Abstract
Objective
The Clinical Research Center for Depression (CRESCEND) study is a 9-year observational collaborative prospective cohort study for the clinical outcomes in participants with depressive disorders in Korea. In this study, we examined the baseline characteristics of the depressive participants as the hospital-based cohort.
Methods
Participants were assessed using various instruments including the Clinical Global Impression scale, 17-item Hamilton Depression Rating Scale (HDRS-17), Hamilton Anxiety Rating Scale, Brief Psychiatric Rating Scale, Social and Occupational Functioning Assessment Scale, Beck Depression Inventory-Second Edition, Scale for Suicide Ideation, and World Health Organization Quality of Life assessment instruments-abbreviated version. Also, personal histories of medical and psychiatric illnesses and the range of socio-epidemiologic and clinical data were collected from each participant.
Results
One thousand one hundred eighty three participants were recruited from 18 hospitals. The mean age of the participants was 47.9±15.9 year-old, 74.4% were female, 82.9% had been diagnosed of major depressive disorder, 40.9% were experiencing their first depressive episode, and 21.4% had a past history of suicide attempts. The majority (85.3%) of the participants were moderately to severely ill. The average HDRS-17 was 19.8±6.1. Significant gender differences at baseline were shown in age, education, marriage, employment, religion, and first depressive episode.
Conclusion
The baseline findings in the CRESCEND study showed some different characteristics of depression in Korea, suggesting a possibility of ethnic and cultural factors in depression.
Keywords: Depression, Hospital-based, Longitudinal, Observational, Prospective
INTRODUCTION
Depression [especially, major depressive disorder (MDD)] is a common psychiatric disorder typically associated with significant suffering, high morbidity and mortality rates, and psychosocial impairment.1 The 12-month prevalence and the lifetime prevalence rates of MDD are estimated at 6.6% and 16.2%, respectively.2,3 However, considering that depression is often under-recognized and undertreated in the community,4 the actual prevalence of the depression may be much higher.
Depression is associated with a wide range of negative consequences, including a significant worsening of comorbid medical conditions, a high mortality risk related to suicide, and a socioeconomic burden resulting from functional impairment.5-7 The magnitude of socioeconomic burden and disability associated with depression is increasing. The World Health Organization (WHO) has reported that by 2020, major depression will be second only to ischemic heart disease as a cause of disability worldwide. This socioeconomic burden will be even greater in the developing countries, where major depression may be the leading cause of disability by 2020.8,9
Depression is a clinical syndrome having pronounced heterogeneity in risk factors, clinical presentation, clinical course, and treatment responsiveness.10 Also its clinical aspects display ethnic and cultural variations.11 To address the many issues depression presents, a nationwide clinical study, as well as international efforts for consensus regarding depression is needed.
In Korea, depression is also a common psychiatric disorder. The 12-month prevalence and the lifetime prevalence rates of the MDD are 1.7% and 4.3%, respectively.12 These rates are lower than those found in the United States2,3 and in European countries,13 and are similar to those in East-Asian countries.14-16 The reported low prevalence of depression in Korea may reflect the fact that there are enormous social stigma attached to depression, ethnic and cultural influences, and methodological differences.11,12,17
Despite the relatively low prevalence of depression, depression has a deep impact on Korean society. The socioeconomic burden of depression in Korea cost over 1.5 billion US dollars in 2004.18 Also, the suicidal rate in Korea is on the increase, up to 26.1 persons per 100,000 people in 2005, which was the highest position in the Organization for Economic Cooperation and Development (OECD) countries.19 The continuous increase of depression itself and suicide, which is one of the serious outcomes of depression, prompted mental health professionals to thoroughly investigate clinical aspects of depression in Korea. Unfortunately, up to now, many investigators in Korea have preferred biological or pharmacological studies to clinical studies of depression due to the relatively easy accessibility of the funding and the fact that there is no long-term prospective clinical study for depression with a large cohort in Korea.
The Clinical Research Center for Depression (CRESCEND) study is a long-term (phase 1, 1-year; phase 2, 8-year) observational collaborative prospective cohort study of clinical outcomes in participants with depressive disorders. The primary objective of the CRESCEND study is to investigate the clinical risk factors, courses, and outcomes of depression in the Korean society. The secondary objectives include evaluating the changes in the quality of life and the risk of suicide according to the clinical course of depression, as well as the actual social and economic burden of depression, and providing the clinical evidence for the development of Korean-specific diagnostic tools and clinical practice guidelines. The CRESCEND study is the first nationwide long-term observational prospective cohort study investigating actual medical care for depressive disorders to be conducted in Korea. The aims of this article are to introduce an overview of the CRESCEND study as well as to provide the baseline socio-epidemiologic and clinical findings of the participants.
