Summary
We reported previously that mice overexpressing Cyp7a1 (Cyp7a1-tg) are protected against high fat diet-induced hypercholesterolemia, obesity and insulin resistance (1). Here we investigated the underlying mechanism of bile acid signaling in maintaining cholesterol homeostasis in Cyp7a1-tg mice. Cyp7a1-tg mice had 2-fold higher Cyp7a1 activity and bile acid pool than wild type mice. Gallbladder bile acid composition changed from predominantly cholic acid (57%) in wild type to chenodeoxycholic acid (54%) in Cyp7a1-tg mice. Cyp7a1-tg mice had higher biliary and fecal cholesterol and bile acid secretion rates than wild type mice. Surprisingly, hepatic de novo cholesterol synthesis was markedly induced in Cyp7a1-tg mice but intestine fractional cholesterol absorption in Cyp7a1-tg mice remained the same as wild type mice despite increased intestine bile acids. Interestingly, hepatic but not intestinal expression of several cholesterol (ABCG5/G8, SR-B1) and bile acid (ABCB11) transporters were significantly induced in Cyp7a1-tg mice. Treatment of mouse or human hepatocytes with a farnesoid X receptor (FXR) agonist GW4064 or bile acids induced hepatic Abcg5/g8 expression. A functional FXR binding site was identified in the Abcg5 gene promoter. Study of tissue-specific Fxr knockout mice demonstrated that loss of the Fxr gene in the liver attenuated bile acid induction of hepatic Abcg5/g8 and gallbladder cholesterol content, suggesting a role of FXR in the regulation of cholesterol transport. In summary, this study revealed a new mechanism by which increased Cyp7a1 activity expands the hydrophobic bile acid pool, stimulating hepatic cholesterol synthesis and biliary cholesterol secretion without increasing intestinal cholesterol absorption. This study demonstrated that Cyp7a1 plays a critical role in maintaining cholesterol homeostasis and underscores the importance of bile acid signaling in regulating overall cholesterol homeostasis.
Keywords: Cholesterol 7α-hydroxylase, bile acid synthesis, nuclear receptors, cholesterol transport, ABCG5/G8, SR-BI
Introduction
The liver is a major organ involved in de novo cholesterol synthesis and catabolism, biliary cholesterol secretion, and reverse cholesterol transport. Cholesterol homeostasis in the liver is maintained by balancing de novo cholesterol synthesis, uptake and elimination. Biliary secretion of cholesterol, either in the form of free cholesterol or bile acids, is the only significant route for eliminating cholesterol in mammals (2). Cholesterol 7α-hydroxylase (CYP7A1) is the rate-limiting enzyme in the bile acid biosynthetic pathway in the liver and thus controls cholesterol and bile acid homeostasis. Deficiency of CYP7A1 in humans is associated with hypercholesterolemia and premature atherosclerosis (3). Bile acids are not only physiological detergents that facilitate intestinal fat, sterols and fat-soluble vitamin absorption and distribution but also act as signaling molecules that activate the farnesoid X receptor (FXR) and several cell signaling pathways to maintain lipid, glucose and energy metabolism (2, 4).
It has been reported that over-expression of CYP7A1 in mouse liver (Cyp7a1-tg mice) prevents lithogenic diet-induced atherosclerosis (5). We recently reported that Cyp7a1-tg mice are resistant to high fat-diet-induced obesity, insulin resistance and fatty liver, and maintained cholesterol, bile acid and triglyceride homeostasis (1). The cholesterol lowering effect of stimulation of bile acid synthesis has been attributed to increased conversion of cholesterol into bile acids and stimulation of LDL receptor-mediated cholesterol uptake into the liver. Hepatic cholesterol is secreted into bile by a heterodimeric cholesterol efflux transporter ABCG5/G8 in the canalicular membrane of hepatocytes (6, 7). In the intestine, ABCG5/G8 effluxes plant sterols and cholesterol to the lumen, preventing plant sterol absorption and limiting dietary cholesterol absorption. Mutations of the ABCG5 and /or ABCG8 genes cause sitosterolemia in humans (8). Mice lacking the Abcg5/g8 genes display markedly decreased biliary cholesterol secretion and increased intestinal fractional cholesterol absorption (9). The ABCG5 and ABCG8 genes are orientated in a head-to-head configuration with only a 140 nucleotides intergenic promoter separating the two genes (8). Current knowledge on transcriptional regulation of ABCG5 and ABCG8 gene is limited. Cholesterol or cholic acid feeding induces Abcg5/g8 expression in wild type, but not Fxr−/− mice suggesting Fxr-dependent transcriptional regulation of Abcg5/g8 expression (7). Liver orphan receptor (LXR) also is implicated in regulation of Abcg5/g8 (10). However, a functional FXR or LXR binding site has not been identified in mouse Abcg5 or Abcg8 genes. It has been reported that ABCG5/G8-independent pathways also contribute to hepatobiliary cholesterol secretion (11, 12).
We studied the mechanism of bile acid signaling in the regulation of cholesterol homeostasis in Cyp7a1-tg mice. We found that biliary and fecal cholesterol and bile acid secretion rates were increased, de novo cholesterol synthesis was also increased, but intestinal fractional cholesterol secretion rate was unchanged in Cyp7a1-tg mice. Bile acids stimulate biliary cholesterol secretion by FXR-mediated induction of ABCG5/G8 and SR-B1 expression. This study suggests that an increased hydrophobic bile acid pool plays a critical role in the regulation of biliary free cholesterol secretion and maintenance of cholesterol and bile acid homeostasis.
Materials and Methods
Animals
Cyp7a1 transgenic mice (Cyp7a1-tg) over-expressing a rat Cyp7a1 cDNA under the control of an ApoE3 hepatic control region were originally generated by the late Dr. Roger A. Davis (13) and were obtained from the Mammalian Mouse Regional Resource Center at University of California Davis (Strain name: B6.Cg-Tg (APOE-Cyp7a1)1Rjd/Mmcd). Mice were further bred with wild type C57BL/6J mice (Jackson Laboratory, Bar harbor, ME). Transgenic mice and wild type littermates, between 6 – 8 generations with > 90% C57BL6J background, were used in this study. All mice were fed a standard chow diet, housed under a 12 hr light/dark cycle (6 am to 6 pm light), and sacrificed at 9 am after fasting for 16 hrs. Liver-specific Fxr knockout mice (L-FXRKO) and intestine-specific Fxr knockout mice (I-FXRKO) were generated as previously described (14). Animal protocols were approved by the Institutional Animal Care and Use Committees at NEOUCOM and the University of Kansas Medical Center.
