Abstract
Myocarditis poses a severe health problem, can lead to dilated cardiomyopathy (DCM) and death, and is thought to be triggered by infections. Enteroviruses such as Coxsackie virus B 3 (CVB3) have been implicated as a culprit, since they can cause acute and chronic heart disease in susceptible mice. CVB was detected in human cardiac myocytes in some cases, whereas acute CVB infection was thought to have caused death. Here we studied, whether nasal administration of cardiac myosin (CM) major histocompatibility class (MHC) II peptides CM947-960 and CM735-747 and OX40 blockade would be able to ameliorate immunopathology and heart disease in BALB/C mice infected with CVB3. We found that nasal CM peptide prophylactic treatment significantly reduced myocarditis and mortality by enhancing Treg and IL-10 induction and that blockade of OX40 signaling could reduce heart inflammation when administered late during pathogenesis. Altogether, these results chart the way for novel prevention and intervention strategies for viral myocarditis.
Keywords: autoimmune myocarditis, IL-10, Treg, cardiac myosin, peptide therapy, Coxsackie virus B3, OX40
1. Introduction
Myocarditis is an inflammatory disease of the heart, which may be the precursor of heart failure due to dilated cardiomyopathy (DCM) (1–4). In this study, we selected two coxsackievirus group B type 3 (CVB3) virally-induced myocarditis (VIM) mouse models, in which disease occurs after infection with CVB3. In the first model, acute VIM with significant damage to cardiomyocytes and sudden death within the first 10 days after infection is induced (5–7). In the second model, following infection with heart-passaged CVB3 (hpCVB3), the initial, non-lethal signs of acute myocarditis become chronic and autoimmune in nature. In both cases, the myocardium becomes infiltrated by macrophages, B cells, and other lymphocytes, and heart damage with fibrosis is often observed (8; 9). The chronic inflammatory disease in the second model is believed to be due to an autoimmune response driven by effector T cells responding to cardiac antigens (10–12). Interestingly, among the most common pathogens related to myocarditis development in humansare enteroviruses and CVB3 in particular (5). Most mouse strains including the C57BL/6 strain are resistant to acute myocarditis and moreover do not progress in developing the chronic features of the disease, while a certain proportion of BALB/C males but not females are susceptible. However, resistance in C57BL/6 mice can be overcome by treatment with LPS (13). Here we studied the effect of nasal treatment simultaneously with cardiac myosin (CM) derived major histocompatibility class (MHC) II epitopes CM947-960 and CM735-747 (CM combo) (14) in male BALB/C mice in acute and chronic CVB3-induced myocarditis.
The rationale for this study was that CM-specific regulatory T cells (Tregs) would be induced after nasal treatment with CM epitopes, a scenario that has been proven to be beneficial in other autoimmune settings (15–17) and in experimental autoimmune myocarditis (EAM) in particular (18; 19). Similar to other autoantigen-induced autoimmune pathologies, EAM results in susceptible mice after subcutaneous injection of CM in complete Freund’s adjuvant (CFA) and pertussis toxin. In both EAM and VIM models, there is evidence that Tregs are involved in disease penetrance and/or precipitation. For example, induction of acute VIM in females during the estrus phase of the ovarian cycle seems to invigorate the function of Tregs, protecting from heart disease and sudden death (20). The role of Th1 and Th2 effector cells in the pathogenesis of both EAM and VIM is still unclear, although tumor necrosis factor (TNF) (21; 22) and more recently IL-6 have been implicated as important mediators of the disease (23). Here, we report that intranasal CM combination peptide treatment protected male BALB/C mice from acute myocarditis, sudden death, and progression to the chronic stage of the disease, through induction of IL-10 and Tregs, and some downregulation of IFNγ production.
In a second, complimentary approach, the pathogenic effector T cell population was targeted. Of potential significance to myocarditis, OX40 (CD134), a costimulatory receptor of the TNFR superfamily, has been detected on pathogenic effector T cells, coinciding with increased levels of OX40-ligand (OX40L) expressed on diseased cardiomyocytes (24–26). Therefore we reasoned to test the efficiency of targeting this interaction to protect from progression to the chronic stage of the disease. Interestingly, a beneficial effect of targeting OX40-OX40L signaling through anti-OX40L blockade administration was revealed in halting disease progression.
2. Materials and Methods
2.1 Mice
Male BALB/C mice 6–8 weeks of age were obtained from the Jackson Laboratories (Bar Harbor, ME). The animal work described was carried out in accordance with the IACUC of the La Jolla Institute for Allergy and Immunology.
2.2 Acute and chronic virally-induced myocarditis models
Acute myocarditis model
10^3 plaque forming units (PFU) CVB3 (Nancy strain), a sublethal dose, was used for the induction of acute heart inflammation followed by sudden death and was prepared as previously described (27).
Chronic myocarditis model
For inducing chronic disease, 10^3 PFU heart-passaged viral stocks of CVB3 (hpCB3) were prepared and used according to (5).
In all cases, viral stocks were stored at −80 °C in Dulbecco’s Modified Eagle Medium (DMEM). BALB/C mice were infected intraperitoneally (i.p.).
2.3 Peptide treatments
Nasal administration-acute myocarditis model
Mice were treated for 3 consecutive days prior to infection with CVB3 (days −3, −2, −1) with the CM-derived peptides CM947-960 and CM735-747 (CM combo) after diluting in sterile 1× DPBS and mixing. 40μg of each peptide was given in the mouse nostril while anesthetized with isoflurane. Peptides were purchased from Abgent with more than 90% purity (San Diego, CA)
Nasal administration-chronic myocarditis model
Mice were treated with the aforementioned CM peptide mix for 3 consecutive days: a) prior to infection with hpCVB3 (days −3, −2, −1), b) during the acute phase of the immune response (days 7, 8, 9), 3), and/or c) during the transition to the chronic phase of the immune response (days 20, 21, 22).
2.4 Flow cytometry
Flow cytometry antibodies were purchased from BD-Pharmingen, e-Bioscience and Biolegend (all San Diego, CA). Single-cell suspensions, after a 2.4G2 blocking step, were stained with the following directly conjugated antibodies: CD4-Pacific Blue or PECy7, CD69-FITC, CD62L-APC, CD45.2-PerCPCy5.5, CD8-APCCy7 or FITC, CD44-Pacific Blue, CTLA-4-PE, CD25-APCCy7, CD127-PeCy7 and OX40-PE (isotype controls for all antibodies were included). For intracellular Foxp3 detection, cells were fixed with Fix/Perm buffer and stained with anti-Foxp3-APC (eBioscience). Cells were acquired on a LSRII flow cytometer (BD Biosciences) and analyzed using FlowJo software (Treestar, Ashland, OR).
2.5 Histopathology and scoring
At the indicated time points, hearts were removed and cut longitudinally into half with a scalpel; one half fixed in 4% PFA overnight and kept in 70% ethanol until further processing. Tissues were paraffin embedded with the cut surface down and sections of 5 μm thickness were cut for hematoxylin and eosin (H&E) staining. Paraffin blocks and sections were prepared and stained by the Histology and Immunohistochemistry Shared Resource (University of California, San Diego, Moores Cancer Center, CA). Inflamed hearts were characterized by the presence of interstitial infiltrate of usually mononuclear cells associated with focal myocyte necrosis and in acute cases fibrosis. In some cases, extensive tissue necrosis was seen in the pericardium (pericarditis). Heart sections were scored blindly according to the following scoring criteria: grade 1: 0–10% of the total heart tissue shows immune inflammation (presence of lymphocytic infiltration) or any kind of tissue pathology i.e. pericarditis, grade 2: 11–25%; grade 3: 26–50%; grade 4: greater than 50%.
2.6 ELISPOT
IL-10, IL-17 and IFNγ (BD-Pharmingen and Biolegend) producing cytokines were detected by ELISPOT as previously described (28). In brief, splenocytes from CM peptide-immunized and control, hpCVB3 infected mice were diluted by factor of two starting at 10^6 cells/well down to 0.25×10^6. Cells were cultured for three days in the presence of CM-combo peptide and recombinant IL-2 (50U/ml) (Roche, Pleasanton, CA). Color was developed with 3-amino-9-ethylcarbazole (AEC) (Sigma-Aldrich, St Louis, MO) and H2O2. Lastly, plates were rinsed in water, left air dried, and spots representing cytokine-producing cells were photographed and counted using a computer-assisted image analysis (Zeiss KS ELISPOT reader).
