Abstract
A 62-year-old lady presented with bilateral nodular lung opacities suspicious of metastatic disease on chest radiography and high-resolution CT. Histopathology, however, revealed caseating granulomas. The correct diagnosis of tuberculosis (TB) was confirmed when she responded clinically and radiologically to antitubercular treatment. TB should be considered in the differential diagnosis of bilateral nodular opacities which is the usual presentation of secondary malignancies of lung.
Background
Pulmonary tuberculosis (TB) is a common worldwide lung infection. The radiological features show considerable variation, but in most cases they are characteristic enough to suggest the diagnosis. Patchy, poorly defined consolidation in the apical and posterior segments of the upper lobes and in the superior segments of the lower lobes is the usual roentgenographic manifestation. Presentation as multiple bilateral nodules is an unusual roentgenographic finding.1
Case presentation
A 62-year-old female, non-smoker, was admitted to our hospital with complaints of low grade fever, fatigue, decreased appetite and exertional dyspnoea of 2 months duration. Physical examination revealed a temperature of 98.5°F, pulse rate of 94 beats/min, blood pressure of 126/84 mm Hg, respiratory rate of 16/min with an oxygen saturation of 96% on room air. She did not have any abnormality on general physical examination. Respiratory system examination revealed diminished breath sounds with prolonged expiration without any adventitious sounds. Cardiovascular, neurological and abdominal examination was within normal limit.
Investigations
Chest x-ray showed bilateral ill-defined nodular opacities (figure 1) and spiral CT of the thorax revealed multiple bilateral nodular shadows (figure 2). Her haematological and biochemical parameters were within normal limits. After studying the chest x-ray and CT thorax, possibility of secondaries in lungs were considered. As thyroid, breast, genitourinary- and gastrointestinal tract malignancies can very commonly present initially as lung metastasis, ultrasound neck for thyroid, mammography for breast nodule, gynaecological evaluation and CT of the abdomen and pelvis were done. But all investigations came out to be normal. Tuberculin test was negative. Bronchoscopy was done and bronchoalveolar lavage was negative for acid fast bacilli, fungi as well as malignant cells. Finally, a CT scan–guided transthoracic needle biopsy of the right lower lobe nodule was performed and the histopathology showed caseating granulomas suggestive of tuberculosis (figure 3). However, the specimen staining with Ziehl–Neelsen technique was negative for acid fast bacilli. Staining for fungi also proved negative. Therefore, the patient was diagnosed with ‘bilateral multiple tuberculoma’.
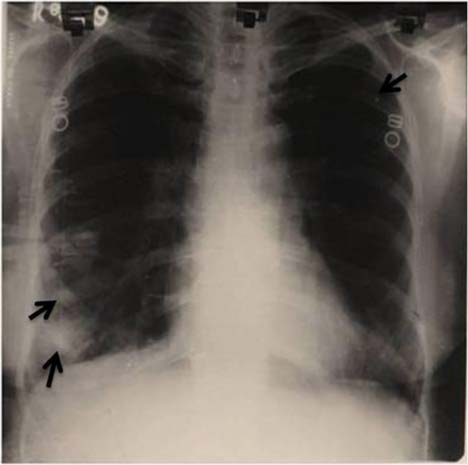
Figure 1.
Chest x-ray showing bilateral ill-defined nodular opacities (arrows).
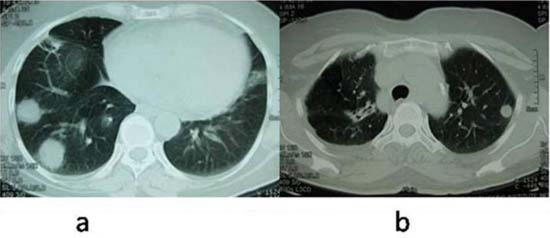
Figure 2.
CT of thorax shows multiple and bilateral nodular opacities without cavitation in the right lower lobe (A) and left upper lobe (B).
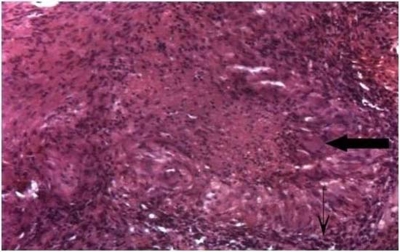
Figure 3.
Epithelioid granuloma with Langerhans’ giant cell (thick arrow) and wall of epithelioid cells (small arrow) around a central area of necrosis on the needle biopsy of the right lower lobe nodule (H&E × 525 × digital magnification).
Differential diagnosis
The differential diagnosis for multiple pulmonary nodules is given below2
-
▶
Inflammatory
-
▶
Granulomas
-
▶
Fungal and opportunistic infections
-
▶
Septic emboli
-
▶
Rheumatoid nodules
-
▶
Wegener’s granulomatosis
-
▶
Sarcoidosis
-
▶
Langerhans cell histiocytosis
-
▶
-
▶
Neoplastic
-
▶
Metastases
-
▶
Malignant lymphoma/lymphoproliferative disorders
-
▶
-
▶
Congenital
-
▶
Arteriovenous malformations (Osler–Weber–Rendu syndrome)
-
▶
-
▶
Miscellaneous
-
▶
Haematomas
-
▶
Pulmonary infarcts
-
▶
Occupational (silicosis).
