Abstract
Kinematic analysis, also commonly referred to as biomechanical analysis, of the swallow is used to measure movement of oropharyngeal structures over time. Two laboratory directors who have used kinematic analysis in their research collaborated to determine the feasibility of establishing agreement between two separate laboratories on measures of structural movements of the swallow. This report describes the process that was followed toward the goal of establishing measurement agreement. Under the direction of the laboratory directors, one research technician from each laboratory participated in a process that included initial meetings, training sessions, and pre- and post-training evaluation of reproducibility.
Because agreement on initial measures of structural movement demonstrated weak correlation on some measures, the research technicians trained together for approximately 6 hours. After training, statistical analyses indicated that (a) most Pearson correlations for measures of structural movements were greater than 0.80 and were highly statistically significant; (b) most percentages of absolute deviation were under 25%; and (c) most concordance coefficients were above .70. These statistics indicate that the two laboratories were able to increase their level of agreement in measuring selected structural movements of the swallow after a brief amount of training.
Factors affecting measurement agreement include image quality, establishment of rules for measuring, and the opportunity for regular discussions among research assistants and investigators from both laboratories.
Introduction
The most commonly used technique to observe the swallow, diagnose dysphagia, and develop a treatment plan for patients with impaired swallow function is the Modified Barium Swallow (MBS) procedure with videofluorography (VFG).1–3 Investigators in the area of deglutition and dysphagia also use this clinical tool in their research by measuring various aspects of the swallow from the recorded fluoroscopic image. A common measurement protocol is assessment of temporal measures of the movement of the bolus through the oral cavity, pharynx, and cervical esophagus as well as duration of specific events in the oropharyngeal swallow. Examples of temporal measures include durations of oral transit time, pharyngeal transit time, esophageal transit time, laryngeal closure, cricopharyngeal opening, and laryngeal elevation, as well as the temporal organization of these events.4–7 These measures have become the foundation for the assessment of different cohorts, such as head and neck cancer patients undergoing different types of primary treatment,8–11 stroke patients12 and non-patient volunteers.13,14 These measures have been use to evaluate the effects of intra-oral prostheses15 and bolus volume and age13 on swallowing function.
Kinematic or biomechanical analysis of structural movements critical to swallow has been developed as a method for characterizing swallow function.17 Kinematic analysis is used to mark the movements of specific oropharyngeal structures over time or at specific points in time from video-fluoroscopic studies. Although measurement algorithms vary, the general procedures for kinematic analysis are consistent across programs. Each video image of interest is digitized; after digitizing, points of interest can be marked on each video image. For most applications, regardless of which software package is used, the researcher will mark an anchor point (a stable, non-moving point in the image), an angle measuring the subject's head tilt relative to true vertical, and a reference distance. These elements are marked on each video image and used in conjunction to control for a subject's head and body movement in the vertical, A-P, and horizontal planes as well as to measure absolute distances of structural movement during the swallow. On each marked video image, the anchor point is adjusted to become the origin of the coordinate system by subtracting its actual x and y pixel values from each point in the digitized image. In this manner, the anchor point on each image always has the adjusted coordinates of (0,0), regardless of how much a subject might move in any plane. The subject's postural angle is also used to virtually rotate each individual digitized image so that the subject's head tilt is mathematically in line with true vertical. This adjustment simplifies calculation of anterior and vertical movement of structures and assures that structural movement is calculated relative to the vertebral column. Finally the reference distance is used to scale the marked points to actual size or to some relative value such as vertebral body units. Because the reference distance is marked on each digitized image, it also adjusts for any movement the subject might make during the study toward or away from the fluoroscope and corrects for differences in fluoroscopic magnification during the swallow. Structures of interest are then marked and calculated relative to the anchor point, angle of head tilt, and reference distance. Figure 1 illustrates an example of a marked image.
Figure 1.

Example of a marked image: lateral view from videofluoroscopy of swallow study with marked points identified including (1) anchor point; (2) postural angle; (3) reference distance (a U.S. penny in this image); (4) most anterior-superior aspect of the hyoid bone; (5) anterior-superior corner of the subglottic air column; (6) upper esophageal sphincter region (UES is closed in this image).
