Abstract
Objectives: The objective of this study was to assess knowledge, attitudes, and behaviors surrounding healthcare-related mobile phone use and text messaging among persons at risk for or infected with tuberculosis (TB) or the human immunodeficiency virus (HIV). Methods: An anonymous survey was conducted in three groups of subjects: (1) HIV-infected persons attending an HIV clinic; (2) persons with latent TB infection at a public health clinic; and (3) persons presenting for TB, HIV, and syphilis screening at a community screening site. Results: Three hundred fifteen (n = 315) persons responded to the survey, of whom 241 (76.5%) owned a cell phone. Cell phone owners were younger and more educated than nonowners. Transportation difficulty and forgetting appointments were cited as significant barriers by 34.2% and 39.5% of respondents, respectively. Fifty-six percent of subjects felt it would be acceptable to receive text message appointment reminders, and 33% felt that text message reminders to take medications would be acceptable. Younger age and cell phone ownership were significantly associated with acceptance of text message reminders. Black and Hispanic subjects were more likely to feel that text message reminders for appointments or medications were helpful than White subjects. Further, Black and Hispanic subjects, as well as subjects with lower educational attainment, were more receptive to healthcare-related educational text messages. Conclusions: Cell phones and text messaging were prevalent among our subjects attending HIV and TB clinics, and subjects were generally receptive to text messaging for healthcare-related communication. Interventions that explore the potential for text messaging to improve clinic attendance, medication adherence, and health knowledge should be explored.
Key words: cellular phone, health disparities, human immunodeficiency virus, tuberculosis
Introduction
Barriers to healthcare utilization are not uncommon among underserved populations with communicable diseases such as tuberculosis (TB), the human immunodeficiency virus (HIV), or syphilis. In a study of HIV-infected women at an urban clinic, barriers to appointment attendance included inclement weather, less than a high-school education, substance abuse, depression, and fear of bad news. However, the biggest barrier to appointment attendance in this study was forgetting about the appointment; 61% of those who missed appointments reported “forgetting” as the reason.1 Because forgetting plays such a large role in adherence to medical care, novel strategies are needed to address this issue.
Americans are increasingly using cellular phones in their daily life, and many use these phones to send text messages. Eighty-two percent of adults in the United States now own a cell phone. Text messaging is increasing dramatically, with the proportion of adults sending and receiving texts increasing from 65% in a September 2009 Pew survey to 72% in May 2010.2 Cell phones have been embraced by a diverse population in the United States; 50% of those ≥65 years had cell phones, and 84% of Hispanics and 71% of African Americans reported owning cell phones.3 In one study of women attending an urban sexually transmitted infections clinic, 93% reported owning a cellular phone and 79% used text messaging to communicate.4
Not surprisingly, text messaging is an increasingly common method of communicating between medical providers and patients. Text message reminders of clinic appointments are being used in a number of healthcare settings. Text messages have been shown to be effective reminders regarding sunscreen application,5 adherence to asthma medications,6 and antirejection medications among liver transplant recipients (as well as decreasing episodes of rejection).7 In a novel program introduced by the San Francisco Public Health Department, youth were encouraged to text “SEXINFO” to a five-digit number and then would receive options to text for health information regarding what to do if a condom broke, if they were concerned they were pregnant, or if they wanted information about sexually transmitted diseases (STDs). Over 4,500 text inquiries were sent in the first 6 months and the program was deemed to be a novel way to reach at-risk youth.8
Given the increasing use of cell phones and text messaging in the United States, there is an increasing need to assess attitudes regarding healthcare-related cell phone use and text messaging and to explore its potential use among patients with or at risk for communicable diseases to improve healthcare utilization and adherence. We sought to describe attitudes regarding cell phones and the prevalence of cell phone use and text messaging among three groups: (1) HIV-infected persons attending an HIV clinic; (2) persons with latent TB attending a public health clinic; and (3) persons presenting for TB, HIV, or syphilis screening at a community-based screening program. We hypothesized that many of these individuals were already using cell phones and text messaging in their daily lives and would be open to receiving text messages from their doctor's office in the form of appointment or medication reminders.