2.7 Antibody treatments
Mice were treated at the indicated time points with 150 μg/mouse anti-OX40L (clone RM134L, Biolegend) or anti-CD25 (clone PC61, BD-Pharmingen) or anti-IL-10 (clone JES5-2A5) and isotype antibody controls.
2.8 Adoptive transfer experiments
Splenocytes from CM combo treated, hpCVB3 infected mice were pooled together. Splenocytes were depleted of CD8 T cells by using anti-CD8 antibody incubation (BioLegend, San Diego, CA, USA), followed by incubation with sheep anti-Rat IgG coated Dynabeads (Invitrogen, San Diego, CA, USA). Following the CD8-depletion step, cells were resuspended at 10×106/ml in 10%vol/vol RPMI containing 50U/ml rhIL-2 and 20μg/ml combo peptide mix, and cultured for 3 days. Next cells were further purified into CD4+CD25+ or CD4+CD25− fractions using the CD4+CD25+ Regulatory T cell isolation kit (Miltenyi Biotech, Auburn, CA). At least 1×106 total purified lymphocytes were stained with CFSE (29) and adoptively transferred intravenously (i.v.) into new BALB/C mice, which were subsequently infected with hpCVB3.
2.9 Heart infiltrate isolation
Heart infiltrate was prepared as previously described (23). In brief, mice were killed with CO2 and immediately perfused with 1× DPBS. One half of the each mouse heart was kept for histology (described above), whereas the other half was minced and digested with 0.2% collagenase type II, 0.25% pancreatin (both from Sigma-Aldrich, USA) and 0.1% DNase I (Roche Applied Science, Basel, Switzerland) for 7 minutes at 37°C. Digestion was stopped with the addition of 0.1M EDTA. Following digestion, single cell suspensions were prepared by filtering through stainless steel mesh 200 gauge.
2.10 Statistics
Unpaired Student’s t-test was implemented for all statistical analysis apart from differences in disease severity, which were calculated with the Mann Whitney U test. p values lower than 0.05 (*) were considered significant.
3. Results
3.1 Intranasal CM combo peptide (CM947-960 and CM735-747) administration protects male BALB/C mice from sublethal CVB3 infection
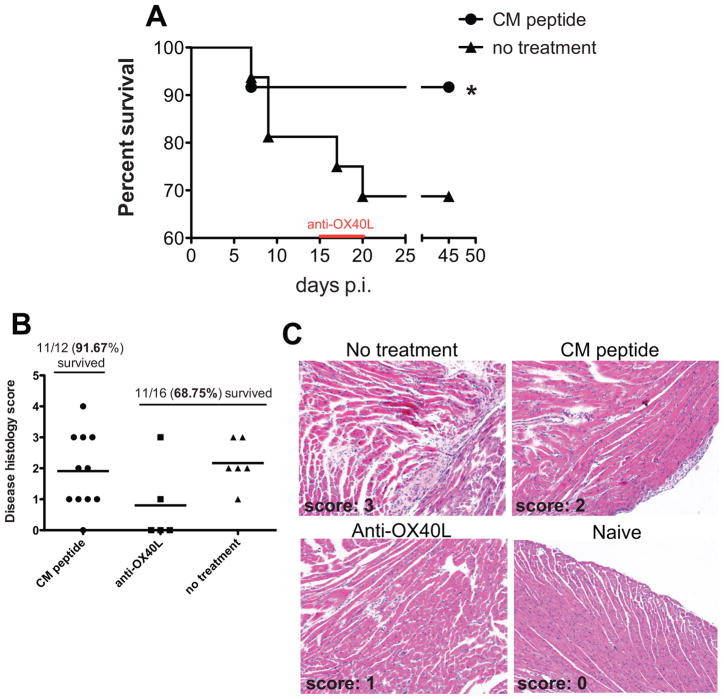
Acute myocarditis can be induced in BALB/C male mice after infection with 10^3 plaque forming units (PFU) of CVB3 (Nancy strain). Acute myocarditis is an inflammation of the heart muscle, which within 10 days after infection typically proceeds into heart failure and sudden death. Disease is more severe in males than females and some studies suggest a role of estrogens on the activity of immunosuppressive Treg populations (20). Here, we attempted to induce cardiac-specific Tregs by nasal immunization with the CM-derived peptides CM947-960 and CM735-747, which were previously described to induce EAM in BALB/C mice (14; 18). We sought to combine both epitopes in order to enhance our protective effect (combination therapy). In order to understand the effect of nasal CM combo peptide vaccination in CVB3-induced acute myocarditis, male BALB/C mice were treated for 3 consecutive days prior to infection with CVB3. Mice were separated in 2 experimental groups: 1) nasal CM peptide treatment (n=12), and 2) no treatment, (n=16). As shown in Fig. 1A, a significant reduction in the percentage of mice dying from the sublethal CVB3 infection was seen. The majority of nasal peptide treated mice survived (11 out of 12), while 5 out of 16 (31.25%) died in the group not treated with the CM peptides by the twentieth day after infection. While most of the untreated mice died in the first 10 days after the infection, few perished later, one at 17 and one at 20 days after infection (next section in more detail). However, in both groups of mice, significant heart inflammation was detectable in those mice that survived the infection (Fig. 1B–C).
Fig. 1. Prevention from death caused by sublethal CVB3 infection after nasal CM peptide treatment, and reduction in cardiac inflammation after anti-OX40L blockade.
Seven-week old male BALB/C mice were infected with 10^3 PFU CVB3. Mice were immunized nasally for 3 consecutive days with CM947-960 and CM735-747 (40μg each) before viral infection (days −3,−2,−1) or left untreated. (A) Survival was followed over time post infection (p.i.) with CVB3. *, p<0.05. Thirteen mice surviving the infection in the untreated group by the fifteenth day after infection were subsequently divided in two groups: one that was treated with anti-OX40L, 150 μg per mouse on days 15, 17, 19 from infection (n=6), and a second that remained untreated (n=7). Of these, two more mice died, one belonging into the anti-OX40L group that was already sick at the time of the treatment and died soon after the first antibody infection and one more belonging to the untreated group, which died at 19–20 days after infection. In the remaining mice, myocarditis severity score was evaluated 45 days after infection shown in (B–C). CVB3-infected BALB/C mice treated with anti-OX40L displayed the highest reduction in heart inflammation. Hematoxylin and eosin (H & E) stained sections from hearts of CVB3-infected and naïve mice treated with CM peptides or anti-OX40L.
3.2 Anti-OX40L blockade inhibits myocarditis progression in mice surviving the lethal CVB3 infection
Given the results described above, we sought to investigate the effect of anti-OX40 blockade (clone RM134L) treatment in halting myocarditis severity. To this end, 13 mice in the untreated group that remained alive by the fifteenth day after infection were divided into two sub-groups: one, which remained untreated (n=7), and a second group that received three anti-OX40L blocking antibody injections (150 μg/mouse) on days 15, 17 and 19 after infection (n=6). Of those, one mouse in the anti-OX40L group and already sick at the time of treatment died after the first antibody injection on day 17, while one more mouse in the group that remained untreated died 2–3 days later. We cannot conclude whether anti-OX40L therapy protected the mice from further lethality to CVB3 infection, however, histological examination of the heart tissue at day 45 revealed a significant reduction in inflammation after OX40L blockade treatment, whereas nasal CM peptide treated and control mice displayed similar degrees of inflammation (Fig. 1B–C). Altogether, nasal CM peptide treatment can protect male BALB/C mice from acute myocarditis acute myocarditis-associated mortality, while persistent CVB3-driven heart inflammation can be reduced by anti-OX40L blockade treatment.
