Abstract
Longitudinal trajectories of depressive symptoms, perceived support from family, and perceived support from friends were examined among 816 emerging adults (480 women; 59%). In the context of a larger longitudinal investigation on the predictors and course of depression, data were drawn from eight self-report questionnaire assessments that roughly spanned the third decade of life. An age-based scaling approach was used to model trajectories of depressive symptoms and perceived social support between the ages of 21 and 30. Associative models of the relations between depressive symptoms and perceived social support from family and friends were tested. Results indicated that depressive symptoms decreased and perceived social support increased during the study period. Associative models suggested that among women, higher initial levels of perceived support from family predicted slower decreases in depressive symptoms (b = .34, p < .01). Among men, higher initial levels of depressive symptoms predicted slower increases in perceived family support (b = −.23, p < .05). Cross-domain predictive effects were not observed for perceived support from friends and depressive symptoms. Implications of the findings are discussed.
Keywords: Depression, Social Support, Emerging Adulthood
A considerable amount of research has explored the relationship between depressive experiences and social support (Brown & Harris, 1978; Coyne & Downey, 1991). Evidence suggests that social support prospectively predicts depressive symptoms (Kendler, Myers, & Prescott, 2005; Moos, Cronkite, & Moos, 1998; Stice, Ragan, & Randall, 2004). The reverse path, in which depressive symptoms erode social support, has received mixed support (Davila, Bradbury, Cohan, & Tolchuk, 1997; Moos et al., 1998; Stice et al., 2004). In conjunction, these findings support poor social support as a vulnerability to depressive symptom increases, and partially support a reciprocal effects model in which depressive symptoms also portend decreases in social support. The primary purpose of the present study was to examine the cross-sectional and prospective relations between depressive symptoms and two sources of perceived social support (friend and family) in emerging adulthood.
Although extensive research has examined the relations between social support and depressive symptoms among adolescents (Prinstein, Borelli, Cheah, Simon, & Aikins, 2005; Sheeber, Hops, Alpert, Davis, & Andrews, 1997; Stice et al., 2004), little attention has been paid to the relations between these variables in emerging adulthood. Emerging adulthood refers to a developmental period between adolescence and adulthood that is relatively independent from social roles and normative expectations (Arnett, 2000). Emerging adults experience more independence than adolescents, but do not have the normative responsibilities of adulthood. They face rapidly changing social opportunities and challenges, such as achieving autonomy from parents and increasing stability and intimacy in social and romantic relationships (Arnett, 2000; Reis, Lin, Bennett, & Nezlek, 1993). In spite of these rapid changes, the transition to adulthood is often gradual and is characterized by ebbs and flows. For example, many emerging adults experience fluctuations between autonomy from and dependence upon families of origin, as reflected in fluid financial, professional, and living arrangements (Cohen, Kasen, Chen, Hartmark, & Gordon, 2003). Research also suggests that supportive relationships may facilitate successful transitions to the roles of adulthood (Shulman, Kalnitzki, & Shahar, 2009). Given these findings and the unique developmental aspects of emerging adulthood, social support may be especially important for emotional well-being during this period. Moreover, based on research that demonstrates the deleterious interpersonal effects of depression (see Pettit & Joiner, 2006), it seems plausible that depressive symptoms may interfere with the development and maintenance of stable, intimate relationships, including the formation of new families. The impact of this effect may be particularly strong in emerging adulthood because of the developmental task of cultivating closer social relationships (Roisman, Masten, Coatsworth, & Tellegen, 2004).
During emerging adulthood, mean levels of social support tend to increase (Schulenberg, O’Malley, Bachman, & Johnston, 2005) and mean levels of depressive symptoms tend to decrease (Galambos, Baker, & Krahn, 2006). Little work has examined longitudinal relations between social support and depressive symptoms during this period. The limited evidence suggests that increases in general social support map onto decreases in depressive symptoms from ages 18-25, especially among women (Galambos et al., 2006). Higher support from parents has been shown to predict better adjustment over time (Holahan, Valentiner, & Moos, 1994; Shulman et al., 2009), and higher support from siblings and spouses has been concurrently related to better adjustment (Davila et al., 1997; Milevsky, 2005). To our knowledge, the path from depressive symptoms to changes in perceived social support has not been examined in this period, and very little research has considered another source of social support: Friends. These are important limitations, because there is evidence that the direction of the relations between perceived social support and depressive symptoms may depend on the source of support. Parental (not peer) support predicted change in depressive symptoms over time in adolescence (Stice et al., 2004) and emerging adulthood (Shulman et al., 2009), but depressive symptoms predicted change in peer (not parental) support over time in adolescence (Stice et al., 2004).
Family support and friend support may relate differentially to depressive symptoms for multiple reasons. First, familial relations are involuntary, in the sense that people do not select family members (except in marriage). Friendship, in contrast, is characterized by the voluntary selection and maintenance of relationships (Collins & van Dulmen, 2006). Second, family members tend to be psychologically closer than friends (Antonucci, 1994) and may therefore have a greater impact on well-being. Third, relationships with family and friends may serve different functions, with friends primarily satisfying needs for social integration and self-worth, and family and romantic partners primarily satisfying needs for intimacy and emotional support (Barry, Madsen, Nelson, Carroll, & Badger, 2009; Furman & Buhrmester, 1992). Finally, certain aspects of the emerging adulthood period, such as the formation of new families and the movement back and forth between dependency on and independence from family of origin, suggest that family support may be especially linked to well-being in this period.
In addition to direct associations between perceived social support and depressive symptoms, it is also possible that different sources of support may operate in an additive or interactive manner to impact depressive symptoms. For example, the presence of positive support in one domain (e.g., friends) may buffer the negative impact of poor support in another domain (e.g., family). This phenomenon of cross-domain buffering has received mixed support, with some studies finding that high friend support buffers against depressive symptoms in the face of low family support (Barrera & Garrison-Jones, 1992) and others not (Cumsille & Epstein, 1994). Unfortunately, most longitudinal research on social support and depressive symptoms has not considered the source of support or interactions between sources of support.