METHODS
Study population
From January 2006 to August 2008, 1,183 participants were enrolled in the CRESCEND study. The 18 hospitals collaborating in this study included psychiatric departments of 16 university hospitals and 2 general hospitals from all over Korea. Each hospital completed a predetermined clinical report form of the participants in each visit and recorded the data in the homepage of the CRESCEND (www.smileagain.or.kr) within 2 days.
The inclusion criteria for the study participants were 1) an age over 7 years and 2) a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV),20 diagnosis of MDD, dysthymic disorder, or depressive disorder, not other specified (NOS), as determined by a DSM-IV-based structured clinical interview.21 Exclusion criteria were 1) a current or lifetime comorbid DSM-IV diagnosis of schizophrenia, other psychotic disorders, bipolar disorders, organic psychosis, or dementia, and 2) a current or past history of any significant medical and neurological illnesses.
The consent form and the research protocol were approved by the respective university and/or hospital institutional review boards. All participants reviewed the informed consent form and signed in the presence of research staff before participating in the study.
Study design
The CRESCEND study included two phases, I and II, with a total of 9 follow-up years. The phase I study period was 1 year. In phase I, if the eligible participants entered the study at baseline, each participant visited the hospital and was assessed at 1, 2, 4, 8, 12, 24, and 52 weeks. The phase II study, an extension study from 1 year to 9 years (total 8 years), in which the participants will be evaluated annually.
At baseline, the participants underwent a diagnostic evaluation and a retrospective personal history of their medical or psychiatric illnesses and treatment. Also, a variety of socio-epidemiologic and clinical data were collected. The clinical, social, and functional outcomes associated with the treatment including clinician- and self-administered measures were evaluated at each visit.
The clinician-administered measures included the Clinical Global Impression scale (CGI),22 the 17-item Hamilton Depression Rating Scale (HDRS-17),23 the Hamilton Anxiety Rating Scale (HARS),24 the Brief Psychiatric Rating Scale (BPRS),25 and the Social and Occupational Functioning Assessment Scale (SOFAS).20
The CGI, which is widely used of extant brief assessment tolls in psychiatry, is a 7-point observer-rated scale that measures illness severity and global improvement or change. The HDRS-17 is the most widely used clinical-administered depression assessment scale. Each item pertains to symptoms of depression experienced over the past week. The HARS is a 14-item clinician-administered rating scale and provides an overall measure of the severity of global anxiety including psychic and somatic symptoms. The BPRS is an 18-item clinician-rated tool designed to assess change in severity of psychopathology. The items of the BPRS focus on symptoms that are common in psychotic disorder including schizophrenia and other psychotic disorders as well as those found in severe mood disorders. The SOFAS is a 100-point, single-item scale that rates functioning on a hypothetical continuum of mental health to mental illness. It focused on the individual's level of social and occupational functioning and is not directly influenced by psychological symptoms.
The self-administered measures consisted of the Beck Depression Inventory-Second Edition (BDI-II),26 the Scale for Suicide Ideation (SSI),27 and the World Health Organization Quality of Life assessment instruments-abbreviated version (WHOQOL-BREF).28
The BDI-II a 21-item self-report instrument intended to assess the existence and severity of symptoms of depression. It was revised in 1996 to be more consistent with DSM-IV criteria for depression than the original BDI. The SSI is a 21-item, 3-point Likert self-administered scale that asks about suicide ideation during the past week. The severity of suicide ideation is calculated by summing the rating for the first 19 items. The WHOQOL-BREF is a 26-item instrument to assess the quality of life, which measures the following broad domains: physical health, psychological health, social relationships, and environment. It is a shorter version of the original WHOQOL that may be more convenient for use.
Twice a year, the raters in each individual hospital participated in formal consensus meetings concerning the use of the rater-administered assessment instruments including the HDRS-17, the HARS, the BPRS, and the SOPAS. The consensus meetings consisted of an observation of the administration of the evaluations by an experienced supervisory psychiatrist and an actual administration via videotapes featuring standard MDD patients with or without psychotic features.
