Abstract
Purpose
To evaluate the physical functioning of Ethiopian trichiasis surgery patients before and six months after surgery.
Design
Nested Cohort Study
Methods
This study was nested within the Surgery for Trichiasis, Antibiotics to Prevent Recurrence (STAR) clinical trial conducted in Ethiopia. Demographic information, ocular examinations, and physical functioning assessments were collected before and 6 months after surgery. A single score for patients’ physical functioning was constructed using Rasch analysis. A multivariate linear regression model was used to determine if change in physical functioning was associated with change in visual acuity.
Results
Of the 438 participants, 411 (93.8%) had both baseline and follow-up questionnaires. Physical functioning scores at baseline ranged from −6.32 (great difficulty) to +6.01 (no difficulty). The percent of participants reporting no difficulty in physical functioning increased by 32.6%; the proportion of participants in the mild/no visual impairment category increased by 8.6%. A multivariate linear regression model showed that for every line of vision gained, physical functioning improves significantly (0.09 units; 95% CI: 0.02–0.16).
Conclusions
Surgery to correct trichiasis appears to improve patients’ physical functioning as measured at 6 months. More effort in promoting trichiasis surgery is essential, not only to prevent corneal blindness, but also to enable improved functioning in daily life.
Introduction
Trachoma, an ocular infection caused by Chlamydia trachomatis, is the leading infectious cause of blindness worldwide. Approximately 40.6 million children have active trachoma, 8.2 million, mainly adults, are suffering from the late sequelae, trichiasis, and about 1.3 million adults are blinded from the end stage, corneal opacity. 1,2
Trachoma is seen in rural, economically underdeveloped areas where living conditions are crowded and good water supplies and basic sanitation services are lacking. Active disease is seen primarily in young children, and repeated bouts lead to conjunctival scarring in young adults. In adults, the prevalence and severity of scarring increases; extensive scarring may result in entropion and trichiasis. Trichiasis requires lid surgery to correct in-turned eyelashes which, if uncorrected, places these individuals at high risk of visual loss and blindness from corneal opacification.3
Ethiopia has one of the highest prevalence of trachoma in the world. A national survey on blindness, low vision, and trachoma conducted in 2005 showed active trachoma prevalence as high as 60% among children aged less than 10 years in certain hyperendemic regions. The prevalence of trichiasis in these regions was as high as 5% among adults. Estimates suggest that greater than one million individuals in Ethiopia are living with trichiasis. 4
The World Health Organization (WHO) has adopted the SAFE (Surgery for trichiasis, Antibiotic use, Face washing, and Environmental change) strategy with the goal of the Global Elimination of Blinding Trachoma by the year 2020.3 A number of different surgical techniques have been used to correct trichiasis; however, the WHO recommends bilamellar tarsal rotation, as this technique has been shown in clinical trials to be effective.5,6
Surgery is performed to prevent further visual loss, but recent research has shown that surgery also improves photophobia and ocular pain, and appears to improve visual acuity.7 Frick et al. showed that in women, trichiasis was associated with excess functional limitation even without visual loss. When vision loss was present in combination with trichiasis functional limitation was greater than has been reported with cataracts.8 However, whether trichiasis surgery translates into improvement in daily life has not been investigated. We hypothesize that trichiasis surgery results in an improvement in self-reported physical functioning associated with improvement in visual acuity in a cohort of trichiasis patients who received surgery, in rural Ethiopia.
Methods
This study was nested within the Surgery for Trichiasis, Antibiotics to Prevent Recurrence (STAR) clinical trial. The STAR trial is a randomized, single-masked clinical trial of antibiotic use in 1452 patients who received trichiasis surgery in the Wolayta Soddo zone of the Southern Nations, Nationalities, and Peoples Region (SNNPR) of Ethiopia. The primary aim was to determine whether postoperative treatment with azithromycin reduces trichiasis recurrence as compared to topical tetracycline within one year after surgery.
The methods have been described in detail elsewhere.9 In summary, patients aged 18 years or older with trichiasis present in at least one eye, with no previous report of trichiasis surgery in that eye, were eligible for enrollment into the study. All patients had bilamellar tarsal rotation surgery performed by trained Integrated Eye Care Workers, all of whom were certified using WHO guidelines.10 Participants were randomly assigned to postoperative azithromycin or tetracycline treatment groups; the primary trial results have been reported previously.11
Examinations were performed at each visit to assess presence of trichiasis and to evaluate trichiasis severity. The 438 participants enrolled during the third recruitment period (October–December 2003) were interviewed using a physical functioning questionnaire, which included perceived difficulty with activities, before and 6 months post-surgery. These 438 participants comprise the cohort used for this sub-study.