The present study sought to address these limitations while investigating the relations between depressive symptoms and perceived social support in emerging adulthood. Hypotheses were derived from Lewinsohn, Hoberman, Teri, and Hautzinger’s (1985) integrative model of depression. The integrative model posits that disruptions in social reinforcement patterns initiate a sequence culminating in depression, which feeds back into continued social disruption. Based on this model, past research (e.g., Kendler et al., 2005), and the unique developmental aspects of emerging adulthood, we hypothesized reciprocal effects between depressive symptoms and perceived social support, particularly support from family (broadly defined to include parents, siblings, spouses, and children). As compared to prior research with adolescents that focused on parental support (e.g., Stice et al., 2004), our broader conceptualization of family reflects the unique developmental aspects of emerging adulthood in which individuals often rely on families of origin and begin to form new families. We also examined cross-domain buffering. Given the mixed previous findings from cross-sectional studies, we refrained from making hypotheses and tested cross-domain buffering in an exploratory manner. Finally, we examined gender as a moderator of the relations between social support and depressive symptoms. On average, women display a stronger relational orientation and affiliative style than men, meaning that women are more likely to prefer close emotional communication and to define themselves and base their self-worth on the quality of interpersonal relationships (Cambron, Acitelli, & Pettit, 2009). Consequently, social functioning and emotional well-being may be more closely intertwined in women than men. Consistent with that notion, research suggests that depressive symptoms more closely relate to social support in women than men (e.g., Flaherty & Richman, 1989; Galambos et al., 2006). We therefore expected to find stronger associations between social support and depressive symptoms among women than men.
Method
Sampling Strategy
The sample was drawn from the Oregon Adolescent Depression Project (OADP). Participants (n=1709) were randomly selected from high schools in western Oregon and completed an initial (T1) assessment (mean age 16.6, SD = 1.2). One year later, 1507 (88%) returned for a second evaluation (T2). Differences between the sample and the larger population from which it was selected, and between participants and those who declined to participate or dropped out of the study before T2, were minimal. T1 participants and non-participants were similar on gender, gender of head of household, family size, parental employment status, middle class socioeconomic status, and race. Those lost to attrition at T2 had a higher lifetime rate of disruptive behavior disorders than those who completed T2, but did not differ on any other Axis I diagnosis, demographic feature, or self-report symptom measure. At age 24, all participants with a history of Axis I psychopathology by T2 (n = 644) and a random sample of participants with no T2 history of psychopathology (n = 457) were invited to participate in a third (T3) evaluation. Due to the extensive expenditures associated with re-assessing all T2 participants, the focus was intentionally narrowed to participants with prior histories of psychopathology and a randomly selected subset of participants with no history of psychopathology. Of those invited, 941 (85%) completed the T3 evaluation. T2 diagnostic groups did not differ on T3 participation rate. At age 30 (mean = 30.1 years, SD = .71), all T3 participants were invited to participate in a T4 evaluation, and 816 (87%) completed the interview. Among those invited to T3 and T4 assessments, women were more likely than men to complete evaluations, χ2 > 5.99, p’s < .05; participation did not differ as a function of other demographic variables or previous diagnoses.
The T4 sample included 480 (59%) women and 453 (56%) married participants. The racial and ethnic distribution was consistent with that of western Oregon: 89.2% White, 2.7% Hispanic, 2.7% Asian/Asian American, 2.6% Native American, 1.1% African American, and 1.7% who selected “Other.” Educational status was as follows: 2.0% did not complete high school, 15.7% completed high school or trade school, 39.3% completed some college, 32.3% graduated college, and 10.7% held a graduate or professional degree. Thirty-eight percent reported an annual income greater than $50,000, and an additional 45.3% reported annual income from $20,000-50,000. The remainder (17%) reported annual income below $20,000.
The 816 participants who completed the four major assessments represent the reference sample for this investigation. In addition to the four major assessment points, participants completed up to seven annual questionnaires that included measures of depressive symptoms and perceived social support (mean age at first questionnaire = 21.53, SD = 1.51 years).Given the emphasis on emerging adulthood and the use of different social support measures at T1 and T2, the present study used data from the seven annual questionnaires and T4. At each of the eight assessment waves, an average of 87.8% of the sample provided data.
Participants provided written informed consent following a study description. This research complied with APA ethical standards and was approved by an Institutional Review Board.
Measures
Center for Epidemiologic Studies-Depression Scale
(CES-D; Radloff, 1977). The CES-D is a reliable and valid 20-item measure of the frequency of depressive symptoms in the past week (e.g., Roberts, Lewinsohn, & Seeley, 1991). Scores on each item range from 0-3, and higher total scores indicate greater severity. Recommended clinical cut-off scores range from 16-24 (Radloff, 1977; Roberts et al., 1991). The scale has displayed moderate test-retest reliability over periods up to one year, with r ranging from .32 to .67. Internal reliability in the present sample was good, with coefficient alpha ranging from .91-.92 across the assessment waves.
Perceived Social Support – Family (PSS-Fa) and Friend (PSS-Fr)
(Procidano & Heller, 1983). The 10-item versions of the PSS-Fa and PSS-Fr were used to measure the degree to which individuals believe that their family and friends, respectively, fulfill their needs for support, feedback, and information. For the PSS-Fa, participants were instructed to consider a family to consist of parents, a spouse, siblings, or children. Items are scored dichotomously, with higher scores reflecting higher perceived support. The measures’ internal consistencies and validities have been supported (Procidano & Heller, 1983). Coefficient alpha was acceptable for both measures across assessment waves (.86-.92 for PSS-Fa, .83-.89 for PSS-Fr).
Analytic Approach
Latent growth modeling (LGM) was used to describe latent trajectories in each domain from age 21 to age 30 and to examine cross-sectional and prospective relationships between perceived social support and depressive symptoms. Advantages of LGM are that individuals do not have to be measured at all waves and that measurement intervals do not have to be constant. In such cases, maximum likelihood estimation was used to incorporate missing data points. All models were estimated using the statistical program Mplus 5.1 (Muthén & Muthén, 1998-2008).
In total, measures were collected at eight waves. Due to age heterogeneity at each wave, data were available at every year of age from 21 to 30 (although no participant had over eight data points). We used an age-based approach that allowed us to examine the 10-year age span represented in the sample. Age was scaled to the youngest value (21) at the first wave, and the outcome at each age year was read in as a separate variable (Mehta & West, 2000). Participants were assumed to have missing data at ages for which they did not provide data. Such missing data points are considered missing by design, and tests confirmed that the missing completely at random criterion was met (available upon request to the first author). This approach takes advantage of the age heterogeneity within assessment points and bridges the data gap in years without assessment. The number of participants with data at each age year is listed in Table 1.