Quantization of cholesterol, phospholipids and bile acids
Lipids were extracted from liver, gallbladder and feces with chloroform/methanol (2:1), dried, and dissolved with 5% Triton X-100 in isopropanol. Cholesterol and phospholipids were quantified with a Cholesterol Assay Kit (Calbiochem, San Diego, CA) or a Phospholipid C Assay Kit (Wako Chemical USA Inc., Richmond, VA). Gallbladder bile was diluted in 70% ethanol; liver, intestine or fecal bile acids were extracted once each with 90% ethanol, 80% ethanol and chloroform/methanol (2:1), vacuum dried and re-dissolved in 70% ethanol. Bile acids in each tissue were determined with a Bile Acid Assay Kit (Genzyme Diagnostic, Framingham, MA).
Assay of biliary cholesterol, bile acids and phospholipids secretion rate
Mice were fasted for 6 hr and anesthetized. The common bile duct and the cystic duct were ligated and common bile duct was cannulated with a G30 needle attached to a PE-10 polyethylene tube (BD Biosciences Primary Care Diagnostics, Sparks, MD). Bile was collected for 60 min. Cholesterol, bile acid, and phospholipid contents in the collected bile were determined by respective assay kits.
Assay of hepatic cholesterol synthesis rate measurement
Mice were briefly fasted for 4 hr then i.p. injected with 10 μCi [1-14C]-sodium acetate (Perkin Elmer, Waltham, MA). Mice were sacrificed 30 min after injection and ~250 mg of liver was rinsed in ice cold PBS. Liver tissues were then saponified in 2.2 ml mixture of 50% KOH: 95% ETOH (1:10, v: v) at 70°C overnight. 3H-cholesterol (1 μCi) was added to the same tube as a recovery control. Sterols were extracted in 3 ml hexane, dried and redissolved in 300 μl mixture of acetone: ETOH (1:1, v: v). Sterols were then precipitated with 1 ml of digitonin (0.5% in 95% ETOH) overnight at room temperature. The radioactivity of 3H and 14C in the precipitates was determined in a scintillation counter. Cholesterol synthesis rate was expressed as the amount of [1-14C]-acetate incorporated into sterols per minute per gram liver tissue.
Assay of intestine cholesterol absorption
Intestine cholesterol absorption was determined by a dual-isotope plasma ratio method (15). Briefly, mice were injected with 2.5 μCi 3H-cholesterol in Intralipid (Sigma, St Louis, MO) via tail vein, immediately followed by oral gavage of 1 μCi 14C-cholesterol in median-chain triglycerides (MCT oil, Mead Johnson, Evansville, IN). Mice were returned to cage with free access to food and water. After 72 h, blood samples were collected and the radioactivity of 14C and 3H were determined by scintillation counting. Intestine cholesterol absorption was determined as the ratio of 14C/3H in 1 ml of plasma.
Analysis of bile acid composition
Gallbladder bile was mixed with D4-labeled bile acids and hydrolyzed in 1 M KOH at 120°C overnight. Samples were extracted with diethyl ether. The water phase was acidified with 6 M HCl and extracted with diethyl ether. The samples were washed with water until neutral, evaporated and methylated with trimethylsilyldiazomethane and derivatized using hexamethyl-disilazane and trimethylchlorosilane in pyridine. Samples were finally analyzed by Gas chromatography-mass spectrometry (16).
Other methods
The following standard methods are described in detail in the Supplemental Methods: cell culture, RNA isolation, quantitative Real-time PCR, Western immunoblot, electrophoretic mobility shift assay (EMSA), chromatin Immunoprecipitation (ChIP) assay, construction of Abcg5 reporters, mutagenesis and transient transfection assay.
Statistical analysis
Results are expressed as mean ± S.E. Statistical analysis was performed by Student’s t-test. A p < 0.05 is considered as statistically significant.
Results
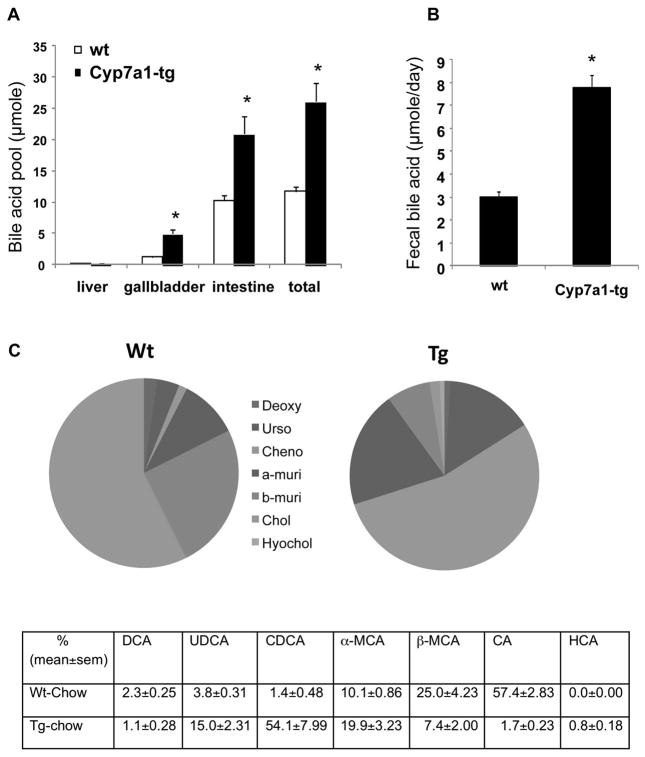
Cyp7a1-tg mice have enlarged bile acid pool and hydrophobic bile acid composition
In this study, we further investigated the effects and mechanisms of CYP7A1 over expression on hepatic cholesterol homeostasis in Cyp7a1-tg mice. Cyp7a1-tg mice had a ~2-fold increase of CYP7A1 enzyme activity (1). As a result, bile acid synthesis and bile acid pool increased 2.5-fold (Fig 1A), and fecal bile acid content increased 2.5-fold (Fig 1B). A detailed analysis of bile acid composition in gallbladder bile using a sensitive GC/MS method showed that gallbladder bile acid composition changed from predominantly tauro-conjugated cholic acid (CA, 58%) in wild type mice to chenodeoxycholic acid (CDCA, 54%) in Cyp7a1-tg mice (Fig 1C). In Cyp7a1-tg mice the CA content was drastically decreased to 1.7%, but α-muricholic acid (α-MCA) content increased two-fold to 20% andβ-MCA reduced to 7.4% in comparison with wild type mice. Ursodeoxycholic acid (UDCA) markedly increased from 3.8% in wild type to 15% in Cyp7a1-tg mice. This altered bile acid composition can be explained by bile acid inhibition of CYP8B1 and cholic acid synthesis in Cyp7a1-tg mice (1). This may lead to significantly higher CDCA production. In mouse livers, excess CDCA is converted to MCAs by Cyp3a11-mediated 6-hydroxylation and epimerization of a hydroxyl group from 7α- to 7β-position, or to UDCA by epimerization of a 7α-hydroxyl group to 7β-position. CDCA is more hydrophobic than CA and MCA and UDCA are highly hydrophilic. Thus, gallbladder bile in Cyp7a1-tg mice is more hydrophobic than that in wild type mice.