Visual acuity was measured at baseline and 6 months post-surgery. Monocular acuity was measured for each eye, with the participant’s presenting refractive correction, using a tumbling ‘E’ chart patterned on a standard Early Treatment for Diabetic Retinopathy Study chart. Trichiasis was defined according to WHO criteria as the presence of one or more lashes touching the globe and/or evidence of epilation. Entropion was graded as mild (all lash bases visible), moderate (some lash bases visible), or severe (no lash bases visible).9–12
Physical functioning was assessed by the administration of a questionnaire. A trained interviewer interviewed the study participants in either Amharic or Wolaytinga, the national and local language, respectively. The questionnaire included activities identified as important for daily functioning in rural Ethiopia. The questionnaire was based on a previous quality of life instrument used in rural Tanzania with Ethiopia-specific factors added, based on field testing.8,9 The items included walking around the village, observing obstacles while walking, recognizing faces, gathering wood, chopping wood, milking cows, helping with the farm, making injera (local bread), grinding coffee, and caring for children. The latter three tasks were specific to women. The possible answers for the first three questions ranged along a 5-point scale: no difficulty, a little difficulty, some difficulty, a lot of difficulty, unable to do the activity. The possible answers for the remaining seven questions included two additional answer choices: never did the activity, stopped doing the activity for reasons other than vision or trichiasis.
Initial Rasch analysis of the questionnaire responses indicated that the categories ‘a little difficulty’ and ’some difficulty’ were not discernibly different. Thus, prior to any further analyses, the physical functioning questionnaire responses of ‘a little’ and ‘some’ were collapsed into one category, turning the 5-point scale into a 4-point scale.
The distribution of responses for all items was examined. Any item for which any degree of difficulty was indicated (none, some, a lot) at baseline but then the response ‘never did’ was given at follow up was re-coded to ‘never did’ at both time points (n=72 responses). Any item for which the response ‘cannot do’ was given at baseline and ‘never did’ was given at follow up was re-coded to ‘cannot do’ at both time points (n=16 responses). Any item for which ‘stopped doing for other reasons’ was given at baseline and ‘never did’ at follow up was re-coded to ‘stopped doing for other reasons’ (n=12 responses). These discrepancies indicate the presence of a possible misunderstanding of meaning of the ‘never did’ response, namely the clear difference between ‘never did the activity’ (meaning never, even before trichiasis) versus ‘can no longer perform the activity’ (meaning never did since trichiasis or eye problem started). Gender specific evaluations of questionnaire responses were conducted since males and females partake in different activities. The questions involving chopping wood for women and milking cows for men were removed from all further analyses since insufficient numbers of persons in the respective genders undertook these activities.
A single score for patients’ physical functioning was constructed using Andrich’s rating scale model, one type of Rasch model. The Rasch model allows responses from different questions (called items) representing different severity or weights to be summed. Weights do not have to be assigned to items in advance. The probability of how a person responds to a rating category of a particular item depends on the characteristic of the item (ie. difficulty of a given question) and the person (ie. perceived impairment in physical functioning from a given disability), plus the response threshold (ie. expected response generated by the Rasch model). The estimated scores were generated from the Rasch analysis on a common logit (log-odds) scale.
The resulting Rasch model was evaluated to ensure that the assumptions were satisfied. Two of the three female-specific items (caring for children and making injera) did not fit into the single scale and were excluded. Subgroup analysis based on gender was carried out and showed consistency among the subgroups; this consistency allowed us to combine the subgroups for subsequent analyses. The remaining seven items applicable to females and the six items for males showed acceptable fit and were kept in the final Rasch model to generate the final physical functioning scores. 13 WINSTEPS (MESA press, Chicago, IL) was used to carry out the Rasch analyses.
Further data analyses were performed using STATA version 11.0 (STATA-Corp LP, College Station, Texas). Visual acuity was scored as the number of letters read and then converted to logMAR values. LogMAR values were converted to snellen values for visual impairment categorization. Visual impairment was categorized as: mild or no visual impairment, visual acuity better than or equal to 20/70; moderate/severe visual impairment, visual acuity worse than 20/70 but equal to or better than 20/400; blindness, visual acuity worse than 20/400. Bivariate relationships were explored to examine differences in baseline characteristics by those who had data at both baseline and follow-up versus those who were missing data at one of these time points, and by those who reported no difficulty with physical functioning at baseline versus those who reported some difficulty. We compared differences between the groups using Fischer’s exact test or a test for trend, if the variable was ordinal.
Changes in visual acuity between baseline and follow-up were assessed. The difference in baseline characteristics and change in vision by change in physical functioning was examined using one-way analysis of variance for continuous variables, test for trend for ordinal variables, and Fisher’s exact test for proportions. Change in vision was defined in two different ways: first, as the difference in acuity between the better eye at baseline and the better eye at follow-up (allowing the eye to change); second, as the maximum difference between baseline and follow up of either the right or left eye. For our final analyses, we chose the second definition, as it appeared to reflect the effect of surgery on vision more completely.
