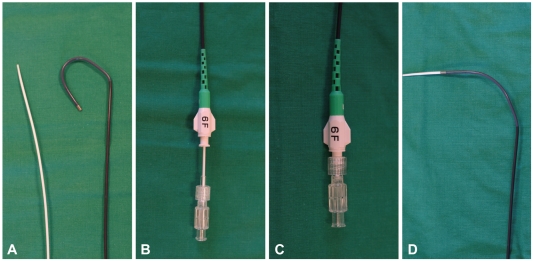
After the diagnostic angiography, the sheath was exchanged for the sheathless catheter over a standard 150 cm J-tipped 0.035-inch (Terumo®, Japan) wire. The shape and size of the sheathless GC was selected at the operator discretion. The sheathless GC was composed of two parts: a hydrophilic catheter and a central dilator. The central dilator was inserted into the catheter and locked in place (Fig. 2). The sheathless GC with the central dilator was advanced along the 0.035-inch wire to the proximal ascending thoracic aorta. The central dilator and 0.035-inch wire were then removed. The ostium of the selected coronary artery was engaged by the GC and PCI was performed.
Fig. 2.
The sheathless GC system (sheathless Eaucath, Asahi Intecc®, Japan). A: 6.5 Fr. hydrophilic GC illustrated with central dilator. B and C: Central dilator was inserted into GC and locked. D: GC with central dilator can be advanced along the 0.035" wire. GC: guiding catheter.
Definition of success
We defined procedural success as the successful implantation of stent(s) with final thrombolysis in myocardial infarction flow grade 3 and residual stenosis <30%, despite the selection of the GC.
Measurement of complications
Dissections of coronary artery and aorta were evaluated by coronary angiography during the procedure. Forearm pain during the procedure was documented when the patient complained of forearm pain. Presence of hematoma or bleeding at access site was evaluated during the admission period. RA occlusion was defined as absence of a RA pulse by clinical assessment.
Statistical analysis
Categorical variables were expressed as proportions while continuous variables were expressed as mean±standard deviation.
Results
A total of 25 patients (29 lesions) with a small RA who underwent PCI using a sheathless GC were included in this study.
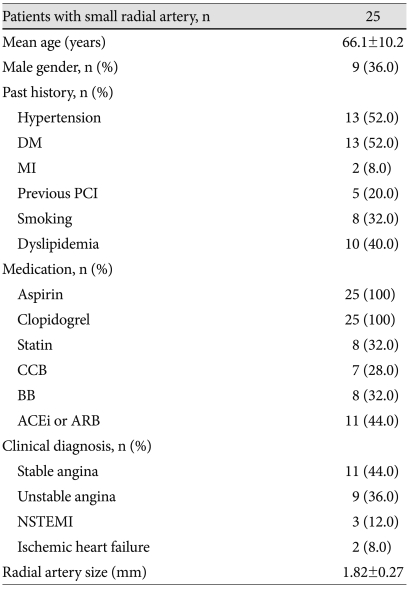
The mean age was 66.1±10.2 years, and nine (36.0%) patients were men. Approximately half of the patients had a history of hypertension (52.0%) and diabetes mellitus (52.0%). Eleven (44.0%) patients had stable angina, 12 (48.0%) had acute coronary syndrome, and two (8.0%) had ischemic heart failure. The mean RA size was 1.82±0.27 mm. Baseline characteristics are presented in Table 1.
Table 1.
Baseline characteristics
DM: diabetes mellitus, MI: myocardial infarction, CCB: calcium channel blocker, BB: beta-blocker, ACEi: angiotensin converting enzyme inhibitor, ARB: angiotensin II receptor blocker, NSTEMI: non-ST-segment elevation myocardial infarction
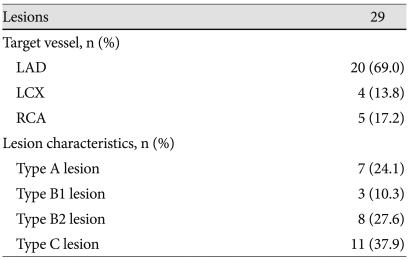
Twenty (69.0%) lesions were located in the left anterior descending (LAD) coronary artery. According to the modified American College of Cardiology/American Heart Association criteria, most of the lesions were type B2 (27.6%) or C (37.9%). Angiographic characteristics are presented in Table 2.