Fig 1.
Cyp7a1-tg mice had increased bile acid pool and altered bile acid composition. Total bile acid pool size was determined by adding bile acid contents in liver, gallbladder and intestine (A). Fecal bile acid contents are shown in (B). Results are expressed as mean ± S.E. n=4. An “*” indicates significant difference, P< 0.05, Cyp7a1-tg vs. wild type controls. (C). Gallbladder bile acid composition was determined in individual wild type or Cyp7a1-tg mouse. Individual bile acids were determined by GC/MS method and expressed as the percentage of total bile acid pool. All data are statistically significant different, Cyp7a1-tg vs. wild type, % mean ±standard error of the mean (sem), p<0.05, n=4. All bile acids determined are tauro-conjugated: DCA, deoxycholic acid; UDCA, ursodeoxycholic acid; CDCA, chenodeoxycholic acid; α-MCA, α-muricholic acid; β-MCA, β-muricholic acid; CA, cholic acid, HCA, hyocholic acid.
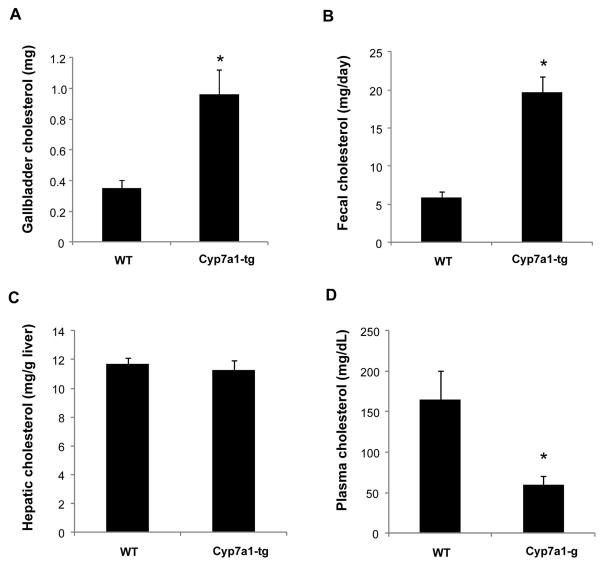
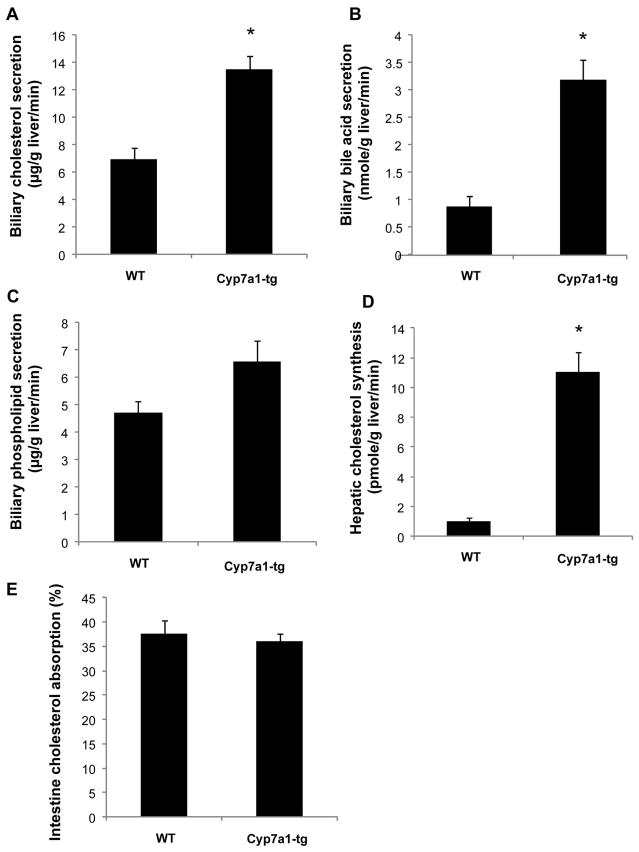
Cyp7a1-tg mice had higher biliary and fecal cholesterol and bile acid secretion, increased de novo cholesterol synthesis, but normal intestine fractional absorption of cholesterol
Interestingly, despite increased cholesterol catabolism in the liver, Cyp7a1-tg mice still had about 2.5-fold higher biliary and fecal cholesterol content than wild type mice (Fig 2A and B). Hepatic total cholesterol levels were unaltered (Fig 2C), but plasma cholesterol was decreased in Cyp7a1-tg mice (Fig 2D). Biliary cholesterol and bile acid secretion rates were 2-and 4- fold higher, respectively, in Cyp7a1-tg mice than wild type mice (Fig 3A and 3B). Biliary phospholipid secretion had a tendency to increase but did not reach statistical significance (Fig 3C). To determine the source of cholesterol, we assayed de novo cholesterol synthesis in Cyp7a1-tg mice. Increased bile acid pool should inhibit de novo cholesterol synthesis as observed in bile acid feeding experiments. However, hepatic de novo cholesterol synthesis rate was markedly increased by ~11-fold (Fig 3D), which is consistent with ~7-fold induction of HMG CoA Reductase expression in Cyp7a1-tg mouse livers (Table 1). Increased bile acid pool normally should stimulate intestine fractional absorption of cholesterol. Surprisingly we found that intestine fractional cholesterol absorption was similar between Cyp7a1-tg mice and wild type mice (Fig 3E). These results suggest that Cyp7a1-tg mice have increased hepatic de novo cholesterol synthesis. Excess cholesterol is metabolized to bile acids, which are efficiently secreted into bile. Thus, the increased fecal cholesterol excretion in Cyp7a1-tg mice more likely resulted from increased biliary secretion of cholesterol rather than decreased intestine cholesterol absorption. Furthermore, plasma total cholesterol was decreased by 60% in Cyp7a1-tg mice, suggesting that increased hepatic cholesterol uptake may also contribute to hepatic cholesterol input.
Fig 2.
Cyp7a1-tg mice had higher gallbladder and fecal cholesterol contents. Gallbladder, fecal, liver and plasma cholesterol content was determined with an assay kit as described under Materials and Methods. Results are expressed as mean ± S.E. n=4–6. An “*” indicates significant difference, P< 0.05, Cyp7a1-tg vs. wild type controls.
Fig 3.
Cyp7a1-tg mice had higher biliary cholesterol and bile acid secretion and increased hepatic cholesterol synthesis, but unaltered intestine cholesterol absorption. Bile was collected from 6 hr fasted mice for one hr via common bile duct cannulation. Biliary cholesterol secretion (A), biliary bile acid secretion (B), biliary phospholipid secretion (C), hepatic de novo cholesterol synthesis (D), and intestine cholesterol absorption (E) were determined as described under Materials and Methods. Results are expressed as mean ± S.E. n=3–4. An “*” indicates significant difference, P< 0.05, Cyp7a1-tg vs. wild type controls.
