Abstract
Background and Purpose
This study examines the independent effect of wealth, income, and education on stroke and how these disparities evolve throughout middle and old age in a representative cohort of older Americans.
Methods
Stroke-free participants in the Health and Retirement Study (n = 19 565) were followed for an average of 8.5 years. Total wealth, income, and education assessed at baseline were used in Cox proportional hazards models to predict time to stroke. Separate models were estimated for 3 age-strata (50 to 64, 65 to 74, and ≥75), and incorporating risk factor measures (smoking, physical activity, body mass index, hypertension, diabetes, and heart disease).
Results
1542 subjects developed incident stroke. Higher education predicted reduced stroke risk at ages 50 to 64, but not after adjustment for wealth and income. Wealth and income were independent risk factors for stroke at ages 50 to 64. Adjusted hazard ratios comparing the lowest decile with the 75th–90th percentiles were 2.3 (95% CI 1.6, 3.4) for wealth and 1.8 (95% CI 1.3, 2.6) for income. Risk factor adjustment attenuated these effects by 30% to 50%, but coefficients for both wealth (HR=1.7, 95% CI 1.2, 2.5) and income (HR=1.6, 95% CI 1.2, 2.3) remained significant. Wealth, income, and education did not consistently predict stroke beyond age 65.
Conclusions
Wealth and income are independent predictors of stroke at ages 50 to 64 but do not predict stroke among the elderly. This age patterning might reflect buffering of the negative effect of low socioeconomic status by improved access to social and health care programs at old ages, but may also be an artifact of selective survival.
Keywords: socioeconomic factors, education, income, stroke, aged
Previous studies indicate that lower socioeconomic status is associated with higher stroke risk in many developed countries.1–3 Although ≈89% of strokes occur after age 65,4 little is known about how socioeconomic status influences stroke risk in the elderly. Available studies in older populations have yielded mixed results, partially because of the limited socioeconomic status measures available, and, in the US studies, the use of small, geographically localized samples.1
In the US, stroke disparities across education and income seem to reverse at age 74, resulting in excess stroke among those with high education or income.1 Several explanations may account for this pattern: First, the negative impact of low socioeconomic status on stroke may diminish because of old-age entitlement programs such as Medicare. However, this hypothesis is not supported by findings from European populations, where socioeconomic disparities in stroke remain up to old ages despite the fact that access to care is universal.2 This age-attenuation may also be an artifact of selective survival,5,6 yet the role of this mechanism remains controversial.7 A third explanation is that conventional socioeconomic status measures such as education and income are not adequate socioeconomic status measures in the very old, and may not fully represent the resources available to these individuals. In contrast, wealth more comprehensively reflects both lifelong earnings and intergenerational transfers, and wealth increases access to medical care and other material and psychosocial resources.6–8 Elderly individuals frequently have little income but substantial wealth.9 Thus, disparities in stroke by income or education may underestimate the true impact of socioeconomic status on stroke at old age. Wealth remains associated with several health outcomes through late life,6 but whether wealth remains associated with stroke at old age is unknown.
Based on follow-up data from the Health and Retirement Study (HRS), we examined the independent effects of wealth, income, and education on incidence of first stroke across age strata. Additionally, we assessed the role of cardiovascular risk factors in explaining stroke disparities in US adults. We hypothesized that wealth predicts stroke incidence independently of income and education, and that this effect persists among the oldest old. To our knowledge, this is the first study assessing the age patterning of wealth, income, and education disparities in stroke in a representative sample of older Americans.
Methods
Study Population
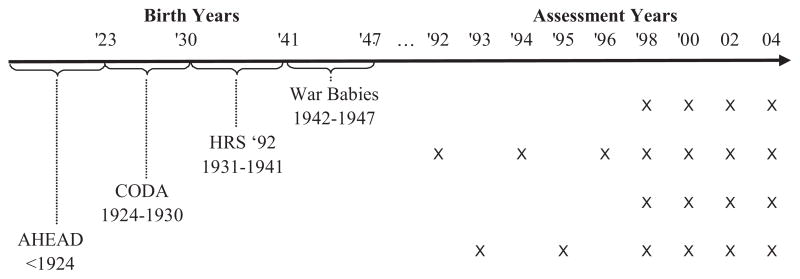
HRS is a longitudinal survey of a national sample of US adults aged 50 or older and their spouses. Details of the study are provided elsewhere.10 The HRS sample is selected using a multi-stage area probability sample design. Enrolment was staggered by birth cohort with enrolments in 1992, 1993, and 1998 (Figure). Response rates were high and ranged from 70% for the 1942 to 1947 birth cohort enrolled in 1998, to a high of 82% for the 1931 to 1941 birth cohort enrolled in 1992, without major differences by demographic factors. The majority of baseline interviews were face-to-face. Biennial interviews (or proxy interviews for decedent participants) were conducted through 2004, with wave-to-wave retention rates being around 90%. We included all HRS participants born 1900 to 1947 who were aged 50-plus and stroke-free at baseline interview.
Figure.
Enrolment and assessment schedule for Health and Retirement Study birth cohorts. Each title refers to a specific cohort that makes part of the total cohort; AHEAD indicates Aging and health dynamics cohort; CODA indicates Children of the Depression cohort; HRS indicates Health and Retirement survey original cohort; and War Babies refers to the cohort born during the second world war (1942 to 1947).
From 22 672 age-eligible respondents interviewed at baseline, we excluded 1074 (4.7%) prevalent stroke cases and 323 (1.4%) with unknown stroke status at enrolment; 539 (2.4%) without follow-up information; and 1291 (5.7%) with missing values on adult risk factors, for a total sample of 19 445 (1542 stroke events). There was no evidence of systematic differences in missing stroke status by socioeconomic status.
