Summary
Paediatric obesity continues to be one of the most important health issues facing children and families today, and there remains a need for effective treatment options. There are a few reports in the literature demonstrating high rates of attrition from paediatric weight management programmes, ranging from 27% to 73%. While some studies show that racial/ethnic minorities, the economically disadvantaged and those with higher levels of obesity are at risk, other studies do not. There is some consistency in reasons given by families for attrition from treatment, most often scheduling issues and programmes not meeting family needs or expectations. This review highlights identified contributors to attrition from paediatric weight management and provides a framework to study this problem, based on models of adherence to paediatric medical regimens.
Keywords: attrition, obesity, paediatric, treatment
Introduction
Nationally representative data from 2003 to 2006 estimate 16.3% of children and adolescents are obese (1,2). This is a remarkable increase from just 10 years earlier in which 11% of children and adolescents were obese (3), which itself was an increase from previous cycles of the survey (1976–1980). This trend is serious, because paediatric obesity substantially increases the risk of later morbidity and mortality, primarily from cardiovascular disease and diabetes (4). Many weight-related comorbidities, such as diabetes, sleep apnoea and pseudotumour cerebri, begin in childhood (5–8). Furthermore, obesity can significantly impact the quality of life of children (9).
Despite increasing interest, few ‘real world’ interventions are available to families or to clinicians searching for better treatment modalities for paediatric obesity (10). Fortunately, hospitals and communities are establishing obesity treatment programmes for children and adolescents, which often involve multidisciplinary teams and long-term follow-up. Unfortunately, approximately half of participating families drop out of treatment. A European study reported over 90% of children dropped out of treatment over a 2-year period (11). While there is a need for efficacious and efficient treatment, such significant attrition must be addressed; even with effective programmes, a child's weight will not improve if he or she drops out of treatment.
This review will survey the literature of attrition from paediatric obesity programmes and identify future areas of research. We searched Medline for English-language studies of attrition from paediatric weight management programmes, and paediatric weight management/obesity treatment trials that reported attrition data in their study. We considered studies published between 2000 and 2010.
Treatment of paediatric obesity
Research conducted in the 1980s and 1990s outlined effective therapies for paediatric obesity, primarily behavioural interventions including the primary parent or caregiver in treatment (12,13). This success has been difficult to reproduce in diverse healthcare settings, as evidenced by the scarcity of available treatment clinics and programmes and the call for more interventional work (10). Epstein, in summarizing a reanalysis of his work in paediatric obesity, called for studying the translation of this work into clinical practice (14). There appears to be increasing interest in evidence-based interventions, with paediatric centres quickly developing such programmes (15). Three-quarters of children's hospitals had obesity-related services; over half of paediatric obesity programmes had been developed in the previous 5 years, with many being supported by grant funding. However, the lack of reimbursement by insurers is a disincentive for primary- and subspecialty-care providers to focus on treatment.
The American Medical Association, in collaboration with the Centers for Disease Control and Prevention and the Department of Health and Human Services, brought together experts in the field to provide recommendations on the assessment, prevention and treatment of childhood obesity (16–19). These expert recommendations outlined a stepwise approach, beginning with an expanded office-based prevention model, focusing on healthy lifestyle habits, progressing to structured weight management, comprehensive intervention and tertiary-care referral.
As an intervention increases in intensity, so does cost, from increased contact time with families, need for additional staff, advanced weight management training and specialized facilities. It is unlikely these expenses will be recouped from normal billing practices (20), and many programmes subsidize costs. The time commitment for families and healthcare professionals is significant. Epstein's interventions varied from 15 to 20 sessions (usually with weekly sessions) (14). Clinical programmes vary between intense, short-term interventions (12 weeks) (21), longer treatments (6 months to a year) (22,23) and open-ended clinical programmes (24).
The profound investment of time and money in weight management, by both healthcare institutions and families, is wasted if families do not complete treatment. Because behavioural change is slow and cumulative, sporadic and temporary participation is unlikely to result in long-term health benefits. In addition, a missed appointment in a multidisciplinary clinic could cause up to 3 hours of lost professional time (e.g. if the family was scheduled for successive 1-hour visits with a dietitian, counsellor and exercise specialist). When reimbursement is already marginal or non-existent, early dropout from treatment compounds programmatic financial losses. Overall, attrition is a significant problem on multiple levels in the treatment of paediatric obesity.
Attrition from clinical obesity treatment programmes
We found very few studies or reports of attrition from paediatric weight management programmes. Six studies primarily investigated attrition, and an additional four studies of programme outcomes reported details of attrition (Table 1). Studies defined and studied attrition variably, but overall, dropouts were defined as not completing an initial phase of a treatment programme (4–5 months) (23,25,26) or failure to return to a weight management clinic (27–29).
Table 1.