Because kinematic or biomechanical analysis is labor intensive and uses resources beyond those generally found in a swallowing clinic, this type of analysis in almost exclusively used in the research laboratory. Kinematic or biomechanical analysis of the swallow has been used to characterize the movement of specific anatomical structures,18–20 assess the effect of varying bolus volume21, 22 or age,23 evaluate specific patient populations,23–25 evaluate specific interventions26–28 and assess non-patient volunteers.29,30
The successful use of kinematic or biomechanical measures for research in multi-center studies hinges on the laboratories at the various centers having reliable measurement processes, so that data on these measures may be pooled for statistical analysis. The goal of this study was to investigate the feasibility of obtaining reproducible kinematic measures from two laboratories, and to define and assess the process of reaching such reproducibility. In order to determine the ability of two different laboratories to make similar measures of structural movements of the swallow, investigators from Northwestern University (NU) and the Medical College of Wisconsin (MCW) collaborated on this laboratory project.
Methods
The key participants in this study were the laboratory directors at Northwestern University (JL) and Medical College of Wisconsin (RS), as well as research technicians (BRP, MK) from each laboratory who were trained in the technical aspects of collecting and processing kinematic or biomechanical data. The laboratory personnel worked with the statistician (AWR) who calculated the reproducibility statistics at each step in the process. Measurements for analysis were made only by the two laboratory research technicians.
Selection of Kinematic Measures
Because of their joint interest in the swallowing function of head and neck cancer patients treated with chemoradiation, the laboratory directors (JAL and RS) chose to focus their kinematic measurements on those structures that contribute to the swallow disorders that are related to reduced oral intake in this population. Recent research indicated that limitations in oral intake and diet during the first year after cancer treatment with chemoradiation were significantly related to reduced laryngeal elevation and reduced upper esophageal sphincter (UES) opening.31 The laboratory directors therefore jointly chose the following measures for evaluation in this reproducibility study: maximum anterior and superior laryngeal displacements, maximum anterior and superior hyoid displacements, maximum UES opening width, and height and width of post-swallow bolus residue in the pyriform sinus. Width and height of post-swallow bolus residue in the pyriform sinus32 were chosen because post-swallow residue is an indicator of both reduced laryngeal elevation and reduced bolus movement through the UES.
Compilation and Assessment of the Initial Set of Images
One technician from each of the two laboratories met at NU to discuss the types of measures they usually make and to review videotape examples from NU's video library. The research technicians discussed how each would make the various measures as they reviewed tapes but did not train together on the actual measurement of any images. The research technicians digitized images of swallows from fifteen different dysphagic patients who were treated for cancer of the head and neck with chemoradiation and no surgical excision. All swallow examples were randomly selected from the modified barium swallow study video archives at the swallow physiology laboratories of Northwestern University and Medical College of Wisconsin. Examples of modified barium swallow studies from patients treated for cancer of the head and neck with chemoradiation and no surgical excision were selected because this patient population is of research interest to both laboratory directors. No swallow maneuvers or postures were used during any of the swallows measured in this study. The two research technicians did not have access to any patient information other than the fact that the subjects were treated with chemoradiotherapy and had no surgical intervention.
Each research technician measured the same swallow images independently in his or her own laboratory on his or her respective systems. NU used its system first reported in Logemann et al.21 and MCW used its system reported in Shaker et al.33 Measurements of maximum larynx anterior movement and elevation, maximum hyoid anterior movement and elevation, width of upper esophageal sphincter (UES) opening at maximum hyolaryngeal excursion, height of pyriform sinus residue, and width of pyriform sinus residue were completed by each laboratory from the same images. The directions for marking the images were:
larynx: mark a point at the anterior-superior corner of the tracheal air column;
hyoid: mark a point at the most anterior-superior aspect of the hyoid bone;
UES: draw a line between the anterior and posterior walls of the UES region at its narrowest width during maximum opening of the segment;
height of pyriform sinus residue: draw a vertical line from the uppermost point of the air-barium residue interface to the inferior surface of pyriform sinus tissue;
width of pyriform sinus residue: draw a horizontal line between the anterior and posterior surfaces of the pyriform sinus at the level of the air-barium residue interface.
These measurements were sent to the statistician for analysis. Statistical analysis of the data included Pearson correlation (high values are a necessary but not sufficient condition for reproducibility), absolute deviation as a percent of the mean, defined as the mean of the absolute value of the swallow-specific difference (between laboratories) in measures, divided by the average across laboratories (low percent absolute deviations indicate good reproducibility) and the Concordance Coefficient34 (concordance coefficients near 1.0 indicate the data lie on a 45 degree line through the origin—i.e. they are truly reproducible).