A multivariate linear regression model was used to determine if change in physical functioning was associated with change in visual acuity, after controlling for age, gender, severity of entropion, vision at baseline, and baseline physical functioning was associated with change in visual acuity.
Results
Of the 438 participants, 18 (4.1%) did not have baseline questionnaires, and 9 (2.1%) were not present at follow up, 5 of whom had developed recurrent trichiasis before the 6 month follow-up. Thus, 411 participants had both baseline and follow-up questionnaires. Most of these 411 participants were female (74.5%). At baseline, 131 (31.9%) had severe entropion, and 330 (80.3%) had surgery on both eyelids (Table 1). When comparing these 411 participants to the 27 participants who were missing a questionnaire at either baseline or follow-up, only mean age was different. The mean age of participants who were missing at least one questionnaire was older than those who answered both questionnaires, (55 vs. 48 years; p = 0.01).
Table 1.
Baseline characteristics of trichiasis surgery patients according to whether functional status was measured at both baseline and the 6 month follow-up or was missing at either time point
| Functional Status Measured at Both Visits |
Functional Status Missing at One Visit |
p-value | |
|---|---|---|---|
| Total Participants | 93.8% (411) | 6.2% (27) | |
| Age (years), Mean (SD) | 48 (14) | 55 (13) | 0.01 |
| Gender, % (N) | 0.65 | ||
| Male | 25.6% (105) | 29.6% (8) | |
| Female | 74.5% (306) | 70.4% (19) | |
| Entropion, % (N) | 0.07a,b | ||
| Mild | 52.6% (216) | 70.4% (19) | |
| Moderate | 15.6% (64) | 11.1% (3) | |
| Severe | 31.9% (131) | 18.5% (5) | |
| Trichiasis Recurrence at 6 months, % (N) | 1.5% (6) | N/A | N/A |
| Trichiasis Recurrence before 6 months % (N) | N/A | 18.5% (5) | N/A |
| Bilateral Surgery, % (N) | 80.3% (330) | 74.1% (20) | 0.46 |
| Mean (SD) Baseline Physical Functioning Score | 3.00 (3.02) | 3.03 (2.62) c | 0.98 |
| Level of Visual Impairment d, % (N) | 0.73b | ||
| Mild/No Visual Impairment | 62.2% (253) | 66.7% (6) | |
| Moderate/Severe Visual Impairment | 26.8% (109) | 11.1% (1) | |
| Blind | 11.1% (45) | 22.2% (2) |
the moderate and severe entropion groups were collapsed prior to significance testing
test for trend
consists of 9 people, 18 were missing baseline data
4 people missing baseline visual acuity data
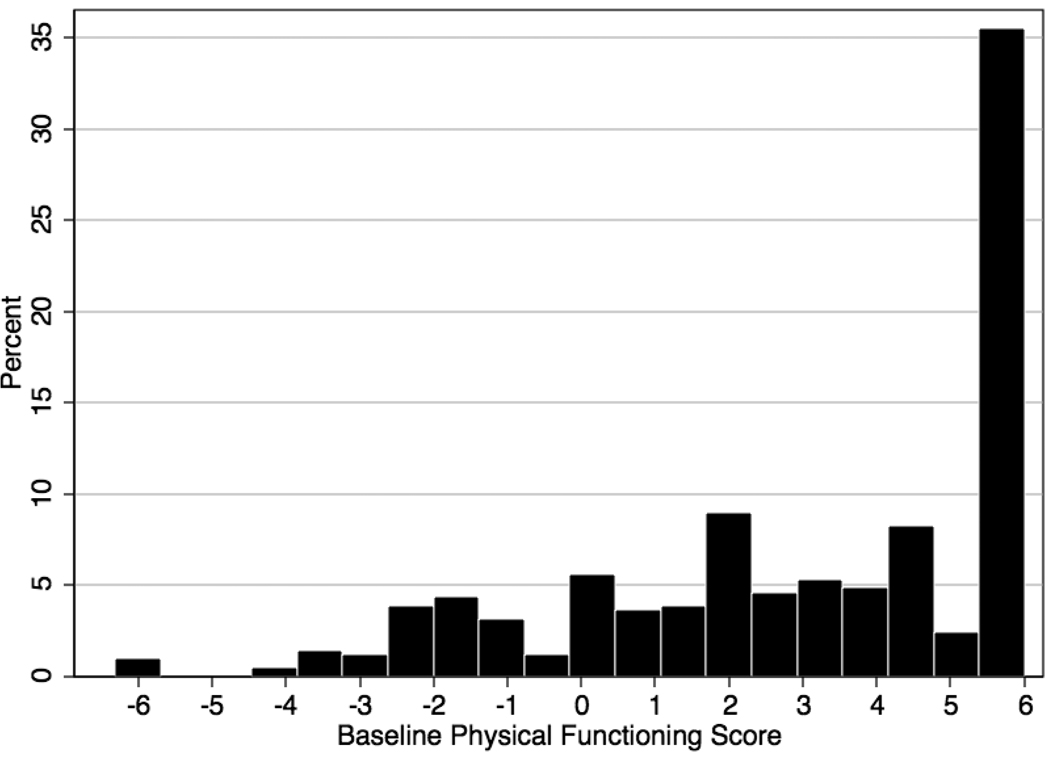
The final physical functioning scores ranged from −6.32 (great difficulty) to +6.01 (no difficulty). The mean physical functioning score at baseline was 3.00. The distribution of the baseline physical functioning scores is shown in Figure 1. The distribution was skewed because greater than one-third of the study participants reported no difficulty with physical functioning, at baseline. Baseline characteristics comparing those with no difficulty (38.9%) to those with some difficulty (61.1%) are presented in Table 2. Age, gender composition, and the percent that underwent bilateral surgery were similar in the two groups; degree of entropion and visual acuity differed significantly. Participants with no difficulty at baseline were more likely to have mild entropion and mild or no visual impairment compared to those with some difficulty at baseline.