Attrition rates in outpatient paediatric weight management programmes
| Study | n | Duration | Attrition | Variables significantly associated with dropout | Not associated with dropout |
|---|---|---|---|---|---|
| Barlow, Ohlemeyer 2006 (27) | 157 | Open-ended | 61% | Higher BMI Presence of obesity-related medical condition (P = 0.06) |
Race/ethnicity Age of child Single- or dual-parent household |
| Cote et al. 2004 (25) | 12 | 12 weeks | 55% (64% total) | Poorer caregiver-rated overall health status of child Lower caregiver-rated quality of care* Medicaid insurance† |
Race* Income* Education* Gender* Age* Health status of child† Percentage over ideal body weight* |
| Denszer et al. 2004 (30) | 294 | Open-ended | 62% by fourth visit | Higher body mass index standard deviation scores (BMI-SDS) associated with more visits in programme | Weight change (reduction in BMI-SDS) Age Gender Regular counselling by dietitian (8-week intervals) |
| Heinberg et al. 2009 (33) | 162 | 12 weeks | 27% (early dropouts and infrequent attenders) | African–American race Higher baseline BMI |
Age Gender |
| Kirk et al. 2005 (23) | 394 | 5–6 months | 55% | Not reported | Not studied |
| Kitscha et al. 2009 (28) | 152 | 6–12 months | 33% | Telephone interview. Major reasons for non-returns: physical barriers (scheduling, parking, location), clinic environment, programme content | |
| Skelton et al. 2008 (24) | 248 total | 9–12 months | 73% | None | Age of child Gender Race/ethnicity Insurance type (Medicaid, HMO, Commercial) Single- or dual-parent household |
| Sothern et al. 2002 (21) | 93 | 12 months | 39% | Not reported | Not reported |
| Tershakovec, Kuppler‡ 2003 (20) | 518 | Open-ended | 49% | African–American race | Gender BMI z-score Insurance |
| Zeller et al.§ 2004 (26) | 212 | 16 weeks | 55% | African–American race* Medicaid* Single parent household Older age (patient)* Higher BMI/BMI z-scores Higher fasting insulin Lower triglyceride and cholesterol Depressive symptoms* School maladjustment Lower self-concept Externalizing behaviour Disruptive behavioural symptoms |
Gender Systolic and diastolic blood pressure measurements High-density lipoprotein and low-density lipoprotein cholesterol Travel distance to clinic Clinical maladjustment Personal maladjustment Internalizing behaviour Adaptive behaviour Caregiver's current psychological symptom status |
By multivariate and bivariate analysis.
By multivariate analysis only.
Patients with indemnity insurance had more clinic visits than patients with managed care.
Multivariate analysis candidate predictors chosen by statistical significance (P < 0.05) and clinically meaningful.
HMO, Health Maintenance Organization.
Three studies (Cote, Kirk, Zeller) from the same midwestern programme report attrition rates of 55% (23,26) and 64% (25) (of 120 participants, 55% dropped out; the 64% attrition rate reflects all patients seen during the study period). The studies by Cote (service quality and attrition) and Zeller (predictors of attrition) focused on attrition. Different sample sizes are reported for each study because of differing study criteria, but all are from January 1998 to November 2002 (personal communication). Attrition was assessed for the initial 3- to 5-month phase of treatment (total treatment time of 1 year). There were slight differences in predictors of attrition; e.g. African–American race was a predictor in Zeller's study but not in Cote's, likely because of different inclusion criteria, sample sizes and objectives. Zeller's study isolated familial factors that would impact participation in intensive behavioural modification (e.g. poor, single parent, severe obesity in the child, behavioural symptomatology). The study by Cote focused on programmatic factors, such as perceived quality of care and satisfaction experienced by the patient and family, with dropouts rating care as lower in quality, as measured by the Consumer Assessment of Health Plan Study (CAHPS 2.0). Levels of satisfaction were explored with the 66 parents who reported reasons for dropping out. Approximately 25% reported that the programme failed to meet their expectations. Over half had difficulty with insurance coverage, and half said the child desired to leave the programme. Most families showed interest in re-engaging in the programme; help with insurance problems was the most common request to facilitate returning. Other common themes for facilitating returning to treatment were: reminder phone calls, flexibility of appointment or scheduling and better engagement of the child in treatment.
An Italian study focused on compliance with treatment and the impact on outcomes, with clinic attendance as the measure of compliance (30). This programme scheduled clinic visits every 8 weeks after an initial assessment with a paediatrician and specially trained dietitian. The goal was 1–2 kg of weight loss each month. Approximately 30% of participants dropped out between each visit, with only 38% remaining in treatment by the fourth visit. Stepwise regression analysis found body mass index standard deviation scores (BMI-SDS) were the only significant contributor to dropout (those with a higher baseline BMI-SDS were more likely to drop out). Further, initial weight loss also did not impact dropout from treatment.