Table 1.
Hepatic and intestine mRNA expression of cholesterol and bile acid transporters in Cyp7a1-tg vs. wild type mice
| Wild type | Cyp7a1-Tg | |
|---|---|---|
| Hepatic mRNA expression | ||
| Abcg5 | 1±0.18 | 2.64±0.17* |
| Abcg8 | 1±0.21 | 1.67±0.21* |
| Sr-bI | 1±0.19 | 1.9±0.11* |
| Ldlr | 1±0.14 | 2.02±0.22* |
| HmgCoAR | 1±0.28 | 6.9±2.5* |
| Bsep | 1±0.08 | 1.75±0.11* |
| Mdr2 | 1±0.11 | 1.02±0.1 |
| Ntcp | 1±0.21 | 0.97±0.22 |
| Intestine mRNA expression | ||
| Abcg5 | 1±0.24 | 1.07±0.28 |
| Abcg8 | 1±0.12 | 0.9±0.26 |
| Npc1l1 | 1±0.19 | 0.7±0.12 |
| Sr-bI | 1±0.05 | 1±0.35 |
| Asbt | 1±0.7 | 0.64±0.48 |
| Shp | 1±0.28 | 8.96±2.6* |
| Fgf15 | 1±0.39 | 24.4±8.33* |
Male wild type and Cyp7a1-tg mice of 12 weeks old, 5 to 8 mice/group, were used in this experiment. Results shown are mean ± SEM.
significant difference, p<0.05, Cyp7a1-tg vs. WT mice.
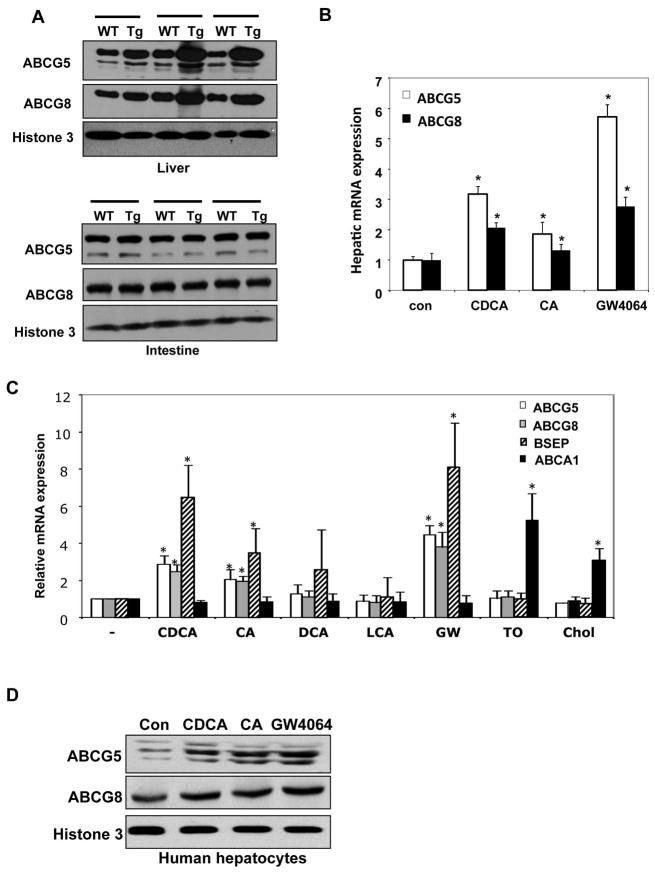
Cyp7a1-tg mice had higher expression of hepatic cholesterol and bile acid transporters
To investigate the mechanism of increased biliary bile acid and cholesterol secretion in Cyp7a1-tg mice, we first analyzed mRNA expression of bile acid and cholesterol transporters in the liver and intestine. Cyp7a1-tg mice had significantly higher Abcg5 (2.7-fold) and Abcg8 (1.7-fold) mRNA expression in the liver, but not in the intestine (Table 1). Hepatic Abcg5/g8 protein levels were higher in Cyp7a1-tg mice than their wild type littermates, while intestine Abcg5/g8 protein expression showed no difference (Fig 4A). Expression of Sr-b1 mRNA increased 1.9-fold in Cyp7a1-tg mouse livers, but not in the intestine (Table 1). Expression of bile salt export pump (Bsep or Abcb11), a major biliary bile acid efflux transporter was significantly increased (1.7-fold) in Cyp7a1-tg mice (Table 1). Expression of liver sinusoidal Na+-dependent taurocholate cotransport peptide (Ntcp), which reabsorbs bile salts from sinusoidal blood, did not change in Cyp7a1-tg mice. Expression of a hepatic phospholipid flipase (Abcb4) or multi-drug resistant protein 2 (Mdr2), which is required for efficient biliary cholesterol secretion, did not change (Table 1). This is consistent with observed no significant increase of biliary phospholipid secretion in Cyp7a1-tg mice (Fig 3C). In the intestine, mRNA expression levels of Niemann-Pick like 1 protein (Npc1l1), which is an intestine cholesterol absorption transporter, and apical sodium-dependent bile salt transporter (Asbt), which reabsorbs bile salts from the lumen, were not changed in Cyp7a1-tg mice (Table 1). Expression levels of the FXR-induced fibroblast growth factor 15 (Fgf15) and Shp were drastically induced in Cyp7a1-tg mice, as a result of increased intestinal bile acids (Table 1). These results indicate that bile acids may coordinately regulate biliary bile acids and cholesterol secretion. Induction of hepatic, but not intestinal cholesterol and bile acid transporters may result in increased biliary cholesterol and bile acid secretion with subsequent fecal elimination in Cyp7a1-tg mice.
Fig 4.
Cyp7a1-tg mice had higher expression of hepatic ABCG5 and ABCG8. (A) Wild type and Cyp7a1-tg mice on chow diet were fasted overnight and ABCG5 and ABCG8 protein levels in the liver and the intestine were determined by Western blot. The protein expression in individual Cyp7a1-tg mouse and its respective littermate control was compared. (B) Hepatocytes were isolated from wild type mouse livers and treated with 25 μM of CDCA or CA, or 2 μM GW4064 for 24 hr, and mRNA expression was determined by real-time PCR. Results are expressed as mean ± S.E. An “*” indicates significant difference, p< 0.05, Cyp7a1-tg vs. non-treated controls. (C) & (D). Primary human hepatocytes (n=3) were treated with 25 μM CDCA or CA, 10 μM DCA or LCA, 2 μM GW4064, 1 μM TO901317 or 20 μg/ml cholesterol for 24 hr. mRNA expression (C) or protein levels (D) was determined by real-time PCR or Western blot, respectively. Results are expressed as mean ± S.E. An “*” indicates significant difference, P< 0.05, Cyp7a1-tg vs. non-treated controls.
