Abstract
Background and Purpose
Amyotrophic lateral sclerosis (ALS) patients display easy fatigability and abnormal decrements on repetitive nerve stimulation (RNS) test of clinically involved limb muscles, which can result in ALS being misdiagnosed as myasthenia gravis. We retrospectively analyzed the RNS tests of ten ALS patients with only or predominant oropharyngeal symptoms without ocular or facial weakness.
Methods
RNS tests were performed on the abductor digiti quinti, flexor carpi ulnaris, orbicularis oculi (OO), nasalis and trapezius muscles at low-rate stimulation frequencies of 3 and 5-Hz. Decrements greater than 10% of the compound muscle action potential amplitude on the fifth stimulation compared to the first was regarded as abnormal.
Results
Six patients complained of muscular fatigue or diurnal fluctuation. Among the ten patients, three exhibited abnormal decrements during low-rate stimulation in the facial muscles but not in the limb muscles, two exhibited abnormal decrements in the OO and nasalis muscles, and one exhibited abnormal decrements in the OO muscle.
Conclusions
These findings show that the facial muscles may be involved in some early oropharyngeal forms of ALS, although facial weakness may not be clinically evident. We confirm herein that abnormal decrement of facial muscles to RNS test cannot make a definite diagnose for myasthenia gravis.
Keywords: amyotrophic lateral sclerosis, repetitive nerve stimulation test, facial muscles
Introduction
Repetitive nerve stimulation (RNS) test is fundamentally an electrophysiologic study for the differential diagnosis of neuromuscular junction (NMJ) disorders, although there are considerable limitations in its diagnostic sensitivity and specificity. Amyotrophic lateral sclerosis (ALS) is occasionally misdiagnosed as myasthenia gravis (MG), showing prominent bulbar muscle weakness without definite atrophy of the limb muscles, or fasciculation. Although ALS is not primarily a disease of the NMJ, there have been several reports of fatigable weakness and RNS abnormalities, especially of clinically involved muscles.1-6 Significant decrements in the facial muscles such as the orbicularis oculi (OO) or nasalis (NA) muscles have only rarely been reported in ALS patients.7
The clinical significance of the RNS test was determined in this study by retrospectively analyzing the RNS tests of ALS patients with only or predominant oropharyngeal manifestations.
Methods
The data of ten patients were analyzed after the diagnosis of ALS was established. They visited the electrophysiology laboratory in the Department of Neurology at Sinchon Severance hospital with predominant oropharyngeal symptoms between January 1997 and December 2008. The serum titer of acetylcholine receptor antibody was measured in five patients. The diagnosis of ALS was confirmed by the clinical course and follow-up electrophysiologic studies.
RNS test was performed on the facial nerve with a recording electrode over the OO and NA muscles, on the spinal accessory nerve with a recording electrode over the upper trapezius muscle, and on the ulnar nerve with the recording electrode over the flexor carpi ulnaris and abductor digiti quinti muscles, using the belly-tendon method. The changes in compound muscle action potential (CMAP) amplitude followed by 3- and 5-Hz supramaximal low-rate stimulation (LRS) were analyzed. For each train of repetitive stimuli, the amplitudes of the first and fifth CMAPs were compared, and the resulting decrement of the latter (if present) is expressed as a percentage. Decrements greater than 10% were considered as abnormal according to the guidelines of American Academy of Emergency Medicine Quality Assurance committee.8
Results
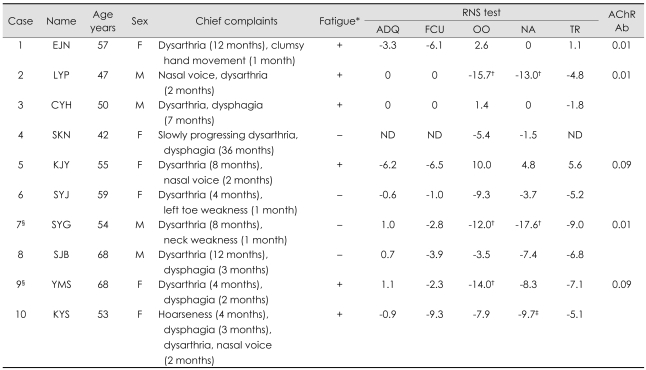
Six of the ten patients were women and their mean age was 55.3 years (range: 42-68 years). The mean duration of symptoms was 9.7 months (range: 2-36 months). All of the patients complained of only or predominant oropharyngeal symptoms including dysarthria, dysphagia and/or nasal voice. In addition to these oropharyngeal symptoms, one patient (case 1) complained of intermittent clumsiness of both hands of 1-month duration, and another (case 7) had experienced difficulty elevating the head for 1 month. None of the patients showed any clinical evidence of facial muscle weakness, ptosis or diplopia. Six patients complained of muscular fatigue or diurnal fluctuation, and two patients (cases 7 and 9) had been previously diagnosed and treated for MG (Table 1).
Table 1.
Summary of clinical manifestations and findings of repetitive nerve stimulation (RNS) tests. A negative RNS test finding represents a decrement
*+: Present, -: Absent, †Abnormal decrement greater than 10% on RNS test, ‡Borderline abnormal decrement on RNS test, §Previously diagnosed and treated for MG.
AChR Ab: acetylcholine receptor antibody, ADQ: abductor digiti quinti muscle, F: female, FCU: flexor carpi ulnaris muscle, M: male, NA: nasalis muscle, ND: no discharge, OO: orbicularis oculi muscle, TR: trapezius muscle.
Abnormal decrements during 3-Hz LRS on more than one facial muscle were noted in three patients (30.0%): in two patients (cases 2 and 7) in both the OO and NA, and in one (case 9) in the OO. Borderline decrements (9.7%) during 5-Hz LRS were recorded in the NA in one other patient (case 10). None of the patients showed any abnormal decrements in the limb muscles.