Table 1.
Observed Means and Standard Deviations on Measured Variables.
| Women | Men | ||||||
|---|---|---|---|---|---|---|---|
| Age | n | CES-D | PSS-Fa | PSS-Fr | CES-D | PSS-Fa | PSS-Fr |
| 21 | 328 | 14.9 (11.7) |
8.3 (2.7) |
9.4 (1.6) |
12.2 (9.1) |
7.5 (2.9) |
8.7 (2.3) |
| 22 | 471 | 14.8 (10.9) |
8.6 (2.5) |
9.3 (1.8) |
12.9 (9.1) |
7.9 (2.7) |
8.6 (2.4) |
| 23 | 576 | 13.8 (10.5) |
8.5 (2.6) |
9.4 (1.6) |
12.5 (9.3) |
8.0 (2.8) |
8.5 (2.3) |
| 24 | 597 | 13.6 (10.8) |
8.9 (1.9) |
9.5 (1.4) |
11.4 (8.5) |
7.9 (2.8) |
8.7 (2.2) |
| 25 | 542 | 12.2 (9.8) |
9.1 (2.1) |
9.5 (1.3) |
10.5 (8.9) |
8.5 (2.4) |
8.7 (2.2) |
| 26 | 513 | 12.1 (10.6) |
8.0 (2.2) |
9.5 (1.5) |
11.0 (9.1) |
8.4 (2.6) |
8.9 (2.1) |
| 27 | 462 | 12.4 (10.7) |
9.0 (2.2) |
9.4 (1.6) |
10.6 (8.9) |
8.5 (2.6) |
8.8 (2.1) |
| 28 | 368 | 11.8 (10.1) |
9.0 (2.3) |
9.5 (1.3) |
11.3 (10.6) |
8.8 (2.1) |
8.9 (1.9) |
| 29 | 434 | 11.9 (10.2) |
9.1 (2.1) |
9.5 (1.4) |
9.6 (8.5) |
8.8 (2.3) |
8.7 (2.4) |
| 30 | 441 | 11.3 (10.4) |
9.3 (1.8) |
9.5 (1.5) |
9.7 (8.3) |
8.9 (2.4) |
9.1 (1.9) |
Note. N = 816. Standard deviations are reported in parentheses. CES-D = Center for Epidemiological Studies-Depression Scale; PSS-Fa = Perceived Social Support-Family; PSS-Fr = Perceived Social Support-Friend.
In each domain, we tested models of no growth (i.e., models with no slope), linear growth, and quadratic growth. Due to the high likelihood of auto-correlated residuals that reflect test-retest properties in longitudinal data, as well as findings that the failure to consider such correlations may lead to biased estimates of standard errors and poor model fit (e.g., Sivo, Fan, & Witta, 2005), auto-correlated residuals were modeled. In associative models, residuals across domains were correlated within each wave to account for shared method variance (Cole, Ciesla, & Steiger, 2007). Gender moderation was examined using multiple group analyses. Because participants with histories of psychopathology were oversampled at T3, sampling weights that reflected the probability of selection for T3 were used in all analyses. Model fit was evaluated with the comparative fit index (CFI) and the Tucker-Lewis index (TLI), with values ≥ .90 representing acceptable fit, and the root-mean-square error of approximation (RMSEA), with values ≤ 0.05 representing acceptable fit (Bentler, 1990; Brown & Cudeck, 1993).
Results
Univariate Unconditional Growth Models
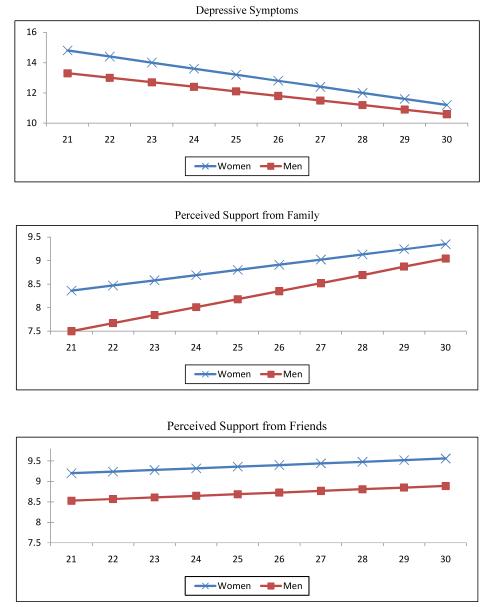
Observed means and standard deviations on the outcome variables at each age year are presented separately by gender in Table 1. Mean depressive symptom scores were consistently in the subclinical range. Model fit indices for the retained model within each domain are presented in Table 2 for women and Table 3 for men. Parameter estimates (Est), standard errors (SE), and critical ratios (CR) are presented in the lower sections of the Tables. In each domain, the linear growth models were retained because they provided a significantly better fit than the no growth models (all χ2 differences > 16.96, df = 3, all p’s < .001) and provided greater parsimony despite not significantly differing from the quadratic models (all χ2 differences < 8.25, df = 4, all p’s > .05). The estimated mean scores from the linear models are plotted in Figure 1.
Table 2.
Model Fit Indices, Parameter Estimates, Standard Errors, and Critical Ratios for Unconditional Growth Models in Women.
| CES-D | PSS-Family | PSS-Friend | |
|---|---|---|---|
| χ2, df | 52.47, 41 | 76.32, 41 | 72.80, 41 |
| CFI | .99 | .92 | .90 |
| TLI | .99 | .92 | .90 |
| RMSEA | .02 | .04 | .04 |
| Est. | SE | Critical Ratio | Est. | SE | Critical Ratio | Est. | SE | Critical Ratio | |
|---|---|---|---|---|---|---|---|---|---|
| Factor mean | |||||||||
| INT | 14.81 | .48 | 30.71 | 8.36 | .13 | 65.41 | 9.26 | .09 | 109.06 |
| Slope | −.43 | .07 | −6.58 | .11 | .02 | 6.83 | .03 | .01 | 2.34 |
| Factor variance | |||||||||
| INT | 71.60 | 7.63 | 9.39 | 5.72 | .53 | 10.84 | 1.74 | .51 | 3.44 |
| Slope | .53 | .16 | 3.23 | .05 | .01 | 5.61 | .03 | .01 | 2.61 |
| Factor covariance | |||||||||
| INT with Slope | −3.25 | .93 | −3.52 | −.40 | .06 | −6.64 | −.14 | .07 | −2.06 |
Note. N = 480. Critical ratios ≥ 1.96 indicate estimates are significant at p < .05. Est. = unstandardized model estimate; SE = standard error of estimated parameter; Critical ratio = estimate divided by standard error; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root-Mean Square Error of Approximation; INT = Intercept.
