Abstract
BACKGROUND
Antiretroviral chemoprophylaxis before exposure is a promising approach for the prevention of human immunodeficiency virus (HIV) acquisition.
METHODS
We randomly assigned 2499 HIV-seronegative men or transgender women who have sex with men to receive a combination of two oral antiretroviral drugs, emtricitabine and tenofovir disoproxil fumarate (FTC–TDF), or placebo once daily. All subjects received HIV testing, risk-reduction counseling, condoms, and management of sexually transmitted infections.
RESULTS
The study subjects were followed for 3324 person-years (median, 1.2 years; maximum, 2.8 years). Of these subjects, 10 were found to have been infected with HIV at enrollment, and 100 became infected during follow-up (36 in the FTC–TDF group and 64 in the placebo group), indicating a 44% reduction in the incidence of HIV (95% confidence interval, 15 to 63; P = 0.005). In the FTC–TDF group, the study drug was detected in 22 of 43 of seronegative subjects (51%) and in 3 of 34 HIV-infected subjects (9%) (P<0.001). Nausea was reported more frequently during the first 4 weeks in the FTC–TDF group than in the placebo group (P<0.001). The two groups had similar rates of serious adverse events (P = 0.57).
CONCLUSIONS
Oral FTC–TDF provided protection against the acquisition of HIV infection among the subjects. Detectable blood levels strongly correlated with the prophylactic effect. (Funded by the National Institutes of Health and the Bill and Melinda Gates Foundation; ClinicalTrials.gov number, NCT00458393.)
A total of 2.7 million new infections with the human immunodeficiency virus (HIV) were diagnosed worldwide in 2008, according to the Joint United Nations Program on HIV/AIDS (UNAIDS). Combination antiretroviral therapy for patients with HIV infection restores health and may decrease the transmission of the virus to uninfected partners.1 Therapy also decreases mother-to-child transmission.2
Postexposure chemoprophylaxis is recommended after occupational or nonoccupational exposure to HIV-infected fluids.3 The use of such chemoprophylaxis requires that people recognize when they might have been exposed to HIV and that they start therapy within 72 hours. Both challenges are substantial limitations to the use of postexposure chemoprophylaxis.4,5
We selected emtricitabine (FTC) and tenofovir disoproxil fumarate (TDF) combination therapy in a single tablet (FTC–TDF) for evaluation of pre-exposure prophylaxis because of several favorable characteristics.6 (Details are provided in the introduction in the Supplementary Appendix, available with the full text of this article at NEJM.org.) The protective activity of FTC and TDF has been shown in mice transplanted with human immune cells7 and in nonhuman primates.8–10 In these studies, there were increased levels of efficacy when both agents were used together, as compared with the use of either agent alone. The administration of the drug both before and after exposure was important for maximizing the protective benefit.11
Daily preexposure prophylaxis with oral TDF had an acceptable side-effect profile in a trial involving West African women.12 A tenofovir 1% vaginal gel reduced HIV infection rates by 39% among women.13 Men and transgender women who have sex with men are disproportionately affected by the global epidemic.14,15 Surveys of such persons in the United States indicate that the current use of preexposure prophylaxis is rare, although the majority would consider such use if evidence of safety and efficacy became available.16,17
In this multinational study, called the Preexposure Prophylaxis Initiative (iPrEx) trial, we aimed to evaluate the safety and efficacy of once-daily oral FTC–TDF as compared with placebo for the prevention of HIV acquisition among men and transgender women who have sex with men.
METHODS
PROTOCOL DEVELOPMENT
We developed the concept and protocol for this study using methods that came to be approved as “good participatory practices” by UNAIDS.18 The development of the protocol was sponsored by the National Institute of Health’s Division of Acquired Immunodeficiency Syndrome (DAIDS). The protocol was approved by national government public health authorities in Peru, Ecuador, South Africa, Brazil, Thailand, and the United States and by the ethics committee at each site. All subjects provided written informed consent. The study coordinator vouches for the fidelity of the report to the protocol. The study protocol is available at NEJM.org, and a detailed description of the methods is provided in the Supplementary Appendix.
STUDY POPULATION AND RANDOMIZATION
Inclusion criteria were male sex at birth, an age of 18 years or older, HIV-seronegative status, and evidence of high risk for acquisition of HIV infection. Subject codes were randomly assigned in blocks of 10, stratified according to site. The subject codes were assigned consecutively at the study sites to eligible subjects at the time of the first dispensation of a study drug. Serologic testing for hepatitis B was performed at screening.
STUDY VISITS
Study visits were scheduled every 4 weeks after enrollment. Each 4-week visit included drug dispensation, pill count, adherence counseling, rapid testing for HIV antibodies, and taking of a medical history. Chemical and hematologic analyses were performed at weeks 4, 8, 12, 16, and 24 and every 12 weeks thereafter. During screening, a computer-assisted structured interview collected information about education level, self-identified sex, and alcohol use, along with subjects’ perceived study-group assignment at week 12. High-risk behavior was assessed by interview every 12 weeks, and physical examinations and evaluations for sexually transmitted infections were performed at least every 24 weeks. Visits through May 1, 2010, are included in this report of the primary analysis of safety and efficacy. The visit cutoff date was set by the study sponsor without any access to interim findings and was intended to ensure observation of the targeted number of seroconversion events (85). The use of study drugs was intensively monitored and promoted (for details, see Methods in the Supplementary Appendix).
STANDARD PREVENTION INTERVENTIONS
At every scheduled visit, subjects received a comprehensive package of prevention services, including HIV testing, risk-reduction counseling, condoms, and diagnosis and treatment of symptomatic sexually transmitted infections, including gonorrhea and chlamydia urethritis, syphilis, and herpes simplex virus type 2 (HSV-2). In addition, at 24-week intervals, subjects were screened for asymptomatic urethritis, syphilis, antibodies to HSV-2, and genital warts and ulcers; treatment was provided when indicated. Sexual partners were offered treatment of sexually transmitted infections that were diagnosed in the subject. Subjects were linked to local prevention and treatment services when required to receive standard-of-care services. All subjects were instructed to protect themselves from HIV with conventional methods, since they were unaware of their study-group assignment. Subjects who reported a recent unprotected exposure to an HIV-infected partner were referred for postexposure prophylaxis (at sites where such therapy was available), and the administration of a study drug was temporarily suspended. Vaccination against hepatitis B virus (HBV) was offered to all susceptible subjects.