The study by Barlow and Ohlemeyer also focused on attrition. Patients attended the multidisciplinary weight management clinic monthly for individual visits with care providers; duration of treatment was open-ended, modelled on a subspecialty clinic (personal communication). One-third of families dropped out after the initial visit, and 60.5% overall were considered ‘non-returners.’ (27) Higher BMI z-score and presence of a weight-related comorbidity (P = 0.06) predicted return to treatment, whereas demographic determinants (e.g. race/ethnicity, age of child and single-parent households) did not. Barlow also surveyed participants who dropped out (n = 85 surveyed out of 95 non-returners). Most commonly, families (33%) reported the programme was ‘not what we are looking for’. Other commonly cited reasons were: child would miss too much school (28%), programme too far from home (23%), scheduling conflicts (21%), insurance does not cover care (21%), child not ready to make change (16%), visits not frequent enough (12%), visits too frequent (7%) and family not ready to make change (5%). Caucasian families were more likely than African–American families to report the programme was too far away and was not what they were looking for, as were families with two parents in the household.
Kitscha et al. conducted a qualitative telephone survey of 21 parent/caregivers who did not return to a paediatric weight management programme featuring exercise and nutrition therapy led by a dietitian (28). The major reasons given for non-return were: physical barriers (scheduling, parking, location), organizational barriers (environment of clinic) and educational content of the programme (educational tools, focus on individual rather than family, exercise interventions). Parent/caregivers recommended greater emphasis on physical activity within appointments, a family-centred approach, interactive learning environments, age-appropriate information for children and parenting support.
The sixth and final study of attrition from paediatric obesity treatment programmes came from a northeastern children's hospital also featuring a multidisciplinary programme with monthly visits in a clinic setting (29). In this study, Tershakovec and Kuppler defined dropout as not returning to clinic after the initial assessment and first intervention visit. They reported similar levels of attrition at 49%. Disproportionately more African–Americans dropped out compared with other racial/ethnic groups. Gender, BMI z-score and insurance coverage (commercial, Medicaid) were not predictive of dropout. Additionally, there was a significant association between children with indemnity insurance coverage and total number of visits; children with indemnity coverage had more clinic visits than those with commercial managed care insurance, but that significance was borderline when race/ethnicity was added to the analysis.
Attrition rates have been reported in other weight management programmes, but without detailed evaluations. The Committed to Kids intervention for obese adolescents (13–17 years) is a year long, multidisciplinary programme that varies in intensity and focus (21). In one report of outcomes, 56 out of 93 participants completed a year of treatment, with an attrition rate of 39%. This intensive programme featured medical supervision, medical nutrition therapy (hypocaloric diets), nutrition education, exercise therapy, activity education and behaviour modification. Earlier reports of this programme's success, carried out as an interventional study, had 100% of families participating in 10-week and in 1-year evaluations (31); subsequent reports stated that 33% of participants dropped out (most between 6 and 9 months) (32). There were no indicators of why these different outcomes were found; no analyses of differences between dropouts and completers were included.
Our preliminary analysis of a mid-western multidisciplinary, outpatient referral programme had even higher attrition, with 73% (182 out of 248) of families dropping out before completing five or more visits over 9 months (24). Limited predictor variables (race/ethnicity, BMI z-score, age, insurance coverage, gender and single vs. dual-parent household) were analyzed, with no significant differences between completers and dropouts.
Finally, Heinberg et al. investigated parental factors impacting BMI change in children attending a paediatric obesity treatment programme (33). Nearly 10% of participants did not return after enrolment or dropped out by the fourth session, and an additional 21% attended less than 50% of sessions. A total of 104 participants completed the study after 143 began the intervention (27% attrition). Families of children with higher BMIs were less likely to enrol, drop out after enrolment, or attend sessions infrequently, as were African–Americans.
In summary, from the existing literature, there are no clear answers on: which families are at risk of dropping out of weight management programmes, the factors contributing to dropout and what changes might improve retention. Studies that reported racial/ethnic differences between dropouts and completers found that African–American participants were more likely to drop out (26,29,33). Similarly, children with higher BMIs (26,27,30,33), weight-related comorbidities (25–27) and significant psychosocial and behavioural stressors (26) were more likely to drop out, but this finding was not consistent. Across several studies, 25–50% of participants dropped out after the initial visit (24,26,27,29,30). The reasons for this are not known, but could include lack of motivation in participating families, loss of motivation during the treatment process, or dissatisfaction with treatment approaches.