Table 3.
Model Fit Indices, Parameter Estimates, Standard Errors, and Critical Ratios for Unconditional Growth Models in Men.
| CES-D | PSS-Family | PSS-Friend | |
|---|---|---|---|
| χ2, df | 81.66, 41 | 88.69, 41 | 45.17, 41 |
| CFI | .95 | .96 | .99 |
| TLI | .95 | .95 | .98 |
| RMSEA | .05 | .05 | .02 |
| Est. | SE | Critical Ratio | Est. | SE | Critical Ratio | Est. | SE | Critical Ratio | |
|---|---|---|---|---|---|---|---|---|---|
| Factor mean | |||||||||
| INT | 13.32 | .52 | 25.65 | 7.50 | .18 | 42.97 | 8.53 | .14 | 59.98 |
| Slope | −.38 | .07 | −5.38 | .17 | .02 | 7.81 | .03 | .02 | 1.30 |
| Factor variance | |||||||||
| INT | 53.42 | 7.70 | 6.93 | 7.76 | .83 | 9.37 | 3.54 | .74 | 4.77 |
| Slope | .39 | .15 | 2.54 | .09 | .01 | 6.55 | .05 | .02 | 3.36 |
| Factor covariance | |||||||||
| INT with Slope | −1.74 | .92 | −1.89 | −.57 | .09 | −6.21 | −.22 | .09 | −2.22 |
Note. N = 336. Critical ratios ≥ 1.96 indicate estimates are significant at p < .05. Est. = unstandardized model estimate; SE = standard error of estimated parameter; Critical ratio = estimate divided by standard error; CFI = Comparative Fit Index; TLI = Tucker-Lewis Index; RMSEA = Root-Mean Square Error of Approximation; INT = Intercept.
Figure 1.
Estimated means from the unconditional growth models. Age is on the on x-axes.
Depressive Symptoms
The linear model provided a good fit for women and men (Tables 2 and 3). A multiple group model with intercept and slope factors constrained to be equal across gender provided a good fit, χ2, df = 127.86, 84; CFI = .98; TLI = .98; RMSEA = .04. Relaxing the intercept equality constraint led to a significantly better fit, χ2 difference (1, N = 816) = 10.97, p < .005, indicating that women had significantly higher initial levels of depressive symptoms than men. Relaxing the slope equality constraint did not improve fit, χ2 difference (1, N = 816) = 2.01, p > .05. As displayed in the top panel in Figure 1, growth in depressive symptoms was characterized by linear decreases from age 21-30. Intercept and slope were not significantly correlated among men (r = −.28, p > .05), but were significantly and negatively correlated among women (r = −.53, p < .01), such that women who scored higher on depressive symptoms at age 21 experienced a faster rate of decrease over time.
Perceived Family Support
The linear model provided a good fit for women and men (Tables 2 and 3). A multiple group model with intercept and slope factors constrained to be equal across gender provided an acceptable fit based on indices of the variance accounted for by the model, χ2, df = 272.15, 84; CFI = .93; TLI = .92, and a marginal fit on the basis of an index of the standardized residuals from the model, RMSEA = .06. Relaxing the intercept equality constraint led to a significantly better model fit, χ2 difference (1, N = 816) = 10.67, p < .005, suggesting that women endorsed significantly higher initial levels of perceived family support than men. Relaxing the slope equality constraints led to further improvement in fit, χ2 difference (1, N = 816) = 5.85, p < .05, suggesting that the rate of increase in perceived family support was significantly greater among men than women. As displayed in the middle panel in Figure 1, growth in perceived family support was characterized by linear increases from age 21-30. Intercept and slope were significantly and negatively correlated (for women, r = −.74, p < .01; for men, r = −.69, p < .01), indicating that participants who scored higher at age 21 experienced a slower rate of increase in perceived family support over time.
Perceived Friend Support
The linear model provided an adequate fit for women and a good fit for men (Tables 2 and 3). A multiple group model with intercept and slope factors constrained to be equal across gender provided a marginal fit, χ2, df = 149.03, 84; CFI = .88; TLI = .87; RMSEA = .04. Relaxing the intercept equality constraint led to a significantly better fit, χ2 difference (1, N = 816) = 21.95, p < .001, CFI = .92; TLI = .91; RMSEA = .04, indicating that women reported higher initial levels of perceived friend support than men. Relaxing the slope equality constraint did not improve fit, χ2 difference (1, N = 816) =.06, p > .05. As displayed in the bottom panel in Figure 1, growth in perceived friend support was characterized by linear increases from age 21-30, although the mean slope was not significant for men. In light of the significant improvement in fit when including the slope factor and the significant variance of the slope factor, its nonsignificant mean indicates that some men experienced an increase in friend support and others experienced a decrease, such that the mean slope coefficient did not differ from zero. Intercept and slope were significantly and negatively correlated (for women, r = −.65, p < .01; for men, r = −.50, p < .05), indicating that participants who scored higher at age 21 experienced a slower rate of increase. It is possible that this correlation, as well as the intercept-slope correlation for perceived family support, may reflect a ceiling effect in that participants who scored highly at age 21 may have had little room to increase in perceived support.
Associative Models
Associative model results are presented separately by gender for ease of presentation. Significance tests of gender moderation effects are reported.
Depressive Symptoms and Perceived Family Support
The associative model between depressive symptoms and perceived family support provided an acceptable fit for women and men (CFI = .94, .91; TLI = .93, .91; RMSEA = .04, .05). Significant correlations (for women, r = −.54, p < .01; for men, r = −.29, p < .05) between the intercepts indicate that participants high in initial level of depressive symptoms tended to be low in initial level of perceived family support. This relationship was significantly stronger among women than men, χ2 difference (1, N = 816) =5.03, p < .05. Significant correlations (for women, r = −.66, p < .01; for men, r = −.29, p < .05) between the slopes suggest that participants who experienced a faster decrease in depressive symptoms experienced a faster increase in perceived family support. This association was significantly stronger among women than men, χ2 difference (1, N = 816) =4.68, p < .05.
