Abstract
Background
Herpes zoster ophthalmicus (HZO) can involve the oculomotor nerve; however, isolated trochlear nerve palsy has rarely been reported.
Case Report
An 83-year-old man who suffered from HZO in the right frontal area and scalp subsequently developed vertical diplopia and severe pain. Cerebrospinal fluid examination and brain MRI revealed no abnormalities. Isolated right trochlear nerve palsy was diagnosed based on the findings of neuro-ophthalmological tests.
Conclusions
Isolated trochlear nerve involvement associated with HZO is very rare and may be easily overlooked. Physicians should carefully examine oculomotor involvement in HZO.
Keywords: cranial nerve involvement, herpes zoster ophthalmicus, trochlear nerve
Introduction
Herpes zoster ophthalmicus (HZO) causes diverse ocular and central nervous system lesions. In HZO, the reported incidence of extraocular muscle palsies has ranged between 7% and 31%,1-4 but many cases are asymptomatic because the diplopia is observed in the extreme of gaze and visual acuity is decreased in the affected eye.4 The oculomotor nerve is most commonly affected, followed by the abducens nerve; the trochlear nerve appears to be the least frequently involved.3-6
We report herein the case of a man who suffered from HZO in the right frontal area and scalp, and who subsequently developed vertical diplopia due to isolated trochlear nerve palsy.
Case Report
An 83-year-old man with a 14-year history of controlled hypertension and diabetes presented to our emergency room with acute confusion. Five days previously a vesicular eruption and lancinating pain had developed over the distribution of the ophthalmic branch of the trigeminal nerve on the right side of the forehead; the headache was treated with oral acetaminophen. On examination, his blood pressure was 170/90 mmHg and his body temperature was 36℃. A neurological examination demonstrated reduced wakefulness associated with time, place, and person disorientation. The cranial nerves, and sensory and motor functions were all normal, and no meningeal irritating signs were detected. Deep tendon reflexes were symmetrically normal and Babinski's sign was not observed. The results of routine laboratory tests were normal, with the exception of an elevated fasting blood glucose level of 252 mg/dL. Brain computed tomography and MRI revealed no abnormalities. Cerebrospinal fluid examination was normal with the exception of increased levels of varicella zoster virus IgG and IgM. The patient was started on intravenous acyclovir at 1,500 mg/day. His blood pressure ranged from 190/100 to 230/110 mmHg during the 24 hours after admission. After adding antihypertensive agents the patient's drowsiness and disorientation were markedly improved, and he was alert and able to answer correctly in response to queries about recent events. However, the dose of acyclovir was changed to 1,000 mg/day orally 2 days later because his serum creatinine levels rose to 1.6 mg/dL and he complained of difficulty urinating and swelling of the lower extremities.
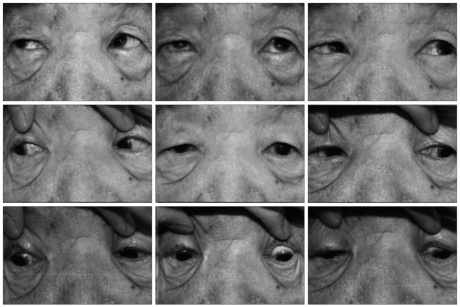
Two weeks after the vesicular eruption appeared on the right side of his forehead, the patient complained of vertical diplopia when he looked in the left lower direction. The diplopia was not observed with other directional eye movements. Ophthalmologic examination revealed his visual acuity to be 20/25 in each eye, and no visual field defects were noted on the Goldmann perimeter. His pupils were isocoric, with prompt and symmetrical light reflexes. The right eye showed a severe inferior oblique overaction and underaction of the superior oblique muscle. The hypertropia increased on leftward gaze (Fig. 1). The Bielschowsky three-step head-tilt test disclosed isolated right superior oblique palsy, and the prism cover-uncover test showed right exodeviation of 10 prism diopters (PD) on near fixation and right hypertrophy of 4 PD on far fixation. Left side downward gaze caused right hypertrophy of 6 PD, and tilting toward the right side produced right hypertrophy of 6 PD. Routine laboratory tests and brain MRI were performed repeatedly but no abnormal findings were observed. The patient was not prescribed acyclovir or steroid. A follow-up examination performed 4 weeks later found that the trochlear nerve palsy had not improved.
Fig. 1.
Nine gaze eye positions. The range of eye motion in the cardinal position revealed overelevation of the right eye in adduction, with inferior oblique overaction of the right eye.