Methods
We conducted an anonymous survey to assess knowledge, attitudes, and behaviors surrounding healthcare-related mobile phone use and text messaging in three groups of subjects: (1) HIV-infected persons attending an HIV clinic; (2) persons with latent TB infection at a public health clinic; and (3) persons presenting for TB, HIV, and syphilis screening at a community-based screening program. Surveys were administered by research staff between June 2009 and November 2009 in English or Spanish to persons 18 years or older. There was a several week pilot period of the survey instrument, during which time unclear questions were revised and refined. The survey instrument was designed using Likert scores, and several “redundant” questions were included to assess internal consistency of responses.
Patients were approached in waiting rooms prior to their appointments at the HIV clinic and the TB public health clinic and asked to complete the anonymous survey. For those who declined, no specific effort was made to approach them again. When research personnel were not present to hand out surveys, blank surveys were kept at the front desk next to check-in with a sign requesting that patients complete and return a survey. The completed surveys were returned to the staff member at the front desk. Persons presenting for TB, HIV, and syphilis screening at the community-based screening program were asked to complete the survey during their point of contact for community screening. Data were entered into a password-protected Microsoft Access database. The Duke University Medical Center's Institutional Review Board granted an exemption from review for this study based on anonymous responses and minimal potential for harm to the subjects.
Statistical analysis was performed using SAS 9.2 (SAS Institute Inc., Cary, NC). Proportions were used to describe categorical data, and medians/interquartile ranges were used to describe Likert scale data. Differences in responses among demographic, site, and/or socioeconomic groups were assessed using the chi-square/Fisher's exact test (categorical data) or the Wilcoxon rank-sum test (comparing two groups)/Kruskal–Wallis test (comparing three or more groups), as appropriate. Correlations were determined using the Spearman rank correlation. Multivariable analysis was performed by simultaneously entering all variables into a model using SAS PROC GENMOD or PROC GLM. The dependent variables in the multivariable analyses were Likert scores (1–5) and were treated as continuous variables for analysis purposes. All p-values were two sided. Educational level was assessed as a categorical response (e.g., elementary school, some high school, graduated high school) and transformed into an ordinal variable for analysis. Cronbach's alpha was used to evaluate intrasurvey reliability by pairwise examination of similar questions (e.g., acceptability of text messaging vs. perceived helpfulness of text messaging); reliability was deemed good as all alpha values were >0.70.
Results
Characteristics Of The Sample
Three-hundred fifteen people responded to the survey: 194 (61.6%) at the HIV clinic, 97 (30.8%) at the TB clinic, and 24 (7.6%) at the community-based screening program (Table 1). Respondents' mean age was 42 years (range: 18–82) and 47.7% were women. The population was ethnically diverse, with 29.2% identifying as White, 53.0% Black, 8.6% Hispanic, 3.8% Asian, and 5.4% other/unknown. Sixteen percent (50/309) had not graduated from high school (309 people answered this question).
Table 1.
Subject Characteristics (n = 315)
| Tuberculosis Clinic (N = 97) | Hiv Clinic (N = 194) | Community-Based Screening Program (N = 24) | |
|---|---|---|---|
| Race/ethnicity | |||
| White, non-Hispanic | 29 (29.9%) | 62 (32.0%) | 0 (0%) |
| Black, non-Hispanic | 36 (37.1%) | 107 (55.1%) | 22 (91.7%) |
| Hispanic | 17 (17.5%) | 9 (4.6%) | 1 (4.2%) |
| Asian | 9 (9.3%) | 3 (1.6%) | 0 (0%) |
| Native American | 0 (0%) | 2 (1.0%) | 0 (0%) |
| Pacific Islander | 1 (1.0%) | 0 (0%) | 0 (0%) |
| Multiracial | 0 (0%) | 2 (1.0%) | 0 (0%) |