Three studies, reviewed earlier from different programmes, asked participants who dropped out why they did not return (25,27,28). Across studies responses ranged from: the significant time commitment involved in treatment, requiring missed work and school, cost and lack of insurance coverage, appointment times and schedule and educational content. The few studies that investigated family dissatisfaction with treatment (25,27,28) drew no clear conclusions; programmes differed in approach, and many participants expressed a desire or willingness to return to treatment. No studies have examined these issues prospectively, which limits interpretation. As most studies were retrospective, the lack of associations with key variables could be due to lack of statistical power. Most importantly, there is an urgent need to study the interaction of families with treatment programmes to determine what contributes to dropout.
Are controlled trials any better?
The most recent Cochrane Systematic Review on obesity interventions in children reported that attrition rates in paediatric weight management trials ranged from 0% to 42% (34). Determinants of attrition are not discussed or highlighted, aside from drug trials having higher dropout and discussion of intention-to-treat analysis in the studies. Further, reports of clinical programmes are excluded in this Cochrane report, as retrospective data would not be included in systematic reviews. Below, we highlight paediatric trials with details of dropout (Table 2). While the primary focus of these studies was not attrition, some findings are related to reported attrition rates.
Table 2.
Attrition in paediatric obesity treatment studies
| Study | n | Study description | Attrition | Comments |
|---|---|---|---|---|
| Ebbeling et al. 2003 (45) | 16 | Randomized controlled trial comparing low-glycemic index diet vs. energy restricted, low-fat diet, aged 13–21 years, 6 month individual session intervention and 6-month follow-up | 12.5% | Small but well designed RCT with process evaluation and thorough study of outcomes No difference between control or intervention group, including attendance, with groups attending 9.4 ± 0.6 of the 12 planned sessions |
| Levine et al. 2001 (36) | 24 | Feasibility study of family-based intervention Families with children aged 8–12 years, 10–12 session, group behavioural intervention, three cohorts |
33% | Small study of family-based intervention following psychosocial factors, with no mention of study power No control group Dropout occurred early (mean of 2.3 ± 1.3 visits) No differences found between completers and dropouts aside from race (significantly more African–American, 67%, vs. Caucasian families, 22% dropped out, P = 0.05) Attrition highest in first cohort (55%), decreased in second and third cohorts (17%, 22%) |
| Resnicow et al. 2000 (35) | 57 | Feasibility study using group sessions, weekly to twice weekly for 6 months, intervention focused on healthy behaviours using social cognitive theory, community-based, aged 11–17 years | 45% attrition rate 43% attendance at sessions 54% of participants classified as ‘low attenders’ |
Developmental study, no control group No differences between low attenders and high attenders aside from high-density lipoprotein cholesterol and diastolic blood pressure |
| Savoye et al. 2007 (37) | 209 | Parallel, randomized, controlled trial of group weight management programme vs. control (less intense intervention, every 6 months visit to outpatient clinic), twice weekly to every other week for 1 year, aged 8–16 years | Intervention: 18% at 6 months, 29% at 12 months Control: 26% at 6 months, 33% at 12 months |
Large, well-designed RCT with control group Adequately powered to assess weight outcomes Original randomization modified after 83% dropped out of structured meal planning at 6 months. No statistical differences in attrition rates among racial/ethnic groups |
| Schwartz et al. 2007 (38) | 91 | Feasibility study of motivational interviewing (MI) in primary care paediatric office with overweight children (body mass index 85th–95th percentile) 3–7 years of age Individual visits in 3-tier intervention: control (routine care), minimal (MD only with MI), intensive (MD, RD with MI) |
33% overall 10% in control 32% in minimal intervention 50% in intensive intervention |
True feasibility study with control group No differences between dropouts and completers in age, gender, body mass index percentiles |
RCT, Randomized Controlled Trial; MI, Motivational Interviewing; RD, Registered Dietitian.
The Go Girls Program (an activity and nutrition pilot study of teenage African–American girls) reported a 45% drop out rate, and children attended only 43% of sessions (35). Levine et al. conducted a family-based weight management programme with 24 families of obese children 8–12 years of age (36). One-third of families dropped out before completing treatment (10–12 sessions), and did so early in treatment.
Savoye et al. conducted a family-based weight management programme from 2002 to 2005 (37). This controlled trial initially randomized families 2:1 to a weight management or a control group, and 1:1 of two different interventions: structured meal planning or better food choices. The first 35 participants randomized to structured meal plans dropped out at a much higher rate in the first 6 months of the trial (83% attrition), and that arm of the study was closed. The intervention group reported 18% dropout at 6 months, and 29% at a year. Of note, the control group, which received clinical counselling for weight management every 6 months, had higher rates of attrition, 26% and 33% at 6 and 12 months, respectively (the percentage dropout at 12 months is cumulative over the total number of patients). In a primary care-based study utilizing motivational interviewing, 33% of participants did not complete the study, with no differences identified between dropouts and completers (38).