Figure 1.
Distribution of Rasch scores for physical functioning of trichiasis patients at baseline
Table 2.
Baseline comparison of trichiasis surgery patients who reported no difficulty on any item of physical functioning to those who reported any difficulty
| No Difficulty | Any Difficulty | p-value | |
|---|---|---|---|
| Total Participants | 38.9% (160) | 61.1% (251) | |
| Age (years), Mean (SD) | 47 (13) | 49 (14) | 0.10 |
| Gender, % (N) | 0.36 | ||
| Male | 28.1% (45) | 23.9% (60) | |
| Female | 71.9% (115) | 76.1% (191) | |
| Entropion, % (N) | 0.01a | ||
| Mild | 60.0% (96) | 47.8% (120) | |
| Moderate | 14.4% (23) | 16.3% (41) | |
| Severe | 25.6% (41) | 35.9% (90) | |
| Trichiasis Recurrence at 6 months, % (N) | 0.6% (1) | 2.0% (5) | 0.41 |
| Bilateral Surgery, % (N) | 76.3% (122) | 82.9% (208) | 0.13 |
| Level of Visual Impairment b, % (N) | <0.0001a | ||
| Mild/No Visual Impairment | 74.8% (119) | 54.0% (134) | |
| Moderate/Severe Visual Impairment | 22.0% (35) | 29.8% (74) | |
| Blind | 3.1% (5) | 16.2% (40) |
test for trend
4 people missing baseline vision data
The mean improvement in the physical functioning score from baseline to 6 months was 2.08 units (Table 3). The percent of participants reporting no difficulty in physical functioning increased by 32.6%. The proportion of participants in the mild/no visual impairment category also increased, commensurate with the decreased proportion of people in the moderate/severe visual impairment and blind categories.
Table 3.
Vision and physical functioning score of trichiasis surgery patients at baseline and six months following surgery
| Baseline level of vision and functioning |
6 months after surgery: level of vision and functioning |
Change in vision and functioning |
|
|---|---|---|---|
| Level of Visual Impairmenta, % (N) | |||
| Mild/No Visual Impairment | 62.2% (253) | 70.8% (291) | 8.6% |
| Moderate/Severe Visual Impairment | 26.8% (109) | 23.6% (84) | −3.2% |
| Blind | 11.1% (45) | 5.6% (23) | −5.5% |
| Score of Physical Functioning | |||
| No difficulty, % (N) | 38.9% (160) | 71.5% (294) | 32.6% |
| Mean (SD) | 3.00 (3.02) | 5.09 (1.64) | 2.08 (2.63) |
| Median | 3.70 | 5.97 | 1.41 |
4 people missing baseline vision data
The change in mean physical functioning score from baseline to follow-up by level of visual impairment is presented in Table 4. Across all categories of visual impairment, physical functioning improved; the blind group had the biggest gain in physical function (3.30 ± 0.52 units).
Table 4.