Discussion
While the clinical course is very important for the differential diagnosis of ALS and MG, the pharmacologic response to anticholinesterase, the determination of anti-acetylcholine receptor antibody titer and electrophysiologic studies including the RNS test are the main ways of ensuring a differential diagnosis.
There are several reports of significant decrements on RNS test of involved limb muscles in ALS.1-6 Denys et al.2 proposed a relationship between muscle atrophy and decremental responses. However, Bernstein et al.3 reported that disease activity and speed of progression might be more important factors for these findings. Restivo et al.7 reported significant decrements in facial muscles in one ALS patient, but this case seem-ed to be a true MG patient with ALS, as evidenced by seropositivity and abnormal decrements in the deltoid muscle.
Abnormal decrements on RNS test suggest the presence of instability of neuromuscular transmission in ALS. The underlying pathogenesis of NMJ instability remains unclear, but the following hypotheses have been proposed. First, motor neuron death causes enlargement of the motor unit territory by collateral sprouting, leading to a reduced safety factor for the NMJ in re-innervated end plates.2,3,5 Second, neuronal degeneration in ALS might disturb axonal transport of the synthetic enzyme choline acetyltransferase.1,3 Third, pathologic changes occur in the NMJ in ALS, as identified in a few muscle biopsies and animal studies.2,9-11
Our results suggest that the facial muscles are involved in some ALS patients with prominent oropharyngeal symptoms, although facial weakness may not be clinically evident. It is understandable that abnormal decremental responses were not recorded in the flexor carpi ulnaris, abductor digiti quinti, and trapezius muscles, because these muscles were not involved at the time of RNS tests. We believe that our patients are not true MG cases because of their seronegativity for MG and poor response to anticholinesterase treatment, as well as their clinical courses. However, it is difficult to reach a firm conclusion because this study was retrospective and included only a small number of subjects. For example, it might be inferred that the three patients who exhibited decrement in the facial muscles presented oropharyngeal manifestations more rapidly than the others. Therefore, the speed of disease progression might be associated with neuromuscular instability in ALS, as indicated by Bernstein et al.3 Further comparative studies with larger cohorts of ALS patients are required to clarify this.
In summary, the facial muscles may be involved in ALS with predominant oropharyngeal symptoms, although facial weakness may not be observed clinically. This study makes clear that we cannot simply diagnose MG because the significant decrement of facial muscles is observed to low-rate RNS test.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Mulder DW, Lamber EH, Eaton LM. Myasthenic syndrome in patients with amyotrophic lateral sclerosis. Neurology. 1959;9:627–631. doi: 10.1212/wnl.9.10.627. [DOI] [PubMed] [Google Scholar]
- 2.Denys EH, Norris FH., Jr Amyotrophic lateral sclerosis. Impairment of neuromuscular transmission. Arch Neurol. 1979;36:202–205. doi: 10.1001/archneur.1979.00500400056008. [DOI] [PubMed] [Google Scholar]
- 3.Bernstein LP, Antel JP. Motor neuron disease: decremental responses to repetitive nerve stimulation. Neurology. 1981;31:204–207. doi: 10.1212/wnl.31.2.202. [DOI] [PubMed] [Google Scholar]
- 4.Killian JM, Wilfong AA, Burnett L, Appel SH, Boland D. Decremental motor responses to repetitive nerve stimulation in ALS. Muscle Nerve. 1994;17:747–754. doi: 10.1002/mus.880170708. [DOI] [PubMed] [Google Scholar]
- 5.Wang FC, De Pasqua V, Gérard P, Delwaide PJ. Prognostic value of decremental responses to repetitive nerve stimulation in ALS patients. Neurology. 2001;57:897–899. doi: 10.1212/wnl.57.5.897. [DOI] [PubMed] [Google Scholar]
- 6.Pinto S, de Carvalho M. Amyotrophic lateral sclerosis patients and ocular ptosis. Clin Neurol Neurosurg. 2008;110:168–170. doi: 10.1016/j.clineuro.2007.08.022. [DOI] [PubMed] [Google Scholar]
- 7.Restivo DA, Bianconi C, Ravenni R, De Grandis D. ALS and myasthenia: an unusual association in a patient treated with riluzole. Muscle Nerve. 2000;23:294–295. doi: 10.1002/(sici)1097-4598(200002)23:2<294::aid-mus25>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 8.AAEM Quality Assurance Committee. American Association of Electrodiagnostic Medicine. Literature review of the usefulness of repetitive nerve stimulation and single fiber EMG in the electrodiagnostic evaluation of patients with suspected myasthenia gravis or Lambert-Eaton myasthenic syndrome. Muscle Nerve. 2001;24:1239–1247. doi: 10.1002/mus.1140. [DOI] [PubMed] [Google Scholar]
- 9.Bjornskov EK, Dekker NP, Norris FH, Jr, Stuart ME. End-plate morphology in amyotrophic lateral sclerosis. Arch Neurol. 1975;32:711–712. doi: 10.1001/archneur.1975.00490520081016. [DOI] [PubMed] [Google Scholar]
- 10.Dupuis L, Loeffler JP. Neuromuscular junction destruction during amyotrophic lateral sclerosis: insights from transgenic models. Curr Opin Pharmacol. 2009;9:341–346. doi: 10.1016/j.coph.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 11.Fischer LR, Culver DG, Tennant P, Davis AA, Wang M, Castellano-Sanchez A, et al. Amyotrophic lateral sclerosis is a distal axonopathy: evidence in mice and man. Exp Neurol. 2004;185:232–240. doi: 10.1016/j.expneurol.2003.10.004. [DOI] [PubMed] [Google Scholar]