Training Based on the Results of the Initial Statistical Analyses
Because these two laboratories had never before collaborated, there were no expectations as to the level of agreement that would be observed in the initial statistical analysis. Since the initial statistical analysis (to be discussed later and presented in the Results section in Table 1) indicated weak correlation on some measures, the research technicians arranged meetings to work on training together to improve their measurement agreement. Rather than continuing to use two separate measurement systems, the laboratory directors agreed to use ImageJ, public domain software available on the NIH website (http://rsb.info.nih.gov/ij/). By using a common measurement system, the research technicians could train together outside their regular laboratories when they did not have access to their usual software. In addition, using the same measurement system would avoid errors that might potentially be caused by differences in measurement algorithms.
TABLE 1.
Summary of statistics for data from first measurement. Because the hyoid moves out of view under the mandible and cannot be measured for one of the swallows, hyoid anterior movement and hyoid elevation measures are based on 14 swallows. Pyriform sinus residue is not present on one of the swallows; therefore height and width of residue are based on 14 observations.
| Measurement (cm) | n | Pearson Correlation | Pearson p-Value | Mean Absolute Deviation (AD) (cm) | Mean of the two Laboratories' Measures (cm) | AD as % of the Mean | Lin's Concordance Coefficient |
|---|---|---|---|---|---|---|---|
| laryngeal anterior movement | 15 | .30 | .28 | 0.55 | 0.83 | 66% | 0.18 |
| laryngeal elevation | 15 | .56 | .028 | 1.52 | 2.04 | 75% | 0.30 |
| hyoid anterior movement | 14 | .85 | <.0001 | 0.49 | 0.58 | 85% | 0.68 |
| hyoid elevation | 14 | .90 | <.0001 | 0.83 | 1.68 | 49% | 0.59 |
| UES diameter | 15 | .91 | <.0001 | 0.13 | 1.06 | 12% | 0.86 |
| height of PS residue | 14 | .54 | .045 | 0.26 | 1.06 | 25% | 0.47 |
| width of PS residue | 14 | .43 | .13 | 0.35 | 1.05 | 33% | 0.25 |
The research technicians met at MCW and worked together marking the previously measured swallows for displacement and residue. They jointly remeasured 10 of the previously measured swallows for anterior and superior hyoid and laryngeal movements and UES diameter until they agreed on the measurements for these swallows, spending 4.2 hours of training time on this task. They also remeasured all of the previously measured images of pyriform sinus residue until they reached agreement, spending 1.7 hours of training time on this task.
The research technicians next jointly measured 5 new swallows for anterior and superior hyoid and laryngeal movement and UES diameter, and 5 new swallows for residue. They checked the resulting measures for agreement and discussed any measures that did not compare sufficiently. These judgments of agreement were for clarification of any problem measures; no data from this training session were subjected to statistical analysis. No measures were identified as being problematic after this training session.
Compilation and Assessment of the Follow-up Set of Images
A follow-up set of 15 new swallows was digitized for post-training measurement by the research technicians. These 15 new swallows were randomly selected from modified barium swallow studies archived at the swallow physiology laboratory at Northwestern University from 15 patients treated for cancer of the head and neck with chemoradiation with no surgical resection. As with the prior data set, the research technicians were blinded to any patient information other than the fact that the subjects were treated with chemoradiation and no surgery for head and neck cancer. Each research technician independently completed measurement of the same images using the ImageJ software at their own laboratory. After completing their independent measurements, the research technicians sent his or her measures to the statistician. The data were subjected to the same statistical analyses as were used as for the initial analysis.
Results
Table 1 summarizes the statistics for the measurements from the initial pretraining measurement. At the time the swallow images were digitized, the research technicians were not aware that on one swallow the hyoid bone moved out of view of the fluoroscope as it approached its maximum excursion. Pyriform sinus residue was not evident on another swallow. Therefore, only 14 samples were available for maximum hyoid anterior movement and elevation, and for height and width of pyriform sinus residue.
UES diameter had the strongest agreement between the laboratories with a Pearson correlation of .91, an absolute deviation of 12%, and a concordance coefficient of .86. Hyoid anterior movement and elevation also had high Pearson correlations but their concordance coefficients were less than .70. All other measures had much weaker correlation and concordance between the laboratories.