Mean physical functioning score of trichiasis surgery patients at baseline and six months after surgery, by level of baseline visual impairment
| Mean (SD) Score of Physical Functioning |
Change in Mean (SD) Score of Physical Functioning b, c |
||
|---|---|---|---|
| Baselinea | 6 months | ||
| Baseline Level of Visual Impairment | |||
| Mild/No Visual Impairment | 3.93 (2.39) | 5.58 (1.02) | 1.66 (0.14) |
| Moderate/Severe Visual | 2.46 (2.91) | 5.02 (1.38) | 2.56 (0.27) |
| Blind | −0.93 (3.11) | 2.37 (2.36) | 3.30 (0.52) |
4 people missing baseline vision data
A positive change score indicates improvement in physical functioning
All change scores were statistically significantly different from zero (p<0.0001 by paired t-test)
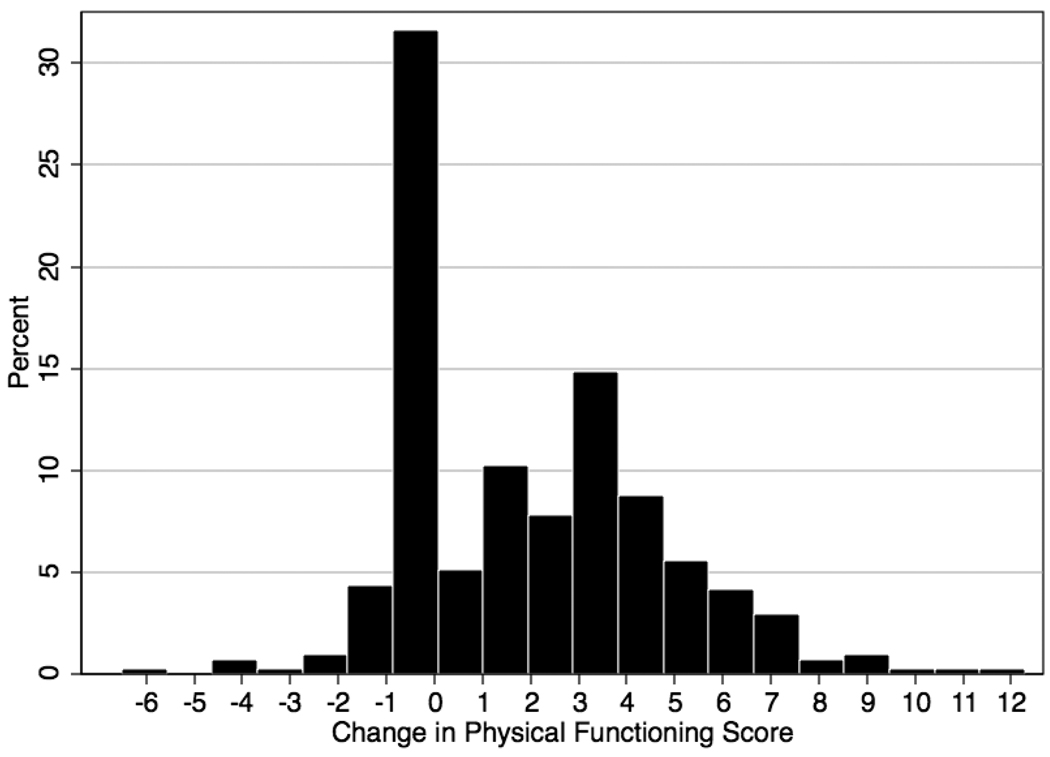
Figure 2 shows the distribution of the change in physical functioning scores. The distribution is bimodal with the first peak occurring at zero (those whose physical functioning scores did not change from baseline to follow-up). The second peak occurs at a score of 4, which is a significant improvement in physical functioning. The mean Rasch score showed significant change between baseline and follow-up (3.00 units vs. 5.09 units; p < 0.0001).
Figure 2.
Distribution of the change in Rasch scores of trichiasis surgery patients from baseline to six months after surgerya
a Paired t-test → p = <0.0001
Table 5 presents the characteristics of participants according to change in physical functioning. The reported physical functioning of the majority of individuals improved (61.8%), while it worsened for a small minority (7.1%). Of the individuals whose physical functioning stayed the same, the vast majority (N=122; 95.3%) reported no difficulty in physical functioning at baseline. Age, degree of entropion at baseline, and the mean change in logMAR differed significantly when comparing those who improved, stayed the same, or worsened in their physical functioning.
Table 5.