Socioeconomic Status
Household wealth, household income, and education were used as indicators of socioeconomic status. Household wealth comprised the sum of all financial and housing wealth minus liabilities of all members of the household. Household income comprised information on annual earnings by all household members. Missing items for household income and wealth were imputed with hot-decking procedures.11
The consumption needs of a household grow with each additional member, eg, a household with 2 members needs more income than a household with only 1 member. However, this increase does not occur in a proportional way, as consumption needs for each additional member decrease gradually.12 To take this into account, we divided income and wealth values by the square root of the number of household members.12 As expected, the distribution of income and wealth was substantially skewed. Therefore, we reclassified income and wealth values into 4 groups of equal size (quartiles) so that one fourth of the population was in each group, breaking the top and bottom groups into 2 separate categories (<10th, 10 to 24th, 25 to 49th, 50 to 74th, 75 to 89th, and ≥90th). This was done to explore nonlinearity at the extremes of the distribution and to avoid that outliers at the top or bottom of the wealth and income distribution would bias results. The 75 to 89th percentile group was treated as the reference category because it represents those in the highest wealth or income groups but excluding possible outliers among the very rich (<10th), thus providing a better estimate of differences in stroke risk by wealth or income. Applying a different categorization (eg, only quartiles) or using a different reference category (eg, the >90th percentile) did not change our results. In supplementary models, we used the ln of income and wealth as continuous variables. Education was coded as continuous years of schooling completed (up to 17 years), as well as using educational qualifications into 5 categories (no degree; high-school diploma/general educational development (GED) diploma; associate’s degree; bachelor’s degree; or master’s/professional degree).
Confounders and Intermediary Variables
All models were adjusted for potential confounders temporally before the exposure of interest, including: Hispanic ethnicity, black race, age at first interview (linear and quadratic terms), sex, region of birth (South, Northeast, Midwest, West, non-US, missing), mother’s education (<8 years, > = 8 years, missing), father’s education (<8 years, > = 8 years, missing), father’s occupation (professional/managerial, white collar, skilled manual, unskilled manual, military, farming, missing), and retrospective report of childhood health (5 point scale from poor to excellent, missing). We adjusted for childhood health because it can influence wealth, income, and education in adulthood, and is thus a potential confounder.
Potential mediators of the association between socioeconomic status and stroke included first available report of: present smoking status, body mass index (BMI), vigorous physical activity (dichotomized at 3+ times a week), and hypertension, diabetes, and heart disease (based on baseline self-report of a doctor’s diagnosis of these conditions).
Stroke Outcomes
Incident events were defined as first nonfatal or fatal strokes. Strokes were ascertained by self-report of doctor’s diagnosis or proxy reports for deceased participants. This approach has been shown to provide accurate estimates of stroke ocurrence.13 Reports of transient ischemic attacks were not coded as strokes because their symptoms are short and are typically not conceived as full strokes in incident studies. At each assessment, the month and year of stroke were recorded, except for 1994 interviews, when only year was ascertained. For these events, we assigned the most likely month of occurrence based on the study interview schedule and the distribution of event timing observed in other waves. 1992 strokes were assigned December, because we expect them to have occurred after the 1992 interview late that year; April was assigned to 1993 strokes based on the distribution of event timing observed in other waves; and January was assigned for 1994 strokes, because we expect they occurred before the 1994 interview wave. For some cases (n = 303), only the 2-year interval in which the stroke occurred was known. For these cases, we assigned the median stroke date for events reported by other participants in the same 2-year interval. Sensitivity analyses assigning interview dates as stroke dates for these cases did not change results.
Methods of Analysis
Cox proportional hazard models were fitted using wealth, income, and education to predict incident stroke, after confounder adjustment. Survival was defined as time from baseline interview to date of first stroke, date of proxy report of death attributable to other causes, or last interview date. Analyses were stratified into 3 age groups representing critical life-course stages: 50 to 64, 65 to 74, and ≥75. Income, wealth, and education were first modeled separately and then simultaneously incorporated into combined socioeconomic status models to estimate their independent effects. Finally, cardiovascular risk factors were added to the combined models to assess their contribution to stroke disparities. Analyses were conducted using SAS 9.1.
Results
Participant characteristics are summarized in Table 1. During an average of 8.5 years, 1542 subjects developed stroke. Education, wealth, and income tended to be lower among sample members with stroke events, who were also more likely to report hypertension, diabetes, and heart disease at baseline. Participants in the youngest group (50 to 64) experienced 460 events per 100 000 person-years; the rate more than doubled to 1245 in those aged 65 to 74 and 2161 in those aged 75 and older. The 3 socioeconomic indicators were correlated, but the magnitude of these correlations was modest. Pearson coefficients were 0.30 (P< 0.001) for the correlation between years of education and income; 0.25 (P< 0.001) for education and wealth; and 0.56 (P< 0.001) for the correlation between wealth and income. As compared to men, women in HRS had generally less education, income, and wealth (results not shown).
Table 1.