Table 2 summarizes the statistical analyses for the post-training follow-up swallows. For all measures other than UES diameter, the correlation coefficients increased (except for the two hyoid measures where the already high correlations decreased very slightly), the absolute deviations decreased and concordance coefficients increased. Prior to training, the correlation coefficients ranged from .30 to .91. After training, the correlation coefficients ranged from .60 to .93, with 5 out of 6 at .83 or above. The concordance coefficients for the 6 measures excluding UES diameter ranged from .18 to .68 prior to the training session; after training they ranged from .52 to .89, with 5 out of 6 at .82 or above. Training therefore resulted in a substantial improvement in inter-rater agreement for all measures except UES diameter. Ironically, UES diameter had the strongest Pearson correlation, the lowest absolute deviation, and the highest concordance coefficient prior to training. The correlation coefficient went from .91 at the first measurement to .07 after training. The concordance coefficient fell from .86 to .07.
TABLE 2.
Summary of statistics for post-training measurement.
| Measurement (cm) | n | Pearson Correlation | Pearson p-Value | Mean Absolute Deviation (AD) (cm) | Mean of the Two Laboratories' Measures (cm) | AD as % of the Two-Lab Mean | Lin's Concordance Coefficient |
|---|---|---|---|---|---|---|---|
| laryngeal anterior movement | 15 | .60 | .02 | 0.25 | 0.73 | 34% | 0.52 |
| laryngeal elevation | 15 | .91 | <.0001 | 0.35 | 2.26 | 16% | 0.83 |
| hyoid anterior movement | 15 | .83 | .0001 | 0.22 | 0.97 | 22% | 0.82 |
| hyoid elevation | 15 | .87 | <.0001 | 0.29 | 1.13 | 25% | 0.75 |
| UES diameter | 15 | .07 | .80 | 0.09 | 0.59 | 16% | 0.07 |
| height of PS residue | 15 | .94 | <.0001 | 0.20 | 1.10 | 19% | 0.88 |
| width of PS residue | 15 | .93 | <.0001 | 0.25 | 1.16 | 21% | 0.89 |
The research technicians felt that the reduction in measurement agreement observed for UES diameter was related to the difference in morphology between the images on which they had trained versus the images they measured post-training. The rule for marking UES diameter was to measure the UES region at the narrowest position during maximum opening. While the original set of images used for training had UES regions represented by an hourglass shape (Figure 2), the images used for independent post-training measurement had examples of rough irregular surfaces and air-filled regions that made the choice of marking position less than obvious (Figure 3). Therefore, the two research technicians did not always measure the same location for the UES, and inter-rater reliability dropped in comparison to the first set of measures.
Figure 2.

Example of hourglass shaped UES. Arrows indicate the narrowest aspect of the opened UES.
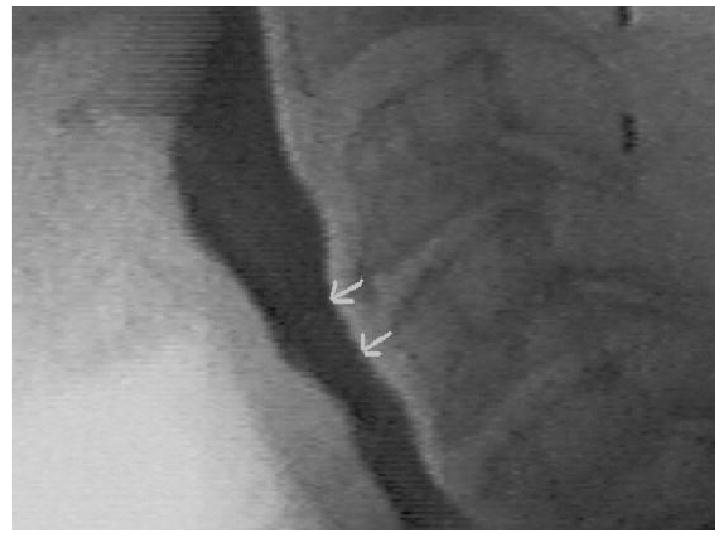
Figure 3.

Example of rough irregular surfaces in UES region. Arrows indicate the irregular surface along the anterior wall of the UES region.