LABORATORY TESTING
Testing for HIV antibody was performed on whole blood with the use of two different rapid tests at every scheduled visit, and reactive rapid tests were tested with the use of Western blot analysis of serum (Fig. S1 in the Supplementary Appendix). Subjects with failed rapid tests were retested during the visit. HIV plasma RNA testing with the use of an assay with a lower limit of quantitation of 40 copies per milliliter was performed if seroconversion was detected within 12 weeks after enrollment. RNA testing was also used to identify the first date of laboratory evidence of infection for the as-treated analysis. Testing for drug-resistance genotyping and phenotyping was performed with the use of clinically validated assays on the basis of the viral load at the seroconversion visit.
SUBGROUP ANALYSIS OF DRUG LEVELS
A prespecified subgroup analysis was performed to investigate whether drug levels correlated with protective effect. Subjects with HIV infection were matched with two control subjects, one from each study group who were selected from among seronegative subjects, according to study site (Fig. S5 in the Supplementary Appendix). Plasma was tested for the presence of FTC and tenofovir (TFV), and peripheral-blood mononuclear cells were tested for FTC triphosphate (FTC-TP) and TFV diphosphate (TFV-DP), which are the active intracellular metabolites of FTC and TFV, respectively, with the use of validated liquid chromatography and tandem mass spectrometry assays.
STUDY OVERSIGHT
The study was designed by four of the investigators in collaboration with all the site investigators and communities. DAIDS reviewers approved the protocol, which was developed by the study investigators, and monitored the conduct of the trial at study sites. The Bill and Melinda Gates Foundation also provided funding but did not have a role in protocol development or site monitoring. Gilead Sciences donated both FTC–TDF and placebo tablets and provided travel-related support for meetings conducted by non-Gilead investigators. The role of Gilead Sciences in the development of the protocol was limited to sections regarding the handling of the study drugs. Neither Gilead Sciences nor any of its employees had a role in the accrual or analysis of the data or in the preparation of the manuscript. DAIDS agreed to give Gilead 30 days to comment on the manuscript, but there was no agreement to accept suggestions. The first author wrote the first draft of the manuscript (except for the drug-level sections, which were drafted by another investigator) and decided to submit the manuscript for publication. The protocol statistician and data manager vouch for the accuracy of the data, and the protocol chair and site investigators vouch for the completeness of the reported data.
STATISTICAL ANALYSIS
Data were collected on case-report forms and faxed to a DataFax server at DF/Net Research. It was determined that the observation of 85 incident HIV infections would yield a power of at least 80% with a one-sided alpha level of 0.05 to reject a null hypothesis of efficacy of 30% or less if the true efficacy were 60% or more. The modified intention-to-treat analysis included available data for all subjects except those with HIV RNA detected in their enrollment sample. The as-treated analysis used a time-dependent covariate indication as to whether the subject was known to fall below the prespecified level of study-drug compliance (50%) on any of the following: records of study-drug dispensation alone, pill-use calculation on the basis of study-drug dispensation and returns, and subjects’ self-report. For the as-treated analysis, pills from unreturned bottles were assumed to have been taken, and late visits were included in the analysis if the last dispensation allowed pill use on 50% or more of days. Safety analyses included all subjects.
RESULTS
STUDY SUBJECTS
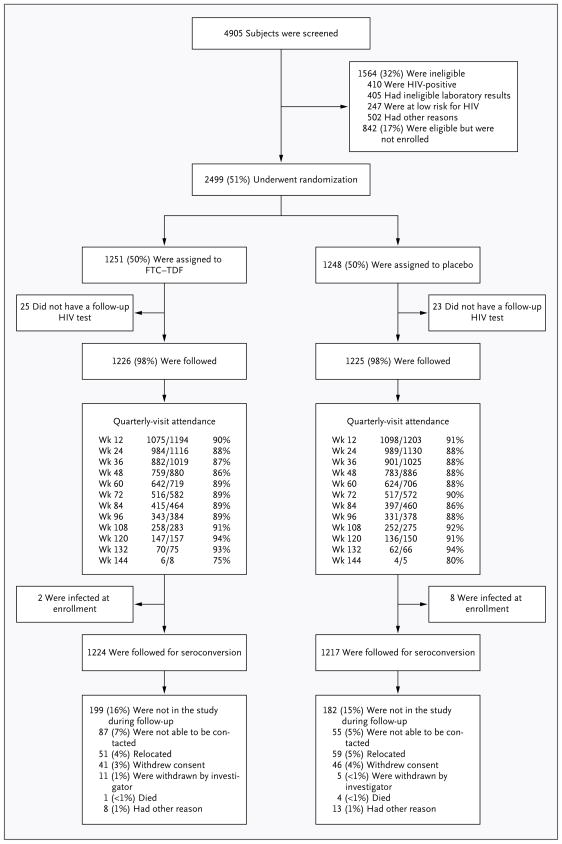
Of 4905 subjects who were screened, 2499 were enrolled in the study from July 10, 2007, through December 17, 2009, at 11 sites in six countries (Fig. 1). The baseline characteristics of the two study groups were similar (Table 1). All subjects were born male, although 29 (1%) reported their current gender identity as female. The ages of the subjects ranged from 18 to 67 years; the FTC–TDF group was on average 9 months older than the placebo group (mean age, 27.5 vs. 26.8 years; P = 0.04).
Figure 1. Enrollment and Outcomes.
The most common laboratory abnormalities that led to exclusion were elevations in hepatic aminotransferase levels, hyperbilirubinemia, and renal insufficiency. A total of 18 enrollees (0.7%) did not meet all eligibility criteria, including 2 subjects with preexisting diabetes mellitus, who were instructed to stop taking a study drug when the history was discovered. All enrolled subjects, including those who were subsequently found to be ineligible, were followed for HIV infection and safety. Quarterly-visit attendance is shown. Visits were considered to have been completed if they occurred before the subsequent visit window, with completion rates of 75 to 94% for all visits. The completion rate was more than 86% for all visits before week 132. Visits occurred within the protocol-defined window of ±5 days in 62 to 86% of visits.
Table 1.