Table 2.
Angiographic characteristics
LAD: left anterior descending, LCX: left circumflex, RCA: right coronary artery
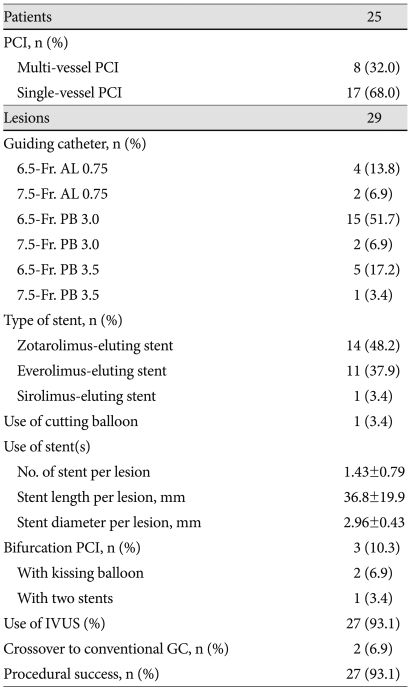
Eight (32.0%) patients underwent multi-vessel PCI. A 6.5 Fr. Power Backup (PB) 3 cm sheathless GC was used in approximately half of the cases (51.7%). Most of the lesions were implanted with a zotarolimus-eluting stent(s) (48.2%) or everolimus-eluting stent(s) (37.9%). One lesion consisting of restenosis of a previously implanted drug-eluting stent was treated using balloon angioplasty with a cutting balloon. The mean number of stents implanted at one lesion was 1.43±0.79. The mean total length of the stents was 36.8±19.9 mm and the mean diameter was 2.96±0.43 mm. Two of three bifurcated lesions were treated with a kissing balloon technique and one lesion was treated with two stents by using a modified T-stenting technique. All PCIs were performed under intravascular ultrasound guidance. Two of the successfully treated lesions required conversion to a conventional GC after insertion of the 6 Fr. introducer sheath. One lesion tried with a 6.5 Fr. PB 3.0 sheathless GC in the LAD was treated by conversion to 6 Fr. Extra Backup 3.5 GC. The other lesion tried with 6.5 Fr. Amplatz Left (AL) 0.75 sheathless GC in the right coronary artery (RCA) was treated by conversion to 6 Fr. Judkins Right 3.5 GC. These two sheathless GCs did not engage the coronary arteries and provided poor guiding support; however, the main reason for conversion to a conventional GC was a limitation in GC shape selection. There were no problems using the 6 Fr introducer sheath in these two patients. Twenty seven of 29 (93.1%) lesions were therefore successfully treated. The two failed lesions were chronic total occlusions (CTO) in the LAD that could not be crossed with a guidewire supported by a microcatheter. The procedural results are presented in Table 3.
Table 3.
Procedural results
AL: amplatz left, PB: power backup, No.: number, PCI: percutaneous coronary intervention, IVUS: intravascular ultrasound, GC: guiding catheter
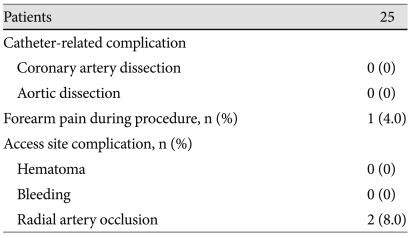
There were no catheter-related complications. Only one patient, who developed RA spasm during coronary angiography using a conventional 5 Fr catheter, complained of forearm pain during PCI. Although there was no immediate access site complication including hematoma and bleeding, two patients lost pulse in the RA used as the access site without hand ischemia during a median 357 (140-432) days of follow-up. The procedural complications are presented in Table 4.