| Unknown | 5 (5.1%) | 9 (4.6%) | 1 (4.2%) |
| Median age (interquartile range) | 32.5 (25–46) | 45 (38–51) | 45 (38–55) |
| Sex | |||
| Male | 33 (34%) | 120 (61.9%) | 9 (37.5%) |
| Female | 62 (63.9%) | 71 (36.6%) | 15 (62.5%) |
| No response | 2 (0.02%) | 3 (1.6%) | 0 (0%) |
| Living situation | |||
| Apartment | 34 (35.1%) | 59 (30.4%) | 15 (62.5%) |
| Single-family home | 48 (49.5%) | 99 (51.0%) | 4 (16.7%) |
| Condominium | 4 (4.1%) | 2 (1.0%) | 0 (0%) |
| Mobile home | 2 (2.1%) | 11 (5.7%) | 1 (4.2%) |
| Homeless shelter | 3 (3.1%) | 2 (1.0%) | 0 (0%) |
| Other | 2 (2.0%) | 2 (1.0%) | 0 (0%) |
| No response | 4 (4.1%) | 14 (7.2%) | 4 (16.7%) |
| Education | |||
| Elementary school | 2 (2.1%) | 4 (2.1%) | 1 (4.2%) |
| Some high school | 9 (9.3%) | 27 (13.9%) | 7 (29.2%) |
| High-school graduate | 25 (25.8%) | 51 (26.3%) | 6 (25.0%) |
| Some college | 26 (26.8%) | 58 (29.9%) | 7 (29.2%) |
| College graduate | 20 (20.6%) | 33 (17.0%) | 1 (4.2%) |
| Postcollege education | 13 (13.4%) | 19 (9.8%) | 0 (0%) |
| No response | 2 (2.1%) | 2 (1.0%) | 2 (8.3%) |
HIV, human immunodeficiency virus.
Results For Cell Phone Ownership By Subjects' Demographics
Two hundred forty-one (76.5%) respondents owned a cell phone, and 142 of these (58.9%) indicated that the cell phone was the preferred method of communication. Cell phone owners were on average younger than respondents who did not own a cell phone (median age: 42 vs. 46 years; p = 0.0003). Cell phone ownership did not significantly differ by sex or race/ethnicity. Subjects enrolled at the HIV or TB clinic were more likely to own a cell phone (76.8% and 80.4%, respectively) than those enrolled at the community screening site (58.3%), but this difference was of borderline significance (p = 0.07). Cell phone ownership significantly increased with increasing level of education (p = 0.0007). However, among subjects who owned cell phones, the frequency of cell phone use and text messaging did not significantly correlate with educational level. Among cell phone owners, the frequency of cell phone use weakly correlated with age (r = −0.12, p = 0.08), but the frequency of sending (r = −0.38, p < 0.0001) and receiving (r = −0.39, p < 0.0001) text messages strongly correlated with age. Neither race nor enrollment site was significantly associated with frequency of cell phone use or text messaging.
Results For Barriers To Attending Clinic Appointments And Taking Medications
Subjects were asked about several barriers to attending appointments. Transportation was noted as a barrier (Likert response of “2” or greater on a 1–5 scale, with “1” denoting “easy” to get transportation to medical appointments and “5” denoting “hard”) by 34.2% of respondents. Twenty-seven percent of respondents indicated that they had missed appointments because of difficulty with obtaining transportation, and not surprisingly, there was a strong correlation between difficulty in obtaining transportation to medical appointments and self-reported frequency of missed appointments due to transportation difficulties (r = 0.60, p < 0.0001). Lack of reliable childcare was noted as a barrier at least some of the time by 9.5% of respondents. Forgetting about appointments was noted as a barrier at least some of the time by 39.5% of respondents. Self-reported frequency of forgetting about appointments also significantly correlated with missing appointments because of transportation difficulty (r = 0.38, p < 0.0001) and lack of reliable childcare (r = 0.17, p = 0.0033). Forgetting appointments was not significantly associated with cell phone ownership, age, educational level, or race.
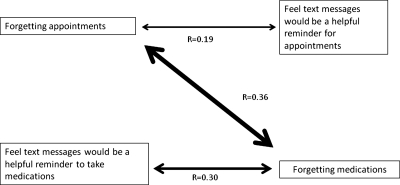
Forty-nine percent of subjects who were prescribed regular medications admitted to at least some difficulty in remembering to take medications regularly. Forgetting to take medications regularly was significantly associated with forgetting to attend medical appointments (r = 0.36, p < 0.0001), but was not significantly associated with cell phone ownership, age, educational level, or race.