Baseline Characteristics of the Subjects.*
| Characteristic | FTC–TDF (N = 1251) | Placebo (N = 1248) | P Value |
|---|---|---|---|
| Age group — no. (%) | 0.04 | ||
| 18–24 yr | 591 (47) | 662 (53) | |
| 25–29 yr | 274 (22) | 241 (19) | |
| 30–39 yr | 249 (20) | 224 (18) | |
| ≥40 yr | 137 (11) | 121 (10) | |
| Education level — no. (%) | 0.26 | ||
| Less than secondary | 279 (22) | 244 (20) | |
| Completed secondary | 430 (34) | 453 (36) | |
| Postsecondary | 525 (42) | 539 (43) | |
| No answer or missing data | 17 (1) | 12 (1) | |
| Race or ethnic group — no. (%)† | 0.40 | ||
| Black | 117 (9) | 97 (8) | |
| White | 223 (18) | 208 (17) | |
| Mixed race or other | 849 (68) | 878 (70) | |
| Asian | 62 (5) | 65 (5) | |
| Hispanic | 900 (72) | 906 (73) | 0.72 |
| No. of alcoholic drinks (on days when subject drank in past month) — no. (%) | 0.66 | ||
| 0 | 206 (16) | 184 (15) | |
| 1–4 per day | 348 (28) | 345 (28) | |
| ≥5 per day | 666 (53) | 687 (55) | |
| No answer or missing data | 31 (2) | 32 (3) | |
| City and country of residence — no. (%) | 1.00 | ||
| Lima, Peru | 470 (38) | 470 (38) | |
| Iquitos, Peru | 230 (18) | 230 (18) | |
| Guayaquil, Ecuador | 150 (12) | 150 (12) | |
| Rio de Janeiro | 147 (12) | 147 (12) | |
| São Paulo | 39 (3) | 37 (3) | |
| San Francisco | 70 (6) | 70 (6) | |
| Boston | 43 (3) | 44 (4) | |
| Chiang Mai, Thailand | 57 (5) | 57 (5) | |
| Cape Town, South Africa | 45 (4) | 43 (3) | |
| Sexual risk factors at screening | |||
| No. of partners in past 12 wk | 18±35 | 18±43 | 0.51 |
| Unprotected receptive anal intercourse in past 12 wk — no. (%) | 732 (59) | 753 (60) | 0.37 |
| Unprotected anal intercourse with partner with positive or unknown HIV status in past 6 mo — no. (%) | 992 (79) | 1009 (81) | 0.34 |
| Transactional sex in past 6 mo — no. (%) | 517 (41) | 510 (41) | 0.84 |
| Known partner with HIV in past 6 mo — no. (%) | 23 (2) | 32 (3) | 0.22 |
| Sexually transmitted infections diagnosed at screening | |||
| Syphilis seroreactivity — no./total no. (%) | 164/1240 (13) | 162/1239 (13) | 0.95 |
| Serum herpes simplex virus type 2 — no./total no. (%) | 458/1241 (37) | 430/1243 (35) | 0.24 |
| Urine leukocyte esterase positive — no. (%) | 23 (2) | 22 (2) | 1.00 |
| Hepatitis B virus status — no. (%) | 0.11 | ||
| Susceptible | 827 (66) | 803 (64) | |
| Immune because of natural infection | 247 (20) | 222 (18) | |
| Immune because of previous vaccination | 149 (12) | 190 (15) | |
| Current infection with hepatitis B virus | 7 (1) | 6 (<1) | |
| Indeterminate | 21 (2) | 27 (2) |
Plus–minus values are means ±SD. Percentages may not total 100 because of rounding. FTC–TDF denotes emtricitabine and tenofovir disoproxil fumarate.
Race or ethnic group was self-reported.
Among HBV-susceptible subjects at screening, 94% accepted HBV vaccination. We enrolled 13 subjects with chronic HBV infection that was detected at screening, and acute HBV infection was reported as an adverse event in 3 additional subjects (2 in the FTC–TDF group and 1 in the placebo group) after enrollment when elevated liver aminotransferase levels were observed. All the HBV infections resolved with detectable levels of immunity.
FOLLOW-UP AND ADHERENCE
The cohort was followed for 3324 person-years with a variable duration of observation (median, 1.2 years; maximum, 2.8 years) (Fig. 1). There were no significant trends in visit completion rates over time. Most subjects said they did not know their study-group assignment at week 12, and those who guessed their assignment were evenly distributed between the two groups (Table S3 in the Supplementary Appendix). No subjects were told their study-group assignment during the course of the trial. A study drug was temporarily discontinued in 21 subjects (8 in the FTC–TDF group and 13 in the placebo group) so that they could receive postexposure prophylaxis for HIV (P = 0.28).
The rate of self-reported pill use was lower in the FTC–TDF group than in the placebo group at week 4 (mean, 89% vs. 92%; P<0.001) and at week 8 (mean, 93% vs. 94%; P = 0.006) but was similar thereafter (mean, 95% in the two groups). At each visit, a portion of subjects (approximately 6%) did not report the number of pills missed. The percentage of pill bottles returned was 66% by 30 days and 86% by 60 days. The rate of pill use that was estimated according to pill count also increased during the first 8 weeks and then remained stable at a median ranging from 89 to 95%, depending on whether pills from unreturned bottles were counted as having been taken or not taken. On the basis of pill-dispensation dates and quantities, the rate of pill use decreased during the first year, from 99% to 91%, a trend that contrasted with pill counts and self-report, which indicated an increased rate of use.
SEXUAL PRACTICES
Sexual practices were similar in the two groups at all time points (P = 0.97) (Fig. S2 in the Supplementary Appendix). The total numbers of sexual partners with whom the respondent had receptive anal intercourse decreased, and the percentage of those partners who used a condom increased after subjects enrolled in the study. There were no significant between-group differences in the numbers of subjects with syphilis (P=0.49), gonorrhea (P=0.74), chlamydia (P=0.43), genital warts (P = 0.53), or genital ulcers (P = 0.62) during follow-up (Table S4 in the Supplementary Appendix).
SAFETY
In testing for elevations in serum creatinine levels, there were 41 instances of elevations that were at least 1.1 times the upper limit of the normal range or more than 1.5 times the baseline level. Of these elevations, 26 (2%) were in the FTC–TDF group and 15 (1%) were in the placebo group (P = 0.08). Two of these elevations increased in grade, accounting for a total of 43 creatinine adverse events (Table 2, and Table S9 in the Supplementary Appendix). Overall, 18 creatinine elevations (44%) remained in the normal range, and 36 (88%) were not confirmed on the next test. A total of 10 elevations led to discontinuation of a study drug (7 in the FTC–TDF group and 3 in the placebo group); study drugs were restarted in 9 subjects. Serum creatinine levels were elevated at more than one consecutive test in 5 subjects in the FTC–TDF group (<1%) and in none of the subjects in the placebo group. All elevations in the serum creatinine level resolved after the discontinuation of a study drug, within 4 weeks in 3 subjects, within 12 weeks in 1 subject, and within 20 weeks in 1 subject. Four of the subjects resumed taking FTC–TDF without recurrence of the elevation.
Table 2.