Overall, paediatric obesity treatment trials have dropout rates comparable to those of clinical weight management programmes. There also appear to be similar predictors of dropout, notably children with higher BMIs (11) and African–American participants (36). Similar is a pattern of participants dropping out early in the treatment process.
Adherence: a model for the study of attrition
Small, but excellent studies of attrition from paediatric weight management programmes have examined both families dropping out and the programmes themselves. Nonetheless, in-depth investigations of the interaction between families and treatment programmes are lacking, and are needed to create more effective therapies, particularly for the highest-risk patients.
There are many unique aspects of paediatric obesity. It is a relatively new problem, with the epidemic less than 25 years old, dealing with comorbidities typically seen only in adults. Treatment not only requires the support of parents and caregivers, but often involves the entire family; the problem is exacerbated by an unhealthy environment; and treatment is evolving from a diet and exercise approach to one involving behavioural therapies and possibly multidisciplinary teams. These factors likely contribute to the difficulty of retention of families in treatment, and should be included in theoretical models going forward.
Many chronic paediatric conditions require frequent contact with health care providers and adherence to complex treatment regimens. Although ‘attrition’ and ‘adherence’ are distinct, attrition can be viewed as an exaggerated form of non-adherence; the patient and family do not adhere to medical advice, and completely withdraw from treatment. Complicating this paradigm is the problem itself, which involves two behaviours – eating habits and physical activity – long proven difficult to change. Thus, models of adherence may offer insight into understanding attrition.
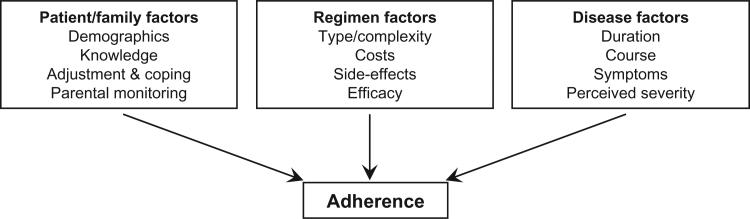
Rapoff provides a useful approach, including key stake-holders, families and treatment providers/programme, while recognizing the complex nature of the disease process (39). He conceptualized adherence to paediatric medical regimens, utilizing established theoretical models such as the Health Belief Model, to investigate correlates of adherence (Fig. 1). This model includes the family and disease and treatment regimen factors (39). Researchers have used this model to develop interventions addressing chronic paediatric diseases (40).
Figure 1.
Model of adherence to paediatric medical regimens. Adapted from Rapoff (39).
The family plays an important role in managing other chronic paediatric health conditions. Smith summarized adherence problems in chronically ill adolescents, highlighting the impact of mental health (depression, cognitive delays), medication regimens and the family – especially issues of poor communication, overall family conflict, parent involvement in treatment, family stress and support (41). Fiese and Everhart reviewed studies examining family factors affecting adherence to medical regimens in chronically ill children (42). Disruptive family interactions, characterized by conflict and disengagement, resulted in poor treatment adherence and child health. McQuaid investigated the transition of responsibility for asthma management from the parent to the child; with increasing age, the child's knowledge of their disease increased, but adherence to medication regimens did not, indicating the complex nature of family dynamics in children with chronic illnesses (43). Many similar issues are not typically measured in paediatric obesity interventions.
Rapoff's model suggests that the treatment programme itself plays a role in adherence. Disease-related correlates, such as duration, course of illness, symptoms and perceived severity, all impact a family's ability and willingness to adhere to treatment (39). Characteristics of treatment also influence adherence, e.g. complexity of treatment regimens, cost, side effects and efficacy. Overly complex treatment regimens are difficult to follow correctly. E.g. if parents think an expensive medication is not helping their child, they are less likely to administer it consistently. It is easy to relate these correlates of paediatric medical adherence to obesity treatment, where family factors influence the ability of a family to fully participate in an expensive, intensive programme resulting in modest weight loss or weight maintenance. The child may not exhibit symptoms of obesity, as hypertension and diabetes can often be asymptomatic in early stages. If multiple family members are obese, they may not feel the child's obesity needs attention. Finally, treatment of paediatric obesity is intensive, featuring numerous health and health-related disciplines, frequent visits and meetings, and necessitating participation of the entire family (16).
Rapoff's model provides an opportunity to address what is known from the existing studies of attrition. Simultaneously addressing the complexities of obesity and its treatment, the family, and the programmatic approach may yield exciting and hopefully effective new therapies. But why are these children and their families dropping out? Is it family or personal stress from obesity, poverty or another health disparity? And how do these factors affect participation and success in weight management? Programmatic determinants, such as cost, engagement with the child and satisfaction, also contribute to attrition. Again, approaching this issue broadly using Rapoff's model of adherence can provide the opportunity to match treatment, family and disease in innovative ways.