Because of the reduced agreement on UES width, the laboratory directors decided to redefine the area for measurement of the UES. The research technicians were instructed to remeasure the UES region in two places: at the level of the anterior-inferior corner of C4 and at the level of the anterior-superior corner of C5. Figure 4 illustrates the redefined area for measurement of the UES. The research technicians independently remeasured the same 15 swallows used in the first post-training evaluation using the new definition for measuring the UES region, with the ImageJ software. The new measures were then sent to the project statistician for statistical analysis. Table 3 summarizes the reanalysis. After redefining of the location for measuring the UES diameter, the agreement between labs increased from a Pearson correlation of .07 and a concordance coefficient of .07 to a correlation of .72 and .84 and a concordance of .69 and .76 for locations C4 and C5 respectively.
Figure 4.
Revised marking of the UES region. Arrows indicate where the width of the UES is measured, at the level of the anterior-inferior corner of C4 and the level of the anterior-superior corner of C5.
TABLE 3.
Summary of statistics for remeasurement of UES diameter after redefinition of measurement location.
| Measurement (cm) | n | Pearson Correlation | Pearson p-Value | Mean Absolute Deviation (AD) (cm) | Mean of the Two Laboratories' Measures (cm) | AD as % of the Two-Lab Mean | Lin's Concordance Coefficient |
|---|---|---|---|---|---|---|---|
| UES diameter at level of anterior-inferior corner of C4 | 15 | .72 | .003 | 0.13 | 0.69 | 18% | 0.69 |
| UES diameter at level of anterior-superior corner of C5 | 15 | .84 | .009 | 0.10 | 0.65 | 15% | 0.76 |
Discussion
The feasibility of establishing measurement agreement between two laboratories for kinematic measures of the swallow was investigated in this study. Prior to any joint training, the measurement agreement between the two research technicians was weak on some measures. After a training period of approximately 6 hours, research technicians from two laboratories were able to reach a high level of reproducibility on the set of kinematic measurements that were studied. From the statistical analyses of the post-training data, the following observations were made: (a) most Pearson correlations were greater than 0.80 and were highly statistically significant; (b) most percentages of absolute deviation were under 25%; and (c) most concordance coefficients were above .70. These statistics indicate that after a relatively brief amount of training, two different laboratories were able to greatly improve their agreement in measuring selected structural movements of the swallow.
In order to establish measurement agreement, laboratory directors should set rules for measuring images, but not be reluctant to compromise or revise when necessary. Occasionally the rules cannot be followed; for example, the mandible may obscure the most anterior-superior aspect of the hyoid at its maximum excursion on a particular swallow. In such cases, the laboratory directors need to consider a compromise and mark another location in order to collect the necessary data. At other times, as in the difficulty encountered with measurement of the UES in this investigation, the rules for measurement must be revised in order to establish agreement. The research technicians were able to increase their measurement agreement for width of UES opening when they were provided with very detailed guidelines for the level at which the UES was to be measured.
When dealing with measurement agreement, laboratory directors and research technicians must be able to discuss deviations from the measurement rules. Laboratory directors and research technicians should view images together in order to discuss specific problems and troubleshoot solutions for measurement difficulties. When dealing with separate laboratories, especially at distant locations, maintaining regular contact can be a problem. Technologic innovations such as web conferencing for follow-up contact may improve the ability of separate facilities to collaborate on reliability training and maintenance of agreement.
Establishing and maintaining measurement agreement is a dynamic process. One cannot expect that agreement, once established, will be unchanging. It is imperative to regularly monitor agreement among research technicians. The raters must regularly reevaluate their agreement and retrain as needed; in addition, as new research technicians are recruited, they must also be trained until they achieve agreement with other research technicians, and then maintain that agreement. Whether personnel are in the same laboratory or in separate laboratories, interrater agreement needs to be established and then monitored regularly with retraining as needed when agreement falls below acceptable levels.
Head and neck cancer patients who were treated with chemoradiation were chosen as the focus for measurement in this study because this population is of particular interest to both the Laboratory Directors. The results of this investigation therefore may have limited generalizability to other dysphagic populations. However, the aim of this study was to determine the feasibility of cross-laboratory training of research technicians. Should other populations be of interest to laboratory directors at multiple laboratories that wish to collaborate, then the laboratory directors should focus training of their technicians with those particular populations.