Adverse Events.*
| Adverse Event | FTC–TDF (N = 1251) | Placebo (N = 1248) | P Value† | ||
|---|---|---|---|---|---|
| no. of patients (%) | no. of events | no. of patients (%) | no. of events | ||
| Any adverse event | 867 (69) | 2630 | 877 (70) | 2611 | 0.50 |
| Any serious adverse event | 60 (5) | 76 | 67 (5) | 87 | 0.57 |
| Any grade 3 or 4 event | 151 (12) | 248 | 164 (13) | 285 | 0.51 |
| Grade 3 event | 110 (9) | 197 | 117 (9) | 225 | 0.65 |
| Grade 4 event | 41 (3) | 51 | 47 (4) | 60 | 0.57 |
| Elevated creatinine level | 25 (2) | 28 | 14 (1) | 15 | 0.08 |
| Headache | 56 (4) | 66 | 41 (3) | 55 | 0.10 |
| Depression | 43 (3) | 46 | 62 (5) | 63 | 0.07 |
| Nausea | 20 (2) | 22 | 9 (<1) | 10 | 0.04 |
| Unintentional weight loss (≥5%) | 27 (2) | 34 | 14 (1) | 19 | 0.04 |
| Diarrhea | 46 (4) | 49 | 56 (4) | 61 | 0.36 |
| Bone fracture | 15 (1) | 16 | 11 (<1) | 12 | 0.41 |
| Death | 1 (<1)‡ | 1 | 4 (<1) | 4 | 0.18 |
| Discontinuation of study drug | |||||
| Permanently | 25 (2) | 26 | 27 (2) | 33 | 0.82 |
| Permanently or temporarily | 79 (6) | 99 | 72 (6) | 92 | 0.49 |
A listing of all laboratory abnormalities and clinical adverse events of grade 2 or higher that were reported in 25 or more subjects (1%) is provided in Tables S9 and S10 in the Supplementary Appendix. FTC–TDF denotes emtricitabine and tenofovir disoproxil fumarate.
P values were calculated by the log-rank test.
This death was due to a motorcycle accident.
Moderate nausea (grade 2 and above) was reported more frequently in the FTC–TDF group than in the placebo group (22 vs. 10 events, P = 0.04), as was unintentional weight loss of 5% or more (34 vs. 19 events, P = 0.04) (for details, see Table S10 in the Supplementary Appendix).
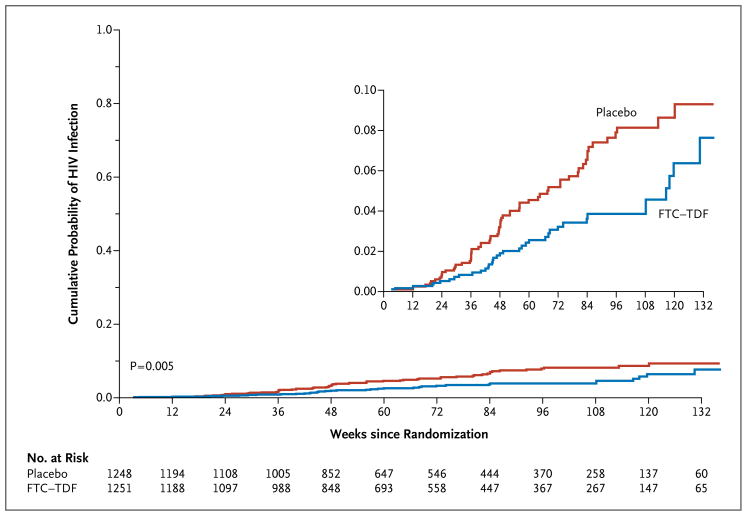
EFFECT OF FTC–TDF ON HIV ACQUISITION
HIV rapid testing was performed at 39,613 visits, during which there were false reactive tests for 3 subjects at 7 visits; each subject had multiple negative tests afterward. HIV seroconversion was observed in 110 persons, of whom 10 had plasma HIV RNA subsequently detected in specimens obtained at the enrollment visit. A finding of fewer than 40 copies per milliliter of plasma HIV RNA was documented for the other 100 HIV-infected subjects before seroconversion. Among the 100 subjects with emergent HIV infection, 36 occurred in the FTC–TDF group, and 64 occurred in the placebo group, representing a relative reduction of 44% in incidence in the modified intention-to-treat population (95% confidence interval [CI], 15 to 63; P = 0.005) (Fig. 2). After adjustment for the difference in age between the two groups, the efficacy was 43% (95% CI, 14 to 62). The rate of pill use on 50% or more of days was recorded on the basis of pill counts, self-report, and dispensation records at 81% of visits on which efficacy was 50% (95% CI, 18 to 70; P = 0.006). This rate did not differ significantly (P = 0.48) from the efficacy at visits with less than 50% pill use of 32% (95% CI, −41 to 67%) (Fig. 3). Efficacy of less than 30% could not be ruled out in the modified intention-to-treat analysis (P = 0.15) or in the prespecified as-treated analysis at 50% pill use (P = 0.09). There was no evidence of a change in HIV efficacy with longer follow-up (P = 0.44).
Figure 2. Kaplan–Meier Estimates of Time to HIV Infection (Modified Intention-to-Treat Population).
The cumulative probability of HIV acquisition is shown for the two study groups. The efficacy of preexposure prophylaxis with emtricitabine and tenofovir disoproxil fumarate (FTC–TDF) was 44%, as compared with placebo (P = 0.005). The inset graph shows a more detailed version of the overall graph up to a probability of 0.10.
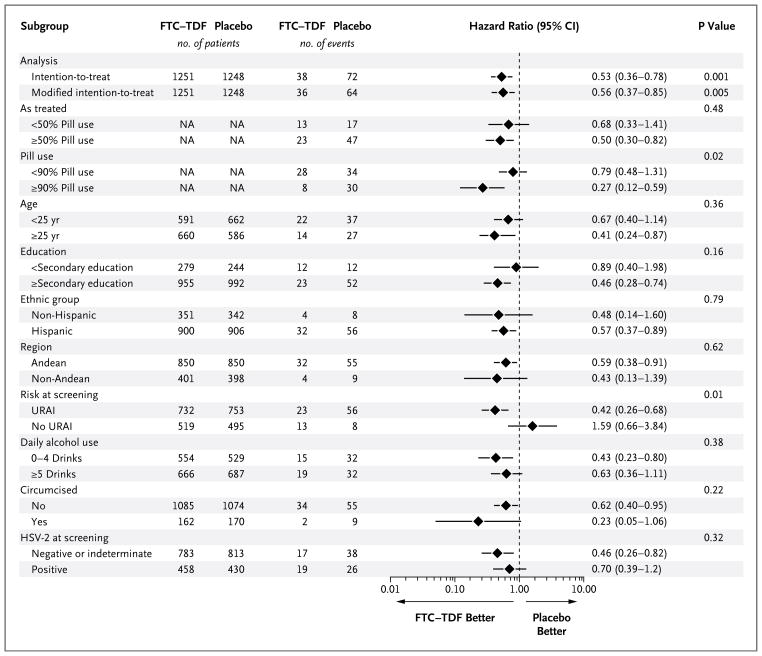
Figure 3. HIV Incidence among Subjects Receiving FTC–TDF, According to Subgroup.