Statistical analysis
All data were presented as number (percentage) for categorical variables and as mean (standard deviation) for continuous variables. Descriptive statistics were used to characterize the study participants at baseline in Table 1 and 2. In Table 3, the chi-square test and unpaired t-test were conducted to compare the categorical and the continuous variables, respectively, between men and women. Also, to adjust for the differences in age between men and women, multivariate logistic regression and analysis of covariance methods were used for the categorical and the continuous variables, respectively. The statistical significance for all tests was set at p<0.05. All statistical analyses were conducted using Statistical Analysis System (SAS), version 9.1 (SAS Institute Inc., Cary, NC).
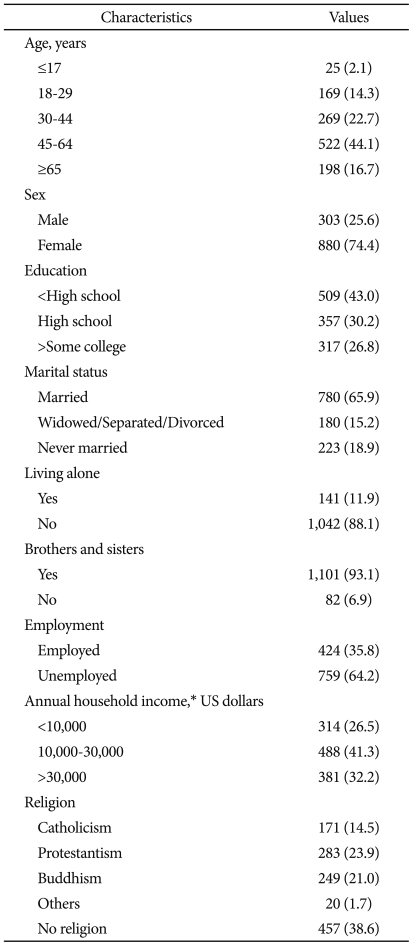
Table 1.
Socioepidemiologic characteristics at baselin
*cutoffs of 10,000 and 30,000 US dollars mean the approximate minimum and average costs of a family of 4 members, respectively, in 2006 in Korea (National Statistics Office, 2007)
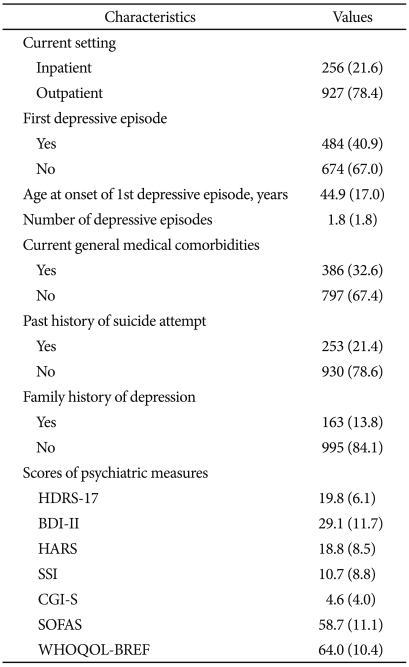
Table 2.
Clinical characteristics at baseline
HDRS-17: 17-item Hamilton Depression Rating Scale, BDI-II: Beck Depression Inventory-Second Edition, HARS: Hamilton Anxiety Rating Scale, SSI: Scale for Suicide Ideation, CGI-S: Clinical Global Impression scale-Severity, SOFAS: Social and Occupational Functioning Assessment Scale, WHOQOL-BREF: World Health Organization Quality of Life assessment instruments-abbreviated version
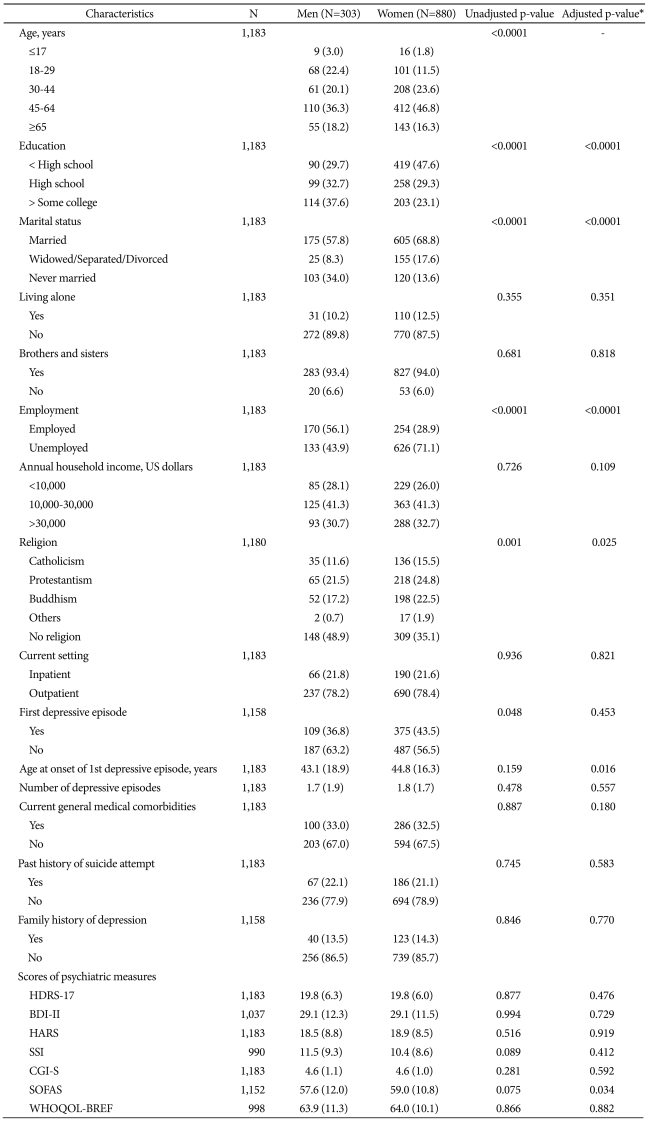
Table 3.
Gender differences of the baseline characteristics
*adjusted for age. HDRS-17: 17-item Hamilton Depression Rating Scale, BDI-II: Beck Depression Inventory-Second Edition, HARS: Hamilton Anxiety Rating Scale, SSI: Scale for Suicide Ideation, CGI-S: Clinical Global Impression scale-Severity, SOFAS: Social and Occupational Functioning Assessment Scale, WHOQOL-BREF: World Health Organization Quality of Life assessment instruments-abbreviated version
RESULTS
Sociodemographic characteristics