Bile acids induce Abcg5/g8 via a functional FXR response element in the Abcg5/g8 genes
To test if increased hepatic Abcg5/g8 expression in Cyp7a1-tg mice could be due to bile acid activation of FXR, we treated mouse hepatocytes with bile acids or a specific FXR agonist GW4064 and analyzed Abcg5/g8 mRNA expression levels. As shown in Fig 4B, CDCA, CA and GW4064 treatment all significantly induced Abcg5/g8 mRNA expression levels in mouse hepatocytes. CDCA induction of Abcg5/g8 was stronger than CA, which is consistent with CDCA being a more efficacious FXR ligand. Furthermore, treating primary human hepatocytes with CDCA, CA and GW4064 also induced ABCG5/G8 mRNA (Fig 4C) and protein expression (Fig 4D), suggesting that FXR induction of ABCG5/G8 is conserved in human hepatocytes. To our surprise, an LXR agonist TO901317 or cholesterol did not induce ABCG5/G8 mRNA in human hepatocytes (Fig 4C), in contrast to a previous report that LXR induce mouse Abcg5 and Abcg8 mRNA expression (10). These data suggest that LXR may differentially regulate ABCG5 and ABCG8 expression in mouse and human hepatocytes.
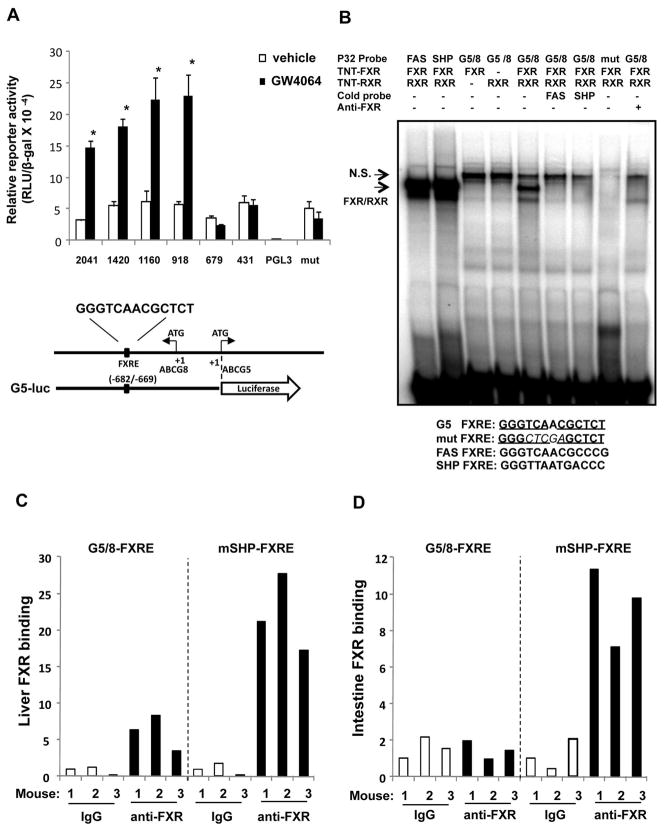
To further elucidate the molecular mechanism of FXR regulation of Abcg5/g8 gene expression, we performed Abcg5 promoter/luciferase reporter assays in HepG2 cells. We found that the Abcg5 reporter activities of the reporter plasmids -2041-luc, -1420-luc, -1160-luc and -918-luc were strongly induced by GW4064 treatment. Reporter activities of shorter constructs -679-luc and -431-luc were not affected. These assays defined a functional FXR responsive region located between nt -680 and -918 on the Abcg5 promoter (Fig 5A). Analysis of nucleotide sequences in this region identified an inverted repeat with one-base spacing (IR1) located between nt -682 to -669 on the Abcg5 promoter (or +309 and +322 of abcg8 in intron 1), which is a typical FXRE (Fig 5A). EMSA showed that FXR/RXRα heterodimer bound to this putative FXRE, and that binding was abolished by excess of unlabeled probes containing the known FXRE from small heterodimer partner (SHP), or fatty acid synthase (FAS) genes, or by antibody super shift assay using an antibody against FXR (Fig 5B). We then performed chromatin immunoprecipitation (ChIP) assays using mouse liver and intestine nuclei. ChIP assays showed that FXR occupied the Abcg5/g8 promoter in the mouse liver (Fig 5C), but not in mouse intestine (Fig 5D). Positive control showed that FXR occupied Shp gene promoter in both mouse liver and mouse intestine (Fig 5C&5D). These results demonstrated that FXR directly bound to the FXRE located in the promoter of Abcg5 (intron 1 of Abcg8 gene) in mouse livers and mediated bile acid induction of both abcg5 and abcg8 gene transcription.
Fig 5.
Mouse Abcg5 promoter and Abcg8 intron 1 has a FXR response element (FXRE) that is functional in the liver, but not intestine. (A) Upper panel: various mouse abcg5 promoter/reporter plasmids were co-transfected with FXR and RXRα expression plasmids into HepG2 cells. Cells were then treated with vehicle (DMSO) or GW4064 (2 μM) for 24 h and luciderase activity was determined and normalized to β-gal activity. Assays were performed in triplicates and expressed as mean ± S.D. An *” indicates significant difference, p< 0.05, Cyp7a1-tg vs. vehicle treated controls. Lower panel: An illustration of the mouse Abcg5 and Abcg8 gene structure, construction of Abcg5 promoter reporter plasmids and localization a putative FXRE sequence in Abcg5 promoter or Abcg8 intron 1. (B) EMSA assay of FXR/RXR binding to 32P labeled mouse FXRE probes from Abcg5/g8, Shp and Fas genes. Mut, mutant ABCG5 FXRE. N.S. none-specific bands. Probes used are: G5/8-FXRE: GGGACAGTCACATGGGTCAACGCTCTGT GATG, mutant G5/8-FXRE: GGGACAGTCACATGGCTCGAGGCTCTGTGATG, FAS-FXRE: GGCGGCGGGGGTCAACGCCCGCACTT, SHP-FXRE: GGCAGCCTGGGTTAATGACCCTG TTTA. (C) & (D). In vivo quantitative ChIP assay of FXR occupancy on Abcg5/g8 gene. Nuclei were isolated from individual mouse liver (left panel) and intestine (right panel) for ChIP assay with an FXR antibody as described in Supplemental Materials and Methods. FXR binding to SHP promoter was used as a positive control.
