Abstract
Christakis and colleagues have shown that health behaviors cluster in social networks and suggest social norms may account for the clustering. This study examined: 1) whether obesity clusters among young adults and whether social norms do in fact account for the clustering, and 2) among OW/OB young adults, whether number of social contacts trying to lose weight is associated with weight loss intentions and whether social norms for weight loss account for this effect. Normal weight (NW) and OW/OB young adults (N=288; 66%Female; 75%Caucasian) completed measures assessing number of OW social contacts and social norms for obesity. OW/OB young adults also indicated number of OW social contacts currently trying to lose weight, social norms for weight loss, and weight loss intentions. Compared to NW, OW/OB young adults were more likely to have OW romantic partners and best friends and had more OW casual friends and family members (p's<.05), but social norms for obesity did not differ between groups, and social norms did not mediate the relationship between OW social contacts and participants' weight status. However, among OW/OB young adults, having more social contacts trying to lose weight was associated with greater intention to lose weight (r=.20, p=.02) and social norms for weight loss fully mediated this effect (p<.01). This study is the first to show that social contacts and normative beliefs influence weight status and intentions for weight control in young adults. Findings underscore the importance of targeting social influence in the treatment and prevention of obesity in this high-risk age group.
Keywords: Social networks, social norms, obesity, young adults
Introduction
Forty percent of young adults age 18 to 25 are overweight or obese (1). Moreover, young adults experience the greatest rate of weight gain, averaging 1 to 2 pounds per year (2,3). Despite the high rates of overweight and obesity in this population, young adults are largely underrepresented in traditional behavioral weight loss interventions and, when they participate, tend to lose less weight than older adults (4). In order to develop both appealing and effective treatment and prevention programs for this age group, it is important to understand the factors that influence weight and weight loss intentions in this population.
There has been an upsurge in studies examining the effects of social influence on health, with the majority demonstrating that social networks play an important role in the promotion of health behaviors (5, 6-9). In a sample of adults age 18 to 70, Christakis and colleagues (6) demonstrated that a person's chance of becoming obese increases 57% if a friend becomes obese, 40% if a sibling becomes obese, and 37% if a spouse becomes obese. Similarly, in a population of adolescents, smoking researchers found that having more social contacts who smoke is associated with greater incidence of smoking (7). Studies have also shown that social ties can promote positive health behavior change. Among adults, Christakis and Fowler (8) showed that a person's chance of quitting smoking increases if a spouse, sibling or friend stops smoking. Similarly, Rosenquist and colleagues (9) showed that individuals are 29% more likely to abstain from alcohol consumption if a close social contact stops consuming alcohol. Taken together, these findings indicate that social ties have a strong influence on health behavior; and recent studies have shown that younger individuals are even more affected by social contacts' health behaviors compared to older individuals (10-11).
While never tested, social norms, or beliefs about what is socially acceptable or expected (12), are thought to at least partially account for the clustering of health behaviors among social contacts (6, 8-9). Studies provide preliminary support for this hypothesis by demonstrating that social norms are powerful determinants of eating and activity behaviors, particularly among young adults. Laboratory paradigms with college-aged students have consistently shown that the induction of social norms for overeating (“previous participants have eaten a lot”) leads to overeating among participants (13-17). Similarly, cross-sectional research with young adults has demonstrated that social norms for healthy eating and physical activity are associated with the consumption of healthy foods, physical activity intentions, and actual physical activity behavior (18-20). Moreover, young adults' health behaviors have been shown to be influenced by social norms in other domains including alcohol use, smoking, and HIV risk behaviors (7, 11, 21). Thus, while never empirically evaluated, social norms are a plausible mechanism by which social contacts influence health behaviors, particularly in a young adult population.
Despite the fact that a large proportion of young adults are overweight or obese, and consistent findings showing that social influence is a powerful determinant of health behavior, especially for younger individuals (11), no one has ever examined whether social network factors influence weight status and weight control intentions in a young adult population. Thus, the purpose of this study was to (a) extend Christakis et al's findings to a young adult population and (b) determine how social influence affects weight control intentions in overweight/obese young adults. Given previous findings (6, 18-20), we hypothesized that overweight/obese young adults would have more overweight social contacts compared to normal weight young adults and that social norms for obesity would mediate the relationship between number of overweight social contacts and young adults' weight status. In addition, in the subsample of overweight/obese young adults, we hypothesized that intention to lose weight would be influenced by number of overweight social contacts trying to lose weight and that social norms for weight control would mediate this relationship.