A total of 1,183 participants with depression were enrolled in this study. The sociodemographic characteristics of the participants at baseline are shown in Table 1. The mean±standard deviation of age and education levels in all participants were 47.9±15.9 year-old and 10.4±4.5 years, respectively. The age ranged between 11 and 83 years old. Fifty-nine participants (5.0%) were not educated at all. Overall, more women (74.4%) than men participated in the study. Among the 780 married participants, only 12 persons (1.5%) had remarried. Fifty-nine persons (6.1%) had no children among 960 participants who had been married. Nine hundred eighty-one participants (82.9%) had a diagnosis of MDD according to the DSM-IV criteria, among which only 24 persons had psychotic features at baseline. The participants who were diagnosed with dysthymic disorder or depressive disorder, NOS at baseline, were 38 (3.2%) and 164 (13.9%) persons, respectively.
Clinical characteristics
The clinical characteristics of the participants at baseline were summarized in Table 2. At baseline, most of the participants (83.8%) took one or more antidepressant medications. Forty-eight participants (4.1%) had 5 or more depressive episodes. The youngest and oldest ages of onset of the first depressive episode were 10 and 83 years old, respectively. The most frequent medical comorbidity was hypertension (178 persons, 15.0%). In the participants who had a past history of suicide attempts (253 persons, 21.4%), the mean±standard deviation number of suicide attempts and age at first suicide attempt were 2.1±2.7 and 31.0±13.8 year-old, respectively. Two hundred eighty participants (23.7%) had experienced adverse life events before the age of twelve, such as the death of the siblings and parents, sexual or physical abuse, the separation/divorce or economic crisis of the parents, natural disaster, and bullying.
Overall, the participants were moderately to severely ill (1,009 persons, 85.3%), based on CGI-severity. Only 29 depressive participants (2.5%) were in the remission state (HDRS-17 ≤7) at baseline. The mean±standard deviation scores of CGI-severity in MDD, dysthymic disorder and depressive disorder NOS were 4.7±1.0, 3.8±1.0, and 4.4±1.0, respectively. Also, the mean±standard deviation scores of HRDS-17 among the three groups were 20.2±6.0, 16.5±5.7, and 18.2±6.0, respectively.