Characteristics of trichiasis surgery patients according to change in physical functioning six months after trichiasis surgery
| Physical Functioning | p-value | |||
|---|---|---|---|---|
| Improved | Same | Worse | ||
| Total Participants | 61.8% (254) | 31.1% (128) | 7.1% (29) | |
| Age (years), Mean (SD) | 49 (14) | 46 (13) | 54 (12) | 0.005 |
| Gender, % (N) | 0.155 | |||
| Male | 24.4% (62) | 30.5% (39) | 13.8% (4) | |
| Female | 75.6% (192) | 69.5% (89) | 86.2% (25) | |
| Baseline Entropion, % (N) | 0.047a | |||
| Mild | 47.6% (121) | 62.5 % (80) | 51.7% (15) | |
| Moderate | 16.5% (42) | 13.3% (17) | 17.2% (5) | |
| Severe | 35.8% (91) | 24.2% (31) | 31.0% (9) | |
| Trichiasis Recurrence by 6 months, % (N) | 2.0% (5) | 0.8% (1) | 0 | N/A |
| Bilateral Surgery, % (N) | 81.5% (207) | 77.3% (99) | 82.8% (24) | 0.605 |
| Mean (SD) change in logMAR of the eye with the maximum change in visionb | −0.243 (0.385) | −0.128 (0.293) | −0.136 (0.358) | 0.009 |
test for trend
4 people missing baseline vision data
A multivariate model including all participants was developed to predict change in physical functioning (Table 6). For a line of vision gained, physical functioning shows significant improvement (0.09 units; 95% CI: 0.02–0.16). In addition, for every line of vision worse in the better eye and for every unit physical functioning is worse, at baseline, physical functioning improves at follow-up (0.21 and 0.46 unit improvement, respectively). As baseline entropion severity increases, physical functioning improves follow-up (0.32 unit improvement, 95% CI: 0.04–0.60).
Table 6.
Multivariate linear regression model of factors predicting improvement in physical functioning in trichiasis patients 6 months after trichiasis surgery
| Characteristic | Coefficient (95% CI)a | p-value |
|---|---|---|
| Maximum change in VA | 0.09 (0.02–0.16) b | 0.013 |
| Baseline Entropion | 0.32 (0.04–0.60) c | 0.026 |
| Baseline logMAR in the better seeing eye | 0.21 (0.14–0.28) d | <0.001 |
| Baseline score of physical functioning | 0.46 (0.27–0.64) e | <0.001 |
adjusted for age and gender
Maximum change in VA: 0.09 unit improvement in physical functioning score per line of improvement in vision from baseline to six months
Baseline Entropion: 0.32 unit improvement in physical functioning score per increasing category of entropion severity
Baseline logMAR in the better eye: 0.21 unit improvement in physical functioning score per line of vision worse at baseline
Baseline score of physical functioning: 0.46 unit improvement in physical functioning score per unit of physical functioning worse at baseline
Discussion
Data from this study suggest that in addition to improving vision, trichiasis surgery can result in improvement in physical functioning at 6 months following surgery. Individuals with the most severe impairment at baseline showed the largest gains in physical functioning at six months after surgery. These individuals included those with severe entropion, worse baseline vision in the better eye and worse baseline physical functioning score.These cases clearly had the most to gain from surgical intervention, but we also observed improvement in functioning of cases in all other strata of baseline levels of acuity.
The improvement in physical functioning after trichiasis surgery shown in our study is consistent with an earlier study conducted in India, which showed that after surgery or epilation interventions for entropion and trichiasis, patients’ health-related quality of life improved.13 However, in that study visual acuity in the better eye did not improve, making the mechanism by which surgery improved quality of life less clear. The study only had 120 patients and may have been underpowered to detect differences in vision. Alternatively, only looking at visual acuity in the better eye may have led to overlooking some improvements in vision that did not affect the better seeing-eye. In addition, the majority of cases had entropion (which they defined as in-turning of the lid margin due to trachoma) and of the cases that had trichiasis, most had minor trichiasis. In that study, entropion was found to be less severe than minor trichiasis; participants with entropion in both eyes were found to have the same self-reported quality of life as participants with minor trichiasis in only one eye. Less severe disease may make it harder to detect the effects of any intervention because these individuals are likely to have less disability to begin with. Finally, the interventions conducted in the study varied from epilation for minor trichiasis to surgery for major trichiasis or entropion. 14 The quality and frequency of epilation was not recorded; as epilation lacks standardization and is dependent on individual ability and adherence, it might be less effective than surgery. The lack of effect of the interventions on vision could be partially explained by these differences.
We have previously shown that trichiasis surgery provides significant visual acuity improvement, as well as a decrease in subjective concerns of photophobia and pain.7 One of the interesting observations made in this study was the fact that change in vision, defined as the maximum change in vision when comparing the change in right and left eye, was the better measure of the impact of vision on physical functioning than using the change in vision between the better eye at baseline and the better eye at 6 months. Classically, it is felt that persons use their better eye for function, and that eye is the measure associated with any change in function.17 However, we reasoned that because trichiasis surgery results in an abrupt improvement in symptoms and in vision in the operated eye(s), that perhaps the maximum acuity gain in an eye might be more predictive of improvement in function in the short term than acuity gain in the better eye. Our findings suggest this approach was reasonable, and that gains in vision after trichiasis surgery could have a significant impact on functioning, at least in these tasks important for rural Ethiopian life.