Methods and Procedures
Procedure
In 2009 in the greater Providence area, 288 young adults (Normal Weight (NW) = 151; Overweight / Obese (OW/OB) = 137) aged 18 to 25 were recruited through a series of email blasts, print and internet ads, as well as flyers posted at locations frequented by young adults (e.g., college campuses, grocery stores, hair salons, and fitness centers). Ads targeted young adults who were willing to participate in an online survey about their eating and activity behaviors. In order to reduce known barriers to participation in this age group (e.g., time, transportation), participants completed questionnaires online via a secure website on their own computers. The questionnaires assessed several areas considered relevant to weight control in this population, including social influence. Participants received $10 for their participation and were enrolled in a raffle to win an iPod. Procedures were approved by a local Institutional Review Board.
Questionnaires
Presentation of questionnaires was counterbalanced to control for fatigue and order effects.
All participants completed the following
Weight and height
Participants reported their weight in pounds and height in feet and inches. Body Mass Index (BMI) was calculated by converting pounds to kilograms, inches to meters, and performing the following computation: weight in kg/height in meters2. Based on the BMI calculation, participants were categorized as normal weight (BMI < 25kg/m2) or overweight/obese (BMI ≥ 25kg/m2).
Overweight social contacts
Participants' perception of number of overweight social contacts was assessed. They were asked to indicate whether their romantic partner was overweight (“yes” = 1; “no” = 0) and whether their best friend was overweight (“yes” = 1; “no” = 0). If participants did not have a romantic partner or best friend, they checked a box indicating that these relationships were not applicable (e.g., “I do not have a romantic partner”). Participants also reported number of overweight casual friends, relatives, and colleagues/classmates on a 5-point scale ranging from “None” (0) to “All” (4).1 For correlation analyses, these five items were summed to create a composite measure of number of overweight social contacts.
Social norms for obesity and obesity-related behaviors
Participants indicated how socially acceptable they thought it was to be overweight, eat unhealthy foods, and be inactive. Response options ranged from “very unacceptable” = 0 to “very acceptable” = 4. For correlation analyses, items were summed to create a composite measure of obesogenic social norms. In this sample, this measure demonstrated good internal consistency (α=.69), and individual item loadings were good to excellent (0.59 for ‘overweight’, 0.86 for ‘eat unhealthy foods’, and 0.88 for ‘inactive’) (22).
Only OW/OB participants completed the following
Number of social contacts trying to lose weight
Participants reported number of overweight social contacts currently trying to lose weight on a 5-point scale from 0 (“Nobody”) to 4 (“All”).2
Social norms for weight loss
A questionnaire that measured smoking cessation norms (23) was adapted to measure social norms for weight loss. Participants reported (1) how frequently social contacts encouraged them to lose weight (“Never” = 0; “Often” = 4); (2) how frequently social contacts offered weight loss information or tools to help with weight loss (“Never” = 0; “Often” = 4); and (3) the extent to which people closest to them would approve or disapprove if they were to lose weight within the next 3-months (“Strongly disapprove” = 0; “Strongly approve” = 4). Items were averaged. Higher scores indicated greater weight loss norms. Reliability, for the 3-item measure was good (α = .70), and item loadings were good to excellent (.88 for ‘encouraged to lose weight’, .81 for ‘offered weight loss information’, and .69 for ‘approve/disapprove of losing weight’).
Intention to lose weight within the next 3-months
Participants were asked to report on a 5-point scale how likely they were to try to lose weight within the next 3-months; options ranged from “very unlikely” (0) to “very likely” (4). While using a single item to assess a construct is not ideal, such an approach is common when assessing behavioral intentions (24).
Statistical Analyses
Differences in demographic characteristics between NW and OW/OB were examined using Analyses of Variance (ANOVA) or chi-square tests for continuous or categorical variables, respectively. Significant demographic differences were controlled for when comparing the two groups. Group comparisons were conducted using ANOVAs.