The efficacy of emtricitabine and tenofovir disoproxil fumarate (FTC–TDF) is 1 minus the hazard ratio. Hazard ratios of less than 1 indicate efficacy, and 95% confidence intervals (shown by horizontal lines) that do not cross 1 indicate significant evidence of efficacy. All subgroup analyses were prespecified except for testing for herpes simplex virus type 2 (HSV-2) at screening and pill use at the rate of 90%. P values for the intention-to-treat analysis and the modified intention-to-treat analysis apply to the hypothesis of any evidence of efficacy; P values for other comparisons refer to the hypothesis that efficacy differed between the two strata. NA denotes not applicable, and URAI unprotected receptive anal intercourse.
In prespecified analyses of efficacy according to subgroup, efficacy was higher among subjects who reported at screening that they had previously had unprotected receptive anal intercourse than among those who did not (efficacy, 58%; 95% CI, 32 to 74) (Fig. 3). There was no significant between-group difference in protection on the basis of region, race or ethnic group, male circumcision, level of education, alcohol use, or age. In post hoc analyses, pill use on 90% or more of days was recorded at 49% of visits on which efficacy was 73% (95% CI, 41 to 88; P<0.001). Among all subjects, without exclusion for HIV infection at enrollment or the degree of compliance to the drug regimen, the efficacy was 47% (95% CI, 22 to 64; P = 0.001).
Among the 10 subjects in whom plasma HIV RNA was subsequently detected in specimens obtained at enrollment, 5 had symptoms of an acute viral syndrome at enrollment, 2 had symptoms 1 week later (prompting an interim study visit), 1 had an anal sore, and 2 had leukopenia at enrollment. In these subjects, the clinicians did not suspect acute HIV infection, because the symptoms were attributed to an upper respiratory tract infection, sinusitis, or other non-HIV cause.
Of the preexisting HIV infections at enrollment, two occurred in the FTC–TDF group and eight in the placebo group (P = 0.06). Among subjects who were infected after enrollment, the numbers with detectable plasma HIV RNA before seroconversion were 5 of 36 (14%) in the FTC–TDF group and 7 of 64 (11%) in the placebo group (P = 0.75). The time to seroconversion after RNA detection was similar in the two groups (P = 0.55). After the discontinuation of a study drug, seroconversion rates were similar among 320 subjects (161 in the FTC–TDF group and 159 in the placebo group) (P = 0.42). These subjects had a total of 1173 visits for HIV testing after the discontinuation of a study drug (642 in the FTC–TDF group and 531 in the placebo group). During these visits, 5 seroconversions were observed (2 in the FTC–TDF group and 3 in the placebo group).
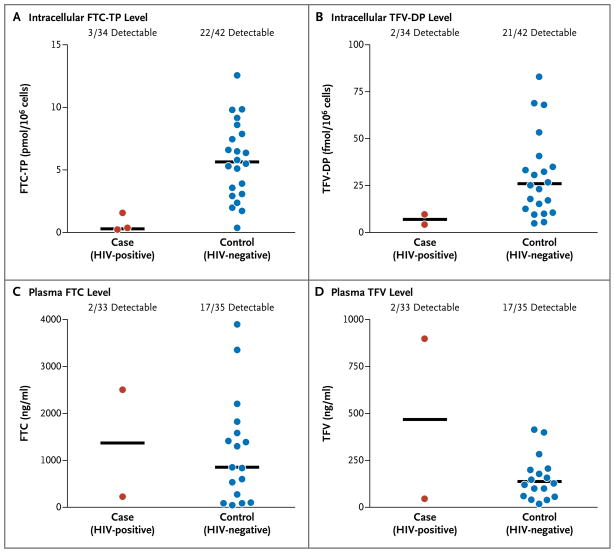
DRUG-LEVEL DETECTION AND PROPHYLACTIC EFFECT
Among subjects who became infected with HIV, the median time between the tested specimen date and the last uninfected visit was 35 days (interquartile range, 28 to 56). No drug was detected in any plasma or cell specimens from subjects in the placebo group. Among subjects in the FTC–TDF group, at least one of the study-drug components was detected in 3 of 34 subjects with HIV infection (9%) and in 22 of 43 seronegative control subjects (51%) (Fig. 4). Of the 3 HIV-infected subjects with a detectable level of a study drug, none had cell-associated drug levels higher than the median for the 22 seronegative control subjects in whom a study-drug component was detected. Only 8% of subjects with HIV infection and 54% of control subjects who were considered “on treatment” on more than 50% of days had a detectable level of a study drug in plasma or peripheral-blood mononuclear cells (Table S8 in the Supplementary Appendix). Detection of the different drug components was more than 95% concordant (Table S6 in the Supplementary Appendix).
Figure 4. Levels of Study-Drug Components in Blood of Subjects Receiving FTC–TDF, According to HIV Status.
Shown are intracellular levels (Panels A and B) and plasma levels (Panels C and D) of components of emtricitabine and tenofovir disoproxil fumarate (FTC–TDF), quantified in specimens obtained from subjects in the FTC–TDF group. FTC-TP denotes emtricitabine triphosphate, and TFV-DP tenofovir diphosphate. The horizontal lines in each panel indicate medians.
In the FTC–TDF group, among subjects with a detectable study-drug level, as compared with those without a detectable level, the odds of HIV infection were lower by a factor of 12.9 (95% CI, 1.7 to 99.3; P<0.001), corresponding to a relative reduction in HIV risk of 92% (95% CI, 40 to 99; P<0.001). After adjustment for reported unprotected receptive anal intercourse, the relative risk reduction was 95% (95% CI, 70 to 99; P<0.001).
EFFECT OF FTC–TDF ON HIV INFECTION
Plasma HIV RNA levels and CD4+ T-cell counts were similar among subjects with seroconversion in the two groups (Fig. S4 in the Supplementary Appendix). Among the 10 subjects who were infected at enrollment, 3 had FTC-resistant infections (2 of 2 in the FTC–TDF group and 1 of 8 in the placebo group) (Table S5 in the Supplementary Appendix). No TDF-resistant infections were observed. Among 36 subjects in the FTC–TDF group and 64 subjects in the placebo group who became infected with HIV during the trial, no FTC or TDF resistance was detected.