Characteristics of Health and Retirement Survey Participants, for All Eligible Sample Members and Participants Who Reported an Incident Stroke
| Eligible Sample |
Sample Members With Events |
|||
|---|---|---|---|---|
| n/mean | %/(std) | n/mean | %/(std) | |
| n | 19 445 | 100 | 1542 | 100 |
| Mean years of follow-up (std) | 8.5 | (3.3) | 5.6 | (3.1) |
| Mean years of education (std) | 11.9 | (3.3) | 11.2 | (3.4) |
| Education credentials | ||||
| No degree | 5554 | 29 | 600 | 39 |
| High school/GED | 10 016 | 52 | 722 | 47 |
| Associates | 603 | 3 | 38 | 2 |
| Bachelors | 1886 | 10 | 105 | 7 |
| Masters/professional | 1386 | 7 | 77 | 5 |
| Median wealth (interquartile range)* | 67 175 | (137 717) | 49 300 | (108 857) |
| Median income (interquartile range)* | 19 224 | (24 285) | 14 004 | (17 096) |
| Age at enrollment | ||||
| 50–64 | 11 640 | 60 | 613 | 40 |
| 65–74 | 4952 | 25 | 465 | 30 |
| 75+ | 2853 | 15 | 464 | 30 |
| Male | 8540 | 44 | 666 | 43 |
| Black | 2813 | 14 | 270 | 18 |
| Hispanic ethnicity | 1444 | 7 | 107 | 7 |
| Birth regions | ||||
| Northeast | 3478 | 18 | 267 | 17 |
| West | 1972 | 10 | 171 | 11 |
| Midwest | 4997 | 26 | 361 | 23 |
| South | 6851 | 35 | 651 | 42 |
| Not US | 891 | 5 | 39 | 3 |
| Unknown | 1256 | 6 | 53 | 3 |
| Mother’s education | ||||
| <8 years | 8047 | 41 | 888 | 58 |
| 8+ years | 9384 | 48 | 444 | 29 |
| Unknown | 2014 | 10 | 210 | 14 |
| Father’s education | ||||
| <8 years | 8499 | 44 | 928 | 60 |
| 8+ years | 8257 | 42 | 370 | 24 |
| Unkown | 2689 | 14 | 244 | 16 |
| Father’s occupation† | ||||
| Unskilled laborer (3) | 3633 | 19 | 290 | 19 |
| Skilled labor (2) | 3391 | 17 | 265 | 17 |
| White collar (1) | 1641 | 8 | 112 | 7 |
| Managerial/professional (0) | 2012 | 10 | 134 | 9 |
| Farming | 4073 | 21 | 361 | 23 |
| Unknown | 4564 | 23 | 375 | 24 |
| Mean childhood health†† (std) | 1.8 | (1.0) | 2.0 | (1.1) |
| Hypertension | 8236 | 42 | 899 | 58 |
| Diabetes | 2210 | 11 | 322 | 21 |
| Heart disease | 3465 | 18 | 465 | 30 |
| Current smoker | 4022 | 21 | 340 | 22 |
| Vigorous activity | 5091 | 26 | 329 | 21 |
| Mean body mass index (std) | 26.8 | (5.0) | 27.0 | (5.4) |
Sample members were all stroke-free at baseline.
Income and wealth values are standardized by dividing by the square root of household size.
Father’s occupation=army is not shown separately because of small cell counts.
Childhood health ranges from 1 (excellent) to 5 (poor).
Ages 50 to 64 Years
The impact of wealth, income, and education on stroke differed across age-strata (Table 2). At ages 50 to 64, higher education predicted lower risk of stroke (HR=0.94, 95% CI: 0.92 to 0.97), but education coefficients were nonsignificant after adjustment for income and wealth. In this young age-group, wealth was strongly associated with stroke incidence. Those in the lowest 10% of wealth had a 3-fold higher risk than those in the 75 to <90th percentile (HR=3.1, 95% CI 2.1, 4.4). This effect was modestly attenuated but remained significant after adjustment for other socioeconomic status indicators (HR=2.3 95% CI 1.6, 3.4). Income was associated with stroke in the basic models. However, after adjustment for wealth and education, the estimated coefficient for income was largely attenuated and only significant for the lowest decile (HR=1.8, 95% CI 1.3, 2.6). Similar results were observed for men and women (results not shown).
Table 2.
The Association of Wealth, Income and Education With Stroke Incidence Among Health and Retirement Survey Participants Aged ≥50 by Age-Strata
| Separate Socioeconomic Status Models* |
Combined Socioeconomic Status Models† |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 50 to 64 |
65 to 74 |
75+ |
50 to 64 |
65 to 74 |
75+ |
|||||||
| HR | (95% CI) | HR | (95% CI) | HR | (95% CI) | HR | (95% CI) | HR | (95% CI) | HR | (95% CI) | |
| Wealth | ||||||||||||
| Lowest 10% | 3.1 | (2.1, 4.4) | 1.4 | (0.9, 2.1) | 1.1 | (0.8, 1.7) | 2.3 | (1.6, 3.4) | 1.1 | (0.7, 1.7) | 1.0 | (0.7, 1.6) |
| 10–<25%ile | 2.2 | (1.6, 3.1) | 1.3 | (0.9, 1.8) | 1.3 | (0.9, 1.9) | 1.8 | (1.3, 2.6) | 1.0 | (0.7, 1.5) | 1.2 | (0.8, 1.8) |
| 25–<50%ile | 2.0 | (1.5, 2.8) | 1.2 | (0.9, 1.6) | 1.3 | (0.9, 1.7) | 1.9 | (1.3, 2.6) | 1.0 | (0.7, 1.4) | 1.2 | (0.8, 1.6) |