To determine whether social norms for obesity mediated the relationship between number of overweight social contacts and participants' BMI, we first confirmed that there was a significant relationship between overweight social contacts and participants' BMI and number of overweight social contacts and social norms for obesity. Similarly, to determine whether social norms for weight control mediated the relationship between number of social contacts trying to lose weight and weight loss intentions within the subgroup of OW/OB young adults, we first examined whether there were significant correlations between number of social contacts trying to lose weight and intention to lose weight and number of social contacts trying to lose weight and social norms for weight control. These analyses were conducted using PASW Statistics 18, Release 18.0.0 (©SPSS, Inc., 2009, Chicago, IL, www.spss.com). Per Baron and Kenny (1986), if the correlations were significant, full model-based mediation analyses were conducted via path analysis using the structural equation modeling software package Mplus, Version 3.11 (25). Evidence for mediation was present if the previously significant relationship was reduced or eliminated when the proposed mediator was added to the model (26).
Results
Participant characteristics
The sample was predominantly female and Caucasian. Race/ethnicity was the only demographic characteristic that differed between overweight/obese (OW/OB) and normal weight (NW) participants; African Americans were more likely to be overweight and Asians were more likely to be normal weight (p's < .01). See Table 1.
Table 1.
Participant demographic and anthropometric characteristics.
| Total Sample (N = 288) |
OW / OB (n = 137) |
NW (n = 151) |
OW / OB vs. NW |
||
|---|---|---|---|---|---|
|
χ2 or F value |
p-value | ||||
| Female, No. (%) | 190 (66.0) | 89 (65.0) | 101 (66.9) | 0.12 | 0.73 |
| Age, years (SD) | 21.9 (2.2) | 21.8 (2.2) | 21.9 (2.1) | 0.36 | 0.55 |
| Race, No. (%) | 15.9 | 0.007 | |||
| Caucasian | 220 (76.4) | 106 (77.4) | 114 (75.5) | 0.1 | 0.71 |
| Black/African American | 6 (2.1) | 6 (4.4) | 0 (0.0) | 6.8 | 0.009 |
| Asian | 24 (8.3) | 5 (3.6) | 19 (12.6) | 7.5 | 0.006 |
| Multi-Racial | 21 (7.3) | 10 (7.3) | 11 (7.3) | 0.0 | 1.00 |
| Other | 16 (5.6) | 10 (7.3) | 6 (4.0) | 1.5 | 0.22 |
| No Response | 1 (0.3) | 0 (0.0) | 1 (0.7) | 0.9 | 0.34 |
| Latino/Hispanic, No. (%) | 16 (5.6) | 9 (6.6) | 7 (4.6) | 0.5 | 0.47 |
| Marital Status, No. (%) | 3.5 | 0.32 | |||
| Single | 240 (83.3) | 112 (81.8) | 128 (84.8) | ||
| Married | 15 (5.2) | 7 (5.1) | 8 (5.3) | ||
| Living with partner | 28 (9.7) | 17 (12.4) | 11 (7.3) | ||
| Declined to answer | 5 (1.7) | 1 (0.7) | 4 (2.6) | ||
| Education, No. (%) | 6.4 | 0.10 | |||
| High School | 34 (11.8) | 17 (12.4) | 17 (11.3) | ||
| Some college | 110 (38.2) | 61 (44.5) | 49 (32.5) | ||
| College | 118 (41.0) | 46 (33.6) | 72 (47.7) | ||
| Graduate / professional Degree | 26 (9.0) | 13 (9.5) | 13 (8.6) | ||
| Weight, kg (SD) | 74.4 (16.8) | 86.3 (15.3) | 63.7 (9.0) | 228.0 | <.001* |
| BMI, kg/m2 (SD) | 25.9 (5.3) | 30.1 (4.7) | 22.1 (1.6) | 360.4 | <.001* |
Robust test statistic used to adjust for homogeneity of variance violation.
The effects of social influence on weight status in young adults
Compared to NW, OW/OB young adults reported more overweight social contacts (F (1, 284) = 25.5, p < 0.001, part. η2 = 0.08). OW/OB were more likely to have overweight romantic partners (25% v. 14%) and overweight best friends (24% v. 14%). OW/OB participants also had more overweight casual friends and more overweight relatives (p's ≤ 0.01). However, OW/OB and NW young adults did not differ in number of overweight colleagues and classmates (p = .08). See Table 2.
Interestingly, social norms for obesity did not differ between OW/OB and NW young adults (F (1, 284) = 0.28, p = .60). The two group were similar in their perceptions of how socially acceptable it is to be overweight, eat unhealthy foods, and be inactive. See Table 2.