3.3 Nasal CM combo peptide treatment increases Treg frequency in blood and spleen and protects from autoimmune myocarditis
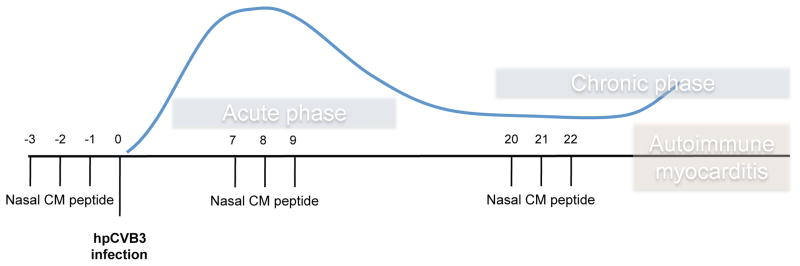
Since autoimmune myocarditis is more relevant to the human disease, the majority of our follow-up studies were conducted with the chronic hpCVB3-induced model. Similarly, we attempted to induce Tregs by nasal immunization with the CM-derived peptides, following several nasal immunization protocols, since we were not sure which would deliver the most beneficial effect. In male BALB/C mice, infection with hpCVB3 virus leads to a peak in myocarditis around day 7 post-infection (p.i.), which resolves after ~21 days and is followed by a second T cell-driven chronic phase of the disease, which occurs around day 28–35 p.i. (8). To this end, three consecutive daily treatments from the day of infection (d=0) were conducted: a) before viral infection (−3, −2, −1), b) during the acute phase of the immune response (7, 8, 9), 3), and/or c) during the transition to the chronic phase of the immune response (20, 21, 22). We also conducted a combination of a), b) and c). Interestingly, the best outcome was obtained when immunizations had started prior to hpCVB3 infection (data not shown). Moreover, the best protection was seen when immunizations were initiated prior to infection and repeated at the peak of the response and again at the transition to the chronic phase (Fig. 2).
Fig. 2. Intranasal CM peptide immunization protocol.
A limited number of mouse strains, including male BALB/C, seem to develop an acute viral myocarditis followed by a chronic stage after infection with a cardiotropic strain of CVB3. The peak of inflammation of this early viral myocarditis is around nine days after the infection indicated by the first wave in the figure. The mice usually do not die from the viral myocarditis in this model but rather progress to a chronic myocarditis with generalized mononuclear infiltration accompanied by the production of antibodies to cardiac myosin (indicated by the second wave, autoimmune myocarditis). Here, six to eight-week old male BALB/C mice were infected with 10^3 PFU heart-passaged CVB3 (hpCVB3, Nancy strain). Mice were immunized nasally for 3 consecutive days with CM947-960 and CM735-747 (40μg each) at the indicated (vertical small lines) time points.
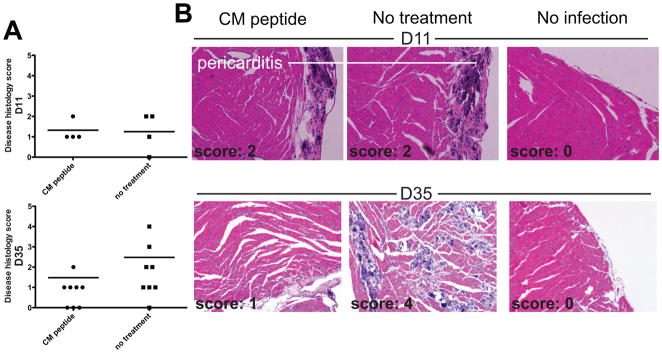
Upon nasal treatment with CM peptides following the scheme presented in Fig. 2, no effect on heart inflammation (mostly seen as pericarditis) was seen 11 days after infection with hpCVB3 (Fig. 3). This time point though coincides with the contraction phase of the initial response, where minimal residual inflammation can usually be detected. Histological examination of the heart tissues 35 days after infection, when the chronic nature of the disease starts to peak, showed significantly reduced inflammation in the hearts of the mice treated with the CM peptides (mean score 1.5±0.5) compared to non treated (mean score: 2.5±1.5) suggesting that induction of tolerance towards the targeted autoantigens -CM peptides- was achieved (Fig. 3). Interestingly, viral titers predominantly in the heart evaluated on day 11 after infection with plaque assay showed no differences, suggesting that the treatment did not significantly alter the antiviral immune response (data not shown).
Fig. 3. Reduced cardiac inflammation after nasal CM combo peptide vaccination.
Seven-week old BALB/C mice were infected with 10^3 PFU hpCVB3 (Nancy strain). Mice were treated according to the protocol shown in Fig. 2. (A) Severity scores of individual diseased and control (naïve) BALB/C mice at 11 days (upper panels) or 35 days (lower panels) post infection (p.i.) (B) H & E histological heart sections from uninfected, CM-peptide combo immunized and untreated CVB3-infected mice for the same time points after infection.
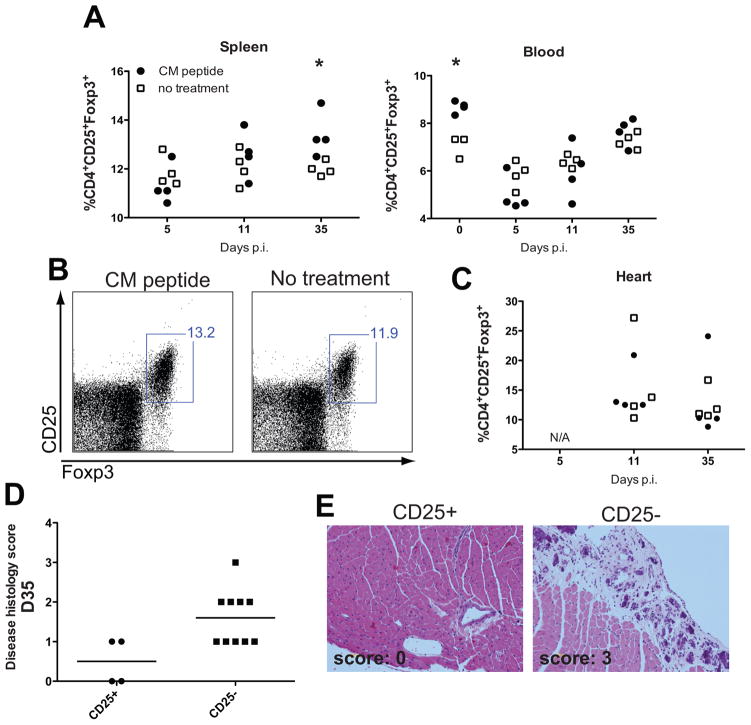
As disease is thought to be driven by T cells and antagonized by Treg, CD4+ and CD8+ T cell populations were analyzed in the spleen, heart and blood by flow cytometry on days 5, 11, and 35 after infection with hpCVB3. Since no significant disease-associated alterations in the markers expressed on CD8+ T cells were observed (data not shown), the results we obtained in the CD4+ population are documented. Nasal treatment with CM peptides showed no difference in the CD4+ effector memory-like population identified as CD44hiCD62Llow cells (data not shown). Interestingly, upon examining Treg fluctuation over time, we observed that after CM combo peptide immunization, there was a transient and significantly higher induction in the blood compared to the control group. Two days after the last nasal immunization prior to infection with hpCVB3, Treg frequency in the blood was ~7% for the control group, while the frequency in immunized mice was 9% (Fig. 4A). However, this difference was lost after CVB3 infection at three time points analyzed (5, 11 and 35 days after infection). In the spleens of infected mice that received CM peptide treatments on the other hand, the Treg frequency slightly peaked at 35 days after infection, somewhat correlating with protection from the disease (Fig. 4A–B). No differences were observed in the Treg frequency within the heart infiltrate (Fig. 4C).
Fig. 4. Treg frequency increases after nasal CM peptide immunization.
(A) Spleen and or blood derived lymphocytes from CM peptide-immunized mice were stained and analyzed with flow cytometry to determine the frequency of Treg (CD25+Foxp3+). The frequency was determined over time after gating on total CD4+/CD127low T cells, n= 4 mice per group. The data are significantly different among CM-peptide treated group and no treatment only for the indicated time points. These can be identified by the asterisk “*”, which determines a p value <0.05. (B) Representative flow cytometry plots indicating the frequency of Treg in the spleen after gating on CD4+/CD127low cells, 35 days post infection (p.i.) with hpCVB3. (C) Treg frequency in the heart infiltrate at the indicated time points p.i. (D) Histological scoring and representative microphotographs from hearts of mice after receiving 1×10^6 CFSE-labeled CD4+CD25+ or CD4+CD25− cells from CM combo peptide immunized mice.