Discussion
The extraocular muscle palsy associated with HZO is usually seen in the elderly and is a self-limiting condition.4 In HZO, extraocular muscle palsy occurs within 1-2 weeks after the appearance of skin lesions and improves significantly within 2 months in most cases.7 However, it has been reported that the duration of diplopia can vary from 2 to 23 months.7
HZO is commonly associated with ocular complications such as keratitis, iridocyclitis, muscular palsies, and optic neuritis in approximately half of cases.8 However, isolated trochlear nerve palsy is very rare in HZO,5,6,9 and vertical double vision is frequently asymptomatic due to the diplopia that is present only in the extremes of gaze or decreased visual acuity of the affected eye in many cases.2,6 In our case it was necessary to discriminate involvement of the inferior rectus muscle. In inferior rectus paralysis the hypertropia is observed in the primary gaze, with looking to the right and down increasing the hypertrophy. The pathogenetic mechanism underlying extraocular muscle palsy in HZO is not clear and several hypotheses have been proposed. First, a virus may cause a direct cytopathic effect or allergic response in the nervous tissue.10 Second, occlusive vasculitis may induce the cranial neuropathy.11 Third, a myositic cause is another possible mechanism.12
While the treatment of extraocular muscle palsy associated with HZO has not been formally investigated, the administration of antiviral agents or systemic steroid has been suggested.13 However, since the paralytic lesions improve spontaneously and satisfactorily in some cases, the necessity for any specific treatment is equivocal.14 One prospective study found that administering acyclovir during the early course of HZO could prevent the ocular complication.15
Ophthalmoplegia associated with HZO is not uncommon, but isolated trochlear nerve involvement is very rare and can be overlooked. Physicians should carefully examine oculomotor involvement in HZO.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Hunt JR. The paralytic complications of herpes zoster of cephalic extremity. JAMA. 1909;53:1456–1457. [Google Scholar]
- 2.Worster-Drought C. Herpes zoster with localized muscular paralysis. Br Med J. 1923;1:970–971. doi: 10.1136/bmj.1.3258.970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edgerton AE. Herpes Zoster Ophthalmicus: Report of Cases and a Review of the Literature. Trans Am Ophthalmol Soc. 1942;40:390–439. [PMC free article] [PubMed] [Google Scholar]
- 4.Marsh RJ, Dulley B, Kelly V. External ocular motor palsies in ophthalmic zoster: a review. Br J Ophthalmol. 1977;61:677–682. doi: 10.1136/bjo.61.11.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Grimson BS, Glaser JS. Isolated trochlear nerve palsies in herpes zoster ophthalmicus. Arch Ophthalmol. 1978;96:1233–1235. doi: 10.1001/archopht.1978.03910060067013. [DOI] [PubMed] [Google Scholar]
- 6.Tsuda H, Ito T, Yoshioka M, Ishihara N, Sekine Y. Isolated trochlear nerve palsy in herpes zoster ophthalmicus. Intern Med. 2007;46:535–536. doi: 10.2169/internalmedicine.46.6373. [DOI] [PubMed] [Google Scholar]
- 7.Chang-Godinich A, Lee AG, Brazis PW, Liesegang TJ, Jones DB. Complete ophthalmoplegia after zoster ophthalmicus. J Neuroophthalmol. 1997;17:262–265. [PubMed] [Google Scholar]
- 8.Ragozzino MW, Melton LJ, 3rd, Kurland LT, Chu CP, Perry HO. Population-based study of herpes zoster and its sequelae. Medicine (Baltimore) 1982;61:310–316. doi: 10.1097/00005792-198209000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Archambault P, Wise JS, Rosen J, Polomeno RC, Auger N. Herpes zoster ophthalmoplegia. Report of six cases. J Clin Neuroophthalmol. 1988;8:185–193. [PubMed] [Google Scholar]
- 10.Cope S, Jones AT. Hemiplegia complicating ophthalmic zoster. Lancet. 1954;267:898–899. doi: 10.1016/s0140-6736(54)92614-8. [DOI] [PubMed] [Google Scholar]
- 11.Naumann G, Gass JD, Font RL. Histopathology of herpes zoster ophthalmicus. Am J Ophthalmol. 1968;65:533–541. doi: 10.1016/0002-9394(68)93869-5. [DOI] [PubMed] [Google Scholar]
- 12.Kawasaki A, Borruat FX. An unusual presentation of herpes zoster ophthalmicus: orbital myositis preceding vesicular eruption. Am J Ophthalmol. 2003;136:574–575. doi: 10.1016/s0002-9394(03)00323-4. [DOI] [PubMed] [Google Scholar]
- 13.Marsh RJ. Current management of ophthalmic herpes zoster. Trans Ophthalmol Soc U K. 1976;96:334–337. [PubMed] [Google Scholar]
- 14.Schoenlaub P, Grange F, Nasica X, Guillaume JC. [Oculomotor nerve paralysis with complete ptosis in herpes zoster ophthalmicus: 2 cases] Ann Dermatol Venereol. 1997;124:401–403. [PubMed] [Google Scholar]
- 15.Hoang-Xuan T, Büchi ER, Herbort CP, Denis J, Frot P, Thénault S, et al. Oral acyclovir for herpes zoster ophthalmicus. Ophthalmology. 1992;99:1062–1070. doi: 10.1016/s0161-6420(92)31849-4. discussion 1070-1071. [DOI] [PubMed] [Google Scholar]