Gender differences
Table 3 summarized gender differences with respect to the socioepidemiologic and clinical characteristics of the depressive participants at baseline. The mean age for women (48.8 years) was higher than that for men (45.5 years)(unadjusted p<0.0001). The gender groups differed in terms of education group (p<0.0001, adjusted for age). Women had fewer years of education (9.9 years) than men (11.9 years)(p<0.0001, adjusted for age). There was a significant gender difference in marital status (p<0.0001, adjusted for age). Widowed, separated, or divorced women were more than 7 times as prevalent in this sample as men having the same status. Employment status differed by gender (p<0.0001, adjusted for age). Among the unemployed women, 466 women (74.4%) were housewives. There was a significant difference in religion status by gender (p=0.025, adjusted for age): more men (48.9%) than women (35.1%) indicated a lack of religious beliefs.
The proportion of women (78.4%) and men (78.2%) who were recruited from the outpatient setting were similar. Women who had experienced their first depressive episode at baseline were more prevalent in this sample than men, but it was not significantly different after adjusting for age (p=0.453). Men had a somewhat earlier onset of their first depressive episode (mean of 43.1 years) than women (mean of 44.8 years, p= 0.016, adjusted for age). The proportions of women and men with respect to the number of depressive episodes and the presences of current general medical comorbidities, past history of suicide attempts, and family history of depression were similar. Also, mean scores of individual psychiatric measures at baseline did not differ by gender in this study.
DISCUSSION
The CRESCEND study is the first long-term prospective collaborative observational cohort study investigating the natural course and outcome of depressive patients to be conducted in Korea. The participants were enrolled in 18 hospitals from all over Korea and the distribution of participated hospitals reflected the spread of population in Korea. Though a number of naturalistic cohort studies of depression have been conducted all over the world (especially in the Western world), there are still numerous questions about the clinical and socioeconomic outcomes resulting from actual clinical and medical practices for depression; the results of those studies are difficult to extend to Eastern societies given broad ethnic and cultural differences. The CRESCEND study was designed to investigate the more long-term comprehensive outcomes of depression in order to overcome the limitations stated above. In this report we have described the research methodology of the CRESCEND study and reported the baseline findings from the depressive samples.
Some interesting baseline findings were found in the CRESCEND study.
Though the age distribution of this study was statistically normal, the child and adolescent depressive participants (≤17 year-old) were very few (2.1%), but the proportion of geriatric depressive participants (≥65 year-old) was relatively high (16.7%). This finding may be an artifact of methodological problems for specific age groups such as parental reluctance to permit children to participate in the study and indirectly, reflection of recent lower birth rate and more increased aged population in Korea. The female prevalence in this study was 74.4%. The gender ratio of 2.9 seen in women vs. men willing to enroll in this study is higher than that of several previous reports,2,29,30 but similar to that reported in the Korean Epidemiologic Catchment Area study.12 Though a higher female prevalence in depression study may indicate that women have greater tendency to seek treatment, or greater willingness to participate in the study,29 this finding may be influenced by the actual gender prevalence of depression in Korea. However, the ethnic or cultural differences of a heightened stigma of depression among men could be also considered.11
Several distinctive clinical findings of depression at baseline were revealed in the CRESCEND study. First, the mean age at onset of the first depressive episode in this study was 44.9 years old, which is higher than that of previous studies.31-33 Textbooks typically suggest a mean age of onset for depression of about 40 years. Considering that the mean age of enrolled participants was 47.9, which is also higher, compared to the previous studies, this finding may reflect a fact of depression in Korea. However, problems of the participants related to inadequate information and the social stigma about depression in the Korean society should not be overlooked. Second, among 1,183 depressive participants, 21.6% had a past history of one or more self-reported suicide attempts. This is higher than the prevalence of 16.5% found in the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study.34 The difference at baseline in the history of suicide attempts between the two studies may be mainly due to sampling procedures and settings, but it should be emphasized that Koreans have the highest rate of suicide among OECD countries. Thirdly, the prevalence of a family history of depression in this study was only 13.8%, which is lower than that of the previous studies.35,36 The family history of depression is an important factor for predicting the likelihood of a person having depression as well as the severity and outcome of depression.37 Some possible explanations of this finding may be 1) no use of a structured interview form to determine family history of depression, 2) lack of reliable information of depression in the participants' family, and 3) unwillingness to expose the history of familial depression due to the cultural stigma of depression.