To determine whether initial levels in one domain predicted the rate of change in the other domain, we reparameterized the associative model by regressing the two slope factors on the two intercept factors. Multiple group analyses revealed that model fit significantly improved when the regression paths were freed to vary across gender, χ2 difference (2, N = 816) =13.30, p < .01. Among women, the path from the intercept of depressive symptoms to the slope of perceived family support was not significant (b = −.06, p > .05), indicating that initial levels of depressive symptoms did not predict change in family support over time. In contrast, the path from the intercept of perceived family support to the slope of depressive symptoms was significant (b = .34, p < .01). The beta weight indicates that a 1 SD increase in the perceived family support intercept corresponded to a .34 SD increase in the depressive symptoms slope. The negative slope means that higher initial levels of perceived family support predicted a slower decrease in depressive symptoms. Among men, the path from the intercept of depressive symptoms to the slope of perceived family support was significant (b = −.23, p < .01), such that higher initial levels of depressive symptoms predicted slower increases in perceived family support through age 30. For every 1 SD increase in the depressive symptoms intercept, the perceived family support slope decreased by .23 SD. The path from the intercept of perceived family support to the slope of depressive symptoms was not significant among men (b = −.006, p > .05).
Depressive Symptoms and Perceived Friend Support
The associative model between depressive symptoms and perceived friend support provided an acceptable fit for women and men (CFI = .90, .92; TLI = .90, .91; RMSEA = .05, .05). Significant correlations (for women, r = −.53, p < .01; for men, r = −.39, p < .01) between the intercepts indicate that participants high in initial level of depressive symptoms tended to be low in initial level of perceived friend support. The magnitudes of these correlations did not differ by gender, χ2 difference (1, N = 816) =.05, p > .05. A significant correlation (r = −.44, p < .01) between the slopes among women suggests that the rate of change in depressive symptoms significantly associated with the rate of change in perceived friend support. The slopes of perceived friend support and depressive symptoms were not significantly correlated among men (r = −.08, p > .05). The magnitude of this association was significantly stronger among women than men, χ2 difference (1, N = 816) =12.47, p < .001.
The regressions of the two slope factors on the two intercept factors were examined to determine whether initial level in one domain predicted change in the opposite domain. In contrast to hypothesis, neither cross-domain effect was significant (largest b = −.16, p’s > .05). Multiple group analyses revealed that gender did not moderate the relations between depressive symptoms and perceived friend support, χ2 difference (2, N = 816) =2.25, p > .05.
Cross-Domain Buffering: Perceived Family Support and Perceived Friend Support
The observed scores for perceived family support and perceived friend support were significantly correlated at each assessment wave (r’s ranged from .30 to .42, mean r = .36, all p’s < .01). An associative LGM between perceived family support and perceived friend support provided an acceptable fit to the data for women and a marginal fit for men (CFI = .93, .89; TLI = .93, .87; RMSEA = .04, .06). Significant correlations (for women, r = .56, p < .01; for men, r = .32, p < .05) between the intercepts indicate that participants high in initial level of perceived family support tended to be high in initial level of perceived friend support. This correlation was significantly stronger for women than men, χ2 difference (1, N = 816) = 4.88, p < .05. Significant correlations (for women, r = .71, p < .01; for men, r = .49, p < .05) between the slopes suggest that participants who experienced a faster rate of change in perceived family support also experienced a faster rate of change in perceived friend support. This correlation did not significantly differ across gender, χ2 difference (1, N = 816) =3.42, p > .05.
To determine whether perceived support from family interacted with perceived support from friends to predict change in depressive symptoms, we ran an associative model with all three variables. The intercept and slope of depressive symptoms were regressed on the intercepts of perceived friend support and perceived family support and the cross-product of perceived friend and family intercepts. Because cross-domain buffering was tested in an exploratory manner, alpha was set at .10. The interaction term did not significantly predict intercept or slope of depressive symptoms for women (Est’s = .08, −.01; SE’s = .10, .02; CR’s = .79, −.71; p’s > .10) or men (Est’s = −.06, .02; SE’s = .18, .02; CR’s = −.38, 1.22, p’s > .10).
Discussion
The present findings indicate that emerging adulthood is characterized by a decreasing course of depressive symptoms and an increasing course of perceived social support. Also, emerging adults who experienced increases in perceived social support were more likely to experience concomitant decreases in depressive symptoms. Overall, emerging adulthood appears to be a period of increasingly positive mental health and social functioning. This accords with the developmental perspective of enhanced stability and intimacy in interpersonal relationships in emerging adulthood (Arnett, 2000; Reis et al., 1993), and is consistent with others’ findings for depressive symptoms (e.g., Galambos et al., 2006). Improvements in the perceived supportiveness of relationships may be due in part to individuals’ greater control in selecting friends, romantic partners, and spouses based on interests and compatibility (Reis, Collins, & Berscheid, 2000). Alternatively, they may reflect a depression-distortion effect, wherein perceptions of social support are biased by current mood state (i.e., as depressive symptoms decreased, the perception of social support as fulfilling increased).
As expected, perceived support from family was significantly associated with depressive symptoms although the direction of the effects differed by gender. Among women, higher levels of perceived family support at age 21 predicted a slower decrease in depressive symptoms through age 30. Initial levels of depressive symptoms did not predict change in perceived family support. This pattern is consistent with findings among adolescent girls of a unidirectional effect of parental support predicting depressive symptoms (Stice et al., 2004), although the present finding of a relation between high family support and a slower rate of decrease in depressive symptoms was unexpected. One possible explanation is a floor effect for depressive symptoms among women high in family support. The moderate correlation (r = −.54) between initial levels of depressive symptoms and family support among women is consistent with this possibility. A related explanation is that women low in family support at age 21 may benefit more from the increasing autonomy from families of origin that often occurs during emerging adulthood. The findings of Galambos et al. (2006) are consistent with this conjecture, as higher levels of conflict with parents at age 18 predicted a faster decrease in depressive symptoms through emerging adulthood. A final explanation is that high family support may sometimes co-occur with behaviors that promote or maintain depressive symptoms in young women. To the extent that close family relations are accompanied by enmeshment and co-rumination, or otherwise interfere with the ability of young women to establish autonomy during emerging adulthood, then they may negatively impact well-being. For example, mother-daughter dyads high in co-rumination reported high relationship quality, but also reported high levels of enmeshment and depressive symptoms (Waller & Rose, 2010). Similarly, among recovered depressed women, a more supportive close family network was associated with increases in depressive symptoms (Veiel, 1993). It seems clear from those investigations that not all family support is equal, and its impact on depressive symptoms in women may differ as a function of related behaviors and developmental level (e.g., adolescence versus emerging adulthood). Furthermore, it is possible that increased autonomy from families of origin in emerging adulthood may enhance emotional well-being among women who have troubled relationships with their families.