DISCUSSION
Once-daily oral FTC–TDF provided 44% additional protection from HIV among men or transgender women who have sex with men who also received a comprehensive package of prevention services. The protective effect of FTC–TDF was significant but not as high as originally hypothesized during the design of the study. Although reported pill use was high, drug exposure that was measured objectively was substantially lower. The intracellular assay that was used in this study is expected to detect TFV-DP for 14 days or more after the last dose of TDF is taken (see Methods in the Supplementary Appendix). Other evidence of low drug exposure included the lack of drug resistance observed among emergent infections and the absence of suppression of the HIV RNA level in plasma at the seroconversion visit. There was no evidence of delayed seroconversion among subjects who were infected in the FTC–TDF group. More information will be available after the entire cohort stops receiving the study drug.
The estimate of biologic activity of FTC–TDF persists after adjustment for high-risk sexual practice, suggesting that the correlation between drug detection and protection is primarily due to the drug and not to other characteristics of subjects that may link poor adherence with higher risk. The testing of a larger number of specimens, from more subjects at more times, is needed to better define the minimum protective drug concentration. Protective drug levels may differ according to the type of exposure (rectal vs. penile). Drug level may have a role in monitoring trials, programs, and individual users. Methods for inexpensively measuring long-term drug exposure, such as that afforded by analysis of hair,19 would be helpful once such a method is fully validated.
Side effects may have contributed to low pill use among some subjects. As with treatment of HIV infection and the use of FTC–TDF in post-exposure prophylaxis,20 the initiation of FTC–TDF preexposure prophylaxis was associated with self-limited start-up symptoms in a few subjects. The trial design involving a placebo may also have contributed to lower-than-expected pill use. All subjects were counseled that the study pill might be a placebo or an active drug having no proven benefit. Open-label research and program development could provide users with clearer information about expected benefits and risks, which might increase the use and efficacy of preexposure prophylaxis. Engagement with communities and additional behavioral research are needed to develop methods of counseling that better support such use.
The initiation of chemoprophylaxis either before or after exposure should be deferred in patients with signs or symptoms of a viral syndrome, which are often present during acute HIV infection.21,22 The initiation of postexposure prophylaxis in patients who are RNA-positive but antibody-negative has been linked with acquisition of resistance to FTC and lamivudine (3TC),5 as occurred in subjects in the FTC–TDF group who were already infected at enrollment in our trial. Ways to increase recognition of acute HIV infection would include routine measurement of body temperature and testing for HIV antibodies to evaluate viral syndromes, regardless of whether the presentation suggests HIV infection or another cause. Testing for HIV RNA at the time of the initiation of preexposure prophylaxis should be considered where available.
TDF treatment is known to cause decreases in renal function,23 and there were trends toward more creatinine elevations in the FTC–TDF group than in the placebo group. Most creatinine elevations were self-limited and were not confirmed on repeat testing of a new specimen, as might occur due to dehydration, creatine use, or exercise. The ability to detect safety outcomes, including drug resistance, may have been decreased by lower-than-expected drug exposure. In light of evidence of the efficacy of FTC–TDF, more information is needed about possible subclinical effects that may affect bone mineral density, low-level drug resistance, and proximal renal tubular function. Flares of hepatitis caused by HBV after stopping preexposure prophylaxis with TDF were not seen in West African women,12 but more information is needed. These issues are being investigated in existing trials of preexposure prophylaxis.
Reported high-risk behavior decreased substantially after enrollment and remained lower than at baseline during the trial. Safer behavior was also observed in a trial of preexposure prophylaxis with TDF in West African women12 and may reflect the services (e.g., counseling, testing, and dispensing of condoms) that are provided as part of such interventions. In addition, taking a pill a day may have served as a daily reminder of imminent risk and may have promoted planning for sex, which has been associated with lower HIV risk.24 Behavioral changes during future open-label use of preexposure prophylaxis may differ because of an increased expectation of benefits, although such “risk compensation” was not observed during an open-label study of postexposure prophylaxis, during which benefits were expected.25
The optimal regimen for preexposure prophylaxis has not been established, and data from the subjects in our study cannot be applied to other populations. Alternative regimens in different populations are being studied. (Details are available in the Discussion in the Supplementary Appendix and at www.avac.org.)
In our study, preexposure prophylaxis with oral FTC–TDF among men and transgender women who have sex with men addressed an important unmet need in public health. HIV prevalence is higher in this population than in other groups in almost all countries.14 In the United States, rates of HIV infection among such men and transgender women have climbed since the early 1990s, affecting in particular black and Hispanic subpopulations.26 Intensive counseling in behavioral risk reduction for such subjects has not been shown to be better than standard counseling.27 Although male circumcision partially protects heterosexual men,28–30 penile circumcision is not expected to protect those who are exposed on the rectal mucosa.31 Heterosexual women were partially protected by tenofovir 1% vaginal gel,13 but the safety and utility of tenofovir topical gels for rectal use is not yet known. In the FTC–TDF group, there was increased efficacy among subjects who reported having unprotected receptive anal intercourse, which is the main mode of HIV transmission among the subjects in our study and increases the risk of heterosexual women who engage in the practice.32 We showed that such subjects with a high risk of exposure to HIV can be mobilized to participate in prevention initiatives and that preexposure prophylaxis is effective for slowing the spread of HIV in this population.
Supplementary Material
Acknowledgments
Supported by the Division of Acquired Immunodeficiency Syndrome (DAIDS), National Institute of Allergy and Infectious Diseases, National Institutes of Health, as a cooperative agreement (UO1 AI64002, to Dr. Grant) and by the Bill and Melinda Gates Foundation. Study drugs were donated by Gilead Sciences. The pharmacological studies were sponsored by a cooperative agreement with DAIDS (UO1 AI84735, to Dr. Anderson). Support for some specimen handling came from a grant from DAIDS (RO1 AI062333, to Dr. Grant) and by the J. David Gladstone Institutes. Some infrastructure support at the University of California at San Francisco was provided by a grant from the National Institutes of Health (UL1 RR024131).
Dr. Grant reports receiving support as an advisor to Siemens (the manufacturer of TruGene HIV-1 Genotyping Kit); Dr. Mayer reports receiving grant support from Gilead, Merck, and Bristol-Myers Squibb; Dr. Kallás reports serving on a data and safety monitoring board for Merck; Dr. Schechter reports receiving consulting fees and grants from Gilead; Drs. Liu and Anderson report receiving donations of study drug from Gilead for various PrEP projects; and Drs. Jaffe and Rooney report being employees of Gilead Sciences and owning stock in the company. No other potential conflict of interest relevant to this article was reported.