Loss of Fxr in the liver decreased biliary cholesterol and attenuated bile acid induction of Abcg5 and Abcg8 gene expression in mice
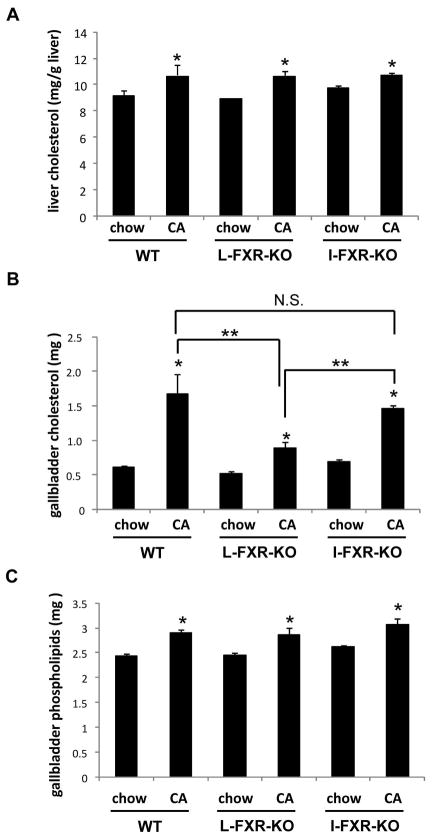
To further investigate the role of hepatic FXR in mediating bile acid regulation of biliary and fecal cholesterol content, we fed wild type, liver-specific Fxr knockout (L-FXR-KO) and intestine-specific Fxr knockout (I-FXR-KO) mice either a chow diet or a chow diet supplemented with 0.5% CA for 1 week. As shown in Fig 6A, deletion of the Fxr gene in the liver or the intestine did not significantly alter hepatic cholesterol content. CA feeding significantly increased biliary cholesterol content by 3-fold in wild type, 2-fold in I-FXR-KO mice, and about 0.3-fold in L-FXR-KO mice (Fig 6B) suggesting that FXR-independent bile acid signaling may be also involved in biliary cholesterol secretion. CA feeding also resulted in a small but significant increase in biliary phospholipid levels in all three genotypes. This suggests that bile acid effect on biliary phospholipid content may be FXR-independent (Fig 6C).
Fig 6.
Hepatic and gallbladder lipid content in tissue-specific Fxr knockout mice. Wild type, Liver-specific Fxr knockout mice (L-FXR-KO) and intestine-specific Fxr knockout mice (I-FXR-KO) were fed either a chow diet or a chow diet supplemented with 0.5% cholic acid (CA) for 1 week. (A) Hepatic cholesterol content. (B) Gallbladder cholesterol content and (C) Gallbladder phospholipid content were determined. Results are expressed as mean ± S.E. n=3–5, an “*” indicates significant difference, p< 0.05, cholic acid fed vs. chow fed controls. A “**” indicates significant difference between two different groups of mice, p< 0.05. NS: not significant.
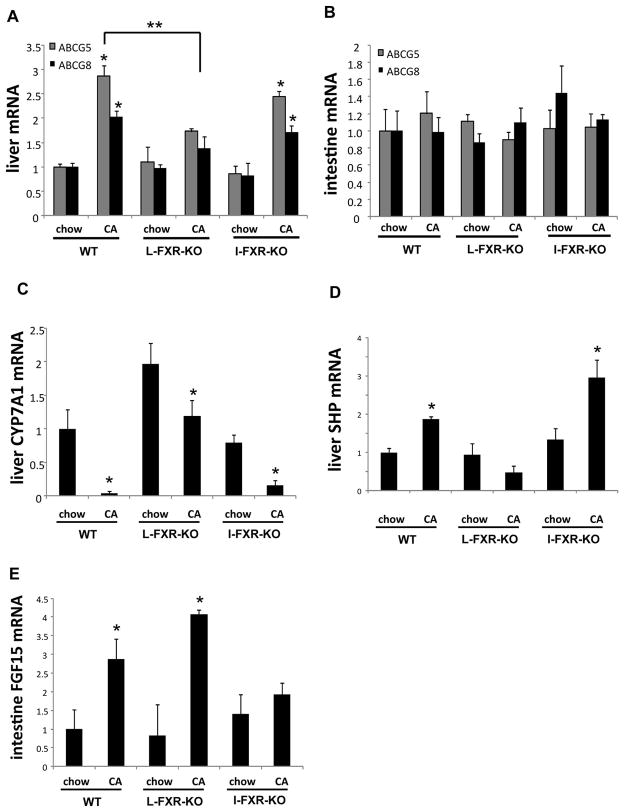
Gene expression analysis showed that CA feeding significantly induced ABCG5 and ABCG8 mRNA expression in the livers of wild type mice and I-FXR-KO mice, but not in the livers of L-FXR-KO mice (Fig 7A). In contrast, CA feeding had no effect on the mRNA expression of intestine ABCG5 and ABCG8 in mice of all three genotypes (Fig 7B). These results further confirmed the role of liver FXR in mediating the bile acid induction of ABCG5/G8 expression in the liver. CA strongly repressed CYP7A1 mRNA expression in wild type mice as expected, but surprisingly had much less effect in L-FXR-KO mice (Fig 7C), despite the fact that loss of liver Fxr abolished CA induction of hepatic SHP while loss of intestine Fxr completely abolished intestine FGF15 induction (Fig 7D&7E). The attenuated repression of CYP7A1 by CA in L-FXR-KO mice may be due to abolished SHP induction in the liver. Taken together, these results suggest that redundant pathways mediate bile acid repression of Cyp7a1 gene.
Fig 7.
Loss of liver Fxr abolished cholic acid induction of ABCG5 and ABCG8 in mouse livers. Wild type, Liver-specific Fxr knockout mice (L-FXR-KO) and intestine-specific Fxr knockout mice (I-FXR-KO) were fed either a chow diet or a chow diet supplemented with 0.5% cholic acid (CA) for 1 week. Hepatic and intestine mRNA expressions were determined by real-time PCR.Results are expressed as mean ± S.E. n=3–5, “*”, statistical significance, p < 0.05, cholic acid fed vs. chow fed controls. A “**” indicates significant difference between two groups of mice, p< 0.05.
Discussion
This study demonstrated that induction of CYP7A1 had profound effects on hepatic cholesterol synthesis, uptake, catabolism and secretion, but hepatic cholesterol homeostasis is maintained to prevent hypercholesterolemia. Increased CYP7A1 promotes biliary and fecal cholesterol secretion without affecting intestine cholesterol absorption in Cyp7a1-tg mice. Induction of CYP7A1 increases CDCA in the bile acid pool, which is the most efficacious ligand of FXR that induces expression of hepatic, but not intestinal cholesterol transporters, ABCG5/ABCG8 and SR-B1, and a hepatic bile acid efflux transporter BSEP. Thus, bile acid synthesis is directly linked to biliary bile acid and cholesterol secretion, but not intestinal cholesterol absorption. In a previous study, lowering circulating cholesterol levels in Cyp7a1-tg mice was attributed to compensatory up-regulation of LDL-mediated uptake of cholesterol, which is converted to bile acids in the liver (5). Since a significant fraction of cholesterol is excreted via feces, the increased biliary cholesterol secretion may be another important mechanism for Cyp7a1-tg mice to eliminate excessive cholesterol and prevent cholesterol accumulation in serum and hepatocytes. The higher ABCG5 and ABCG8 mRNA and protein expressions in the liver and higher biliary cholesterol secretion rate, with unchanged cholesterol absorption in the intestine, provide direct evidence that bile acids promote biliary cholesterol secretion and contribute to higher fecal cholesterol loss in Cyp7a1-tg mice.