The improvement in physical functioning was significantly greater if baseline levels of visual acuity or if baseline physical function was worse. In part, this may reflect the greater degree of improvement possible with worse functioning at baseline (i.e., those who start out with no difficulty at baseline can only do worse or stay the same). It may also indicate that surgery provides more perceptible gain to those who are most impaired in vision and function, and less perceived gain to those with mild impairment. Prior studies have shown the dependency of change in function on baseline function. In one study looking at self-reported quality of life in patients with cataracts assessed before and after cataract surgery, a greater magnitude of change in self-reported quality of life was seen with lower (poorer) baseline scores.15
This study has some limitations. First, we have attributed the observed improvement in physical function to trichiasis surgery. However, we did not have a cohort of trichiasis cases who did not undergo surgery for comparison; this would help account for possible natural improvements over time, or controlled for the Hawthorn effect (improvement that might be seen simply due to participants undergoing any intervention, unrelated to trichiasis alleviation). However, to randomize patients with trichiasis to observation in order to create a control group would have been unethical, since these patients are at high risk of vision loss. Others have used refusals of surgery, but we had no refusals to surgery, and refusals would be different from acceptors of surgery in ways that would bias the comparisons. While this is a possible limitation, we feel it is unlikely that this cohort of severe trichiasis cases would have experienced secular trends resulting in improved physical functioning over the 6-month period. Furthermore, the improvements in physical function in our study are related to improvements in visual acuity, the result of surgery. Thus, there appears to be a mechanism by which we would expect improvement in function to occur post-surgery, thereby strengthening our findings.
Second, the final physical functioning score includes a limited number of items. For example, a full quality of life scale such as the NEI –VFQ includes domains such as social roles and mental functioning.16 This may lead to overlooking certain aspects of physical functioning not included in the questionnaire or in the final score, in which changes may have occurred and thus result in an underestimate of the overall impact of trichiasis surgery. In addition, we did not measure quality of life because several other domains were not measured. However, creating a scale of social roles and mental functioning, which had meaning in rural Ethiopia, was beyond the scope of this study.
Third, the items in the questionnaire itself were basic to life, and key to functioning in a rural African setting, including walking, cooking, farming, etc. The wide variety of activities that characterize physical functioning in other settings, like driving a car, computer or cell phone use, etc. are not part of life in rural Africa. As such, the responses at baseline, even in patients with trichiasis, tended to show a ceiling effect. As expected, participants reporting no difficulty on any item would also largely report no difficulty in any item at follow up. This may have diminished our ability to detect changes that may have been observed if we had had many more items in the questionnaire.
Fourth, our findings present a relatively short-term effect of trichiasis surgery on physical functioning and it is unclear whether or not these effects persist over time. Other factors such as increasing infirmity in this older population or onset of other eye diseases would also be expected to impact functional status over time, and diminish our ability to detect any gains from surgery. We did observe 7.1% of participants who worsened in their functional score even over the 6-month period. Assessing functioning earlier than 6 months may not allow patients enough time to recover from and adjust to the changes resulting from surgery. Thus we feel that six months was a reasonable time for assessment.
In summary, a previous study conducted in Tanzania noted that trichiasis was associated with functional limitation in daily activities of village life, when comparing trichiasis patients to those without trichiasis.8 The next step was to determine if some functional loss can be restored with surgical intervention. This study suggests that improvements in physical functioning can be seen 6 months post-trichiasis surgery, in association with improvements in vision after surgery. Our findings reinforce the importance of trichiasis surgery as part of the SAFE strategy for trachoma control, and go further to suggest that the benefit of trichiasis surgery goes beyond prevention of vision loss to recovery of vision and recovery of physical function.
Acknowledgements
A. Funding/Support:
This study was funded by grant EY01387 and EY01765 from the National Eye Institute. Dr West is the recipient of a Senior Scientific Investigator award from Research to Prevent Blindness. Dr. Gower is the recipient of an Ernest and Elizabeth Althouse Special Scholars award from Research to Prevent Blindness.
E. Other Acknowledgements
The STAR Clinical Trial team who collected the data, and the patients who participated in this study.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures
B. Financial Disclosures:
None
C. Contributions of Authors:
Design and conduct of the study (EG, WA, BM, SW)
Collection, management, analysis, and interpretation of the data (MW, SC, EG, BM, JW, WA, SK)
Preparation, review, or approval of the manuscript (MW, SC, EG, BM, JW, WA, SK)
D. Statement about Conformity with Author Information:
All procedures and protocols for this study were reviewed and approved by the Johns Hopkins Medicine Institutional Review Board (JHM-IRB) and the Ethiopian Science and Technology Commission (ESTC).