Summary and future directions
Unfortunately, most children who begin obesity treatment do not complete it. With few available treatment outlets, the problem is compounded by attrition, and is in need of further study. There is little in the literature upon which to base better treatment approaches. Available studies suggest a pattern of ‘severely’ affected children and their families dropping out, in the presence of comorbidities, higher BMI and behavioural issues. Further, vulnerable families seem to be at risk of dropping out (i.e. racial/ethnic minorities, poor and single-parent households), although these data are not definitive. There is some evidence that treatment is not meeting families’ expectations (content of the programme, help with insurance coverage or cost and engaging the child) or schedule (schedule of clinic visits, missed school and work). Despite the value of these studies to date, there is still much to be learned.
Because significant effort and resources are dedicated to obesity treatment programmes, clinics, community programmes and hospitals must maximize their investments. Rather than blaming the programme or the families, efforts should evaluate the interface between programme and family to determine why a programme successfully reaches one family, but others do not return even for a second visit. Similar in approach to other complex diseases – e.g. smoking cessation, diabetes control, or cancer therapies – the interaction of treatment and the patient is of great importance. The Chronic Care Model (44) has focused on this interaction as a means to maximize medical care, and is likely relevant to the problem of paediatric obesity treatment; however, obesity is a unique and complex disease. With many of those at risk of attrition, such as morbidly obese or racial/ethnic minorities, being from high risk or disparate groups, culturally-competent or individualized approaches are needed.
The study of adherence to medical regimens provides a useful approach to this problem, looking beyond familial factors to assess aspects of the disease and the treatment, to elucidate how these factors impact a child's adherence to a chronic treatment regimen. Researchers can use a similar approach, investigating the interaction of families and treatment programmes while accounting for the complex nature of obesity and its treatment. As reviewed here, there are many questions still to ask:
Do families drop out of treatment because of dissatisfaction with treatment, stressors within the family, or both?
How can treatment better fit into the lives of busy families?
With the diversity within families (single parents, blended families, dual-working parents), how can treatment programmes provide equally diverse treatment approaches?
How can treatment meet the needs of families in racial/ethnic minority groups, who are more severely affected by obesity, yet appear to be at greater risk of dropping out of treatment?
New and innovative approaches are a possible outgrowth of this study. Behavioural therapies that overcome barriers of time and schedule, such as home visits or internet-based video meetings, may provide a new arena for treatment. While parents and caregivers are key to treatment, engagement of the child also appears to contribute to dropout. Providing entertaining and engaging activities for children could improve compliance with clinic visits. The family stress and behavioural issues could be addressed through different approaches, such as increased support of family efforts or a dedicated approach to psychological management before or during obesity treatment. Customized and tailored approaches may not only prove successful with those at high risk of dropout, but could improve overall outcomes of treatment.
Researchers and clinicians must address these issues while undertaking the study and treatment of obese children and their families. Increasingly, children are living with chronic illness and interact with diverse medical specialties and professionals; study of attrition from paediatric obesity treatment may provide valuable information in these areas, even with efforts to prevent obesity. Further, improving the efficiency of treatment by minimizing attrition may have significant financial implications for hospitals and clinics. With increasing attention given to obesity and its treatment, the study of attrition should also receive increasing focus if effective therapies are to be developed and disseminated.
Acknowledgement
The authors would like to thank Karen Klein (Research Support Core, Office of Research, Wake Forest University Health Sciences) for providing helpful revisions of this manuscript.
Source of support: Supported in part by a grant from The Duke Endowment (No. 6110-SP).
Footnotes
Conflict of Interest Statement: The authors have no other financial disclosures to make.