In order to further demonstrate the involvement of Treg in mediating tolerance after nasal CM peptide treatment, CD4+ T cells from treated and un-infected mice were purified two days after the last treatment and separated into CD25+ and CD25− fractions. Both fractions were CFSE labeled and subsequently adoptively transferred by i.v. injection into recently infected mice (day 6 after infection). We monitored the engraftment of the cells by weekly blood withdraws and we saw no signs of proliferation, while Foxp3 levels became reduced over time in mice that received the CD25+ fraction (data not shown). Next, we evaluated for the presence of heart inflammation in mice receiving these T cells, assessed 35 days after virus infection. Interestingly, as shown in Fig. 4D–E, CD4+CD25+ cells from the nasal CM peptide treated group were able to halt autoimmune myocarditis progression. While additional experimentation is necessary to fully reveal their in vivo mechanism of action, the data discussed further below indirectly implicate IL-10 production in tolerance induction.
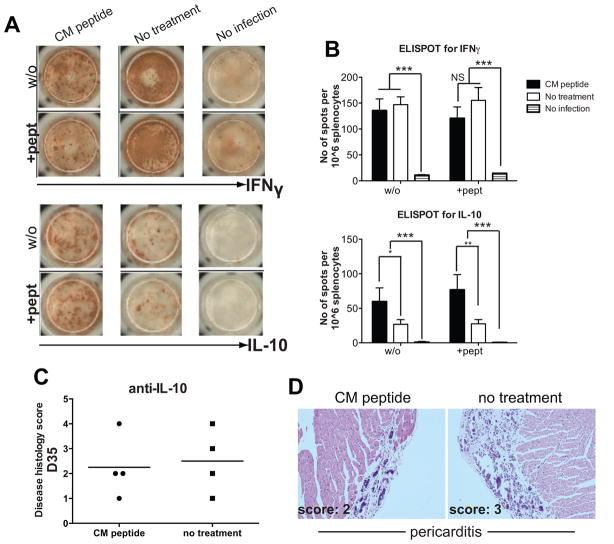
3.4 Nasal CM combo peptide treatment increases IL-10 production in the spleen
In this study, we measured IL-17, IFNγ and IL-10 levels with ELISPOT immuno-assay in spleens derived from mice immunized with CM combo peptide at 11 and 35 days post infection (p.i.). Interestingly, we could not identify clear alterations in the expression levels of IL-17. Nevertheless, as it is clearly shown in Fig. 5A–B (and data not shown), an increased expression IL-10 was seen in mice treated nasally, while IFNγ was somewhat but not statistically significantly dampened 11 days after disease induction. In order to examine the importance of the elevated IL-10 levels, anti-IL-10 blocking approaches were conducted simultaneously with nasal CM peptide treatments. More specifically, mice that were nasally immunized following the regimen described in Fig. 2, were treated intraperitoneally (i.p.) twice with 150μg anti-IL-10 (clone JES-A25) at days 2 and 22 after infection. As controls, mice infected with CVB3 but not treated with CM peptides were treated with anti-IL-10. As shown in Fig. 5C–D, upon in vivo IL-10 neutralization, the majority of CM peptide nasally treated mice displayed an enhanced degree of autoimmune myocarditis. These results provide significant evidence for IL-10 in mediating protection from the disease after nasal CM peptide treatment.
Fig. 5. IL-10 induction in the spleen of nasally CM combo peptide treated mice.
Seven week-old BALB/C mice were treated nasally with CM peptides according to the scheme shown in Fig. 2. Mice were infected with 10^3 PFU of hpCVB3 (Nancy strain). On day 11 after infection, mice were killed and assayed for the production of IFNγ, IL-10 and IL-17 by ELISPOT. (A) Representative ELISPOT pictures for IFNγ and IL-10 cytokines without (w/o) or after in vitro stimulation with the CM peptides (+pept). As control, untreated and uninfected mice were included. (B) Cumulative ELISPOT results for IFNγ and IL-10, n=4 mice per group. *, p<0.05, **, p<0.005, ***, p<0.001. (C) Histological scoring for the presence of heart inflammation in individual diseased BALB/C mice at 35 days p.i. treated with anti-IL-10 blocking antibody. Mice were treated twice i.p. with 150μg anti-IL-10 mAb (clone JES-A25) at days 2 and 22 post infection (p.i.). (D) H & E stained sections from hearts of anti-IL-10 blockade treated mice 35 days after infection. The degree of pericarditis is increased after anti-IL-10 blockade treatment in CM peptide treated and control mice.
Interestingly, upon closer look at bystander cytokine production (without stimulation) ELISPOT results, an interesting observation was made: CVB3 viral infection induced increased levels of IFNγ and IL-10 in splenocytes from mice 11 days after infection (Fig. 5). While the elevation of IFNγ was somewhat expected, we were startled to observe the elevated of IL-10 levels caused by CVB3. Interestingly, IL-10 neutralization seemed to somewhat exacerbate disease progression suggesting that among the mechanisms controlling excessive immunopathology following CVB3 infection is through IL-10 production. Following similar cytokine production analysis at a later time point, 35 days after infection, no such bystander IL-10 cytokine production was seen (data not shown).
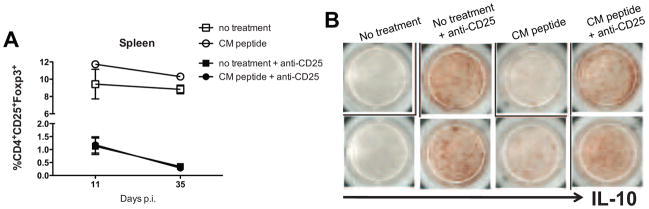
3.5 Anti-CD25 treatment increases bystander IL-10 production and protects from autoimmune myocarditis
Our results in Fig. 4 implicated a role for CD4+CD25+Foxp3+ Tregs in tolerance induction after nasal CM peptide treatment. In order to further address how this population might be involved in tolerance induction, we followed an additional approach: Tregs were depleted concomitantly with CM peptide treatments. More precisely, mice vaccinated nasally with CM peptides following the regimen described in Fig. 2, were concomitantly treated four times i.p. with 150μg anti-CD25 (clone PC61), at days −8, −2, 18 and 22 from infection. In the control group, mice infected with CVB3 not treated with CM peptides were included. Interestingly, upon in vivo CD25 depletion significantly reduced autoimmune myocarditis was seen in all of the groups (data not shown). We next examined for the presence of CD4+CD25+Foxp3+ cells on days 11 and 35 after infection and for the presence of cytokines by ELISPOT immunoassay. Anti-CD25 in vivo administration was effective in depleting CD4+CD25+Foxp3+ cells in CM peptide treated and control mice. Phenotypic analysis conducted in spleen, blood and heart infiltrate showed great reduction in the frequency of CD4+CD25+Foxp3+ cells (Fig. 6A and data not shown). Since effectors are also expressing CD25 upon CVB3 infection, we assume that the protective effect observed after anti-CD25 depletion was due to elimination of the auto-reactive effectors and not the Tregs.
Fig. 6. Anti-CD25 treatment depletes Treg and effector cells while it upregulates bystander IL-10 production in the spleen.
Mice were treated with anti-CD25 (clone PC61) depleting antibody four times i.p. with 150μg at days −8, −2, 18 and 22 p.i., n= 3–4 mice per group. (A) Spleen cells from CM peptide-immunized treated mice were stained and analyzed for flow cytometry to determine the frequency CD4+CD25+Foxp3+ (Treg) on days 11 and 35 after infection. The frequency was determined after gating on total CD4+ T cells. (B) Representative ELISPOT results for IL-10 without or after stimulation with the CM peptides in mice treated or not-treated with the anti-CD25 depleting antibody.
Taking our model further, we analyzed the cytokine production profile in mice after anti-CD25 treatment by ELISPOT analysis. To our great surprise, an unexpected outcome was revealed: anti-CD25 blockade increased the bystander IL-10 cytokine production in the spleens of the anti-CD25 treated mice (Fig. 6B). Based on these findings, we assume that anti-CD25 treatment abolished the generation of CD25+ Tregs and but also effectors, while it enhanced the overall bystander IL-10 production already set in place by the CVB3 infection. These results provide a novel concept regarding the regulation of the antiviral CVB3 response and consequently autoimmune myocarditis in infected mice. Progression to CVB3-induced myocarditis appears to be controlled to a great extent by an IL-10 circuit that requires further investigation in order to be fully elucidated.