| 50–<75%ile | 1.0 | (0.7, 1.5) | 1.1 | (0.8, 1.5) | 1.2 | (0.9, 1.6) | 1.0 | (0.7, 1.4) | 1.0 | (0.8, 1.4) | 1.1 | (0.8, 1.6) |
| 75–<90%ile | reference | reference | ||||||||||
| Top 10% | 0.9 | (0.6, 1.5) | 0.9 | (0.6, 1.2) | 1.0 | (0.6, 1.5) | 1.0 | (0.6, 1.6) | 0.9 | (0.6, 1.3) | 1.1 | (0.7, 1.7) |
| Income | ||||||||||||
| Lowest 10% | 2.7 | (2.0, 3.7) | 1.9 | (1.2, 3.0) | 1.2 | (0.7, 2.0) | 1.8 | (1.3, 2.6) | 1.7 | (1.0, 2.8) | 1.1 | (0.6, 2.0) |
| 10–<25%ile | 1.9 | (1.4, 2.6) | 1.5 | (1.0, 2.2) | 1.7 | (1.1, 2.7) | 1.3 | (0.9, 1.9) | 1.3 | (0.9, 2.0) | 1.6 | (1.0, 2.6) |
| 25–<50%ile | 1.6 | (1.2, 2.1) | 1.5 | (1.0, 2.1) | 1.3 | (0.8, 2.0) | 1.2 | (0.9, 1.7) | 1.3 | (0.9, 2.0) | 1.2 | (0.8, 2.0) |
| 50–<75%ile | 1.3 | (1.0, 1.7) | 1.0 | (0.7, 1.5) | 1.3 | (0.8, 2.1) | 1.2 | (0.9, 1.5) | 0.9 | (0.6, 1.4) | 1.2 | (0.7, 2.0) |
| 75–<90%ile | reference | reference | ||||||||||
| Top 10% | 0.9 | (0.6, 1.3) | 1.2 | (0.8, 2.0) | 1.0 | (0.5, 2.0) | 1.0 | (0.6, 1.5) | 1.3 | (0.8, 2.1) | 1.0 | (0.5, 2.0) |
| Education credential | ||||||||||||
| No degree | 1.4 | (1.1, 1.7) | 1.1 | (0.9, 1.4) | 1.2 | (0.9, 1.4) | 1.1 | (0.9, 1.4) | 1.0 | (0.8, 1.3) | 1.1 | (0.9, 1.4) |
| High school/GED | reference | reference | ||||||||||
| Associates degree | 1.1 | (0.7, 1.7) | 1.0 | (0.5, 1.9) | 1.1 | (0.5, 2.2) | 1.2 | (0.8, 1.9) | 1.0 | (0.5, 2.0) | 1.1 | (0.5, 2.2) |
| Bachelor’s degree | 0.9 | (0.7, 1.2) | 0.7 | (0.5, 1.0) | 1.0 | (0.7, 1.5) | 1.1 | (0.8, 1.5) | 0.7 | (0.5, 1.1) | 1.1 | (0.7, 1.7) |
| Masters/professional | 0.7 | (0.5, 1.1) | 0.9 | (0.6, 1.4) | 1.2 | (0.7, 1.8) | 0.9 | (0.6, 1.4) | 1.0 | (0.6, 1.5) | 1.3 | (0.8, 2.1) |
| Years of education | 0.94 | (0.92, 0.97) | 0.97 | (0.94, 1.00) | 0.99 | (0.96, 1.02) | 0.99 | (0.96, 1.02) | 0.99 | (0.95, 1.03) | 1.00 | (0.97, 1.04) |
Separate socioeconomic status models are adjusted for: age, age-squared, male, black, Hispanic, birth regions (northeast, west, Midwest, south, not US, unknown), father’s occupation (professional/managerial, white collar, skilled manual, unskilled manual, farming, military, or unknown), mother’s education (<8 years, 8+ years, unknown), father’s education (<8 years, 8+ years, unknown), and self-reported childhood health. Each of the 3 models includes measures for only a single dimension of socioeconomic status.
Combined socioeconomic status models are adjusted for the above confounders and include education, income categories, and wealth categories in the same model.
HR indicates hazard ratio; 95% CI indicates 95% confidence interval; GED indicates General Education development.
Range for annual income percentiles are: <10th percentile (<$5657); 10 to 24th percentile ($5657 to $10 521); 25 to 49th percentile ($10 522 to $19 699); 50 to 74th percentile ($19 700 to $35 504); 75 to 89th percentiles ($35 505 to $56 992) and ≥90th percentile (≥$56 993).
Range for wealth percentiles are: <10th percentile (<$1000); 10 to 24th percentile ($1000 to $20 999); 25 to 49th percentile ($21 000 to $67 260); 50 to 74th percentile ($67 261 to $161 299); 75 to 89th percentiles ($162 300 to $344 499) and ≥90th percentile (≥$344 499).
Ages 65 Years or Older
Above age 65, wealth was no longer significantly associated with stroke risk. This pattern remained unchanged after adjustment for education and income (Table 2), and applied to both men and women (results not shown). A decline in the effect of income on stroke was also observed at older ages. After adjustment for education and wealth, the risk associated with low income was only significant for the lowest decile at ages 65 to 74 (HR=1.7, 95% CI 1.0, 2.8), and for the 10 to <25th income percentile group at ages 75 or over (HR=1.6, 95% CI 1.0, 2.6) (Table 2), but sex-stratified models indicated that these effects were only evident among men. Income did not predict stroke in women or in other income categories in either sex beyond age 65 (results not shown). Education was not a significant predictor of stroke beyond age 65. To test whether the apparent age-attenuation was statistically significant, we tested for interactions between age and (continuous) log income, log wealth, and education; in all cases the interaction terms were statistically significant (P<0.01) and indicated that the relative risk associated with low socioeconomic status declined with age.