Mediation analyses testing whether social norms for obesity mediate the relationship between number of overweight social contacts and BMI
Correlation analyses, using composite scores for number of overweight social contacts and social norms for obesity, revealed similar patterns to those reported above. Having more overweight social contacts was associated with higher BMI (r = .33, p < .001), but BMI was not associated with obesogenic social norms (r = .08, p = .19). Moreover, the relationship between number of overweight contacts and social norms for obesity was non-significant (r = 0.01, p = 0.83). Given these latter findings, mediation analyses were not conducted (26).
The effects of social influence on weight loss intentions in OW/OB young adults
OW/OB young adults reported experiencing social influence for weight loss (social contacts = 1.7 ± 1.1; social norms = 1.9 ± 0.8) and high levels of intention to lose weight (3.4 ± 1.0 out of 4). Moreover, social influence factors were associated with weight loss intentions. Having more social contacts trying to lose weight and having greater social norms for weight loss were both correlated with greater intention to lose weight (r = .20, p = 0.02; r = .35, p < 0.001). In addition, there was a significant relationship between having more social contacts trying to lose weight and social norms for weight loss (r = .26, p = 0.002).
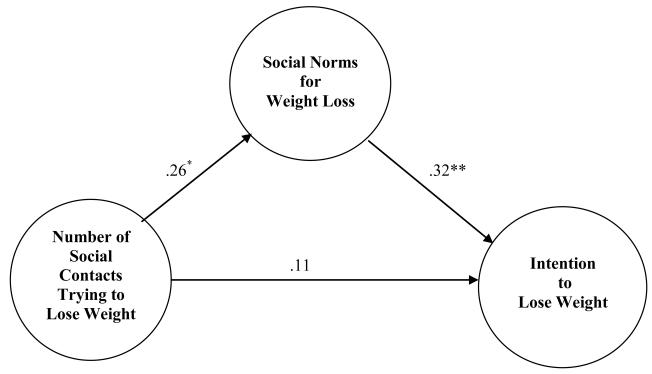
Given this initial set of significant relationships, we examined whether social norms for weight loss mediated the relationship between number of social contacts trying to lose weight and weight loss intentions. When weight loss norms was added into the model, the previously significant relationship between social contacts trying to lose weight and weight loss intentions was no longer significant (β = .11, p =.17). However, weight loss norms remained a significant predictor of weight loss intentions (β = .32, p <.001). These findings are consistent with a model in which social norms for weight loss fully mediate the association between having more social contacts trying to lose weight and weight loss intentions among young adults. See Figure 1.
Figure 1.
Social norms for weight loss mediate the relationship between number of social contacts trying to lose weight and the intention to lose weight. (*p<.01. **p<.001.)
Discussion
This study provides preliminary support that social network factors influence weight status and intention to lose weight among young adults. Our data suggest that obesity “clusters” in this population; overweight / obese (OW/OB) young adults report more overweight social contacts than normal weight (NW) young adults. However, contrary to our hypothesis, social norms for obesity do not account for the clustering (i.e. social norms did not mediate the relationship between social contacts' weight status and participants' weight status). We also examined whether social influence for weight control affects weight loss intentions among OW/OB young adults; interestingly, we found that having more social contacts trying to lose weight is associated with greater intention to lose weight and that weight control social norms fully mediate this effect.
Our finding suggesting that obesity clusters in young adults is consistent with previous studies demonstrating that adults age 18 to 70 who are overweight are more likely to have overweight social contacts (6). Christakis and Fowler (2007) found that overweight / obese adults have more overweight friends, relatives, and partners but that neighbors' weight status is not associated with participants' weight status. Similarly, our study showed that overweight young adults, age 18 to 25, report more overweight friends, relatives, and romantic partners but reported weight status of coworkers or classmates is not associated with participants' weight. Taken together, these findings indicate that for both adults and young adults “psychologically close” social ties (e.g., partners, friends, family) have a greater influence on obesity status than geographically close social ties (e.g., coworkers, neighbors).