In these baseline results, some gender differences noted among the depressive participants in socioepidemiologic data (e.g., higher education level in males, higher employment in males, and higher religion-seeking tendency in females) may be influenced in part by cultural gender differences in current Korean society. These findings were inconsistent compared to Western countries.29,38 Interestingly, no gender difference adjusted for age in past history of suicide attempts was found in this study. One of the most consistent research findings in the literature on suicide is that men have higher suicide rates than women, even though women make more suicide attempts than men.39 In Korea, one person every 90 seconds attempted suicide regardless of actual suicide success in 2003.40 This finding reflects the relative increase of suicide attempts in Korean depressive men, which might be related to increased psychosocial stress in men directly influenced by the recent economic crisis in Korea.41
This study has several limitations. While the cross-sectional observational methodology is useful for the better understanding of real-life clinical practice, there are limitations on the causal inferences that can be drawn due to uncontrollable confounding factors, selection bias, and reverse causality. Though the results of this study were cross-sectional and observational, the CRESCEND study itself was designed as a prospective cohort study. Thus, further analyses of the longitudinal data may overcome several limitations. In this study, nearly three-fourths of participants with depression were enrolled from outpatient settings. This fact may have resulted in a selection bias that influenced findings of symptom severity, the presence of psychotic symptoms, and the frequency of subtypes of depression including dysthymic disorder and depressive disorder NOS. Only 2.0 percent of depressive participants, all of whom were enrolled from the inpatient setting, had psychotic features. However, the differences in depressive symptom severity at baseline between inpatients and outpatients were not significant in this study.
The CRESCEND study is the first long-term hospital-based prospective collaborative observational cohort study investigating the in situ course and outcome of depressive participants to be conducted in Korea. In this cohort study, we will investigate the Korean-specific characteristics of depression including psychopathology, risk factors, clinical courses, and prognosis and establish the clinical evidences to develop the clinical practice guidelines for depression in the Korean society. A series of the results from the CRESCEND study will provide valuable information about real-life clinical practices for depression in Korea as well as the ethnic and cultural differences in depression between the East and the West.
Acknowledgments
This research was supported by a grant of the Korea Health 21 R&D, Ministry of Health and Welfare, Republic of Korea (A050047).
The list of 16 university hospitals and 2 general hospitals which participate in the CRESCEND study is below;
Affiliated hospitals of the Catholic University of Korea (Seoul St. Mary's Hospital, Seoul; St. Mary's Hospital, Seoul; Uijeongbu St. Mary's Hospital, Uijeongbu; Incheon St. Mary's Hospital, Incheon; St. Vincent's Hospital, Suwon); Chonnam National University Hospital, Gwangju; Chonnam National University Hwasun Hospital, Hwasun; Chosun University Hospital, Gwangju; Hanyang University Hospital, Guri; Inje University Pusan Paik Hospital, Busan; Kangwon National University Hospital, Chuncheon; Keimyung University Dongsan Medical Center, Daegu; Korea University Anam Hospital, Seoul; Sunchunhyang University Bucheon Hospital, Bucheon; Sunchunhyang University Hospital, Seoul; Sungkyunkwan University Kangbuk Samsung Hospital, Seoul; Bongseng Memorial Hospital, Busan; Maryknoll Medical Center, Busan.
References
- 1.Fava M, Cassano P. Mood Disorders: major depressive disorder and dysthymic disorder. In: Stern TA, Rosenbaum JF, Fava M, Biederman J, Rauch SL, editors. Massachusetts General Hospital Comprehensive Clinical Psychiatry. Philadelphia: Mosby; 2008. pp. 391–398. [Google Scholar]