We thank the study subjects for their dedication to finding new ways to protect communities and for their trust in us; the community advisory boards; the members of the DAIDS multinational independent data and safety monitoring board, Kathy Edwards (chair), Shrikant I. Bangdiwala, KyungMann Kim, W.D. Francois Venter, Alejandro Llanos-Cuentas, Olavo Henrique Munhoz Leite, V.I. Mathan, Carlos Seas, Panpit Suwangool, Wafaa El-Sadr, Gary Maartens, Gabriel Thimonthe, Michael Proschan, and Dennis Dixon; community advocates Mitchell Warren, Julie Davids, Susana Chavez, Jorge (Tito) Bracamonte, and Carlos Caceres; Caitlin Fernandez, Joseph Rower, and Brandon Klein for their analytical pharmacology assistance; Grace Chow and Stephen Becker for their guidance as project officers; John Carroll of the Gladstone Institutes for providing original versions of the figures; Miguel Bernal and Ximena Barra for their print and film work; Mark Aurigemma for developing communication materials; Malu Robles for her assistance in the preparation of the manuscript; and Mark Wainberg, Mike Youle, Sandra Lehrman, Jose Pilotto, Neptali Arias, Vivian Levy, Kimberly Page, and Renee Ridzon for inspiration and logistical work.
APPENDIX
The authors’ affiliations are as follows: the Gladstone Institute of Virology and Immunology (R.M.G., V.M., P.G., R.J.H., J.J.M., P.D., J.L.), the University of California, San Francisco (R.M.G., A.Y.L., S.P.B., K.M., F.W., D.V.G.), and the HIV Research Section, San Francisco Department of Public Health (A.Y.L., S.P.B.) — all in San Francisco; Investigaciones Medicas en Salud, Lima (J.R.L., L.V.), Asociación Civil Impacta Salud y Educación, Lima (J.R.L., J.V.G.-C., M.E.R.-C., C.G.), and Asociación Civil Selva Amazónica, Iquitos (M.C.) — all in Peru; the University of Colorado, Denver (P.L.A., L.R.B., J.-H.Z.).; Fundación Ecuatoriana Equidad, Guayaquil, Ecuador (O.M.-H., T.F.); Instituto de Pesquisa Clinica Evandro Chagas–Fundação Oswaldo Cruz (V.G.V.), and Projeto Praça Onze, Hospital Escola São Francisco de Assis, Universidade Federal do Rio de Janeiro (M.S.) — both in Rio de Janeiro; Brown University, Providence, RI (K.H.M.); the Fenway Institute, Fenway Health, Boston (K.H.M.); the Division of Clinical Immunology and Allergy, School of Medicine, University of São Paulo, and Instituto de Investigação em Imunologia — both in São Paulo (E.G.K.); Research Institute for Health Sciences, Chiang Mai University, Chiang Mai, Thailand (S.C.); Desmond Tutu HIV Centre and Department of Medicine, University of Cape Town, Cape Town, South Africa (L.-G.B.); Division of AIDS, National Institute of Allergy and Infectious Diseases, National Institutes of Health, Bethesda, MD (A.I.M., D.N.B.); Gilead Sciences, Foster City, CA (J.F.R., H.S.J.); DF/Net Research, Seattle (B.P.); Applied Health Research, Brighton, MI (K.R.A.); and the Center for Health, Intervention, and Prevention, University of Connecticut, Storrs (K.R.A.).
Footnotes
Disclosure forms provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Donnell D, Baeten JM, Kiarie J, et al. Heterosexual HIV-1 transmission after initiation of antiretroviral therapy: a prospective cohort analysis. Lancet. 2010;375:2092–8. doi: 10.1016/S0140-6736(10)60705-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Connor EM, Sperling RS, Gelber R, et al. Reduction of maternal-infant transmission of human immunodeficiency virus type 1 with zidovudine treatment. N Engl J Med. 1994;331:1173–80. doi: 10.1056/NEJM199411033311801. [DOI] [PubMed] [Google Scholar]
- 3.Smith DK, Grohskopf LA, Black RJ, et al. Antiretroviral postexposure prophylaxis after sexual, injection-drug use, or other nonoccupational exposure to HIV in the United States: recommendations from the U.S. Department of Health and Human Services. MMWR Recomm Rep. 2005;54(RR-2):1–20. [PubMed] [Google Scholar]
- 4.Schechter M, do Lago RF, Mendelsohn AB, Moreira RI, Moulton LH, Harrison LH. Behavioral impact, acceptability, and HIV incidence among homosexual men with access to postexposure chemoprophylaxis for HIV. J Acquir Immune Defic Syndr. 2004;35:519–25. doi: 10.1097/00126334-200404150-00010. [DOI] [PubMed] [Google Scholar]
- 5.Roland ME, Neilands TB, Krone MR, et al. Seroconversion following nonoccupational postexposure prophylaxis against HIV. Clin Infect Dis. 2005;41:1507–13. doi: 10.1086/497268. [DOI] [PubMed] [Google Scholar]
- 6.Grant RM, Buchbinder S, Cates W, Jr, et al. AIDS: promote HIV chemoprophylaxis research, don’t prevent it. Science. 2005;309:2170–1. doi: 10.1126/science.1116204. [DOI] [PubMed] [Google Scholar]
- 7.Denton PW, Estes JD, Sun Z, et al. Anti-retroviral pre-exposure prophylaxis prevents vaginal transmission of HIV-1 in humanized BLT mice. PLoS Med. 2008;5(1):e16. doi: 10.1371/journal.pmed.0050016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tsai C-C, Follis KE, Sabo A, et al. Prevention of SIV infection in macaques by (R)-9-(2-phosphonylmethoxypropyl)adenine. Science. 1995;270:1197–9. doi: 10.1126/science.270.5239.1197. [DOI] [PubMed] [Google Scholar]
- 9.Van Rompay KKA, McChesney MB, Aguirre NL, Schmidt KA, Bischofberger N, Marthas ML. Two low doses of tenofovir protect newborn macaques against oral simian immunodeficiency virus infection. J Infect Dis. 2001;184:429–38. doi: 10.1086/322781. [DOI] [PubMed] [Google Scholar]
- 10.García-Lerma JG, Otten RA, Qari SH, et al. Prevention of rectal SHIV transmission in macaques by daily or intermittent prophylaxis with emtricitabine and tenofovir. PLoS Med. 2008;5(2):e28. doi: 10.1371/journal.pmed.0050028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.García-Lerma JG, Cong ME, Mitchell J, et al. Intermittent prophylaxis with oral Truvada protects macaques from rectal SHIV infection. Sci Transl Med. 2010;2:14ra4. doi: 10.1126/scitranslmed.3000391. [DOI] [PubMed] [Google Scholar]