Researchers have speculated that social norms may explain the interconnectedness of health behaviors between individuals and their friends and family (6, 8-9). This is the first study to test whether social norms for obesity do in fact account for the relationship between participants' weight status and the weight status of their social ties. Our findings suggest that normative beliefs, measured by social acceptability of overweight and associated behaviors, did not mediate the relationship between participants' weight and the reported weight status of their social contacts. In fact, normal weight and overweight / obese individuals reported similarly low levels of social acceptability of overweight and associated behaviors. Given the stigma associated with overweight and obesity (27), perceived societal acceptability of overweight may be low, even for overweight individuals. Thus, social norms for obesity may not explain the shared weight status among social ties. Instead, other social phenomena may be accounting for the effects of social contacts on weight. Laboratory and quasi-experimental studies have shown that social modeling strongly affects eating and activity behaviors. For example, participants randomly assigned to eat with confederates who ate either very large or very small amounts of food, have been shown to consistently copy the eating behavior of the confederate; confederates who overate induced overeating in participants, and confederates who ate very little induced restrained eating in participants, even hungry participants (28-31). Similarly, confederates who model stair use have been shown to prompt stair use in participants (32). Taken together, our results suggest that societal level social norms may not be the primary mechanism that accounts for the transmission of health behavior among social ties. Instead, other social influence factors, such a social modeling, may explain the similarity of health behaviors among social contacts. In order to inform treatment and prevention efforts, future research should continue to elucidate social influence factors that account for the clustering of health behavior within social networks.
Interestingly, this study also provides evidence that OW/OB young adults who perceive their overweight social contacts as trying to lose weight have greater weight loss intentions and that social norms for weight control fully mediate this effect. Previous interventions for young adults in the areas of substance abuse, safe sex, and healthy eating have shown that addressing social norms for health risk behaviors is associated with positive treatment outcomes (33-36). Moreover, changes in perceived norms have been shown to mediate intervention effects (35, 36). Thus, weight loss interventions that target young adults may be more successful at recruiting and retaining participants if they not only encourage individuals to join with friends and/or family but, even more importantly, aim to increase social norms for weight control among young adult participants and their close social ties.
It is important to note that the results of this study showed contrasting findings with regards to social norms. In the entire sample, social norms did not mediate the relationship between number of overweight social contacts and participants' weight status. However, in the OW/OB subsample, social norms did mediate the relationship between number of contacts trying to lose weight and weight loss intentions. These discrepant findings may be explained by the fact that two different types of norms were assessed. When examining social norms for obesity, we assessed whether injunctive norms, or beliefs about what is generally acceptable in society, mediate the effects of social contacts on BMI; however, when we assessed social norms for weight control, we tested whether subjective norms, or beliefs about what is socially acceptable among social contacts (e.g., friends, family), mediate the relationship between number of social contacts trying to lose weight and participants' weight loss intentions. Given that the subjective norms successfully mediated the effects of social contacts on weight loss intentions, social norms specific to the individual's social network may influence weight moreso than broad societal level norms. Future research should consider both injunctive and subjective norms and also motivation to comply with such norms when investigating the effects of social contacts on weight and associated behaviors.
Limitations of this study include self-reported weight data, a predominantly Caucasian sample, and a cross-sectional design (limiting our ability to draw definitive conclusions regarding mediation). Despite these limitations, this study has several important strengths. First, it included a large proportion of males, a demographic that is typically underrepresented in weight control research. Moreover, while social contacts and social norms have been shown to influence young adults' health behaviors in other domains (e.g., alcohol use, smoking, HIV risk behaviors, etc.), this is the first study to show that number of social contacts and normative beliefs influence weight status and intentions for weight control in young adults. Findings from this study underscore the importance of targeting social network factors in obesity interventions; such an approach may address an important aspect of health behavior change among young adults, namely social influence, which may lead to more effective obesity treatment and prevention programs for this high-risk population.
Supplementary Material
Acknowledgements
Preparation of this paper was supported in part by grants F32-DK082128 (TML, PI) and K23DK083440 (JGL, PI) from the National Institute of Diabetes and Digestive and Kidney Diseases. We would like to thank Richard Daniello, Erica Robichaud, and Brittany James for their work on this project.
Footnotes
Disclosure.
The authors declare no conflict of interest.
Even though a likert scale was used to assess overweight casual friends, relatives, and colleagues / classmates, for ease of description and interpretation, “number” of overweight social contacts will be used.
Even though a likert scale was used to assess overweight contacts trying to lose weight, for ease of description and interpretation, we will refer to this as “number” of social contacts trying to lose weight.