-
▶
Treatment
She was prescribed category 1 regimen of Revised National Tuberculosis Control Programme of India which consists of isoniazid (600 mg), rifampicin (450 mg), ethambutol (1200 mg) and pyrazinamide (1500 mg) three times weekly for 2 months followed by isoniazid (600 mg) and rifampicin (450 mg) three times weekly for 4 months.
Outcome and follow-up
After completion of treatment, there was both clinical and radiological improvement (figure 4), and she was asymptomatic in the short follow-up period of 1 year.
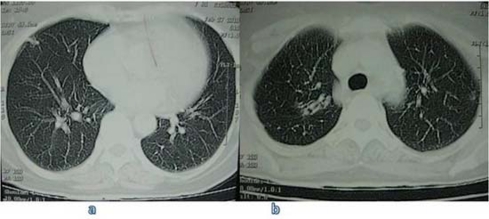
Figure 4.
CT of thorax at the completion of antitubercular treatment revealed complete resolution of nodular opacities in the right lower lobe (A) and left upper lobe (B).
Discussion
Tuberculomas are avascular, spherical and granulomatous masses of small tubercles with varying incidence in different parts of the world.3 These represent the manifestations of primary as well as post primary disease. Calcification is not uncommon and cavitation may also be present.4 The margins are usually smooth and sharp, and the usual location is in the upper lobes. A negative tuberculin test in this case could be due to the advanced age of the patient, as it has been observed that many older patient fail to respond to tuberculin test due to age-related immune defects. The diagnosis of tuberculomas remain a challenge, not only because these require invasive procedures, such as percutaneous needle aspiration or transbronchial lung biopsy, but also because there may also be accompanying malignancy as well, although rare.5–8 The importance of early detection lies in the fact that the findings on chest radiography and CT scans may be indistinguishable from those of malignancy.9 The pattern of multiple bilateral, non-cavitary discrete pulmonary nodules as seen in our case, is not generally recognised as a radiographic presentation of pulmonary tuberculosis, but such findings have been previously reported by us as well as others.9–11 In conclusion, tuberculomas should be considered in the differential diagnosis of the patients presenting with clinical and radiological features of metastatic lung disease.
Learning points.
-
▶
All multiple pulmonary opacities are not malignant.
-
▶
In tuberculosis-endemic countries like India, pulmonary tuberculosis should be one of the differential diagnoses of nodular pulmonary opacities.
-
▶
The treatment of nodular pulmonary opacities should be based on histological diagnosis.
Footnotes
Competing interests None.
Patient consent Obtained.
References
- 1.Erasmus JJ, Connolly JE, McAdams HP, et al. Solitary pulmonary nodules: part I. Morphologic evaluation for differentiation of benign and malignant lesions. Radiographics 2000;20:43–58 [DOI] [PubMed] [Google Scholar]
- 2.Armstrong P. Basic patterns in lung disease. In: Armstrong P, Wilson AG, Dee P, Hansell DM, eds. Imaging of Diseases of the Chest. Second edition St. Louis, MO: Mosby-Year Book; 1995:96–107 [Google Scholar]
- 3.Winer-Muram HT, Rubin SA. Thoracic complications of tuberculosis. J Thorac Imaging 1990;5:46–63 [DOI] [PubMed] [Google Scholar]
- 4.Arora VK, Arora R. Radiology of tuberculosis-clinicians perspective. In: Arora VK, Arora R, eds. Practical Approach to Tuberculosis Management. First edition New Delhi: Jaypee Brothers; 2006:239–76 [Google Scholar]
- 5.Fraser RG, Pare JA, Fraser RS. Multiple pulmonary nodules with or without cavitation. In: Fraser RG, Peter Paré JA, Pare PD, et al., eds. Diagnosis of Diseases of the Chest. Third edition Philadelphia, PA: W.B. Saunders and Co; 1991:3074–9 [Google Scholar]
- 6.Choi YH, Im JG, Han BK, et al. Thoracic manifestation of Churg-Strauss syndrome: radiologic and clinical findings. Chest 2000;117:117–24 [DOI] [PubMed] [Google Scholar]
- 7.Steele JD. The solitary pulmonary nodule. report of a cooperative study of resected asymptomatic solitary pulmonary nodules in males. J Thorac Cardiovasc Surg 1963;46:21–39 [PubMed] [Google Scholar]
- 8.Kant S, Garg R, Tripathi AK. Approach to a solitary pulmonary nodule. JIMI 2000;3:131–6 [Google Scholar]
- 9.Zaizen Y, Chujo M, Yamaguchi C, et al. Diagnosis by needle biopsy of tuberculoma that mimics lung cancer. Gen Thorac Cardiovasc Surg 2008;56:616–20 [DOI] [PubMed] [Google Scholar]
- 10.Ariyürek MO, Karçaaltincaba M, Demirkazik FB, et al. Bilateral multiple pulmonary tuberculous nodules mimicking metastatic disease. Eur J Radiol 2002;44:33–6 [DOI] [PubMed] [Google Scholar]
- 11.Kant S, Kushwaha R, Verma SK, et al. Bilateral nodular pulmonary tuberculosis simulating metastatic lung cancer. The Internet Journal of Pulmonary Medicine 2007;8 NLM Unique ID: 101090208. ISSN: 1531-2984 http://www.ispub.com/journal/the_internet_journal_of_pulmonary_medicine.html [Google Scholar]