The Role of Risk Factors
At ages 50 to 64 and 65 to 74, lower wealth, income, and education were associated with higher prevalence of hypertension, smoking, low physical activity, BMI, diabetes, and heart disease. At ages 75+ associations were less consistent, but at least 1 of the socioeconomic status indicators predicted hypertension, physical activity, BMI, and heart disease (results not shown). Among participants ages 50 to 64, cardiovascular risk factor adjustment attenuated wealth and income disparities in stroke by 30% to 50% (Table 3). However, a significantly increased stroke risk remained for all categories of wealth below the median and for the lowest income decile (HR=1.6, 95% CI 1.2, 2.3). Coefficients for education were not statistically significant after adjustment for wealth and income, and hazard ratios were unchanged after adjustment for cardiovascular risk factors.
Table 3.
The Association of Wealth, Income, and Education With Stroke Incidence After Adjustment for Cardiovascular Risk Factors Among Health and Retirement Survey Participants Aged ≥50 Years
| 50 to 64 |
65 to 74 |
75+ |
||||
|---|---|---|---|---|---|---|
| HR | (95% CI) | HR | (95% CI) | HR | (95% CI) | |
| Wealth | ||||||
| Lowest 10% | 1.7 | (1.2, 2.5) | 0.9 | (0.6, 1.4) | 0.9 | (0.6, 1.5) |
| 10–<25%ile | 1.5 | (1.1, 2.2) | 0.9 | (0.6, 1.3) | 1.2 | (0.8, 1.7) |
| 25–<50%ile | 1.7 | (1.2, 2.3) | 1.0 | (0.7, 1.3) | 1.1 | (0.8, 1.6) |
| 50–<75%ile | 0.9 | (0.7, 1.3) | 1.0 | (0.7, 1.3) | 1.1 | (0.8, 1.5) |
| 75–<90%ile | reference | |||||
| Top 10% | 1.0 | (0.6, 1.7) | 0.9 | (0.6, 1.3) | 1.0 | (0.6, 1.7) |
| Income | ||||||
| Lowest 10% | 1.6 | (1.2, 2.3) | 1.5 | (0.9, 2.5) | 1.1 | (0.6, 1.9) |
| 10–<25%ile | 1.2 | (0.9, 1.7) | 1.2 | (0.8, 1.9) | 1.5 | (0.9, 2.5) |
| 25–<50%ile | 1.2 | (0.9, 1.6) | 1.3 | (0.9, 1.9) | 1.2 | (0.7, 2.0) |
| 50–<75%ile | 1.1 | (0.9, 1.5) | 0.9 | (0.6, 1.4) | 1.2 | (0.7, 2.0) |
| 75–<90%ile | reference | |||||
| Top 10% | 1.0 | (0.6, 1.5) | 1.3 | (0.8, 2.1) | 1.0 | (0.5, 2.1) |
| Education credential | ||||||
| No degree | 1.1 | (0.9, 1.3) | 1.0 | (0.8, 1.3) | 1.1 | (0.9, 1.4) |
| High school/GED | reference | |||||
| Associates degree | 1.3 | (0.8, 2.0) | 1.0 | (0.5, 2.0) | 1.1 | (0.6, 2.3) |
| Bachelor’s degree | 1.1 | (0.8, 1.6) | 0.7 | (0.5, 1.1) | 1.1 | (0.7, 1.7) |
| Masters/professional | 1.0 | (0.7, 1.6) | 1.0 | (0.7, 1.6) | 1.4 | (0.9, 2.2) |
| Years of education | 1.00 | (0.97, 1.03) | 0.99 | (0.96, 1.03) | 1.01 | (0.98, 1.04) |
Models are adjusted for: education, income categories, wealth categories, age, age-squared, male, black, Hispanic, birth regions (northeast, west, Midwest, south, not US, unknown), father’s occupation (professional/managerial, white collar, skilled manual, unskilled manual, military, farming, missing), mother’s education (<8 years, 8+ years, unknown), father’s education (<8 years, 8+ years, unknown), and self-reported childhood health, self-reported diagnosis of hypertension, current smoking, diabetes, heart disease at baseline, level of vigorous activity at baseline, and body mass index at baseline.
HR indicates hazard ratio; 95% CI indicates 95% confidence interval.
Range for annual income percentiles are: <10th percentile (<$5657); 10 to 24th percentile ($5 657 to $10 521); 25 to 49th percentile ($10 522 to $19 699); 50 to 74th percentile ($19 700 to $35 504); 75 to 89th percentiles ($35 505 to $56 992) and ≥90th percentile (≥$56 993).
Range for wealth percentiles are: <10th percentile (<$1000); 10 to 24th percentile ($1000 to $20 999); 25 to 49th percentile ($21 000 to $67 260); 50 to 74th percentile ($67 261 to $161 299); 75 to 89th percentiles ($162 300 to $344 499) and ≥90th percentile (≥$344 499).
Sensitivity Analysis
We conducted sensitivity analysis using the ln of wealth and income as continuous variables and observed similar results. Among 50- to 64-year-olds, the estimated coefficients were 0.96 (0.94 to 0.99) for log wealth, 0.97 (0.92 to 1.02) for log income, and 0.98 (0.95, 1.01) for education, in models adjusted for all 3 socioeconomic status measures and cardiovascular risk factors. At age 75+, these coefficients were all 1.00. Similar results were found for men and women in sex-stratified models (results not shown). Furthermore, results for educational level and wealth did not differ by race. Although the effect of income was slightly stronger among blacks than whites, this interaction was small and not significant.