Table 4.
Complications
Discussion
Our study shows the feasibility of TRI using a sheathless GC in 25 consecutive patients (29 lesions) with small RAs (diameter ≤2.3 mm).
The procedural success rate of TRI is comparable to that of transfemoral coronary intervention with the benefit of lower rates of bleeding and fewer vascular complications.1),2) However, a larger GC and introducer sheath cannot be used in some patients because of the small diameter of their RA. Saito et al.3) demonstrated that the RAs were smaller than the outer diameter of a 6 Fr. introducer sheath in 14.3% of males and 27.4% of females. They also reported that when the ratio of the RA inner diameter to the cannulated sheath outer diameter was less than 1.0, the incidence of flow reduction was increased. They therefore suggested that smaller catheters should be considered to prevent RA occlusions or narrowing.
With the sheathless GC system, one can use the larger-bore GC in patients with a small RA without using an introducer sheath and thereby minimizing radial discomfort.4) Yoo et al.5) have shown that the mean RA diameter measured by ultrasound was 2.66±0.44 mm (male: 2.69±0.40 mm, female: 2.43±0.38 mm) in Korean patients. Although direct comparison is difficult because we did not use ultrasound to measure RA diameter, the mean diameter of the RA in our study was 1.82±0.27 mm, which is smaller than the mean RA diameter in Korean patients and smaller than the outer diameter of the sheathless GC. Despite this finding, only one patient complained of forearm pain, namely discomfort during PCI. This patient developed severe RA spasm before using the sheathless GC and the operator has difficulty in performing diagnostic coronary angiography with the conventional 5 Fr. catheter. However, the operator did not experience any difficulty in manipulating the catheter during PCI.
Despite the above-mentioned results, a disadvantage in using a sheathless GC was noted. Because sheathless GCs slide easily within vessels due to the hydrophilic coating, disengagement of the catheter could happen in cases requiring good guiding support. In our study, the sheathless GC frequently slipped away from the ostium in two cases of RCA intervention, despite the small size of the RA. Mamas et al.6) fixed the sheathless GC to the forearm at the point of entry to the RA using a Tegaderm adhesive dressing to avoid slippage during the procedure. Even if this solution could be helpful in preventing the slippage of GC, it could also be very dangerous if the patient were to move unconsciously as it may result in an aortic or coronary dissection.
Two studies have reported successful use of a sheathless GC in complex interventions with large bore catheters including rotablation, crush stent bifurcation lesions, 7 Fr. proximal protection, thrombectomy devices, and simultaneous kissing stenting.7),8) In our study, we successfully performed three complex procedures including two in which the kissing balloon technique was used and one in which the modified T-stenting technique was used. These results suggest that other complex procedures may also be performed using sheathless GCs. Most recently, Mamas et al.6) reported a 100% procedural success using the sheathless GC in 100 patients. They included patients requiring primary PCI. The primary difference in our study is that we enrolled only patients with small radial arteries, because the use of a sheathless GC is more beneficial for these patients.
Although we failed to treat two cases of CTO lesions which required catheter conversion from sheathless to conventional, these results were not due to the GC itself but to limitations in GC selection with different shapes. Only AL, PB, Hotkey stick, and Judkins Left GCs were available at our institute, and the shapes of catheters were slightly different from those of conventional catheters.
During a median 357 days of follow-up, two patients (8%) developed RA occlusion, and this is consistent with a previous report of an asymptomatic RA occlusion rate of 5-10%.9) Because the outer diameter of the sheathless GC is smaller than that of the conventional GC, we expected a lower incidence of RA occlusion, and our results may be related to the fact that we included only patients with small RAs and some of the patients had a RA with a diameter smaller than the outer diameter of sheathless GCs. Even though the sheathless GC could be beneficial in forearm pain, the risk of RA occlusion should be considered in treating patients with small RAs.