References
- 1.McCracken M, Jiles R, Blanck HM. Health Behaviors of the young adult U.S. population: Behavioral Risk Factor Surveillance System, 2003. Prev Chronic Dis. 2007;4(2):A25. [PMC free article] [PubMed] [Google Scholar]
- 2.Truesdale KP, Stevens J, Lewis CE, Schreiner PH, Loria CM, Cai J. Changes in risk factors for carciovascular disease by baseline weight status in young adults who maintain or gain weight over 15 years: The CARDIA study. Int J Obes (London) 2006;30(9):1397–1407. doi: 10.1038/sj.ijo.0803307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lewis CE, Jacobs DR, McCreath H, Kiefe CI, Schreiner PJ, Smith DE, Williams OD. Weight gain continues in the 1990s: 10-year trends in weight and overweight from the CARDIA study. Coronary Artery Risk Development in Young Adults. Am J Epidemiol. 2000;151(12):1172–1181. doi: 10.1093/oxfordjournals.aje.a010167. [DOI] [PubMed] [Google Scholar]
- 4.Gokee-LaRose J, Gorin AA, Raynor HA, et al. Are standard behavioral weight loss programs effective for young adults? Int J Obes (London) 2009;33(12):1374–1380. doi: 10.1038/ijo.2009.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Fowler JH, Christakis NA. Estimating peer effects on health in social networks: A response to Cohen-Cole and Fletcher; Trogdon, Nonnemaker, Pais. J Health Econ. 2008;27:1400–1405. doi: 10.1016/j.jhealeco.2008.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Christakis NA, Fowler JH. The spread of obesity in a large social network over 32 years. N Engl J Med. 2007;357(4):370–379. doi: 10.1056/NEJMsa066082. [DOI] [PubMed] [Google Scholar]
- 7.Piko BF, Luszczynska A, Gibbons FX, Teközel M. A culture-based study of personal and social influences of adolescent smoking. Eur J Public Health. 2005;15(4):393–398. doi: 10.1093/eurpub/cki008. [DOI] [PubMed] [Google Scholar]
- 8.Christakis NA, Fowler JH. The collective dynamics of smoking in a large social network. N Engl J Med. 2008;358(21):2249–2258. doi: 10.1056/NEJMsa0706154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rosenquist JN, Murabito J, Fowler JH, Christakis NA. The spread of alcohol consumption behavior in a large social network. Ann Intern Med. 2010;152(7):426–433. doi: 10.1059/0003-4819-152-7-201004060-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kerr M, Stattin H, Bisecker G, Ferrer-Wreder L. Parents and peers as developmental context. In: Lerner RM, Easterbrooks MA, Mistry J, Weiner IB, editors. Comprehensive handbook of psychology: developmental psychology. John Wiley; New York: 2002. [Google Scholar]
- 11.Albarracin D, Kumkale GT, Johnson BT. Influences of social power and normative support on condom use decisions: a research synthesis. AIDS Care. 2004;16(6):700–723. doi: 10.1080/09540120412331269558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cialdini RB, Trost MR. Social influence: Social norms, conformity, and compliance. In: Gilbert DT, Fiske ST, Kindzey G, editors. The Handbook of Social Psychology: Volume II. McGraw-Hill; New York: 1998. [Google Scholar]
- 13.Leone T, Pliner P, Peter Herman C. Influence of clear versus ambiguous normative information on food intake. Appetite. 2007;49(1):58–65. doi: 10.1016/j.appet.2006.11.005. [DOI] [PubMed] [Google Scholar]
- 14.Herman CP, Polivy J. Normative influences on food intake. Physiol Behav. 2005;86(5):762–772. doi: 10.1016/j.physbeh.2005.08.064. [DOI] [PubMed] [Google Scholar]
- 15.Pliner P, Mann N. Influence of social norms and palatability on amount consumed and food choice. Appetite. 2004;42(2):227–237. doi: 10.1016/j.appet.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 16.Roth DA, Herman CP, Polivy J, Pliner P. Self-presentational conflict in social eating situations: a normative perspective. Appetite. 2001;36(2):165–171. doi: 10.1006/appe.2000.0388. [DOI] [PubMed] [Google Scholar]
- 17.Herman CP, Roth DA, Polivy J. Effects of the presence of others on food intake: a normative interpretation. Psychol Bull. 2003;129(6):873–886. doi: 10.1037/0033-2909.129.6.873. [DOI] [PubMed] [Google Scholar]