There was only one research technician in each laboratory trained and available to perform the kinematic analysis technique for this investigation. University laboratories are subject to an ever-changing personnel profile as doctoral and postdoctoral students complete their studies, and as the number of regular employees fluctuates depending upon funding levels and availability of qualified candidates. Because research technicians may be limited in any individual laboratory, collaboration between laboratories is a useful method for increasing the number of research technicians available for data reduction and analysis. Establishing and maintaining measurement agreement between research technicians at separate laboratories is essential for successful collaboration.
Because kinematic or biomechanical analysis is labor-intensive and uses equipment and resources beyond those generally found in a clinical setting, this type of analysis in almost exclusively used in the research laboratory. Nevertheless, the results from kinematic analyses of the swallow may directly affect clinical practice. For example, kinematic analysis of the effects of various postures or maneuvers on the swallow can provide much-needed outcome data to support evidence-based practice. The information to be gained from kinematic or biomechanical analysis of the oropharyngeal swallow can be quite significant, therefore, in both research and clinical settings. This report on the feasibility of establishing measurement agreement for kinematic or biomechanical analysis indicates that agreement can be improved greatly between research technicians after only a few hours of training. Greater time committed to training should yield higher levels of agreement; sufficient time must be invested in training research technicians, either within a single laboratory or between laboratories if reliable data are to be obtained.
Acknowledgments
This research was supported by NIDDK R01DK62178 and NIH/NCI R01CA095576.
Contributor Information
Barbara Roa Pauloski, Department of Communication Sciences and Disorders, Northwestern University, Evanston, Illinois
Alfred W. Rademaker, Department of Preventive Medicine, Northwestern University Feinberg School of Medicine, Chicago, Illinois
Mark Kern, Division of Gastroenterology and Hepatology, Medical College of Wisconsin, Milwaukee
Reza Shaker, Division of Gastroenterology and Hepatology, Medical College of Wisconsin, Milwaukee
Jeri A. Logemann, Department of Communication Sciences and Disorders, Northwestern University, Evanston, Illinois
References
- 1.Logemann JA. Evaluation and treatment of swallowing disorders. 2nd. Austin, TX: Pro-Ed; 1998. [Google Scholar]
- 2.Cook IJ, Kahrilas PJ. AGA technical review on management of oropharyngeal dysphagia. Gastroenterology. 1999;116:455–478. doi: 10.1016/s0016-5085(99)70144-7. [DOI] [PubMed] [Google Scholar]
- 3.Martin-Harris B, Logemann JA, McMahon S, Schleicher M, Sandidge J. Clinical utility of the modified barium swallow. Dysphagia. 2000;15:136–141. doi: 10.1007/s004550010015. [DOI] [PubMed] [Google Scholar]
- 4.Kahrilas PJ, Dodds W, Dent J, Logemann J, Shaker R. Upper esophageal sphincter function during deglutition. Gastroenterology. 1988;95:52–62. doi: 10.1016/0016-5085(88)90290-9. [DOI] [PubMed] [Google Scholar]
- 5.Dodds WJ, Logemann JA, Stewart ET. Radiological assessment of abnormal oral and pharyngeal phases of swallowing. American Journal of Roentgenology. 1990;154:965–974. doi: 10.2214/ajr.154.5.2108570. [DOI] [PubMed] [Google Scholar]
- 6.Dodds WJ, Stewart ET, Logemann J. Physiology and radiology of the normal oral and pharyngeal phases of swallowing. American Journal of Roentgenology. 1990;154:953–963. doi: 10.2214/ajr.154.5.2108569. [DOI] [PubMed] [Google Scholar]