Results For Attitudes Regarding Cell Phone Use And Text Messaging For Healthcare
Fifty-six percent of subjects felt it would be acceptable (Likert score of 4 or higher) to receive text messages reminding them of doctor's appointments, and of those who felt it would be acceptable, 88% felt it would also be helpful to receive text appointment reminders. Another 14.3% of subjects were unsure of the acceptability of text message appointment reminders, and 29.6% felt that text message appointment reminders were not acceptable. Thirty-three percent felt it would be acceptable to receive text messages to remind them to take medications, and of those who felt it would be acceptable, 67% felt it would be helpful to receive text reminders to take their medications. Another 17.1% of subjects were unsure of the acceptability of text message medication reminders, and 42.5% felt that text message medication reminders were not acceptable. In multivariable analysis (Table 2), younger age and cell phone ownership were significantly associated with more positive attitudes toward the acceptability of text messaging for appointment reminders, but only younger age was significantly associated with believing that text messaging to remind one to take medications was acceptable. Younger persons and persons of either Black or Hispanic race/ethnicity were more likely to feel that text message reminders for either appointments or medications would be helpful; cell phone ownership was not significantly associated with either of these attitudes. There was a significant positive association between missing doctor's appointments because of forgetting them and feeling that text messages would be helpful as a reminder for doctor's appointments (r = 0.19, p = 0.01; Fig. 1). There was also a significant positive association between forgetting one's medications and feeling that text messaging would be a helpful reminder to take medications (r = 0.29, p < 0.0001). Several reasons were mentioned among persons who did not feel that text reminders would be acceptable: 62 indicated that cost was a consideration, 53 respondents mentioned concerns about privacy, and 28 felt that text messages from one's healthcare provider would be annoying (each respondent could mention more than one reason).
Table 2.
Multivariable Models Examining Receptiveness to Text Messaging for Doctor's Appointments, Medications, and Health Education by Subjects' Demographics and Cell Phone Ownership
| Model Coefficient | P-Value | |
|---|---|---|
| Acceptable to receive text reminders of appointments | ||
| Increasing age | −0.0355 | <0.0001 |
| Female gender (vs. male) | 0.0762 | 0.70 |
| Race/ethnicity | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.3076 | 0.21 |
| Hispanic | 0.4550 | 0.24 |
| Other | 0.3405 | 0.37 |
| Increasing education | 0.0669 | 0.44 |
| Cell phone owner (vs. nonowner) | 0.7432 | 0.006 |
| Acceptable to receive text reminders to take medications | ||
| Increasing age | −0.0194 | 0.029 |
| Female gender (vs. male) | −0.1085 | 0.60 |
| Race/ethnicity | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.3707 | 0.15 |
| Hispanic | 0.4006 | 0.34 |
| Other | 0.4714 | 0.23 |
| Increasing education | −0.0381 | 0.68 |
| Cell phone owner (vs. nonowner) | 0.3150 | 0.23 |
| Helpful to receive text reminders of appointments | ||
| Increasing age | −0.0374 | <0.0001 |
| Female gender (vs. male) | 0.3037 | 0.1281 |
| Race/ethnicity | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.4805 | 0.04 |
| Hispanic | 0.7008 | 0.08 |
| Other | 0.0031 | 0.99 |
| Increasing education | 0.0816 | 0.35 |
| Cell phone owner (vs. nonowner) | 0.2832 | 0.26 |
| Helpful to receive text reminders to take medications | ||
| Increasing age | −0.0292 | 0.001 |
| Female gender (vs. male) | 0.3209 | 0.14 |
| Race/ethnicity | ||
| continued | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.4571 | 0.07 |
| Hispanic | 0.7844 | 0.09 |
| Other | 0.2358 | 0.55 |
| Increasing education | −0.1094 | 0.24 |
| Cell phone owner (vs. nonowner) | 0.1023 | 0.70 |
| Helpful to receive educational texts on HIV or sexually transmitted diseases | ||
| Increasing age | −0.0138 | 0.09 |
| Female gender (vs. male) | 0.2652 | 0.18 |
| Race/ethnicity | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.5334 | 0.02 |
| Hispanic | 0.7535 | 0.05 |
| Other | 0.1761 | 0.63 |
| Increasing education | −0.2183 | 0.01 |
| Cell phone owner (vs. nonowner) | −0.2876 | 0.25 |
| Helpful to receive educational texts on tuberculosis | ||
| Increasing age | −0.0085 | 0.31 |
| Female gender (vs. male) | 0.1031 | 0.61 |
| Race/ethnicity | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.5935 | 0.01 |
| Hispanic | 0.8713 | 0.03 |
| Other | 0.2078 | 0.58 |
| Increasing education | −0.1810 | 0.04 |
| Cell phone owner (vs. nonowner) | 0.3618 | 0.16 |
| Helpful to receive other health-related educational texts (e.g., diabetes, hypertension) | ||
| Increasing age | −0.0092 | 0.28 |
| Female gender (vs. male) | 0.2073 | 0.30 |
| Race/ethnicity | ||
| White, non-Hispanic | Referent | N/A |
| Black, non-Hispanic | 0.6069 | 0.01 |
| Hispanic | 0.9045 | 0.02 |
| Other | 0.1730 | 0.64 |
| Increasing education | −0.1972 | 0.02 |
| Cell phone owner (vs. nonowner) | 0.4708 | 0.07 |
N/A, not applicable.