References
- 1.Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 3.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101:497–504. [PubMed] [Google Scholar]
- 4.Dietz WH. Health consequences of obesity in youth: childhood predictors of adult disease. Pediatrics. 1998;101:518–525. [PubMed] [Google Scholar]
- 5.Dean HJ, Sellers EA. Comorbidities and microvascular complications of type 2 diabetes in children and adolescents. Pediatr Diabetes. 2007;8(Suppl. 9):35–41. doi: 10.1111/j.1399-5448.2007.00340.x. [DOI] [PubMed] [Google Scholar]
- 6.Lee WW. An overview of pediatric obesity. Pediatr Diabetes. 2007;8(Suppl. 9):76–87. doi: 10.1111/j.1399-5448.2007.00337.x. [DOI] [PubMed] [Google Scholar]
- 7.Stanley T, Misra M. Polycystic ovary syndrome in obese adolescents. Curr Opin Endocrinol Diabetes Obes. 2008;15:30–36. doi: 10.1097/MED.0b013e3282f41d55. [DOI] [PubMed] [Google Scholar]
- 8.Stevenson SB. Pseudotumor cerebri: yet another reason to fight obesity. J Pediatr Health Care. 2008;22:40–43. doi: 10.1016/j.pedhc.2007.05.004. [DOI] [PubMed] [Google Scholar]
- 9.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003;289:1813–1819. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 10.Robinson TN. Treating pediatric obesity: generating the evidence. Arch Pediatr Adolesc Med. 2008;162:1191–1192. doi: 10.1001/archpedi.162.12.1191. [DOI] [PubMed] [Google Scholar]
- 11.Pinelli L, Elerdini N, Faith MS, Agnello D, Ambruzzi A, De Simone M, Leggeri G, Livieri C, Monetti N, Peverelli P, Salvatoni A, Seminara S, Uasone R, Pietrobelli A. Childhood obesity: results of a multicenter study of obesity treatment in Italy. J Pediatr Endocrinol Metab. 1999;12(Suppl. 3):795–799. [PubMed] [Google Scholar]
- 12.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year follow-up of behavioral, family-based treatment for obese children. JAMA. 1990;264:2519–2523. [PubMed] [Google Scholar]
- 13.Epstein LH, Valoski A, Wing RR, McCurley J. Ten-year outcomes of behavioral family-based treatment for childhood obesity. Health Psychol. 1994;13:373–383. doi: 10.1037//0278-6133.13.5.373. [DOI] [PubMed] [Google Scholar]
- 14.Epstein LH, Paluch RA, Roemmich JN, Beecher MD. Family-based obesity treatment, then and now: twenty-five years of pediatric obesity treatment. Health Psychol. 2007;26:381–391. doi: 10.1037/0278-6133.26.4.381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Eneli IU, Patel D, Cunningham A, Hinton T, Stephens J, Murray R. Pediatric Obesity Programs in US Children's Hospitals. Pediatric Academic Societies; American Public Health Association; Honolulu, Hawaii: Washington, D.C.: 2008. 2007. [Google Scholar]
- 16.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl. 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 17.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl. 4):S229–S253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 18.Krebs NF, Himes JH, Jacobson D, Nicklas TA, Guilday P, Styne D. Assessment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl. 4):S193–S228. doi: 10.1542/peds.2007-2329D. [DOI] [PubMed] [Google Scholar]
- 19.Spear BA, Barlow SE, Ervin C, Ludwig DS, Saelens BE, Schetzina KE, Taveras EM. Recommendations for treatment of child and adolescent overweight and obesity. Pediatrics. 2007;120(Suppl. 4):S254–S288. doi: 10.1542/peds.2007-2329F. [DOI] [PubMed] [Google Scholar]
- 20.Tershakovec AM, Watson MH, Wenner WJ, Jr, Marx AL. Insurance reimbursement for the treatment of obesity in children. J Pediatr. 1999;134:573–578. doi: 10.1016/s0022-3476(99)70243-x. [DOI] [PubMed] [Google Scholar]
- 21.Sothern MS, Schumacher H, von Almen TK, Carlisle LK, Udall JN. Committed to kids: an integrated, 4-level team approach to weight management in adolescents. J Am Diet Assoc. 2002;102:S81–S85. doi: 10.1016/s0002-8223(02)90429-3. [DOI] [PubMed] [Google Scholar]
- 22.Hipsky J, Kirk S. HealthWorks! Weight management program for children and adolescents. J Am Diet Assoc. 2002;102:S64–S67. doi: 10.1016/s0002-8223(02)90423-2. [DOI] [PubMed] [Google Scholar]
- 23.Kirk S, Zeller M, Claytor R, Santangelo M, Khoury PR, Daniels SR. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005;13:876–882. doi: 10.1038/oby.2005.101. [DOI] [PubMed] [Google Scholar]
- 24.Skelton JA, Demattia LG, Flores G. A pediatric weight management program for high-risk populations: a preliminary analysis. Obesity. 2008;16:1698–1701. doi: 10.1038/oby.2008.243. [DOI] [PubMed] [Google Scholar]
- 25.Cote MP, Byczkowski T, Kotagal U, Kirk S, Zeller M, Daniels S. Service quality and attrition: an examination of a pediatric obesity program. Int J Qual Health Care. 2004;16:165–173. doi: 10.1093/intqhc/mzh015. [DOI] [PubMed] [Google Scholar]