It is surprising that depressive symptoms did not predict a more negative course of perceived family support among women, in light of the preponderance of research linking depressive symptoms to poor interpersonal functioning (e.g., Pettit & Joiner, 2006; Prinstein et al., 2005). Rather, the present results suggest that perceived family support may be an antecedent to, not a consequence of, depressive symptom changes in young women.
Among men, higher levels of depressive symptoms at age 21 predicted a slower increase in perceived family support through age 30, but initial levels of perceived family support did not predict change in depressive symptoms. Poor perceived family support may be a consequence, rather than an antecedent, of depressive symptoms in young men. Prior research suggests that the relationships between children and parents become increasingly supportive in the transition from adolescence to young adulthood (Aquilino, 1997; Thornton, Orbuch, & Axinn, 1995). It may be that depressive symptoms interfere with this process in young men, and may also hamper the formation of new families. Depressive symptoms lead to reductions in social activities and reinforcement (cf. Lewinsohn et al., 1985), greater social conflict (Hammen, 1991), and a withdrawal of support from others (Segrin & Abramson, 1994). Further, depressed men display lower levels of socially interactive behaviors than depressed women, and generally display social withdrawal (Troisi & Moles, 1999). It may be that social withdrawal among young men with depressive symptoms negatively impacts perceived family support over time, whereas the comparatively higher level of socially interactive behaviors among women with depressive symptoms minimizes that effect. Although the present study did not examine those variables, they may represent mechanisms by which young men who experience depressive symptoms are less likely to experience increases in supportive familial relations.
In contrast to expectation, no predictive effects were found between depressive symptoms and perceived friend support. This diverges from reports that depressive symptoms predicted a poor course of peer support in adolescence (Stice et al., 2004) and low peer support predicted the onset of depression (Eberhart & Hammen, 2006). However, it is consistent with the idea that family relations are more strongly linked to well-being (Antonucci, 1994) and with studies that have failed to find significant relations between peer support and depressive symptoms (e.g., Shulman et al., 2009; Windle, 1992). In addition to the absence of predictive relationships between depressive symptoms and perceived friend support, a cross-domain buffering model was not supported. This extends mixed findings on buffering among adolescents (Barrera & Garrison-Jones, 1992; Cumsille & Epstein, 1994) to emerging adulthood, and suggests that if cross-domain buffering occurs, it is likely a weak and unreliable effect. As a whole, the findings suggest that perceived support from friends may be correlated with depressive symptoms in emerging adulthood, but that temporally predictive effects are unlikely.
What might explain the absence of predictive relations between perceived friend support and depressive symptoms in this period? The transition from adolescence to emerging adulthood is characterized by an ascendance of romantic partners as sources of support (Furman & Buhrmester, 1992). It may be that the impact of friends, which assumes priority in adolescence, declines in emerging adulthood as romantic relations become more important sources of support. In addition, individuals’ relationships with family members often improve during emerging adulthood and parents are often the preferred source of support when major decisions are considered, as is the case in emerging adulthood (Aquilino, 1997; Shulman et al., 2009). Although friendships provide companionship and social integration during emerging adulthood, their contribution to emotional well-being may be overshadowed by the importance of forming new families and relying on families of origin when navigating the transition to adulthood.
Limitations of the present study must be considered when interpreting the findings. Only self-report measures were included in analyses, and measures of social support were limited to perceptions of the quality of support. We were unable to tease apart distinct sources of family support. It may be that support from family of origin and voluntarily-selected family members (i.e., spouse/partner) relates differentially to depressive symptoms. The generalizability of our findings is limited by an ethnically homogeneous sample and attrition, including higher attrition among men than women. Also, oversampling participants with histories of psychopathology likely led to higher levels of depressive symptoms than in the general population. Sampling weights were used to reduce bias, but replication of these findings in diverse samples is needed.
In summary, the present study suggests that emerging adulthood is a period of increasingly supportive social relationships and increasing emotional well-being. Despite the ascendance of friends as sources of support in adolescence and the increased autonomy from families of origin in emerging adulthood, family support appears to be closely connected to depressive symptoms during this period. Moreover, the relations between depressive symptoms and family support may differ by gender, which suggests that a nuanced approach may be needed when targeting social support to prevent or reduce depressive symptoms. Among emerging adult women, it should not be assumed that higher family support universally leads to decreases in depressive symptoms. It may be important to examine and address additional familial processes, such as enmeshment and co-rumination, which can occur within the context of supportive familial relations but have deleterious effects. In such cases, prevention efforts may target women with the goals of assisting family members in offering support in nurturing, nondirective ways, and assisting women in effectively soliciting familial support while increasing their autonomy (Beach & Gupta, 2006). Among men in emerging adulthood who experience depressive symptoms, special attention may be given to the impact of such symptoms on the amount and quality of social interactions with family members. It may be that reducing depressive symptoms leads to improvements in familial functioning among men (cf. Hirschfeld et al., 2002). In cases in which family members’ negative views of depressed men are firmly entrenched (cf. blame maintenance; Pettit & Joiner, 2006), cognitive-behavioral family interventions geared toward changing depressed men’s interpersonal behaviors and family members’ attributions of them may improve social functioning (e.g., Baucom & Epstein, 1990).
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/fam
Contributor Information
Jeremy W. Pettit, Florida International University
Robert E. Roberts, University of Texas Health Science Center at Houston
John R. Seeley, Oregon Research Institute
Ilya Yaroslavsky, University of Houston.