Fig. 1.
Correlation between forgetting doctor's appointments and medications and helpfulness of text messages. Thickness of line indicates strength of correlation.
Twenty-eight percent felt that receiving text messages about ways to prevent HIV infection or other sexually transmitted diseases would be helpful (Likert score of 4 or higher), and 30.5% felt that receiving texts about ways to prevent TB would be helpful. Thirty-seven percent of respondents felt that receiving text messages containing information about weight loss, hypertension, or diabetes would be helpful. In general, lower educational level and being of either Black or Hispanic race/ethnicity was associated with increased interest in receiving educational text messages (Table 2).
Discussion
Significant barriers to healthcare access and utilization disproportionately obstruct receipt of appropriate healthcare among disadvantaged minorities and persons of lower socioeconomic status.9–12 Our data suggest that persons in these groups would be highly receptive to text message reminders. Cell phone ownership was found to extend across socioeconomic lines; even among persons surveyed who were homeless or marginally housed, nearly 40% (7 of 18) owned a cell phone. In the case of these individuals, text messages may reach a person when traditional mail delivery services cannot reach them. Further, receiving a text message does not impose the inconvenience of having to answer a telephone call, and the message is saved for later viewing.
Our data suggest that cell phones may be increasingly useful in reaching disadvantaged populations. A recent survey from the Center for Health Statistics reported that 22.9% of all adults surveyed during July–December 2009 resided in households in which the only telephone is a cell phone, a proportion that has been increasing dramatically over the past 5 years.8 Further, adults residing in these “cell phone only” households were more likely to report being uninsured, experiencing financial barriers to healthcare, and participating in deleterious behaviors such as binge drinking and smoking.13,14 The demographics of cell phone use are evolving rapidly; for example, in a 2007 study of 515 individuals with HIV, Whites, those with more education, and those who were employed were more likely to use cell phones.15 However, a 2008 study of primarily African-American women attending an urban sexually transmitted infection clinic reported very high rates of cell phone ownership (93%) and text messaging (79%).4 Our data confirm that the demographic reach of cell phones has expanded, and further we found that minority groups (African-Americans and Hispanics) surveyed were more amenable to receiving information from healthcare providers via text messaging than White patients.
There are some drawbacks to using text messaging for healthcare-related communication. A significant minority of respondents in our survey did not own cell phones. Further, use of text messaging requires adequate literacy, which may be a problem in some populations. For a healthcare provider to utilize this mode of communication, there is the expense of purchasing software and the logistical challenge of automating the reminders. Cost to the receiver is another issue; although each text message may only cost a few cents, many survey respondents listed cost of texting as one of their main reservations about receiving texts from healthcare providers. However, as the cost of text messaging is relatively low, a relatively small increase in appointment attendance due to text messaging would probably be cost-effective even if the provider paid for the cost of the message. We found less enthusiasm for frequent, daily reminders to take medications than for less-frequent appointment reminders. In addition, fewer people were amenable to the idea of receiving text messages for health education purposes than for reminders. This suggests that the frequency and content of text messages from healthcare providers is important; based on this survey, it appears that less-frequent, targeted reminders would be most acceptable. Overutilization of text messaging as a means of communication could lead to loss of effect; text messages could become like “spam” e-mails, deleted without reading. Fatigue with loss of text message efficacy may also occur over time, as demonstrated in a recent randomized trial of text messaging for diabetes management.16 However, persons with more complex medical conditions may accept more intensive texting interventions, as demonstrated by a recent study of a relatively intensive cell phone-based program for patients with cystic fibrosis17 and pilot studies of health-monitoring programs for blood pressure, blood glucose, and TB medication adherence.18,19 Designing systems that are easy to use and educating users as to the importance of the underlying health condition may also improve acceptance of more intensive texting interventions.20 It will be important to find a balance with this technology that provides adequate information without causing information overload.