- 18.Øygard L, Klepp KI. Influence of social groups on eating patterns: A study among young adults. J Behav Med. 1996;19(1):1–15. doi: 10.1007/BF01858171. [DOI] [PubMed] [Google Scholar]
- 19.Gabriele JM, Walker MS, Gill DL, Harber KD, Fisher EB. Differentiated roles of social encouragement and social constraint on physical activity behavior. Ann Behav Med. 2005;29(3):210–215. doi: 10.1207/s15324796abm2903_7. [DOI] [PubMed] [Google Scholar]
- 20.Everson ES, Daley AJ, Ussher M. Brief report: The theory of planned behaviour applied to physical activity in young people who smoke. J Adolesc. 2007;30(2):347–351. doi: 10.1016/j.adolescence.2006.11.001. [DOI] [PubMed] [Google Scholar]
- 21.Oostveen T, Knibbe R, De Vries H. Social influences on young adults' alcohol consumption: Norms, modeling, pressure, socializing, and conformity. Addict Behav. 1996;21(2):187–197. doi: 10.1016/0306-4603(95)00052-6. [DOI] [PubMed] [Google Scholar]
- 22.Comrey AL, Lee HB. A first course in factor analysis. 2nd ed. Erlbaum; Hillsdale, NJ: 1992. [Google Scholar]
- 23.van den Putte B, Yzer MC, Brunsting S. Social influences on smoking cessation: a comparison of the effect of six social influence variables. Prev Med. 2005;41(1):186–193. doi: 10.1016/j.ypmed.2004.09.040. [DOI] [PubMed] [Google Scholar]
- 24.Sutton S. Predicting and explaining intentions and behavior: How well are we doing? Journal of Applied Social Psych. 1998 [Google Scholar]
- 25.Muthén LK, Muthén BO. Mplus User's Guide. 3rd ed. Muthén & Muthén; Los Angeles, CA: 2004. [Google Scholar]
- 26.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 27.Brownell KD, Puhl RM, Schwartz MB, Rudd L. Weight bias: Nature, consequences, remedies. Guilford Publications; New York: 2005. [Google Scholar]
- 28.Goldman SJ, Goldman C, Herman P, Polivy J. Is the effect of a social model on eating attenuated by hunger? Appetite. 1991;17(2):129–140. doi: 10.1016/0195-6663(91)90068-4. [DOI] [PubMed] [Google Scholar]
- 29.Rosenthal B, McSweeney FK. Modeling influences on eating behavior. Addict Behav. 1979;4(3):205–214. doi: 10.1016/0306-4603(79)90029-7. [DOI] [PubMed] [Google Scholar]
- 30.Polivy J, Herman CP, Younger JC, Erskine B. Effects of a model on eating behavior: the introduction of a restrained eating style. J Pers. 1979;47(1):100–117. doi: 10.1111/j.1467-6494.1979.tb00617.x. [DOI] [PubMed] [Google Scholar]
- 31.Conger JC, Conger AJ, Costanzo PR, Wright KL, Matter JA. The effect of social cues on the eating behavior of obese and normal subjects. J Pers. 1980;48(2):258–271. doi: 10.1111/j.1467-6494.1980.tb00832.x. [DOI] [PubMed] [Google Scholar]
- 32.Adams MA, Hovell MF, Irvin V, Sallis JF, Coleman KJ, Liles S. Promoting stair use by modeling: an experimental manipulation of the Behavior Ecological Model. Am J Health Promot. 2006;21(2):101–109. doi: 10.4278/0890-1171-21.2.101. [DOI] [PubMed] [Google Scholar]
- 33.Moreira MT, Smith LA, Foxcroft D. Social norms interventions to reduce alcohol misuse in university or college students. Cochrane Database Syst Rev. 2009 Jul 8;(3):CD006748. doi: 10.1002/14651858.CD006748.pub2. [DOI] [PubMed] [Google Scholar]
- 34.Chernoff RA, Davison GC. An evaluation of a brief HIV/AIDS prevention intervention for college students using normative feedback and goal setting. AIDS Educ Prev. 2005;17(2):91–104. doi: 10.1521/aeap.17.3.91.62902. [DOI] [PubMed] [Google Scholar]
- 35.Ranby KW, Aiken LS, MacKinnon DP, et al. A mediation analysis of the ATHENA intervention for female athletes: Prevention of athletic-enhancing substance use and unhealthy weight loss behaviors. J Pediatr Psychol. 2009;34(10):1069–1083. doi: 10.1093/jpepsy/jsp025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Williams J, Herman-Stahl M, Calvin SL, Pemberton M, Bradshaw M. Mediating mechanisms of a military web-based alcohol intervention. Drug Alcohol Depend. 2009;100:248–257. doi: 10.1016/j.drugalcdep.2008.10.007. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.