- 2.Kessler RC, Berglund P, Demler O, Jin R, Koretz D, Merikangas KR, et al. The epidemiology of major depressive disorder: results from the National Comorbidity Survey Replication (NCS-R) JAMA. 2003;289:3095–3105. doi: 10.1001/jama.289.23.3095. [DOI] [PubMed] [Google Scholar]
- 3.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 4.Gelenberg A. Depression is still underrecognized and undertreated. Arch Intern Med. 1999;159:1657–1658. doi: 10.1001/archinte.159.15.1657. [DOI] [PubMed] [Google Scholar]
- 5.Bostwick JM, Pankratz VS. Affective disorders and suicide risk: a reexamination. Am J Psychiatry. 2000;157:1925–1932. doi: 10.1176/appi.ajp.157.12.1925. [DOI] [PubMed] [Google Scholar]
- 6.Greenberg PE, Kessler RC, Birnbaum HG, Leong SA, Lowe SW, Berglund PA, et al. The economic burden of depression in the United States: how did it change between 1990 and 2000? J Clin Psychiatry. 2003;64:1465–1475. doi: 10.4088/jcp.v64n1211. [DOI] [PubMed] [Google Scholar]
- 7.Katon WJ. Clinical and health services relationships between major depression, depressive symptoms, and general medical illness. Biol Psychiatry. 2003;54:216–226. doi: 10.1016/s0006-3223(03)00273-7. [DOI] [PubMed] [Google Scholar]
- 8.Murray CJ, Lopez AD. Global mortality, disability, and the contribution of risk factors: Global Burden of Disease Study. Lancet. 1997;349:1436–1442. doi: 10.1016/S0140-6736(96)07495-8. [DOI] [PubMed] [Google Scholar]
- 9.Murray CJ, Lopez AD. Alternative projections of mortality and disability by cause 1990-2020: Global Burden of Disease Study. Lancet. 1997;349:1498–1504. doi: 10.1016/S0140-6736(96)07492-2. [DOI] [PubMed] [Google Scholar]
- 10.Rush AJ. The varied clinical presentations of major depressive disorder. J Clin Psychiatry. 2007;68(Suppl 8):4–10. [PubMed] [Google Scholar]
- 11.Ballenger JC, Davidson JR, Lecrubier Y, Nutt DJ, Kirmayer LJ, Lépine JP, et al. Consensus statement on transcultural issues in depression and anxiety from the International Consensus Group on Depression and Anxiety. J Clin Psychiatry. 2001;62(Suppl 13):47–55. [PubMed] [Google Scholar]
- 12.Cho MJ, Kim JK, Jeon HJ, Suh T, Chung IW, Hong JP, et al. Lifetime and 12-month prevalence of DSM-IV psychiatric disorders among Korean adults. J Nerv Ment Dis. 2007;195:203–210. doi: 10.1097/01.nmd.0000243826.40732.45. [DOI] [PubMed] [Google Scholar]
- 13.Alonso J, Angermeyer MC, Bernert S, Bruffaerts R, Brugha TS, Bryson H, et al. Prevalence of mental disorders in Europe: results from the European Study of the Epidemiology of Mental Disorders (ESEMeD) project. Acta Psychiatr Scand Suppl. 2004:21–27. doi: 10.1111/j.1600-0047.2004.00327.x. [DOI] [PubMed] [Google Scholar]
- 14.Chen CN, Wong J, Lee N, Chan-Ho MW, Lau JT, Fung M. The Shatin community mental health survey in Hong Kong. II. Major findings. Arch Gen Psychiatry. 1993;50:125–133. doi: 10.1001/archpsyc.1993.01820140051005. [DOI] [PubMed] [Google Scholar]
- 15.Hwu HG, Chang IH, Yeh EK, Chang CJ, Yeh LL. Major depressive disorder in Taiwan defined by the Chinese diagnostic Interview Schedule. J Nerv Ment Dis. 1996;184:497–502. doi: 10.1097/00005053-199608000-00007. [DOI] [PubMed] [Google Scholar]
- 16.Kawakami N, Shimizu H, Haratani T, Iwata N, Kitamura T. Lifetime and 6-month prevalence of DSM-III-R psychiatric disorders in an urban community in Japan. Psychiatry Res. 2004;121:293–301. doi: 10.1016/s0165-1781(03)00239-7. [DOI] [PubMed] [Google Scholar]
- 17.Chang SM, Sohn JH, Lee JY, Choi JH, Cho SJ, Jeon HJ, et al. Characterstics and diagnostic criteria for depression in Korea. J Korean Neuropsychiatr Assoc. 2007;46:447–452. [Google Scholar]
- 18.Jung SH. The socioeconomic burden of suicide and depression in Korea. Seoul, Korea: National Center for Mental Health Research and Education; 2005. [Google Scholar]
- 19.Korea National Statistical Office. Annual report on the cause of death statistics of 2005. Seoul, Korea: 2006. [Google Scholar]
- 20.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV) Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 21.First MB, Spitzer RL, Gibbon M, Williams JB. User's Guide for the Structured Clinical Interview for DSM-IV Axis I Disorders Research Version (SCID-I) New York: New York State Psychiatric Institute, Biometrics Research; 1996. [Google Scholar]