Another interesting finding was that a number of persons who do not own cell phones had positive attitudes toward healthcare-related text message reminders. Inexpensive, disposable cell phones are now available with the ability to remotely add prepaid minutes. Given the positive attitudes observed here, one could envision programs in which inexpensive cell phones were given to targeted populations specifically for healthcare-related communication. The use of cell phones for medical purposes in vulnerable or hard-to-reach populations was effective in one study of homeless cocaine-addicted adults in a treatment program. Subjects were given cell phones to record information about craving and using cocaine, and 80% completed the full 2-week protocol. The cell phone self-reports in this study were also quite reliable; drug use reported via text messaging was in agreement with urine toxicology results 73% of the time.21
Our study has some important limitations. Individuals in waiting rooms were given the opportunity to complete a survey if they were so inclined; this was not a randomly generated sample. Because the population of survey respondents was self-selected, this may limit the ability to generalize these findings to a larger population. However, the findings of this survey suggest that using text messaging to enhance healthcare utilization and adherence may be an effective tool in traditionally underserved individuals such as those with HIV or TB infection. Further studies are needed to assess the effect of text message reminders and health-related educational texts on health outcomes.
Acknowledgments
The authors gratefully acknowledge the staff of the Duke Adult Infectious Diseases Clinic and of the Wake County Human Services Clinic E for assistance with administering this survey. This study was funded by a National Institutes of Health AIDS Training Grant (5T32 AI007392 to A.K.P.).
Disclosure Statement
No competing financial interests exist.
References
- 1.Tello MA. Jenckes M. Gaver J. Anderson JR. Moore RD. Chander G. Barriers to recommended gynecologic care in an urban United States HIV clinic. J Womens Health (Larchmt) 2010;19:1511–1518. doi: 10.1089/jwh.2009.1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Lenhart A. Cell phones and American Adults. Pew Internet and American Life Project; 2010. http://pewinternet.org/∼/media//Files/Reports/2010/PIP_Adults_Cellphones_Report_2010.pdf. [Sep 2;2010 ]. http://pewinternet.org/∼/media//Files/Reports/2010/PIP_Adults_Cellphones_Report_2010.pdf cited 2010 09/11/2010.
- 3.Horrigan JB. Seeding The Cloud: What Mobile Access Means for Usage Patterns and Online Content. Pew Internet and American Life Project; 2008. www.pewinternet.org/∼/media//Files/Reports/2008/PIP_Users.and.Cloud.pdf. [Sep 11;2010 ]. www.pewinternet.org/∼/media//Files/Reports/2008/PIP_Users.and.Cloud.pdf
- 4.Samal L. Hutton HE. Erbelding EJ. Brandon ES. Finkelstein J. Chander G. Digital divide: Variation in internet and cellular phone use among women attending an urban sexually transmitted infections clinic. J Urban Health. 2010;87:122–128. doi: 10.1007/s11524-009-9415-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Armstrong AW. Watson AJ. Makredes M. Frangos JE. Kimball AB. Kvedar JC. Text-message reminders to improve sunscreen use: A randomized, controlled trial using electronic monitoring. Arch Dermatol. 2009;145:1230–1236. doi: 10.1001/archdermatol.2009.269. [DOI] [PubMed] [Google Scholar]
- 6.Strandbygaard U. Thomsen SF. Backer V. A daily SMS reminder increases adherence to asthma treatment: A three-month follow-up study. Respir Med. 2010;104:166–171. doi: 10.1016/j.rmed.2009.10.003. [DOI] [PubMed] [Google Scholar]