Discussion
Among men and women aged 50 or older, lower wealth, income, and education were associated with higher stroke incidence rates. This association was mainly attributable to large effects in those aged 50 to 64, among whom wealth and income were strong stroke predictors independently of other socioeconomic dimensions. The effect of all socioeconomic status indicators decreased sharply beyond age 65, resulting in no consistent effect of wealth, income, or education among the elderly. Adjustment for risk factors attenuated income and wealth disparities in stroke at ages 50 to 64×30% to 50%. Results suggest that wealth and income are independent predictors of stroke at ages 50 to 64, whereas they do not consistently predict stroke beyond age 65.
Study Limitations
Despite the unique strengths in the HRS data, some limitations should be considered. Medical record verification of strokes was not possible, and self-reported stroke data may be inaccurate. However, incidence rates in our sample were similar to those reported in other US studies. For comparison, the Greater Cincinnati/Northern Kentucky stroke study reported first stroke rates in the 50 to 64 year age stratum of 273/100 000 for whites and 637/100 000 for blacks.14 This is consistent with previous evidence that self-reports are sufficiently accurate for ascertaining stroke events in population surveys.13 Incomplete stroke ascertainment might have occurred differentially by socioeconomic status, which may have biased our results. However, missing stroke status was unrelated to socioeconomic status.
Misreporting of socioeconomic status is possible, but HRS has some of the best available wealth data on US adults, and extensive efforts at verification have been conducted. By using percentiles, the impact of moderate inaccuracies in income and wealth reports was substantially reduced. Furthermore, analyses using substantial amounts of imputed data tend to provide conservative estimates.11,15 Differential misreporting of some risk factors may also have occurred, as individuals in the low socioeconomic status groups may be less aware of risk factors such as hypertension and diabetes. Therefore, we may have underestimated their prevalence and thus underestimated their impact on the association between socioeconomic status and stroke in fully adjusted models.16 Furthermore, we did not have information on other risk factors for stroke that may explain associations, including genetic factors and family history of stroke, and number of years of smoking.
We did not have data on stroke subtypes. Although previous research indicates that lower socioeconomic status is associated with similar increases in risk of ischemic and hemorrhagic stroke,3,17 future studies should assess whether wealth effects differ across stroke subtypes.
We presented results simultaneously adjusting for income, wealth, and education. Because these factors influence each other, we may have underestimated their direct effect.18 For instance, education influences income and wealth, which may have resulted in underestimation of the effect of education in fully adjusted models. Nevertheless, this underestimation cannot explain the overall age-pattern we observed.
Comparisons With Previous Studies
Socioeconomic disparities in stroke have been reported in Europe and the US.1–3,17,19 We found large socioeconomic disparities in stroke at ages 50 to 64, but these were substantially attenuated or null after age 65. A previous study in 10 European populations reported that educational disparities in stroke mortality diminish but persist into old age.2 In contrast, results from a study in New Haven (US) found large disparities in stroke incidence at ages 65 to 74, but a crossover at age 75.1 Although we observed a similar effect of income on stroke incidence at ages 65 to 74, this effect was largely attenuated after adjustment for education and wealth. Furthermore, although a crossover was not observed in HRS, our results support the view that lower socioeconomic status does not predict excess risk in individuals older than 75.
To our knowledge, this is the first study reporting that lower wealth predicts increased stroke incidence independently of income and education before age 65. Previous reports indicate that wealth is associated with health throughout adulthood and becomes more important than education or income at older ages.6,7 Our results suggest this pattern does not apply to stroke, as the age attenuation holds across all socioeconomic indicators, including wealth.
Previous studies suggest that risk factors such as smoking and hypertension explain about half of stroke disparities.19 Consistently, we found that adjustment for smoking, hypertension, diabetes, heart disease, physical activity, and BMI attenuated income and wealth effects by 30% to 50%, but associations remained significant among those aged 50 to 64.
Interpretation of Findings
Our results offer a mixed picture on the role of wealth as a predictor of stroke. On the one hand, over and above income and education, wealth predicted stroke among 50- to 64-year-olds. Characterizing socioeconomic risk exclusively in terms of education and income may thus underestimate the excess stroke burden potentially attributable to socioeconomic status. It is yet unclear why wealth was more strongly associated with stroke than other socioeconomic dimensions at these ages. A possible explanation is that in the US, wealth is more unequally distributed than income,9 and racial inequalities in wealth are especially stark.20 This may result in larger contrast between the top and bottom wealth groups than between the top and bottom income groups.9 Furthermore, wealth is a special form of capital that represents a broad array of material resources.6,20 It is a much more permanent stock that reflects intergenerational transfers of material resources, lifelong accumulation of income, and the impact of costly health and economic shocks.6,20 Financial wealth can also provide liquidity in periods of economic stress or lack of income, such as unemployment episodes.9 Wealth more comprehensively reflects the traditional notion of economic resources available to foster health6,20 and may thus have a stronger influence on stroke than income and education at ages 50 to 64.
The mechanisms through which wealth influences stroke risk may involve different pathways. Possessing assets may enhance access to care before and after stroke occurs, buffering the negative impact of risk factors on stroke incidence and increasing survival after stroke. Lower wealth is also associated with higher prevalence of smoking,21 obesity,22 diabetes23 and alcohol consumption,24 which may increase stroke risk. However, the attenuation of wealth effects on stroke after adjustment for these factors at ages 50 to 64 was small. Alternative hypotheses suggest that wealth may increase individuals’ sense of control over their lives, reducing psychosocial stress25 and subsequently stroke risk.26 Other psychosocial risk factors such as depression and low social support are also more common in the low socioeconomic status groups and may influence stroke risk.1 This may occur via cardiovascular risk factors or through direct pathways involving central nervous system activation of autonomic and neuroendocrine responses.25
On the other hand, one of our most striking findings was the age-attenuation of wealth effects on stroke, because we expected that wealth would be a strong predictor in the elderly.6 The interpretation of these findings is crucial because the majority of strokes occur after age 65.4 Our study was based on a relative risk measure (hazard ratio), which typically decreases with age. However, this is not an adequate explanation for our findings, because absolute rate differences between wealth categories also declined with age. This age-attenuation may reflect the impact of entitlement programs such as Medicare, which potentially buffer negative effects of low wealth and income on stroke in the oldest old by enhancing opportunities to access care. However, this hypothesis is not supported by findings from European populations, where the age-attenuation in socioeconomic disparities in stroke is less marked2 despite universal access to care and generous egalitarian welfare policies. Furthermore, stroke risk is largely determined by exposures across the life course, including those before age 65. Thus, these mechanisms are unlikely to account for our results.