- 22.Guy W. ECDEU Assessment Manual for Psychopharmacology, Revised. Rockville: National Institute of Mental Health; 1976. [Google Scholar]
- 23.Hamilton MA. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Hamilton MA. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32:50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- 25.Overall JE, Gorham DR. The Brief Psychiatric Rating Scale. Psychol Rep. 1962;10:779–812. [Google Scholar]
- 26.Beck AT, Steer RA, Brown GK. Manual for the Beck Depression Inventory-II. San Antonio, Tx: Psychological Corporation; 1996. [Google Scholar]
- 27.Beck AT, Kovacs M, Weissman M. Assessment of suicidal intention: The Scale for Suicide Ideation. J Consult Clin Psychol. 1979;47:343–352. doi: 10.1037//0022-006x.47.2.343. [DOI] [PubMed] [Google Scholar]
- 28.The WHOQOL., Group Development of the World Health Organization WHOQOL-BREF quality of life assessment. The WHOQOL Group. Psychol Med. 1998;28:551–558. doi: 10.1017/s0033291798006667. [DOI] [PubMed] [Google Scholar]
- 29.Marcus SM, Young EA, Kerber KB, Kornstein S, Farabaugh AH, Mitchell J, et al. Gender differences in depression: findings from the STAR*D study. J Affect Disord. 2005;87:141–150. doi: 10.1016/j.jad.2004.09.008. [DOI] [PubMed] [Google Scholar]
- 30.Weissman MM, Bland RC, Canino GJ, Faravelli C, Greenwald S, Hwu HG, et al. Cross-national epidemiology of major depression and bipolar disorder. JAMA. 1996;276:293–299. [PubMed] [Google Scholar]
- 31.Akerblad AC, Bengtsson F, von Knorring L, Ekselius L. Response, remission and relapse in relation to adherence in primary care treatment of depression: a 2-year outcome study. Int Clin Psychopharmacol. 2006;21:117–124. doi: 10.1097/01.yic.0000199452.16682.b8. [DOI] [PubMed] [Google Scholar]
- 32.Eaton WW, Shao H, Nestadt G, Lee HB, Bienvenu OJ, Zandi P. Population-based study of first onset and chronicity in major depressive disorder. Arch Gen Psychiatry. 2008;65:513–520. doi: 10.1001/archpsyc.65.5.513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: a STAR*D report. Am J Psychiatry. 2006;163:1905–1917. doi: 10.1176/ajp.2006.163.11.1905. [DOI] [PubMed] [Google Scholar]
- 34.Claassen CA, Trivedi MH, Rush AJ, Husain MM, Zisook S, Young E, et al. Clinical differences among depressed patients with or without a history of suicide attempts: findings from the STAR*D trial. J Affect Disord. 2007;97:77–84. doi: 10.1016/j.jad.2006.05.026. [DOI] [PubMed] [Google Scholar]
- 35.Husain MM, Rush AJ, Wisniewski SR, McClintock SM, Fava M, Nierenberg AA, et al. Family history of depression and therapeutic outcome: findings from STAR*D. J Clin Psychiatry. 2009;70:185–195. doi: 10.4088/jcp.07m03571. [DOI] [PubMed] [Google Scholar]
- 36.Sullivan PF, Wells JE, Joyce PR, Bushnell JA, Mulder RT, Oakley-Browne MA. Family history of depression in clinic and community samples. J Affect Disord. 1996;40:159–168. doi: 10.1016/0165-0327(96)00056-0. [DOI] [PubMed] [Google Scholar]
- 37.Weissman MM, Merikangas KR, Wickramaratne P, Kidd KK, Prusoff BA, Leckman JF, et al. Understanding the clinical heterogeneity of major depression using family data. Arch Gen Psychiatry. 1986;43:430–434. doi: 10.1001/archpsyc.1986.01800050028003. [DOI] [PubMed] [Google Scholar]
- 38.Dekker J, Koelen JA, Peen J, Schoevers RA, Gijsbers-van Wijk C. Gender differences in clinical features of depressed outpatients: preliminary evidence for subtyping of depression? Women Health. 2007;46:19–38. doi: 10.1300/j013v46n04_02. [DOI] [PubMed] [Google Scholar]
- 39.Kerkhof A. Attempt suicide: patterns and trends. In: Hawton K, Van Heeringen K, editors. The International Handbook of Suicide and Attempted suicide. Chichster: John & Wiley & Sons Ltd; 2000. pp. 49–64. [Google Scholar]
- 40.Lee DW, Kim MS, Lee MS. Community psychiatry approach to suicide prevention. Psychiatry Investig. 2006;3:51–56. [Google Scholar]
- 41.Khang YH, Lynch JW, Kaplan GA. Impact of economic crisis on cause-specific mortality in South Korea. Int J Epidemiol. 2005;34:1291–1301. doi: 10.1093/ije/dyi224. [DOI] [PubMed] [Google Scholar]