References
- Antonucci TC. A life-span view of women’s social relations. In: Turner BF, Troll LE, editors. Women growing older: Psychological perspectives. Sage Publications; Thousand Oaks, CA: 1994. pp. 239–269. [Google Scholar]
- Aquilino W. From adolescent to young adult: A prospective study of parent-child relations during the transition to adulthood. Journal of Marriage and the Family. 1997;59:670–686. doi:10.2307/353953. [Google Scholar]
- Arnett JJ. Emerging adulthood: A theory of development from the late teens through the twenties. American Psychologist. 2000;55:469–480. doi:10.1037/0003-066X.55.5.469. [PubMed] [Google Scholar]
- Barrera M, Garrison-Jones C. Family and peer social support as specific correlates of adolescent depressive symptoms. Journal of Abnormal Child Psychology. 1992;20:1–16. doi: 10.1007/BF00927113. doi:10.1007/BF00927113. [DOI] [PubMed] [Google Scholar]
- Barry CM, Madsen SD, Nelson LJ, Carroll JS, Badger S. Friendship and romantic relationship qualities in emerging adulthood: Differential associations with identity development and achieved adulthood criteria. Journal of Adult Development. 2009;16:209–222. doi:10.1007/s10804-009-9067-x. [Google Scholar]
- Baucom DH, Epstein N. Cognitive–behavioral marital therapy. Brunner/Mazel; New York: 1990. [Google Scholar]
- Beach SRH, Gupta M. Directive and nondirective spousal support: differential effects? Journal of Marital and Family Therapy. 2006;32:465–477. doi: 10.1111/j.1752-0606.2006.tb01621.x. doi:10.1111/j.1752-0606.2006.tb01621.x. [DOI] [PubMed] [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. doi:10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Brown GW, Harris T. Social origins of depression: A study of psychiatric disorder in women. Free Press; New York: 1978. [Google Scholar]
- Brown MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen K, Long J, editors. Testing structural equation models. Sage; Newbury Park, CA: 1993. pp. 136–162. [Google Scholar]
- Cambron MJ, Acitelli LK, Pettit JW. Explaining gender differences in depression: An interpersonal contingent self-esteem perspective. Sex Roles. 2009;61:751–761. doi:10.1007/s11199-009-9616-6. [Google Scholar]
- Cohen P, Kasen S, Chen H, Hartmark C, Gordon K. Variations in patterns of developmental transitions in the emerging adulthood period. Developmental Psychology. 2003;39:657–669. doi: 10.1037/0012-1649.39.4.657. doi:10.1037/0012-1649.39.4.657. [DOI] [PubMed] [Google Scholar]
- Cole DA, Ciesla JA, Steiger JH. The insidious effects of failing to include design-driven correlated residuals in latent-variable covariance structure analysis. Psychological Methods. 2007;12:381–398. doi: 10.1037/1082-989X.12.4.381. doi:10.1037/1082-989X.12.4.381. [DOI] [PubMed] [Google Scholar]
- Collins WA, Van Dulmen M. Friendships and romantic relationships in emerging adulthood: Continuities and discontinuities. In: Arnett JJ, Tanner J, editors. Emerging adults in America: Coming of age in the 21st century. American Psychological Association; Washington, DC: 2006. pp. 219–234. doi:10.1037/11381-009. [Google Scholar]
- Coyne JC, Downey G. Social factors and psychopathology: Stress, social support, and coping processes. Annual Review of Psychology. 1991;42:401–425. doi: 10.1146/annurev.ps.42.020191.002153. doi:10.1146/annurev.ps.42.020191.002153. [DOI] [PubMed] [Google Scholar]
- Cumsille PE, Epstein N. Family cohesion, family adaptability, social support, and adolescent depressive symptoms in outpatient clinic families. Journal of Family Psychology. 1994;8:202–214. doi:10.1037/0893-3200.8.2.202. [Google Scholar]
- Davila J, Bradbury TN, Cohan CL, Tochluk S. Marital functioning and depressive symptoms: Evidence for a stress generation model. Journal of Personality and Social Psychology. 1997;73:849–861. doi: 10.1037//0022-3514.73.4.849. doi:10.1037/0022-3514.73.4.849. [DOI] [PubMed] [Google Scholar]
- Eberhart NK, Hammen CL. Interpersonal predictors of onset of depression during the transition to adulthood. Personal Relationships. 2006;13:195–206. doi:10.1111/j.1475-6811.2006.00113.x. [Google Scholar]
- Flaherty J, Richman JA. Gender differences in the perception and utilization of social support: Theoretical perspectives and an empirical test. Social Science and Medicine. 1989;28:1221–1228. doi: 10.1016/0277-9536(89)90340-7. doi:10.1016/0277-9536(89)90340-7. [DOI] [PubMed] [Google Scholar]
- Furman W, Buhrmester D. Age and sex differences in perceptions of networks of personal relationships. Child Development. 1992;63:103–115. doi: 10.1111/j.1467-8624.1992.tb03599.x. doi:10.2307/1130905. [DOI] [PubMed] [Google Scholar]
- Galambos NL, Barker ET, Krahn HJ. Depression, self-esteem, and anger in emerging adulthood: Seven-year trajectories. Developmental Psychology. 2006;42:350–365. doi: 10.1037/0012-1649.42.2.350. doi:10.1037/0012-1649.42.2.350. [DOI] [PubMed] [Google Scholar]
- Hammen CL. The generation of stress in the course of unipolar depression. Journal of Abnormal Psychology. 1991;100:555–561. doi: 10.1037//0021-843x.100.4.555. doi:10.1037/0021-843X.100.4.555. [DOI] [PubMed] [Google Scholar]
- Hirschfeld RM, Dunner DL, Keitner G, Klein DN, Koran LM, Kornstein SG, Keller MB. Does psychosocial functioning improve independent of depressive symptoms? A comparison of nefazodone, psychotherapy, and their combination. Biological Psychiatry. 2002;51:123–133. doi: 10.1016/s0006-3223(01)01291-4. doi:10.1016/S0006-3223(01)01291-4. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Valentiner DP, Moos RH. Parental support and psychological adjustment during the transition to young adulthood in a college sample. Journal of Family Psychology. 1994;8:215–223. doi:10.1037/0893-3200.8.2.215. [Google Scholar]