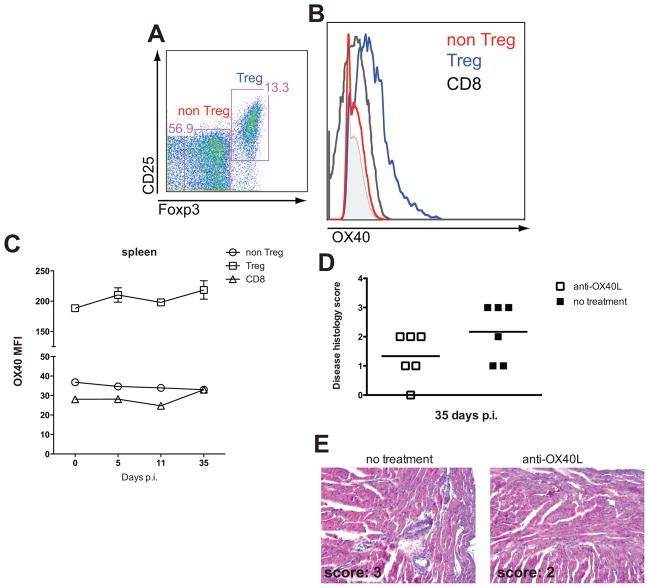
3.6 OX40 is primarily expressed on CD8+ and Tregs; blockade of OX40-OX40L signaling reduces CVB3-induced autoimmune myocarditis
Here, we investigated the effect of blocking OX40-OX40L interaction in affecting autoimmune myocarditis progression. At first, we monitored the OX40 levels within the CD4+ and CD8+ populations in spleen and blood. Within the CD4+, Treg cells constitutively high expressed OX40 (Mean Fluorescence Intensity [MFI]: 180±10), which increased over time after CVB3 infection (Fig. 7A–C and data not shown). While non Treg cells did not express neither significantly upregulated OX40, we observed an increase in CD8+ cells. More precisely, CD8 cells constitutively expressed low levels of OX40 (MFI: 28±2), which increased at the transition to the chronic stage of myocarditis (MFI: 32±2) (Fig. 7A–C and data not shown). The elevated expression of OX40 on CD8+ and moreover Tregs further perplexes our second hypothesis, where anti-OX40L blocking treatments were initially considered.
Fig. 7. OX40 is expressed predominantly on Treg and CD8+ cells; Reduced cardiac inflammation after i.p. anti-OX40L blockade treatment.
Eight-week old BALB/C mice were infected with 10^3 PFU of hpCVB3 (Nancy strain). (A) Representative flow cytometry plot depicting Treg versus non Treg gating based on which OX40 mean fluorescent intensity (MFI) levels were analyzed. (B) Histogram overlay showing the levels of OX40 on Treg (blue line), non Treg (red line) and CD8+ cells (black line) versus isotype control (filled gray line). (C) Splenocytes from CVB3-infected mice were stained and analyzed with flow cytometry to determine the MFI of OX40 on Treg, non Treg and total CD8+ T cells for the indicated time points post infection (p.i.) with CVB3. n= 3–4 mice per group. (D–E) Mice were treated i.p. with 150μg of blocking anti-OX40L mAb (clone RM134L) three times, at days 16, 18 and 20 p.i. Severity scores of individual diseased BALB/C mice at 35 days p.i. are shown in (D), while in (E) H & E stained sections from their hearts.
Mouse Treg constitutively express OX40, and some studies have suggested that OX40 might regulate the expansion or survival of Treg. However, whether this is a natural physiological activity of OX40 for Treg is unclear as other studies have shown that OX40 signaling can prevent the induction of adaptive Foxp3+ (aTreg) or IL-10+ Treg, and can also downregulate suppressive activity in natural Foxp3+ Treg. Ultimately, the effect of blocking OX40-OX40L interactions will depend on the balance of OX40 signaling to either an effector T cell or aTreg. As most studies of OX40L neutralization in autoimmune and inflammatory models have shown reduced disease and inflammation, this implies that targeting OX40L predominantly affects the effector arm of the T cell response. This is also substantiated by the observation that in murine as well as in human diseased cardiac myocytes, expression of TNF ligand superfamily co-stimulatory molecules was elevated implying a role in cell-cell mediated myocardial damage (24–26). In addition, targeting a number of other costimulatory molecules that can also be expressed on Treg as well as effectors, including CD40-CD40L, CD28-B7, and 4-1BB-4-1BBL have been proven beneficial in ameliorating the course of many autoimmune diseases, including myocarditis (30–32). Therefore, in order to address this question in CVB3-induced myocarditis, BALB/C mice infected with CVB3 were treated with 150μg of blocking anti-OX40L mAb (clone RM134L) i.p. three times, at the transition to the chronic phase (days 16, 18 and 20 p.i.) and monitored for signs of disease. Significantly, the degree of heart inflammation was decreased as evaluated histologically (Fig. 7D–E and data not shown) suggesting that while Treg might express OX40, blocking OX40-OX40L interactions predominantly suppresses the effector/pathogenic T cells.
Taken together, our results have shown that nasal CM combo peptide treatment ameliorates CVB3-myocarditis progression when initiated at a prophylactic setting. The mechanism involves invigoration of Foxp3+ Treg and IL-10 production. Interestingly, endogenous IL-10 production seems to act as a compensatory mechanism involved in controlling excessive immunopathology following infection with CVB3. On the other hand, OX40 is predominantly expressed on CD4+ effector T cells and Treg and anti-OX40L blockade approaches can provide additional treatment strategies when conducted late during disease progression.
4. Discussion
Infection with cardiotropic viruses, such as CVB3 (Nancy strain), can lead to myocardial damage in a limited number of susceptible mouse strains, which depending on its severity, can lead to sudden death or progress to autoimmune myocarditis (5; 33). In humans, infection by viral, bacterial, protozoan and other pathogens can in some severe cases cause heart infarction followed by heart failure and in some rare cases death (34; 35). The most common virus associated with persisting, chronic inflammation of the myocardium in humans is CVB3. Interestingly, in the majority of these cases, persistent viral genome can be found, suggesting that the remaining inflammatory response is due to an ongoing antiviral immunity (36). Despite the lack of strong direct evidence in humans (37), results in mice suggest that autoimmunity as a result of cardiotropic CVB3 infection can occur (8). In such cases, cardiac myosin specific antibodies and T cell clones that persist after viral clearance can be found that can cause de novo myocarditis upon adoptive transfer into unmanipulated hosts (10–12). Here, we took advantage of a virally-induced myocarditis model, where acute disease followed by sudden death and progression to autoimmune myocarditis can be recapitulated in BALB/C male mice following infection with CVB3. Given the difficulties to fully translate our findings to humans, we were able to show that nasal CM peptide treatment initiated at a prophylactic setting can greatly reduce acute infection-induced death and inhibit transition to the chronic phase. Moreover, further targeting the OX40-OX40L co-stimulatory pathway during the transition to the chronic stage, strongly halted myocarditis progression.
Amelioration of disease progression following autoantigen administration in a tolerogenic manner is known to occur in several autoimmune settings (38), including diseases induced after pathogen infection (39). Of importance to myocarditis, whole CM nasal administration or oral CM peptide (614–629) treatment was able protect susceptible mice from EAM (18; 19). EAM studies showed that IL-10 induction and Treg invigoration was involved, which shut down the effector Th1 and Th17 response. Recent findings attribute a detrimental role for IL-23 and IL-17 in EAM. Mice lacking T-bet expression and thus IFNγ responses develop severe EAM, due to increased IL-17 production in the inflamed heart (40). In another study however, IL-17 was found to be important in postmyocarditis cardiac remodeling and the progression to DCM (33). However, the role of IL-17 in CVB3-induced myocarditis is less clear and here we could not attribute any specific effect on CVB3-induced disease progression after nasal CM peptide treatment.
On the other hand, we were able to show that IL-10 and Treg induction were set in place to achieve tolerance after CM peptide combo immunization, where CVB3 myocarditis was induced. More precisely, Treg identified as CD4+CD25+Foxp3+ cells, were slightly increased in the blood and spleen of CM combo immunized mice, but not in controls. In addition, adoptive transfer of CD4+CD25+ cells from immunized but uninfected mice into new hosts, was able to confer protection from CVB3-induced myocarditis. Interestingly, anti-CD25 depletion following CM peptide treatment did not restore progression to autoimmune myocarditis. To our surprise, disease progression was greatly halted. Interestingly, in another study, oral administration of antigens coupled to the B subunit of the cholera toxin (CTB) into mice depleted of CD25+ cells still gave rise to systemic tolerance (41). While depletion of effector CD25+ cells could account for this and our observation, the increased IL-10 levels in the spleens of anti-CD25-treated mice suggest that in CVB3-infected animals IL-10 plays a significant role in controlling disease severity per se.