The attenuation of socioeconomic status effects on stroke may be explained by selective survival. This hypothesis postulates that low socioeconomic status individuals die earlier than high socioeconomic status individuals from multiple causes.6,7,27 As a consequence, low socioeconomic status survivors at older ages are a selection of the fit test and therefore no longer comparable to high socioeconomic status survivors.7 Thus, selective survival could artificially attenuate the association between socioeconomic status and stroke. Previous studies indicate that this is a plausible explanation for the observed attenuation of the effect of socioeconomic status and other demographic factors such as race on mortality.5,6,28 As an age-attenuation was also observed for wealth, our results suggest that this socioeconomic status indicator may also be susceptible to the effect of selective survival.
Cohort and period effects might also explain our results, as the age-attenuation of socioeconomic status disparities in stroke may reflect a different impact of socioeconomic status in different cohorts or periods. For instance, in earlier birth cohorts there may be less variability in socioeconomic status or in risk factors related to socioeconomic status, resulting in weaker associations with stroke compared with more recent cohorts. Age, period, and cohort effects are not distinguished in our study and may make those in the low socioeconomic status groups appear relatively protected from an increased stroke risk. Future studies with longer follow-up should explore how these mechanisms might explain the age-attenuation in socioeconomic status disparities in stroke.
Implications
Our results identify low wealth and income as important risk factors for stroke before age 65. Characterizations of socioeconomic disparities based exclusively on income or education measures probably understate the magnitude of social disparities in stroke risk. Although wealth is a major determinant of stroke, many US residents reach these ages with few assets. Policies that improve economically disadvantaged groups’ access to basic resources before reaching old age might reduce stroke rates as these cohorts age. Alternatively, enhancing opportunities for low socioeconomic status individuals to accumulate assets before retirement age might help reduce stroke rates and ameliorate socioeconomic status disparities in stroke. The role of income and wealth may appear limited from a public health perspective because these factors are not related to stroke beyond age 65. However, the age-attenuation of socioeconomic disparities in stroke likely reflects selective survival, a consequence of the cumulative disadvantage faced by individuals throughout the life-course. Disentangling substantive from artifactual explanations will be crucial for interpreting and predicting population trends in stroke and prioritizing prevention strategies.
Acknowledgments
The authors gratefully acknowledge helpful comments from Dr Lisa F. Berkman and Dr Johan Mackenbach.
Sources of Funding
This work was supported by the US National Institute of Aging (AG023399). Maria Glymour is a Robert Wood Johnson Health & Society Scholar at Columbia University. Mauricio Avendano was supported by a grant from the Netherlands Organisation for Scientific Research (NWO, grant No. 451-07-001).
Footnotes
Disclosures
None.
References
- 1.Avendano M, Kawachi I, van LFJ, Boshuizen H, Mackenbach JP, van den Bos GAM, Fay ME, Berkman LF. Socioeconomic status and stroke incidence in the us elderly: The role of risk factors in the epese study. Stroke. 2006;37:1368–1373. doi: 10.1161/01.STR.0000221702.75002.66. [DOI] [PubMed] [Google Scholar]
- 2.Avendano M, Kunst AE, Huisman M, van Lenthe F, Bopp M, Borrell C, Valkonen T, Regidor E, Costa G, Donkin A, Borgan JK, Deboosere P, Gadeyne S, Spadea T, Andersen O, Mackenbach JP. Educational level and stroke mortality: A comparison of 10 european populations during the 1990s. Stroke. 2004;35:432–437. doi: 10.1161/01.STR.0000109225.11509.EE. [DOI] [PubMed] [Google Scholar]
- 3.Jakovljevic D, Sarti C, Sivenius J, Torppa J, Mahonen M, Immonen-Raiha P, Kaarsalo E, Alhainen K, Kuulasmaa K, Tuomilehto J, Puska P, Salomaa V. Socioeconomic status and ischemic stroke: The finmonica stroke register. Stroke. 2001;32:1492–1498. doi: 10.1161/01.str.32.7.1492. [DOI] [PubMed] [Google Scholar]
- 4.Center for Disease Control. Disparities in deaths from stroke among persons aged <5 years–united states, 2002. JAMA. 2005;294:299–300. doi: 10.1001/jama.294.3.299. [DOI] [PubMed] [Google Scholar]
- 5.House JS, Lepkowski JM, Kinney AM, Mero RP, Kessler RC, Herzog AR. The social stratification of aging and health. J Health Soc Behav. 1994;35:213–234. [PubMed] [Google Scholar]
- 6.Robert S, House JS. Ses differentials in health by age and alternative indicators of ses. J Aging Health. 1996;8:359–388. doi: 10.1177/089826439600800304. [DOI] [PubMed] [Google Scholar]