- 26.Zeller M, Kirk S, Claytor R, Khoury P, Grieme J, Santangelo M, Daniels S. Predictors of attrition from a pediatric weight management program. J Pediatr. 2004;144:466–470. doi: 10.1016/j.jpeds.2003.12.031. [DOI] [PubMed] [Google Scholar]
- 27.Barlow SE, Ohlemeyer CL. Parent reasons for nonreturn to a pediatric weight management program. Clin Pediatr. 2006;45:355–360. doi: 10.1177/000992280604500408. [DOI] [PubMed] [Google Scholar]
- 28.Kitscha CE, Brunet K, Farmer A, Mager DR. Reasons for non-return to a pediatric weight management program. Can J Diet Pract Res. 2009;70:89–94. doi: 10.3148/70.2.2009.89. [DOI] [PubMed] [Google Scholar]
- 29.Tershakovec AM, Kuppler K. Ethnicity, insurance type, and follow-up in a pediatric weight management program. Obes Res. 2003;11:17–20. doi: 10.1038/oby.2003.4. [DOI] [PubMed] [Google Scholar]
- 30.Denzer C, Reithofer E, Wabitsch M, Widhalm K. The outcome of childhood obesity management depends highly upon patient compliance. Eur J Pediatr. 2004;163:99–104. doi: 10.1007/s00431-003-1376-7. [DOI] [PubMed] [Google Scholar]
- 31.Sothern MS, von Almen TK, Schumacher HD, Suskind RM, Blecker U. A multidisciplinary approach to the treatment of childhood obesity. Del Med J. 1999;71:255–261. [PubMed] [Google Scholar]
- 32.Sothern MS, Udall JN, Jr, Suskind RM, Vargas A, Blecker U. Weight loss and growth velocity in obese children after very low calorie diet, exercise, and behavior modification. Acta Paediatr. 2000;89:1036–1043. doi: 10.1080/713794562. [DOI] [PubMed] [Google Scholar]
- 33.Heinberg LJ, Kutchman EM, Lawhun SA, Berger NA, Seabrook RC, Cuttler L, Horowitz SM. Parent involvement is associated with early success in obesity treatment. Clinical Pediatrics. 2009;49:457–465. doi: 10.1177/0009922809337531. [DOI] [PubMed] [Google Scholar]
- 34.Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O'Malley C, Stolk RP, Summerbell CD. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009;(4):CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]
- 35.Resnicow K, Yaroch AL, Davis A, Wang DT, Carter S, Slaughter L, Coleman D, Baranowski T. GO GIRLS!: results from a nutrition and physical activity program for low-income, overweight African American adolescent females. Health Educ Behav. 2000;27:616–631. doi: 10.1177/109019810002700507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Levine MD, Ringham RM, Kalarchian MA, Wisniewski L, Marcus MD. Is family-based behavioral weight control appropriate for severe pediatric obesity? Int J Eat Disord. 2001;30:318–328. doi: 10.1002/eat.1091. [DOI] [PubMed] [Google Scholar]
- 37.Savoye M, Shaw M, Dziura J, Tamborlane WV, Rose P, Guandalini C, Goldberg-Gell R, Burgert TS, Cali AM, Weiss R, Caprio S. Effects of a weight management program on body composition and metabolic parameters in overweight children: a randomized controlled trial. JAMA. 2007;297:2697–2704. doi: 10.1001/jama.297.24.2697. [DOI] [PubMed] [Google Scholar]
- 38.Schwartz RP, Hamre R, Dietz WH, Wasserman RC, Slora EJ, Myers EF, Sullivan S, Rockett H, Thoma KA, Dumitru G, Resnicow KA. Office-based motivational interviewing to prevent childhood obesity: a feasibility study. Arch Pediatr Adolesc Med. 2007;161:495–501. doi: 10.1001/archpedi.161.5.495. [DOI] [PubMed] [Google Scholar]
- 39.Rapoff MA. Adherence to Pediatric Medical Regimens. 1st edn. Springer; New York: 1999. [Google Scholar]
- 40.Rapoff MA. Commentary: pushing the envelope: furthering research on improving adherence to chronic pediatric disease regimens. J Pediatr Psychol. 2001;26:277–278. doi: 10.1093/jpepsy/26.5.277. [DOI] [PubMed] [Google Scholar]
- 41.Smith BA, Shuchman M. Problem of nonadherence in chronically ill adolescents: strategies for assessment and intervention. Curr Opin Pediatr. 2005;17:613–618. doi: 10.1097/01.mop.0000176443.26872.6e. [DOI] [PubMed] [Google Scholar]
- 42.Fiese BH, Everhart RS. Medical adherence and childhood chronic illness: family daily management skills and emotional climate as emerging contributors. Curr Opin Pediatr. 2006;18:551–557. doi: 10.1097/01.mop.0000245357.68207.9b. [DOI] [PubMed] [Google Scholar]
- 43.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28:323–333. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 44.Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness: the chronic care model, Part 2. JAMA. 2002;288:1909–1914. doi: 10.1001/jama.288.15.1909. [DOI] [PubMed] [Google Scholar]
- 45.Ebbeling CB, Leidig MM, Sinclair KB, Hangen JP, Ludwig DS. A reduced-glycemic load diet in the treatment of adolescent obesity. Arch Pediatr Adolesc Med. 2003;157:773–779. doi: 10.1001/archpedi.157.8.773. [DOI] [PubMed] [Google Scholar]