IL-10 seemed to play a role in mediating tolerance induction after CM combo peptide treatment; while IL-10 levels increased in spleens of CM-treated mice, IFNγ levels were reduced. The spleen seems to be a vital organ in long-term tolerance maintenance induced after mucosal antigen administration in mice involving Treg and IL-10 (Tr1) induction (42). In the present study, bystander IL- 10 production was increased in CVB3-infected compared to naïve mice. No direct evidence regarding the source of IL-10 was seen, however our CD25-depletion studies suggest that IL-10 was derived from a non-CD25+ T cell source, perhaps Tr1 cells (43). The role of IL-10 in CM-peptide induced tolerance and CVB3-induced myocarditis was revealed through an additional approach. When anti-IL-10 neutralizing antibodies were concomitantly administered with CM combo peptide treatments, disease was significantly exacerbated. The severity was worse than in the control, non anti-IL-10-treated mice, suggesting that IL-10 production is among the mechanisms taking place that control excessive immunopathology due to CVB3 infection. Interestingly, in studies of lymphocytic choriomeningitis virus (LCMV) in mice, IL-10 was associated with viral persistence (44; 45). Moreover, in the acute LCMV infection model followed by viral clearance, IL-10 production directly inhibited effector and memory CD4 T cell responses (46). These and our observations here suggest that IL-10 production following viral infection is involved in controlling excessive CD4 T cell immunity.
In addition to enhancing Treg generation, we reveal another approach to therapy of myocarditis. Costimulatory receptor signaling to T cells has been found to be important for the full differentiation of CD4+ cells into Th1, Th2 and more recently Th17 phenotypes(47–49). Of importance to myocarditis, OX40 (CD134), a costimulatory receptor of the TNFR superfamily, was detected on pathogenic effector T cells, coinciding with increased levels of OX40-ligand (OX40L) expression on diseased cardiomyocytes (24–26). Whether increased expression of TNF-superfamily costimulatory molecules on cardiac myocytes represents the cause or the result of the disease is not clear. Infiltrating cells producing Th1 cytokines such as IFNγ, could induce the expression of costimulatory molecules, while the virus might directly induce their expression which in turn leads to activation of T cells (26). Perhaps fitting with the latter scenario, signaling through OX40 ligand was shown to induce vascular endothelial cells to produce RANTES/CCL5 (50) which might selectively facilitate the diapedesis of Th1 pathogenic T cells at the site of inflammation (51). Interestingly, in EAM, targeting CD28/CTLA-4/B7, CD40/CD40L, ICOS/ICOSL and 4-1BB/4-1BBL costimulatory pathways attenuated disease development (30; 32; 52–54). Therefore we reasoned that targeting the OX40-OX40L signaling cascade through anti-OX40L blockade would result in further halting disease progression.
Apart from the potentially indirect role in recruiting effector T cells at the site of inflammation, OX40 has been shown to directly mediate the binding of T cells to vascular endothelial cells (47; 55). On the other hand, OX40 costimulation in other systems has been shown to inhibit the generation of Foxp3+ aTreg from naïve precursors, suggesting that OX40 can both promote effector T cell generation while at the same time antagonizing the differentiation of aTreg (56–58). Alternatively, some studies have highlighted that OX40 might also positively aid natural Treg survival or their response to IL-2 in some situations (59–60). Given the potential complexity of blocking OX40L in a situation where both effector T cells and Treg were responding, we initially monitored the expression levels of OX40 during the course of CVB3 infection. While no significant expression was detected on CD8+ T cells, CD4+ T cells and Treg expressed OX40 particularly at the peak of the antiviral response. Based on these findings, we reasoned to block the OX40 signaling axes at a window, where the Treg compartment and the anti-CVB3 response might be less affected. To this end, anti-OX40L blocking antibody was administered in CVB3-infected mice at the transition phase towards autoimmune myocarditis. Quite significantly, we found no exacerbation in disease progression as might be expected if OX40 were supporting Treg activity, but rather we observed a strong reduction in disease severity implying an action in blocking the effector/pathogenic response.
Altogether, in the present study we were able to show that nasal administration of CM peptides, initiated before CVB3 infection, can significantly reduce acute and chronic myocarditis in BALB/C male mice. The key finding was that therapeutic activity is more efficient when treatment is initiated before the onset of the autoimmune disease and this activity involves Treg induction and IL- 10 increases. How this approach might impact the physiological antiviral response is not clear, however no significant alterations in endogenous CVB3 titers were seen. Translating our findings to clinical setting faces many obstacles posed by the difficulty in attributing the cause of heart immune pathology to a viral or autoimmune cause. Interestingly though, in our acute CVB3-induced myocarditis studies, where immune pathology is mostly virally-driven, a significant reduction in mortality was seen, suggesting that such an approach would be beneficial in treating CVB3-induced myocarditis or other infection associated autoimmune disorders. In line with these observations, female BALB/C mice are less susceptible to acute myocarditis, and some studies implicate estrogens in the activity of Treg (20). Altogether, our results along with previous studies suggest that CM combo peptide treatment might be proven beneficial in viral-induced myocarditis, since Treg invigoration could result in reduced damage to the host and control of excessive immunopathology.
5. Conclusions
Our findings highlight the importance of Treg and IL-10 in controlling excessive immunopathology following acute CVB3 infection as well as progression to autoimmune myocarditis.
Acknowledgments
This work was funded by an NIAID P01 grant to MGvH. Georgia Fousteri was an American Heart Association Western States Affiliate Awardee for the academic period 2008–2010. Additional support from NIH grants AI67341 and CA91837 to MC. The sponsors for this study had no role in study design; in the collection, analysis, and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Afanasyeva M, Georgakopoulos D, Rose NR. Autoimmune myocarditis: cellular mediators of cardiac dysfunction. Autoimmun Rev. 2004;3:476–486. doi: 10.1016/j.autrev.2004.08.009. [DOI] [PubMed] [Google Scholar]
- 2.Leuschner F, Katus HA, Kaya Z. Autoimmune myocarditis: past, present and future. J Autoimmun. 2009;33:282–289. doi: 10.1016/j.jaut.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 3.Rose NR, Herskowitz A, Neumann DA. Autoimmunity in myocarditis: models and mechanisms. Clin Immunol Immunopathol. 1993;68:95–99. doi: 10.1006/clin.1993.1102. [DOI] [PubMed] [Google Scholar]
- 4.Taqueti VR, Mitchell RN, Lichtman AH. Protecting the pump: controlling myocardial inflammatory responses. Annu Rev Physiol. 2006;68:67–95. doi: 10.1146/annurev.physiol.68.040104.124611. [DOI] [PubMed] [Google Scholar]
- 5.Cihakova D, Rose NR. Pathogenesis of myocarditis and dilated cardiomyopathy. Adv Immunol. 2008;99:95–114. doi: 10.1016/S0065-2776(08)00604-4. [DOI] [PubMed] [Google Scholar]