- 7.Shaker R, Dodds WJ, Dantas EO, Hogan WJ, Arndorfer RC. Coordination of deglutitive glottic closure with oropharyngeal swallowing. Gastroenterology. 1990;98:1478–1484. doi: 10.1016/0016-5085(90)91078-k. [DOI] [PubMed] [Google Scholar]
- 8.Logemann JA, Pauloski BR, Rademaker AW, McConnel FMS, Heiser MA, Cardinale S, Shedd D, Stein D, Beery Q, Johnson J, Saunders A, Baker T. Speech and swallow function after tonsil/base of tongue resection with primary closure. Journal of Speech Hearing Research. 1993;36:918–926. doi: 10.1044/jshr.3605.918. [DOI] [PubMed] [Google Scholar]
- 9.Pauloski BR, Logemann JA, Rademaker A, McConnel F, Heiser MA, Cardinale S, Shedd D, Lewin J, Baker S, Graner D, Cook B, Milianti F, Collins S, Baker T. Speech and swallowing function after anterior tongue and floor of mouth resection with distal flap reconstruction. Journal of Speech Hearing Research. 1993;36:267–276. doi: 10.1044/jshr.3602.267. [DOI] [PubMed] [Google Scholar]
- 10.Pauloski BR, Rademaker AW, Logemann JA, Colangelo LA. Speech and Swallowing in Irradiated and Nonirradiated Postsurgical Oral Cancer Patients. Otolaryngology—Head and Neck Surgery. 1998;118:616–624. doi: 10.1177/019459989811800509. [DOI] [PubMed] [Google Scholar]
- 11.Pauloski BR, Logemann JA, Colangelo LA, Rademaker AW, McConnel FMS, Heiser MA, Cardinale S, Shedd D, Stein D, Beery Q, Myers E, Lewin J, Haxer M, Esclamado R. Surgical Variables Affecting Speech in Treated Oral/Oropharyngeal Cancer Patients. Laryngoscope. 1998;108:908–916. doi: 10.1097/00005537-199806000-00022. [DOI] [PubMed] [Google Scholar]
- 12.Logemann JA, Shanahan T, Rademaker AW, Kahrilas PJ, Lazar R, Halper A. Oro-pharyngeal swallowing after stroke in the left basal ganglion/internal capsule. Dysphagia. 1993;8:230–234. doi: 10.1007/BF01354543. [DOI] [PubMed] [Google Scholar]
- 13.Rademaker AW, Pauloski BR, Colangelo LA, Logemann JA. Age and volume effects on liquid swallowing function in normal women. Journal of Speech Hearing Research. 1998;41:275–284. doi: 10.1044/jslhr.4102.275. [DOI] [PubMed] [Google Scholar]
- 14.Kern M, Bardan E, Arndorfer R, Hofmann C, Ren J, Shaker R. Comparison of upper esophageal sphincter opening in healthy asymptomatic young and elderly volunteers. Annals of Otology, Rhinology & Laryngology. 1999;108(10):982–989. doi: 10.1177/000348949910801010. [DOI] [PubMed] [Google Scholar]
- 15.Pauloski BR, Logemann JA, Colangelo LA, Stein D, Beery Q, Heiser MA, Cardinale S. Effect of intraoral prostheses on swallowing function in postsurgical oral and oropharyngeal cancer patients. American Journal of Speech-Language Pathology. 1996;5(3):31–46. [Google Scholar]
- 16.Ren J, Shaker R, Zamir Z, Dodds WJ, Hogan WJ, Hofmann C. Effect of age and bolus variables on the coordination of the glottis and upper esophageal sphincter during swallowing. American Journal of Gastroenterology. 1993;88(5):665–669. [PubMed] [Google Scholar]
- 17.Logemann JA, Kahrilas PJ, Begelman J, Dodds WJ, Pauloski BR. Interactive computer program for biomechanical analysis of videoradiographic studies of swallowing. American Journal of Roentgenology. 1989;153:277–280. doi: 10.2214/ajr.153.2.277. [DOI] [PubMed] [Google Scholar]
- 18.Kahrilas PJ, Logemann JA, Krugler C, Flanagan E. Volitional augmentation of upper esophageal sphincter opening during swallowing. American Journal of Physiology. 1991;260:G450–G456. doi: 10.1152/ajpgi.1991.260.3.G450. [DOI] [PubMed] [Google Scholar]
- 19.Logemann JA, Kahrilas PJ, Cheng J, Pauloski BR, Gibbons PJ, Rademaker AW, Lin S. Closure mechanisms of the laryngeal vestibule during swallowing. American Journal of Physiology. 1992;262:G338–344. doi: 10.1152/ajpgi.1992.262.2.G338. [DOI] [PubMed] [Google Scholar]
- 20.Fujiu M, Logemann JA, Pauloski BR. Increased post-operative pharyngeal wall movement in anterior oral cancer patients—preliminary findings and possible implications for potential therapy. American Journal of Speech-Language Pathology. 1995;4:24–30. [Google Scholar]