Despite increased hepatic cholesterol synthesis, liver cholesterol homeostasis in Cyp7a1-tg mice is maintained. Our results suggest a new mechanism that increased CYP7A1 activity may stimulate de novo cholesterol synthesis and secretion without affecting intestine cholesterol absorption. It is well known that serum cholesterol in mice consists of mainly HDL-C. Thus, induction of LDLR-mediated cholesterol uptake, as previously suggested (13), may not fully explain lower plasma cholesterol in Cyp7a1-tg mice. Instead, bile acid induction of hepatic SR-BI could contribute to both increased hepatic HDL-mediated cholesterol uptake by hepatocytes and biliary cholesterol secretion in Cyp7a1-tg mice (17). SR-BI in the intestine is not induced in Cyp7a1-tg mice, consistent with a report that SR-BI is not required for intestinal cholesterol absorption (17). Bile acid induction of SR-BI in the liver may be mediated by FXR, but the FXR response element has not been identified. A recent study suggests that bile acid induces SR-BI by an indirect mechanism (18).
Intestine fractional cholesterol absorption serves as the first barrier to limit the amount of cholesterol being absorbed and could have a significant effect on biliary cholesterol content. However, our results suggest that increased fecal cholesterol content in Cyp7a1-tg mice is not likely a result of decreased intestinal cholesterol absorption. In the intestine, bile acids form mixed micelles with cholesterol and phospholipids to facilitate absorption of cholesterol and fats. Mice deficient of Cyp7a1 showed a markedly reduced intestinal cholesterol absorption and significantly higher fecal cholesterol content due to bile acid deficiency (19). Cholate has the lowest critical micelle concentration among bile acids, thus is the most effective in facilitating intestinal cholesterol absorption. Cyp8b1 knockout mice are defective in cholic acid synthesis and have reduced intestinal cholesterol absorption despite a slightly increased bile acid pool (20). These studies collectively suggest that both bile acid pool size and CA content are important determinants of intestinal cholesterol absorption. In Cyp7a1-tg mice, CDCA became the predominant bile acid and CA was very low. However, Cyp7a1-tg mice did not show reduced fractional absorption of cholesterol in the absence of CA. This may be explained by an enlarged bile acid pool that compensates for the loss of CA. In Cyp7a1-tg mice, intestine expression levels of ABCG5/G8, NPC1L1 and SRB1 were unaltered, which ruled out the possibility that bile acids could affect intestine cholesterol absorption by regulating these lipid transporters (17, 21).
A previous report shows that LXR induces expression of both CYP7A1 and Abcg5/g8 in mice (10). However, LXR does not induce human CYP7A1 expression (22). It was unexpected that a potent LXR agonist TO901317 or cholesterol treatment failed to induce ABCG5 and ABCG8 in primary human hepatocytes. However, this is consistent with a previous observation that feeding a high cholesterol diet to human ABCG5 and ABCG8 transgenic mice induces mouse Abcg5/g8, but not human ABCG5/G8 mRNA expression in the liver (23). Based on these results, we suggest that LXR may differentially regulate Abcg5/g8 in mice and humans. In mice, cholesterol activates LXR to induce CYP7A1 and ABCG5/ ABCG8 to stimulate cholesterol catabolism and biliary cholesterol secretion, and thus prevents hepatic cholesterol accumulation. The lack of such LXR-mediated mechanisms in human livers suggests that bile acid-activated FXR signaling may play a predominant role in control of hepatic cholesterol homeostasis in humans.
In this study, we demonstrated that FXR/RXR directly bind to a functional FXRE only in the liver. Tissue-specific FXR binding of the Abcg5/g8 gene in this study is consistent to our genome-wide gene profiling study that ~11% of FXR target genes overlap in the liver and in the intestine (24). This suggests that tissue-specific regulation of gene expression by FXR is not limited to abcg5/g8 but may also many other FXR target genes. Combinatorial actions of different transcription factors and co-regulators, as well as histone modification and epigenetic regulation may determine tissue-and gene-specific gene transcription.
In summary, we showed that induction of CYP7A1 expression and expansion of a hydrophobic bile acid pool stimulate cholesterol conversion into bile acids, de novo cholesterol synthesis, and biliary free cholesterol secretion, without increasing intestinal cholesterol absorption. This study underscores the importance of bile acid signaling in maintaining cholesterol homeostasis and preventing hypercholesterolemia.
Supplementary Material
Acknowledgments
This research was supported by NIH grants DK44442 and DK58379 (JYLC), and DK081343 (GLG).