- 6.Henke A, Huber S, Stelzner A, Whitton JL. The role of CD8+ T lymphocytes in coxsackievirus B3-induced myocarditis. J Virol. 1995;69:6720–6728. doi: 10.1128/jvi.69.11.6720-6728.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Huber SA, Gauntt CJ, Sakkinen P. Enteroviruses and myocarditis: viral pathogenesis through replication, cytokine induction, and immunopathogenicity. Adv Virus Res. 1998;51:35–80. doi: 10.1016/s0065-3527(08)60783-6. [DOI] [PubMed] [Google Scholar]
- 8.Fairweather D, Rose NR. Coxsackievirus-induced myocarditis in mice: A model of autoimmune disease for studying immunotoxicity. Methods. 2007;41:118–122. doi: 10.1016/j.ymeth.2006.07.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cihakova D, Sharma RB, Fairweather D, Afanasyeva M, Rose NR. Animal models for autoimmune myocarditis and autoimmune thyroiditis. Methods Mol Med. 2004;102:175–193. doi: 10.1385/1-59259-805-6:175. [DOI] [PubMed] [Google Scholar]
- 10.Neu N, Beisel KW, Traystman MD, Rose NR, Craig SW. Autoantibodies specific for the cardiac myosin isoform are found in mice susceptible to Coxsackievirus B3-induced myocarditis. J Immunol. 1987;138:2488–2492. [PubMed] [Google Scholar]
- 11.Neumann DA, Lane JR, LaFond-Walker A, Allen GS, Wulff SM, Herskowitz A, Rose NR. Heart-specific autoantibodies can be eluted from the hearts of Coxsackievirus B3-infected mice. Clin Exp Immunol. 1991;86:405–412. doi: 10.1111/j.1365-2249.1991.tb02945.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Neumann DA, Rose NR, Ansari AA, Herskowitz A. Induction of multiple heart autoantibodies in mice with coxsackievirus B3- and cardiac myosin-induced autoimmune myocarditis. J Immunol. 1994;152:343–350. [PubMed] [Google Scholar]
- 13.Lane JR, Neumann DA, Lafond-Walker A, Herskowitz A, Rose NR. LPS promotes CB3-induced myocarditis in resistant B10.A mice. Cell Immunol. 1991;136:219–233. doi: 10.1016/0008-8749(91)90396-s. [DOI] [PubMed] [Google Scholar]
- 14.Pummerer CL, Luze K, Grassl G, Bachmaier K, Offner F, Burrell SK, Lenz DM, Zamborelli TJ, Penninger JM, Neu N. Identification of cardiac myosin peptides capable of inducing autoimmune myocarditis in BALB/c mice. J Clin Invest. 1996;97:2057–2062. doi: 10.1172/JCI118642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Nagler-Anderson C, Terhoust C, Bhan AK, Podolsky DK. Mucosal antigen presentation and the control of tolerance and immunity. Trends Immunol. 2001;22:120–122. doi: 10.1016/s1471-4906(00)01830-5. [DOI] [PubMed] [Google Scholar]
- 16.Mestecky J, Russell MW, Elson CO. Perspectives on mucosal vaccines: is mucosal tolerance a barrier? J Immunol. 2007;179:5633–5638. doi: 10.4049/jimmunol.179.9.5633. [DOI] [PubMed] [Google Scholar]
- 17.von Herrath MG, Harrison LC. Antigen-induced regulatory T cells in autoimmunity. Nat Rev Immunol. 2003;3:223–232. doi: 10.1038/nri1029. [DOI] [PubMed] [Google Scholar]
- 18.Gonnella PA, Del Nido PJ, McGowan FX. Oral tolerization with cardiac myosin peptide (614–629) ameliorates experimental autoimmune myocarditis: role of STAT 6 genes in BALB/CJ mice. J Clin Immunol. 2009;29:434–443. doi: 10.1007/s10875-009-9290-z. [DOI] [PubMed] [Google Scholar]
- 19.Kaya Z, Dohmen KM, Wang Y, Schlichting J, Afanasyeva M, Leuschner F, Rose NR. Cutting edge: a critical role for IL-10 in induction of nasal tolerance in experimental autoimmune myocarditis. J Immunol. 2002;168:1552–1556. doi: 10.4049/jimmunol.168.4.1552. [DOI] [PubMed] [Google Scholar]
- 20.Huber SA. Coxsackievirus B3-induced myocarditis: infection of females during the estrus phase of the ovarian cycle leads to activation of T regulatory cells. Virology. 2008;378:292–298. doi: 10.1016/j.virol.2008.05.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Smith SC, Allen PM. Neutralization of endogenous tumor necrosis factor ameliorates the severity of myosin-induced myocarditis. Circ Res. 1992;70:856–863. doi: 10.1161/01.res.70.4.856. [DOI] [PubMed] [Google Scholar]
- 22.Bachmaier K, Pummerer C, Kozieradzki I, Pfeffer K, Mak TW, Neu N, Penninger JM. Low-molecular-weight tumor necrosis factor receptor p55 controls induction of autoimmune heart disease. Circulation. 1997;95:655–661. doi: 10.1161/01.cir.95.3.655. [DOI] [PubMed] [Google Scholar]
- 23.Poffenberger MC, Straka N, El Warry N, Fang D, Shanina I, Horwitz MS. Lack of IL-6 during coxsackievirus infection heightens the early immune response resulting in increased severity of chronic autoimmune myocarditis. PLoS One. 2009;4:e6207. doi: 10.1371/journal.pone.0006207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Seko Y, Ishiyama S, Nishikawa T, Kasajima T, Hiroe M, Suzuki S, Ishiwata S, Kawai S, Tanaka Y, Azuma M, Kobata T, Yagita H, Okumura K, Nagai R. Expression of tumor necrosis factor ligand superfamily costimulatory molecules CD27L, CD30L, OX40L and 4-1BBL in the heart of patients with acute myocarditis and dilated cardiomyopathy. Cardiovasc Pathol. 2002;11:166–170. doi: 10.1016/s1054-8807(02)00101-1. [DOI] [PubMed] [Google Scholar]
- 25.Seko Y, Takahashi N, Oshima H, Shimozato O, Akiba H, Kobata T, Yagita H, Okumura K, Azuma M, Yazaki Y. Expression of tumour necrosis factor (TNF) receptor/ligand superfamily co-stimulatory molecules CD40, CD30L, CD27L, and OX40L in murine hearts with chronic ongoing myocarditis caused by coxsackie virus B3. J Pathol. 1999;188:423–430. doi: 10.1002/(SICI)1096-9896(199908)188:4<423::AID-PATH373>3.0.CO;2-8. [DOI] [PubMed] [Google Scholar]
- 26.Seko Y, Takahashi N, Oshima H, Shimozato O, Akiba H, Takeda K, Kobata T, Yagita H, Okumura K, Azuma M, Nagai R. Expression of tumour necrosis factor (TNF) ligand superfamily co-stimulatory molecules CD30L, CD27L, OX40L, and 4-1BBL in murine hearts with acute myocarditis caused by Coxsackievirus B3. J Pathol. 2001;195:593–603. doi: 10.1002/path.986. [DOI] [PubMed] [Google Scholar]
- 27.Filippi CM, Estes EA, Oldham JE, von Herrath MG. Immunoregulatory mechanisms triggered by viral infections protect from type 1 diabetes in mice. J Clin Invest. 2009;119:1515–1523. doi: 10.1172/JCI38503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fousteri G, Dave A, Bot A, Juntti T, Omid S, von Herrath M. Subcutaneous insulin B:9-23/IFA immunisation induces Tregs that control late-stage prediabetes in NOD mice through IL-10 and IFNgamma. Diabetologia. 53:1958–1970. doi: 10.1007/s00125-010-1777-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chatzidakis I, Fousteri G, Tsoukatou D, Kollias G, Mamalaki C. An essential role for TNF in modulating thresholds for survival, activation, and tolerance of CD8+ T cells. J Immunol. 2007;178:6735–6745. doi: 10.4049/jimmunol.178.11.6735. [DOI] [PubMed] [Google Scholar]
- 30.Seko Y, Takahashi N, Azuma M, Yagita H, Okumura K, Yazaki Y. Expression of costimulatory molecule CD40 in murine heart with acute myocarditis and reduction of inflammation by treatment with anti-CD40L/B7-1 monoclonal antibodies. Circ Res. 1998;83:463–469. doi: 10.1161/01.res.83.4.463. [DOI] [PubMed] [Google Scholar]
- 31.Seko Y, Takahashi N, Azuma M, Yagita H, Okumura K, Yazaki Y. Effects of in vivo administration of anti-B7-1/B7-2 monoclonal antibodies on murine acute myocarditis caused by coxsackievirus B3. Circ Res. 1998;82:613–618. doi: 10.1161/01.res.82.5.613. [DOI] [PubMed] [Google Scholar]
- 32.Haga T, Suzuki J, Kosuge H, Ogawa M, Saiki H, Haraguchi G, Maejima Y, Isobe M, Uede T. Attenuation of experimental autoimmune myocarditis by blocking T cell activation through 4-1BB pathway. J Mol Cell Cardiol. 2009;46:719–727. doi: 10.1016/j.yjmcc.2009.02.003. [DOI] [PubMed] [Google Scholar]