Clinical Trial Registration: www.clinicaltrials.gov— Identifier: NCT00347776
References
- 1.Resnikoff S, Pascolini D, Etya’ale D, et al. Global data on visual impairment in the year 2002. Bull World Health Organ. 2004;82(11):844–851. [PMC free article] [PubMed] [Google Scholar]
- 2.Mariotti S, Pascolini D, Rose-Nussbaumer J. Trachoma: global magnitude of a preventable cause of blindness. Br J Ophthalmol. 2009;93:563–568. doi: 10.1136/bjo.2008.148494. [DOI] [PubMed] [Google Scholar]
- 3.West SK. Trachoma: new assault on an ancient disease. Prog Retin Eye Res. 2004;23(4):381–401. doi: 10.1016/j.preteyeres.2004.04.001. [DOI] [PubMed] [Google Scholar]
- 4.Berhane Y, Worku A, Bejiga A. National Survey on Blindness, Low Vision and Trachoma in Ethiopia. Addis Abeba, Ethiopia: Federal Ministry of Health of Ethiopia; 2006. [Google Scholar]
- 5.Adamu Y, Alemayehu W. A randomized clinical trial of the success rates of bilamellar tarsal rotation and tarsotomy for upper eyelid trachomatous trichiasis. Ethiop Med J. 2002;40(2):107–114. [PubMed] [Google Scholar]
- 6.Reacher MH, Munoz B, Alghassany A, Daar AS, Elbualy M, Taylor HR. A controlled trial of surgery for trachomatous trichiasis of the upper lid. Arch Ophthalmol. 1992;110(5):667–674. doi: 10.1001/archopht.1992.01080170089030. [DOI] [PubMed] [Google Scholar]
- 7.Woreta TA, Munoz BE, Gower EW, Alemayehu W, West SK. Effect of trichiasis surgery on visual acuity outcomes in Ethiopia. Arch Ophthalmol. 2009;127(11):1505–1510. doi: 10.1001/archophthalmol.2009.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Frick KD, Melia BM, Buhrmann RR, West SK. Trichiasis and disability in a trachoma-endemic area of Tanzania. Arch Ophthalmol. 2001;119(12):1839–1844. doi: 10.1001/archopht.119.12.1839. [DOI] [PubMed] [Google Scholar]
- 9.West ES, Alemayehu W, Munoz B, Melese M, Imeru A, West SK. Surgery for trichiasis, Antibiotics to Prevent Recurrence (STAR) Clinical Trial Methodology. Ophthalmic Epidemiol. 2005;12(4):279–286. doi: 10.1080/09286580591005769. [DOI] [PubMed] [Google Scholar]
- 10.West S, Mariotti SP, Bedri A, Melese M, West E. Certification for Trichiasis Surgery Using the Bilamellar Tarsal Rotation Procedure. Geneva, Switzerland: WHO; 2004. [Google Scholar]
- 11.West SK, West ES, Alemayehu W, et al. Single-dose azithromycin prevents trichiasis recurrence following surgery: randomized trial in Ethiopia. Arch Ophthalmol. 2006;124(3):309–314. doi: 10.1001/archopht.124.3.309. [DOI] [PubMed] [Google Scholar]
- 12.West ES, Munoz B, Imeru A, Alemayehu W, Melese M, West SK. The association between epilation and corneal opacity among eyes with trachomatous trichiasis. Br J Ophthalmol. 2006;90(2):171–174. doi: 10.1136/bjo.2005.075390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Massof RW. Application of Stochastic Measurement Models to Visual Function Rating Scale Questionnaires. Ophthalmic Epidemiol. 2005;12(2):103–124. doi: 10.1080/09286580590932789. [DOI] [PubMed] [Google Scholar]
- 14.Dhaliwal U, Nagpal G, Bhatia MS. Health-Related Quality of Life in Patients with Trachomatous Trichiasis or Entropion. Ophthalmic Epidemiol. 2006;13(1):59–66. doi: 10.1080/09286580500473803. [DOI] [PubMed] [Google Scholar]
- 15.Rosen PN, Kaplan RM, David K. Measuring outcomes of cataract surgery using the Quality of Well-Being Scale and VF-14 Visual Function Index. J Cataract Refract Surg. 2005;31(2):369–378. doi: 10.1016/j.jcrs.2004.04.043. [DOI] [PubMed] [Google Scholar]
- 16.Mangione CM, Berry S, Spritzer K, Janz NK, Klein R, Owsley C, Lee PP. Identifying the content area for the 51-item National Eye Institute Visual Function Questionnaire. Arch Ophthalmol. 1998;116(2):227–233. doi: 10.1001/archopht.116.2.227. [DOI] [PubMed] [Google Scholar]