- Kendler KS, Myers J, Prescott CA. Sex differences in the relationship between social support and risk for major depression: A longitudinal study of opposite-sex twin pairs. American Journal of Psychiatry. 2005;162:250–256. doi: 10.1176/appi.ajp.162.2.250. doi:10.1176/appi.ajp.162.2.250. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Hoberman HM, Teri L, Hautzinger M. An integrative theory of depression. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. Academic Press; New York: 1985. pp. 331–359. [Google Scholar]
- Mehta PD, West SG. Putting the individual back into growth curves. Psychological Methods. 2000;5:23–43. doi: 10.1037/1082-989x.5.1.23. doi:10.1037/1082-989X.5.1.23. [DOI] [PubMed] [Google Scholar]
- Milevsky A. Compensatory patterns of sibling support in early adulthood: variations in loneliness, self-esteem, depression, and life satisfaction. Journal of Social and Personal Relationships. 2005;22:743–755. doi:10.1177/0265407505056447. [Google Scholar]
- Moos RH, Cronkite RC, Moos BS. Family and extrafamily resources and the 10-year course of treated depression. Journal of Abnormal Psychology. 1998;107:450–460. doi: 10.1037//0021-843x.107.3.450. doi:10.1037/0021-843X.107.3.450. [DOI] [PubMed] [Google Scholar]
- Muthén LK, Muthén BO. Mplus: The comprehensive modeling program for applied researchers. User’s guide. 5th ed Muthén & Muthén; Los Angeles: 1998-2008. [Google Scholar]
- Pettit JW, Joiner TE., Jr. Chronic depression: Interpersonal sources, therapeutic solutions. American Psychological Association; Washington, DC: 2006. doi:10.1037/11291-000. [Google Scholar]
- Prinstein MJ, Borelli JL, Cheah CSL, Simon VA, Atkins JW. Adolescent girls’ interpersonal vulnerability to depressive symptoms: A longitudinal examination of reassurance-seeking and peer relationships. Journal of Abnormal Psychology. 2005;114:676–688. doi: 10.1037/0021-843X.114.4.676. doi:10.1037/0021-843X.114.4.676. [DOI] [PubMed] [Google Scholar]
- Procidano M, Heller K. Measures of perceived social support from friends and from family: Three validation studies. American Journal of Community Psychology. 1983;11:1–24. doi: 10.1007/BF00898416. doi:10.1007/BF00898416. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. doi:10.1177/014662167700100306. [Google Scholar]
- Reis HT, Collins WA, Berscheid E. The relationship context of human behavior and development. Psychological Bulletin. 2000;126:844–872. doi: 10.1037/0033-2909.126.6.844. doi:10.1037/0033-2909.126.6.844. [DOI] [PubMed] [Google Scholar]
- Reis HT, Lin Y, Bennett ME, Nezlek JB. Change and consistency in social participation during early adulthood. Developmental Psychology. 1993;29:633–645. doi:10.1037/0012-1649.29.4.633. [Google Scholar]
- Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. Journal of the American Academy of Child and Adolescent Psychiatry. 1991;30:58–66. doi: 10.1097/00004583-199101000-00009. doi:10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- Roisman GI, Masten AS, Coatsworth JD, Tellegen A. Salient and emerging developmental tasks in the transition to adulthood. Child Development. 2004;75:123–133. doi: 10.1111/j.1467-8624.2004.00658.x. doi:10.1111/j.1467-8624.2004.00658.x. [DOI] [PubMed] [Google Scholar]
- Schulenberg JE, O’Malley PM, Bachman JG, Johnston LD. Early adult transitions and their relation to well-being and substance use. In: Settersten RA Jr., Furstenberg FF Jr., Rumbaut RG, editors. On the frontier of adulthood: Theory, research, and public policy. University of Chicago Press; Chicago: 2005. pp. 417–453. [Google Scholar]
- Segrin C, Abramson LY. Negative reactions to depressive behaviors: A communication theories analysis. Journal of Abnormal Psychology. 1994;103:655–668. doi: 10.1037//0021-843x.103.4.655. doi:10.1037/0021-843X.103.4.655. [DOI] [PubMed] [Google Scholar]
- Sheeber L, Hops H, Alpert A, Davis B, Andrews J. Family support and conflict: Prospective relations to adolescent depression. Journal of Abnormal Child Psychology. 1997;25:333–344. doi: 10.1023/a:1025768504415. doi:10.1023/A:1025768504415. [DOI] [PubMed] [Google Scholar]
- Shulman S, Kalnitzki E, Shahar G. Meeting developmental challenges during emerging adulthood: The role of personality and social resources. Journal of Adolescent Research. 2009;24:242–267. doi:10.1177/0743558408329303. [Google Scholar]
- Sivo SA, Fan X, Witta L. The biasing effects of unmodeled ARMA time series processes on latent growth curve model estimates. Structural Equation Modeling. 2005;12:215–231. doi:10.1207/s15328007sem1202_2. [Google Scholar]
- Stice E, Ragan J, Randall P. Prospective relations between social support and depression: Differential direction of effects for parent and peer support? Journal of Abnormal Psychology. 2004;113:155–159. doi: 10.1037/0021-843X.113.1.155. doi:10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- Thornton A, Orbuch T, Axinn W. Parent-child relationships during the transition to adulthood. Journal of Family Issues. 1995;16:538–564. doi:10.1177/019251395016005003. [Google Scholar]
- Troisi A, Moles A. Gender differences in depression: an ethological study of nonverbal behavior during interviews. Journal of Psychiatric Research. 1999;33:243–250. doi: 10.1016/s0022-3956(98)00064-8. doi:10.1016/S0022-3956(98)00064-8. [DOI] [PubMed] [Google Scholar]
- Veiel HOF. Detrimental effects of kin support networks on the course of depression. Journal of Abnormal Psychology. 1993;102:419–429. doi: 10.1037//0021-843x.102.3.419. doi:10.1037/0021-843X.102.3.419. [DOI] [PubMed] [Google Scholar]
- Waller EM, Rose AJ. Adjustment trade-offs of co-rumination in mother-adolescent relationships. Journal of Adolescence. 2010;33:487–497. doi: 10.1016/j.adolescence.2009.06.002. doi:10.1016/j.adolescence.2009.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windle M. A longitudinal study of stress buffering for adolescent problem behaviors. Developmental Psychology. 1992;28:522–530. doi:10.1037/0012-1649.28.3.522. [Google Scholar]