- 21.Kahrilas PJ, Lin S, Logemann JA, Ergun GA, Facchini F. Deglutitive tongue action: Volume accommodation and bolus propulsion. Gastroenterology. 1993;104:152–162. doi: 10.1016/0016-5085(93)90847-6. [DOI] [PubMed] [Google Scholar]
- 22.Kahrilas PJ, Lin S, Chen J, Logemann JA. Oropharyngeal accommodation to swallow volume. Gastroenterology. 1996;111:297–306. doi: 10.1053/gast.1996.v111.pm8690194. [DOI] [PubMed] [Google Scholar]
- 23.Bardan E, Kern M, Arndorfer RC, Hofmann C, Shaker R. Effect of age on bolus kinematics during the pharyngeal phase of swallowing. American Journal of Physiology, GI. 2006;290:458–465. doi: 10.1152/ajpgi.00541.2004. [DOI] [PubMed] [Google Scholar]
- 24.Logemann JA, Gibbons PJ, Rademaker AW, Pauloski BR, Kahrilas PJ, Bacon M, Bowman J, McCracken E. Mechanisms of recovery of swallow after supraglottic laryngectomy. Journal of Speech Hearing Research. 1994;37:965–974. doi: 10.1044/jshr.3705.965. [DOI] [PubMed] [Google Scholar]
- 25.Pauloski BR, Logemann JA, Fox JC, Colangelo LA. Biomechanical analysis of the pharyngeal swallow in post-surgical patients with anterior tongue and floor of mouth resection and distal flap reconstruction. Journal of Speech Hearing Research. 1995;38:110–123. doi: 10.1044/jshr.3801.110. [DOI] [PubMed] [Google Scholar]
- 26.Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA. Super-supraglottic swallow in irradiated head and neck cancer patients. Head Neck. 1997;19:535–540. doi: 10.1002/(sici)1097-0347(199709)19:6<535::aid-hed11>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 27.Logemann JA, Pauloski BR, Colangelo LA. Light digital occlusion of the tracheostomy tube: a pilot study of effects on aspiration and biomechanics of the swallow. Head Neck. 1998;20:52–57. doi: 10.1002/(sici)1097-0347(199801)20:1<52::aid-hed8>3.0.co;2-2. [DOI] [PubMed] [Google Scholar]
- 28.Shaker R, Easterling C, Kern M, Nitschke T, Massey B, Daniels S, Grande B, Kazandjian M, Dikeman K. Rehabilitation of swallowing by exercise in tube-fed patients with pharyngeal dysphagia secondary to abnormal UES opening. Gastroenterology. 2002;122(5):1314–1321. doi: 10.1053/gast.2002.32999. [DOI] [PubMed] [Google Scholar]
- 29.Logemann JA, Pauloski BR, Rademaker AW, Colangelo LA, Kahrilas PJ, Smith CH. Temporal and biomechanical characteristics of oropharyngeal swallow in younger and older men. Journal of Speech, Language, and Hearing Research. 2000;43:1264–1274. doi: 10.1044/jslhr.4305.1264. [DOI] [PubMed] [Google Scholar]
- 30.Logemann JA, Pauloski BR, Rademaker AW, Kahrilas PJ. Oropharyngeal swallow in younger and older women: Temporal and biomechanical characteristics. Journal of Speech and Hearing Research. 2002;45:434–445. doi: 10.1044/1092-4388(2002/034). [DOI] [PubMed] [Google Scholar]
- 31.Pauloski BR, Rademaker AW, Logemann JA, Newman L, MacCracken E, Gaziano J, Stachowiak L. Relationship between swallow motility disorders on VFG and oral intake in patients treated for head and neck cancer with radiotherapy ± chemotherapy. Head and Neck. 2006;28:1069–76. doi: 10.1002/hed.20459. [DOI] [PubMed] [Google Scholar]
- 32.Logemann JA, Williams RB, Rademaker AW, Pauloski BR, Lazarus CL, Cook I. The relationship between observations and measures of oral and pharyngeal residue from videofluorography and scintigraphy. Dysphagia. 2005;20:226–231. doi: 10.1007/s00455-005-0019-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shaker R, Kern M, Bardan E, Taylor A, Stewart ET, Hoffman RG, Arndorfer RC, Hofmann C, Bonnevier J. Augmentation of deglutitive upper esophageal sphincter opening in the elderly by exercise. American Journal of Physiology. 1997;272(6 Pt 1):G1518–G1522. doi: 10.1152/ajpgi.1997.272.6.G1518. [DOI] [PubMed] [Google Scholar]
- 34.Lin LI. A concordance correlation coefficient to evaluate reproducibility. Biometrics. 1989;45:255–268. [PubMed] [Google Scholar]