- 33.Baldeviano GC, Barin JG, Talor MV, Srinivasan S, Bedja D, Zheng D, Gabrielson K, Iwakura Y, Rose NR, Cihakova D. Interleukin-17A is dispensable for myocarditis but essential for the progression to dilated cardiomyopathy. Circ Res. 106:1646–1655. doi: 10.1161/CIRCRESAHA.109.213157. [DOI] [PubMed] [Google Scholar]
- 34.Feldman AM, McNamara D. Myocarditis. N Engl J Med. 2000;343:1388–1398. doi: 10.1056/NEJM200011093431908. [DOI] [PubMed] [Google Scholar]
- 35.Guilherme L, Kalil J. Rheumatic fever and rheumatic heart disease: cellular mechanisms leading autoimmune reactivity and disease. J Clin Immunol. 30:17–23. doi: 10.1007/s10875-009-9332-6. [DOI] [PubMed] [Google Scholar]
- 36.Kuhl U, Pauschinger M, Seeberg B, Lassner D, Noutsias M, Poller W, Schultheiss HP. Viral persistence in the myocardium is associated with progressive cardiac dysfunction. Circulation. 2005;112:1965–1970. doi: 10.1161/CIRCULATIONAHA.105.548156. [DOI] [PubMed] [Google Scholar]
- 37.Neumann DA, Burek CL, Baughman KL, Rose NR, Herskowitz A. Circulating heart-reactive antibodies in patients with myocarditis or cardiomyopathy. J Am Coll Cardiol. 1990;16:839–846. doi: 10.1016/s0735-1097(10)80331-6. [DOI] [PubMed] [Google Scholar]
- 38.Fousteri G, von Herrath M, Bresson D. Mucosal exposure to antigen: cause or cure of type 1 diabetes? Curr Diab Rep. 2007;7:91–98. doi: 10.1007/s11892-007-0017-3. [DOI] [PubMed] [Google Scholar]
- 39.Collins LV, Eriksson K, Ulrich RG, Tarkowski A. Mucosal tolerance to a bacterial superantigen indicates a novel pathway to prevent toxic shock. Infect Immun. 2002;70:2282–2287. doi: 10.1128/IAI.70.5.2282-2287.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Rangachari M, Mauermann N, Marty RR, Dirnhofer S, Kurrer MO, Komnenovic V, Penninger JM, Eriksson U. T-bet negatively regulates autoimmune myocarditis by suppressing local production of interleukin 17. J Exp Med. 2006;203:2009–2019. doi: 10.1084/jem.20052222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.George Chandy A, Hultkrantz S, Raghavan S, Czerkinsky C, Lebens M, Telemo E, Holmgren J. Oral tolerance induction by mucosal administration of cholera toxin B-coupled antigen involves T-cell proliferation in vivo and is not affected by depletion of CD25+ T cells. Immunology. 2006;118:311–320. doi: 10.1111/j.1365-2567.2006.02368.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Alvarez D, Swirski FK, Yang TC, Fattouh R, Croitoru K, Bramson JL, Stampfli MR, Jordana M. Inhalation tolerance is induced selectively in thoracic lymph nodes but executed pervasively at distant mucosal and nonmucosal tissues. J Immunol. 2006;176:2568–2580. doi: 10.4049/jimmunol.176.4.2568. [DOI] [PubMed] [Google Scholar]
- 43.Battaglia M, Gianfrani C, Gregori S, Roncarolo MG. IL-10-producing T regulatory type 1 cells and oral tolerance. Ann N Y Acad Sci. 2004;1029:142–153. doi: 10.1196/annals.1309.031. [DOI] [PubMed] [Google Scholar]
- 44.Ejrnaes M, Filippi CM, Martinic MM, Ling EM, Togher LM, Crotty S, von Herrath MG. Resolution of a chronic viral infection after interleukin-10 receptor blockade. J Exp Med. 2006;203:2461–2472. doi: 10.1084/jem.20061462. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Brooks DG, Trifilo MJ, Edelmann KH, Teyton L, McGavern DB, Oldstone MB. Interleukin-10 determines viral clearance or persistence in vivo. Nat Med. 2006;12:1301–1309. doi: 10.1038/nm1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Brooks DG, Walsh KB, Elsaesser H, Oldstone MB. IL-10 directly suppresses CD4 but not CD8 T cell effector and memory responses following acute viral infection. Proc Natl Acad Sci U S A. 107:3018–3023. doi: 10.1073/pnas.0914500107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Nohara C, Akiba H, Nakajima A, Inoue A, Koh CS, Ohshima H, Yagita H, Mizuno Y, Okumura K. Amelioration of experimental autoimmune encephalomyelitis with anti-OX40 ligand monoclonal antibody: a critical role for OX40 ligand in migration, but not development, of pathogenic T cells. J Immunol. 2001;166:2108–2115. doi: 10.4049/jimmunol.166.3.2108. [DOI] [PubMed] [Google Scholar]
- 48.Zhang Z, Rosenbaum JT, Zhong W, Lim C, Hinrichs DJ. Costimulation of Th17 cells: Adding fuel or putting out the fire in the inflamed gut? Semin Immunopathol. 32:55–70. doi: 10.1007/s00281-009-0190-3. [DOI] [PubMed] [Google Scholar]
- 49.Croft M. Co-stimulatory members of the TNFR family: keys to effective T-cell immunity? Nat Rev Immunol. 2003;3:609–620. doi: 10.1038/nri1148. [DOI] [PubMed] [Google Scholar]
- 50.Kotani A, Hori T, Matsumura Y, Uchiyama T. Signaling of gp34 (OX40 ligand) induces vascular endothelial cells to produce a CC chemokine RANTES/CCL5. Immunol Lett. 2002;84:1–7. doi: 10.1016/s0165-2478(02)00082-2. [DOI] [PubMed] [Google Scholar]
- 51.Kawai T, Seki M, Hiromatsu K, Eastcott JW, Watts GF, Sugai M, Smith DJ, Porcelli SA, Taubman MA. Selective diapedesis of Th1 cells induced by endothelial cell RANTES. J Immunol. 1999;163:3269–3278. [PubMed] [Google Scholar]
- 52.Ford ML, Larsen CP. Translating costimulation blockade to the clinic: lessons learned from three pathways. Immunol Rev. 2009;229:294–306. doi: 10.1111/j.1600-065X.2009.00776.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Futamatsu H, Suzuki J, Kosuge H, Yokoseki O, Kamada M, Ito H, Inobe M, Isobe M, Uede T. Attenuation of experimental autoimmune myocarditis by blocking activated T cells through inducible costimulatory molecule pathway. Cardiovasc Res. 2003;59:95–104. doi: 10.1016/s0008-6363(03)00334-1. [DOI] [PubMed] [Google Scholar]
- 54.Seko Y, Takahashi N, Ishiyama S, Nishikawa T, Kasajima T, Hiroe M, Suzuki S, Ishiwata S, Kawai S, Azuma M, Yagita H, Okumura K, Yazaki Y. Expression of costimulatory molecules B7-1, B7-2, and CD40 in the heart of patients with acute myocarditis and dilated cardiomyopathy. Circulation. 1998;97:637–639. doi: 10.1161/01.cir.97.7.637. [DOI] [PubMed] [Google Scholar]
- 55.Imura A, Hori T, Imada K, Ishikawa T, Tanaka Y, Maeda M, Imamura S, Uchiyama T. The human OX40/gp34 system directly mediates adhesion of activated T cells to vascular endothelial cells. J Exp Med. 1996;183:2185–2195. doi: 10.1084/jem.183.5.2185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Duan W, So T, Croft M. Antagonism of airway tolerance by endotoxin/lipopolysaccharide through promoting OX40L and suppressing antigen-specific Foxp3+ T regulatory cells. J Immunol. 2008;181:8650–8659. doi: 10.4049/jimmunol.181.12.8650. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Gramaglia I, Weinberg AD, Lemon M, Croft M. Ox-40 ligand: a potent costimulatory molecule for sustaining primary CD4 T cell responses. J Immunol. 1998;161:6510–6517. [PubMed] [Google Scholar]
- 58.So T, Croft M. Cutting edge: OX40 inhibits TGF-beta- and antigen-driven conversion of naive CD4 T cells into CD25+Foxp3+ T cells. J Immunol. 2007;179:1427–1430. doi: 10.4049/jimmunol.179.3.1427. [DOI] [PubMed] [Google Scholar]
- 59.Griseri T, Asquith M, Thompson C, Powrie F. OX40 is required for regulatory T cell-mediated control of colitis. J Exp Med. 207:699–709. doi: 10.1084/jem.20091618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Piconese S, Pittoni P, Burocchi A, Gorzanelli A, Care A, Tripodo C, Colombo MP. A non-redundant role for OX40 in the competitive fitness of Treg in response to IL-2. Eur J Immunol. 40:2902–2913. doi: 10.1002/eji.201040505. [DOI] [PubMed] [Google Scholar]