Abbreviations
- ABCG5/G8
ATP binding cassette G5/G8
- CA
cholic acid
- CDCA
chenodeoxycholic acid
- ChIP
chromatin immunoprecipitation assay
- CYP7A1
Cholesterol 7α-hydroxylase
- Cyp7a1-tg mice
Cyp7a1-transgenic mice
- CYP8B1
sterol 12α-hydroxylase
- FXR
farnesoid X receptor
- LXR
liver orphan receptor
- MDR2
multidrug resistance protein 2
- SR-BI
scavenger receptor-BI
Footnotes
Potential conflict of interest: nothing to report
References
- 1.Li T, Owsley E, Matozel M, Hsu P, Novak CM, Chiang JY. Transgenic expression of cholesterol 7α-hydroxylase in the liver prevents high-fat diet-induced obesity and insulin resistance in mice. Hepatology. 2010;52:678–690. doi: 10.1002/hep.23721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chiang JY. Bile acids: regulation of synthesis. J Lipid Res. 2009;50:1955–1966. doi: 10.1194/jlr.R900010-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pullinger CR, Eng C, Salen G, Shefer S, Batta AK, Erickson SK, Verhagen A, et al. Human cholesterol 7α-hydroxylase (CYP7A1) deficiency has a hypercholesterolemic phenotype. J Clin Invest. 2002;110:109–117. doi: 10.1172/JCI15387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hylemon PB, Zhou H, Pandak WM, Ren S, Gil G, Dent P. Bile acids as regulatory molecules. J Lipid Res. 2009;50:1509–1520. doi: 10.1194/jlr.R900007-JLR200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Miyake JH, Duong-Polk XT, Taylor JM, Du EZ, Castellani LW, Lusis AJ, Davis RA. Transgenic Expression of Cholesterol 7α-Hydroxylase Prevents Atherosclerosis in C57BL/6J Mice. Arterioscler Thromb Vasc Biol. 2002;22:121–126. doi: 10.1161/hq0102.102588. [DOI] [PubMed] [Google Scholar]
- 6.Graf GA, Yu L, Li WP, Gerard R, Tuma PL, Cohen JC, Hobbs HH. ABCG5 and ABCG8 are obligate heterodimers for protein trafficking and biliary cholesterol excretion. J Biol Chem. 2003;278:48275–48282. doi: 10.1074/jbc.M310223200. [DOI] [PubMed] [Google Scholar]
- 7.Yu L, Gupta S, Xu F, Liverman AD, Moschetta A, Mangelsdorf DJ, Repa JJ, et al. Expression of ABCG5 and ABCG8 Is Required for Regulation of Biliary Cholesterol Secretion. J Biol Chem. 2005;280:8742–8747. doi: 10.1074/jbc.M411080200. [DOI] [PubMed] [Google Scholar]
- 8.Berge KE, Tian H, Graf GA, Yu L, Grishin NV, Schultz J, Kwiterovich P, et al. Accumulation of dietary cholesterol in sitosterolemia caused by mutations in adjacent ABC transporters. Science. 2000;290:1771–1775. doi: 10.1126/science.290.5497.1771. [DOI] [PubMed] [Google Scholar]
- 9.Yu L, Hammer RE, Li-Hawkins J, Von Bergmann K, Lutjohann D, Cohen JC, Hobbs HH. Disruption of Abcg5 and Abcg8 in mice reveals their crucial role in biliary cholesterol secretion. Proc Natl Acad Sci U S A. 2002;99:16237–16242. doi: 10.1073/pnas.252582399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Repa JJ, Berge KE, Pomajzl C, Richardson JA, Hobbs H, Mangelsdorf DJ. Regulation of ATP-binding cassette sterol transporters ABCG5 and ABCG8 by the liver X receptors alpha and beta. J Biol Chem. 2002;277:18793–18800. doi: 10.1074/jbc.M109927200. [DOI] [PubMed] [Google Scholar]
- 11.Plosch T, van der Veen JN, Havinga R, Huijkman NC, Bloks VW, Kuipers F. Abcg5/Abcg8-independent pathways contribute to hepatobiliary cholesterol secretion in mice. Am J Physiol Gastrointest Liver Physiol. 2006;291:G414–423. doi: 10.1152/ajpgi.00557.2005. [DOI] [PubMed] [Google Scholar]
- 12.Wiersma H, Gatti A, Nijstad N, Oude Elferink RP, Kuipers F, Tietge UJ. Scavenger receptor class B type I mediates biliary cholesterol secretion independent of ATP-binding cassette transporter g5/g8 in mice. Hepatology. 2009;50:1263–1272. doi: 10.1002/hep.23112. [DOI] [PubMed] [Google Scholar]
- 13.Miyake JH, Doung XD, Strauss W, Moore GL, Castellani LW, Curtiss LK, Taylor JM, et al. Increased production of Apo B100-containing lipoproteins in the absence of hyperlipidemia in transgenic mice expressing cholesterol 7α-hydroxylase. J Biol Chem. 2001;276:23304–23311. doi: 10.1074/jbc.M101853200. [DOI] [PubMed] [Google Scholar]
- 14.Kim I, Ahn SH, Inagaki T, Choi M, Ito S, Guo GL, Kliewer SA, et al. Differential regulation of bile acid homeostasis by the farnesoid X receptor in liver and intestine. J Lipid Res. 2007;48:2664–2672. doi: 10.1194/jlr.M700330-JLR200. [DOI] [PubMed] [Google Scholar]
- 15.Zilversmit DB. A single blood sample dual isotope method for the measurement of cholesterol absorption in rats. Proc Soc Exp Biol Med. 1972;140:862–865. doi: 10.3181/00379727-140-36568. [DOI] [PubMed] [Google Scholar]
- 16.Bjorkhem I, Falk O. Assay of the major bile acids in serum by isotope dilution-mass spectrometry. Scand J Clin Lab Invest. 1983;43:163–170. doi: 10.1080/00365518309168239. [DOI] [PubMed] [Google Scholar]
- 17.Mardones P, Quinones V, Amigo L, Moreno M, Miquel JF, Schwarz M, Miettinen HE, et al. Hepatic cholesterol and bile acid metabolism and intestinal cholesterol absorption in scavenger receptor class B type I-deficient mice. J Lipid Res. 2001;42:170–180. [PubMed] [Google Scholar]
- 18.Zhang Y, Yin L, Anderson J, Ma H, Gonzalez FJ, Willson TM, Edwards PA. Identification of novel pathways that control farnesoid X receptor-mediated hypocholesterolemia. J Biol Chem. 2010;285:3035–3043. doi: 10.1074/jbc.M109.083899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Schwarz M, Russell DW, Dietschy JM, Turley SD. Marked reduction in bile acid synthesis in cholesterol 7α-hydroxylase-deficient mice does not lead to diminished tissue cholesterol turnover or to hypercholesterolemia. J Lipid Res. 1998;39:1833–1843. [PubMed] [Google Scholar]
- 20.Li-Hawkins J, Gafvels M, Olin M, Lund EG, Andersson U, Schuster G, Bjorkhem I, et al. Cholic acid mediates negative feedback regulation of bile acid synthesis in mice. J Clin Invest. 2002;110:1191–1200. doi: 10.1172/JCI16309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Altmann SW, Davis HR, Jr, Zhu LJ, Yao X, Hoos LM, Tetzloff G, Iyer SP, et al. Niemann-Pick C1 Like 1 protein is critical for intestinal cholesterol absorption. Science. 2004;303:1201–1204. doi: 10.1126/science.1093131. [DOI] [PubMed] [Google Scholar]
- 22.Chiang JY, Kimmel R, Stroup D. Regulation of cholesterol 7α-hydroxylase gene (CYP7A1) transcription by the liver orphan receptor (LXRa) Gene. 2001;262:257–265. doi: 10.1016/s0378-1119(00)00518-7. [DOI] [PubMed] [Google Scholar]
- 23.Yu L, Li-Hawkins J, Hammer RE, Berge KE, Horton JD, Cohen JC, Hobbs HH. Overexpression of ABCG5 and ABCG8 promotes biliary cholesterol secretion and reduces fractional absorption of dietary cholesterol. J Clin Invest. 2002;110:671–680. doi: 10.1172/JCI16001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thomas AM, Hart SN, Kong B, Fang J, Zhong XB, Guo GL. Genome-wide tissue-specific farnesoid X receptor binding in mouse liver and intestine. Hepatology. 2010;51:1410–1419. doi: 10.1002/hep.23450. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.