- 7.Beckett M. Converging health inequalities in later life–an artifact of mortality selection. J Health Soc Behav. 2000;41:106–119. [PubMed] [Google Scholar]
- 8.Oliver ML, Shapiro TM. Black Wealth, White Wealth: A New Perspective on Racial Inequality. New York: Routledge; 1995. [Google Scholar]
- 9.Wolf E. International comparisons of wealth inequalities. Review of Income and Wealth. 1996:42. [Google Scholar]
- 10.Juster F, Suzman R. An overview of the health and retirement study. J Hum Resur. 1995;30(suppl):S7–S56. [Google Scholar]
- 11.St Clair P, Bugliari D, Chien S, Haider S, Hayden O, Hurd MD, Ilchuk S, Lopez G, Loughran D, Panis C, Pantoja P, Rastegar A, Reti M, Rowhwedder S, Roth E, Zissimopoulos J. Rand hrs data documentation version e. 2005 [Google Scholar]
- 12.Buhmann B, Rainwater LGS, Smeeding T. Equivalence scales, well-being, inequality and poverty: Sensitivity estimates across ten countries using the luxembourg income study (lis) data base. Income & Wealth. 1998;2:115–142. [Google Scholar]
- 13.Engstad T, Bonaa KH, Viitanen M. Validity of self-reported stroke: The tromso study. Stroke. 2000;31:1602–1607. doi: 10.1161/01.str.31.7.1602. [DOI] [PubMed] [Google Scholar]
- 14.Broderick J, Brott T, Kothari R, Miller R, Khoury J, Pancioli A, Gebel J, Mills D, Minneci L, Shukla R. The greater cincinnati/northern kentucky stroke study: Preliminary first-ever and total incidence rates of stroke among blacks. Stroke. 1998;29:415–421. doi: 10.1161/01.str.29.2.415. [DOI] [PubMed] [Google Scholar]
- 15.Schafer J. Analysis of Incomplete Multivariate Data. New York: Chapman Hall; 1997. [Google Scholar]
- 16.Mackenbach JP, Looman CW, van der Meer JB. Differences in the misreporting of chronic conditions, by level of education: The effect on inequalities in prevalence rates. Am J Public Health. 1996;86:706–711. doi: 10.2105/ajph.86.5.706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Jakovljevic D, Sarti C, Sivenius J, Torppa J, Mahonen M, Immonen-Raiha P, Kaarsalo E, Alhainen K, Tuomilehto J, Puska, et al. Socioeconomic differences in the incidence, mortality and prognosis of intracerebral hemorrhage in finnish adult population. The finmonica stroke register. Neuroepidemiology. 2001;20:85–90. doi: 10.1159/000054765. [DOI] [PubMed] [Google Scholar]
- 18.Cole SR, Hernan MA. Fallibility in estimating direct effects. Int J Epidemiol. 2002;31:163–165. doi: 10.1093/ije/31.1.163. [DOI] [PubMed] [Google Scholar]
- 19.Hart CL, Hole DJ, Smith GD. The contribution of risk factors to stroke differentials, by socioeconomic position in adulthood: The renfrew/paisley study. Am J Public Health. 2000;90:1788–1791. doi: 10.2105/ajph.90.11.1788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Conley D. Being Black, Living in the Red: Race, Wealth, and Social Policy in America. Berkeley: University of California Press; 1999. [Google Scholar]
- 21.Cavelaars AE, Kunst AE, Geurts JJ, Crialesi R, Grotvedt L, Helmert U, Lahelma E, Lundberg O, Matheson J, Mielck A, Rasmussen NK, Regidor E, do Rosario-Giraldes M, Spuhler T, Mackenbach JP. Educational differences in smoking: International comparison. Bmj. 2000;320:1102–1107. doi: 10.1136/bmj.320.7242.1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhang Q, Wang Y. Trends in the association between obesity and socioeconomic status in u.S. Adults: 1971 to 2000. Obes Res. 2004;12:1622–1632. doi: 10.1038/oby.2004.202. [DOI] [PubMed] [Google Scholar]
- 23.Rathmann W, Haastert B, Giani G, Koenig W, Imhof A, Herder C, Holle R, Mielck A. Is inflammation a causal chain between low socioeconomic status and type 2 diabetes? Results from the kora survey 2000. Eur J Epidemiol. 2006;21:55–60. doi: 10.1007/s10654-005-5085-6. [DOI] [PubMed] [Google Scholar]
- 24.Cavelaars A, Kunst A, Mackenbach JP. Socio-economic differences in risk factors for morbidity and mortality in the european community: An international comparison. J Health Psychol. 1997;2:353–372. doi: 10.1177/135910539700200306. [DOI] [PubMed] [Google Scholar]
- 25.Steptoe A, Marmot M. The role of psychobiological pathways in socioeconomic inequalities in cardiovascular disease risk. Eur Heart J. 2002;23:13–25. doi: 10.1053/euhj.2001.2611. [DOI] [PubMed] [Google Scholar]
- 26.Everson SA, Lynch JW, Kaplan GA, Lakka TA, Sivenius J, Salonen JT. Stress-induced blood pressure reactivity and incident stroke in middle-aged men. Stroke. 2001;32:1263–1270. doi: 10.1161/01.str.32.6.1263. [DOI] [PubMed] [Google Scholar]
- 27.Kaplan GA, Haan MN, Wallace RB. Understanding changing risk factor associations with increasing age in adults. Annu Rev Public Health. 1999;20:89–108. doi: 10.1146/annurev.publhealth.20.1.89. [DOI] [PubMed] [Google Scholar]
- 28.Markides KS, Machalek R. Selective survival, aging and society. Arch Gerontol Geriatr. 1984;3:207–222. doi: 10.1016/0167-4943(84)90022-0. [DOI] [PubMed] [Google Scholar]