- 7.Miloh T. Annunziato R. Arnon R. Warshaw J. Parkar S. Suchy FJ, et al. Improved adherence and outcomes for pediatric liver transplant recipients by using text messaging. Pediatrics. 2009;24:e844–e850. doi: 10.1542/peds.2009-0415. [DOI] [PubMed] [Google Scholar]
- 8.Levine D. McCright J. Dobkin L. Woodruff AJ. Klausner JD. SEXINFO: A sexual health text messaging service for San Francisco youth. Am J Public Health. 2008;98:393–395. doi: 10.2105/AJPH.2007.110767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kidder DP. Wolitski RJ. Campsmith ML. Nakamura GV. Health status, health care use, medication use, and medication adherence among homeless and housed people living with HIV/AIDS. Am J Public Health. 2007;97:2238–2245. doi: 10.2105/AJPH.2006.090209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Shi L. Lebrun LA. Tsai J. Access to medical care, dental care, and prescription drugs: The roles of race/ethnicity, health insurance, and income. South Med J. 2010;103:509–516. doi: 10.1097/SMJ.0b013e3181d9c2d8. [DOI] [PubMed] [Google Scholar]
- 11.Lillie-Blanton M. Stone VE. Snow Jones A. Levi J. Golub ET. Cohen MH, et al. Association of race, substance abuse, and health insurance coverage with use of highly active antiretroviral therapy among HIV-infected women, 2005. Am J Public Health. 2010;100:1493–1499. doi: 10.2105/AJPH.2008.158949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Flores G. Tomany-Korman SC. Racial and ethnic disparities in medical and dental health, access to care, and use of services in US children. Pediatrics. 2008;121:e286–e298. doi: 10.1542/peds.2007-1243. [DOI] [PubMed] [Google Scholar]
- 13.Blumberg SJ. Luke JV. Early release of estimates from the National Health Interview Survey, July–December 2009. National Center for Health Statistics; 2010. www.cdc.gov/nchs/nhis.htm. [May 1;2010 ]. www.cdc.gov/nchs/nhis.htm cited 2010 09/26/2010.
- 14.Lee S. Brick JM. Brown ER. Grant D. Growing cell-phone population and noncoverage bias in traditional random digit dial telephone health surveys. Health Serv Res. 2010;45:1121–1139. doi: 10.1111/j.1475-6773.2010.01120.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shacham E. Stamm K. Overton ET. Can you hear me now? Limited use of technology among an urban HIV-infected cohort. AIDS Care. 2009;21:1000–1006. doi: 10.1080/09540120802612832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hanauer DA. Wentzell K. Laffel N. Laffel LM. Computerized Automated Reminder Diabetes System (CARDS): E-mail and SMS cell phone text messaging reminders to support diabetes management. Diabetes Technol Ther. 2009;11:99–106. doi: 10.1089/dia.2008.0022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Marciel KK. Saiman L. Quittell LM. Dawkins K. Quittner AL. Cell phone intervention to improve adherence: Cystic fibrosis care team, patient, and parent perspectives. Pediatr Pulmonol. 2010;45:157–164. doi: 10.1002/ppul.21164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Agarwal S. Lau CT. Remote health monitoring using mobile phones and Web services. Telemed J E Health. 2010;16:603–607. doi: 10.1089/tmj.2009.0165. [DOI] [PubMed] [Google Scholar]
- 19.Hoffman JA. Cunningham JR. Suleh AJ. Sundsmo A. Dekker D. Vago F, et al. Mobile direct observation treatment for tuberculosis patients: A technical feasibility pilot using mobile phones in Nairobi, Kenya. Am J Prev Med. 2010;39:78–80. doi: 10.1016/j.amepre.2010.02.018. [DOI] [PubMed] [Google Scholar]
- 20.Jen WY. The adoption of mobile weight management services in a virtual community: The perspective of college students. Telemed J E Health. 2010;16:490–497. doi: 10.1089/tmj.2009.0126. [DOI] [PubMed] [Google Scholar]
- 21.Freedman MJ. Lester KM. McNamara C. Milby JB. Schumacher JE. Cell phones for ecological momentary assessment with cocaine-addicted homeless patients in treatment. J Subst Abuse Treat. 2006;30:105–111. doi: 10.1016/j.jsat.2005.10.005. [DOI] [PubMed] [Google Scholar]