- 12.Peterson L, Taylor D, Roddy R, et al. Tenofovir disoproxil fumarate for prevention of HIV infection in women: a phase 2, double-blind, randomized, placebo-controlled trial. PLoS Clin Trials. 2007;2(5):e27. doi: 10.1371/journal.pctr.0020027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Abdool Karim Q, Abdool Karim SS, Frohlich JA, et al. Effectiveness and safety of tenofovir gel, an antiretroviral microbicide, for the prevention of HIV infection in women. Science. 2010;329:1168–74. doi: 10.1126/science.1193748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Griensven F, de Lind van Wijngaarden JW, Baral S, Grulich A. The global epidemic of HIV infection among men who have sex with men. Curr Opin HIV AIDS. 2009;4:300–7. doi: 10.1097/COH.0b013e32832c3bb3. [DOI] [PubMed] [Google Scholar]
- 15.Beyrer C, Baral SD, Walker D, Wirtz AL, Johns B, Sifakis F. The expanding epidemics of HIV type 1 among men who have sex with men in low- and middle-income countries: diversity and consistency. Epidemiol Rev. 2010;32:137–51. doi: 10.1093/epirev/mxq011. [DOI] [PubMed] [Google Scholar]
- 16.Liu AY, Kittredge PV, Vittinghoff E, et al. Limited knowledge and use of HIV post- and pre-exposure prophylaxis among gay and bisexual men. J Acquir Immune Defic Syndr. 2008;47:241–7. [PubMed] [Google Scholar]
- 17.Mimiaga MJ, Case P, Johnson CV, Safren SA, Mayer KH. Preexposure antiretroviral prophylaxis attitudes in high-risk Boston area men who report having sex with men: limited knowledge and experience but potential for increased utilization after education. J Acquir Immune Defic Syndr. 2009;50:77–83. doi: 10.1097/QAI.0b013e31818d5a27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Good participatory practice: guidelines for biomedical HIV prevention trials. Geneva: UNAIDS; 2007. [Google Scholar]
- 19.Liu A, Vittinghoff E, Gandhi M, et al. Validating measures of tenofovir drug exposure in a US pre-exposure prophylaxis trial. Program and abstracts of the 17th Conference on Retroviruses and Opportunistic Infections; San Francisco. February 27–March 2, 2010; abstract. [Google Scholar]
- 20.Mayer KH, Mimiaga MJ, Cohen D, et al. Tenofovir DF plus lamivudine or emtricitabine for nonoccupational post-exposure prophylaxis (NPEP) in a Boston community health center. J Acquir Immune Defic Syndr. 2008;47:494–9. doi: 10.1097/QAI.0b013e318162afcb. [DOI] [PubMed] [Google Scholar]
- 21.Schacker TW, Hughes JP, Shea T, Coombs RW, Corey L. Biological and virologic characteristics of primary HIV infection. Ann Intern Med. 1998;128:613–20. doi: 10.7326/0003-4819-128-8-199804150-00001. [DOI] [PubMed] [Google Scholar]
- 22.Hofer CB, Harrison LH, Struchiner CJ, et al. Acute retrovirus syndrome among prospectively identified homosexual men with incident HIV infection in Brazil. J Acquir Immune Defic Syndr. 2000;25:188–91. doi: 10.1097/00042560-200010010-00014. [DOI] [PubMed] [Google Scholar]
- 23.Gallant JE, Winston JA, DeJesus E, et al. The 3-year renal safety of a tenofovir disoproxil fumarate vs. a thymidine analogue-containing regimen in antiretroviral-naive patients. AIDS. 2008;22:2155–63. doi: 10.1097/QAD.0b013e3283112b8e. [DOI] [PubMed] [Google Scholar]
- 24.van Griensven F, Thienkrua W, Sukwicha W, et al. Sex frequency and sex planning among men who have sex with men in Bangkok, Thailand: implications for pre- and post-exposure prophylaxis against HIV infection. J Int AIDS Soc. 2010;13:13. doi: 10.1186/1758-2652-13-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martin JN, Roland ME, Neilands TB, et al. Use of postexposure prophylaxis against HIV infection following sexual exposure does not lead to increases in high-risk behavior. AIDS. 2004;18:787–92. doi: 10.1097/00002030-200403260-00010. [DOI] [PubMed] [Google Scholar]
- 26.Hall HI, Song R, Rhodes P, et al. Estimation of HIV incidence in the United States. JAMA. 2008;300:520–9. doi: 10.1001/jama.300.5.520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Koblin B, Chesney M, Coates T. Effects of a behavioural intervention to reduce acquisition of HIV infection among men who have sex with men: the EXPLORE randomised controlled study. Lancet. 2004;364:41–50. doi: 10.1016/S0140-6736(04)16588-4. [DOI] [PubMed] [Google Scholar]
- 28.Auvert B, Taljaard D, Lagarde E, Sobngwi-Tambekou J, Sitta R, Puren A. Randomized, controlled intervention trial of male circumcision for reduction of HIV infection risk: the ANRS 1265 Trial. PLoS Med. 2005;2(11):e298. doi: 10.1371/journal.pmed.0020298. [Erratum, PLoS Med 2006;3(5):e226.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Bailey RC, Moses S, Parker CB, et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet. 2007;369:643–56. doi: 10.1016/S0140-6736(07)60312-2. [DOI] [PubMed] [Google Scholar]
- 30.Gray RH, Kigozi G, Serwadda D, et al. Male circumcision for HIV prevention in men in Rakai, Uganda: a randomised trial. Lancet. 2007;369:657–66. doi: 10.1016/S0140-6736(07)60313-4. [DOI] [PubMed] [Google Scholar]
- 31.Templeton DJ, Millett GA, Grulich AE. Male circumcision to reduce the risk of HIV and sexually transmitted infections among men who have sex with men. Curr Opin Infect Dis. 2010;23:45–52. doi: 10.1097/QCO.0b013e328334e54d. [DOI] [PubMed] [Google Scholar]
- 32.Baggaley RF, White RG, Boily MC. HIV transmission risk through anal intercourse: systematic review, meta-analysis and implications for HIV prevention. Int J Epidemiol. 2010;39:1048–63. doi: 10.1093/ije/dyq057. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.