We did not use the sheathless GC during the primary PCI in our study. Although the use of the sheathless GC is feasible in cases of primary PCI, this system requires more time to assemble because it is composed of two parts, and the introducer sheath must be removed before inserting it. We usually use a 6 Fr. introducer sheath from the beginning in cases of primary PCI via a transradial approach.
Our study has some limitations. First, although we measured the diameter of the RA by angiography after using a vasodilator, this intervention could not completely prevent vasospasm. This fact could result in a smaller RA diameter than the diameter measured by non-invasive methods such as ultrasound. Second, we documented the presence of forearm pain only when the patient complained of forearm pain and did not use a pain scale such as the visual analogue scale or the 4-category verbal rating scale. Finally, this was not a randomized trial to compare the sheathless GC with the conventional GC.
Conclusion
The use of a sheathless GC was feasible in almost clinical settings for patients with small RAs regardless of complexity or severity of the lesion. However, disengagement of the GC and limitations in the setting of primary PCI should be taken into account.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Jolly SS, Amlani S, Hamon M, Yusuf S, Mehta SR. Radial versus femoral access for coronary angiography or intervention and the impact on major bleeding and ischemic events: a systematic review and meta-analysis of randomized trials. Am Heart J. 2009;157:132–140. doi: 10.1016/j.ahj.2008.08.023. [DOI] [PubMed] [Google Scholar]
- 2.Agostoni P, Biondi-Zoccai GG, de Benedictis ML, et al. Radial versus femoral approach for percutaneous coronary diagnostic and interventional procedures: systematic overview and interventional procedures. J Am Coll Cardiol. 2004;44:349–356. doi: 10.1016/j.jacc.2004.04.034. [DOI] [PubMed] [Google Scholar]
- 3.Saito S, Ikei H, Hosokawa G, Tanaka S. Influence of the ratio between radial artery inner diameter and sheath outer diameter on radial artery flow after transradial coronary intervention. Catheter Cardiovasc Interv. 1999;46:173–178. doi: 10.1002/(SICI)1522-726X(199902)46:2<173::AID-CCD12>3.0.CO;2-4. [DOI] [PubMed] [Google Scholar]
- 4.Kiemeneij F, Fraser D, Slagboom T, Laarman G, van der Wieken R. Hydrophilic coating aids radial sheath withdrawal and reduces patient discomfort following transradial coronary intervention: a randomized double-blind comparison of coated and uncoated sheaths. Catheter Cardiovasc Interv. 2003;59:161–164. doi: 10.1002/ccd.10444. [DOI] [PubMed] [Google Scholar]
- 5.Yoo BS, Lee HH, Yoon J, et al. The study of branching anomaly and tortuosity of radial artery for trans-radial coronary procedure. Korean Circ J. 2000;30:82–89. [Google Scholar]
- 6.Mamas M, D'Souza S, Hendry C, et al. Use of the sheathless guide catheter during routine transradial percutaneous coronary intervention: a feasibility study. Catheter Cardiovasc Interv. 2010;75:596–602. doi: 10.1002/ccd.22246. [DOI] [PubMed] [Google Scholar]
- 7.Mamas MA, Fath-Ordoubadi F, Fraser DG. Atraumatic complex transradial intervention using large bore sheathless guide catheter. Catheter Cardiovasc Interv. 2008;72:357–364. doi: 10.1002/ccd.21637. [DOI] [PubMed] [Google Scholar]
- 8.Liang M, Puri A, Linder R. Transradial simultaneous kissing stenting (SKS) with SheathLess access. Catheter Cardiovasc Interv. 2010;75:222–224. doi: 10.1002/ccd.22236. [DOI] [PubMed] [Google Scholar]
- 9.Cubero JM, Lombardo J, Pedrosa C, et al. Radial compression guided by mean artery pressure versus standard compression with a pneumatic device (RACOMAP) Catheter Cardiovasc Interv. 2009;73:467–472. doi: 10.1002/ccd.21900. [DOI] [PubMed] [Google Scholar]