Abstract
Purpose
To investigate the impact of worries on weight concerns and emotional eating and body mass index (BMI) percentile in an ethnically diverse sample of female youth.
Methods
This study uses baseline and follow-up data from a brief school-based physical activity intervention trial in minority female youth. Partial correlations adjusted for intervention status, age, and ethnicity were used to assess the relationship among emotional eating, weight concerns, and BMI percentile at follow-up. Multi-level modeling was used to analyze the relationships between baseline worries and follow-up emotional eating, weight concerns, and BMI percentile. Additional analysis assessed whether emotional eating mediated and/or moderated the relationship between baseline worries and follow-up BMI. Data were analyzed using SAS v9.1.
Results
The sample consisted of 404 minority females (67.1% Latina; mean age 12.5±0.6; 60.6% normal weight). Weight concerns were positively correlated with emotional eating and BMI percentile (p< 0.001 for both). Baseline worries significantly predicted emotional eating (p= 0.027) and weight concerns (p< 0.001) but not BMI percentile (p= 0.183) at follow-up. Emotional eating did not mediate the relationship between baseline worries and follow-up BMI percentile; however it did moderate the relationship between baseline worries and follow-up BMI percentile (p= 0.003).
Conclusions
Worries were associated with psychosocial variables but not BMI percentile in this sample. Reducing worries in those with high emotional eating scores may influence future weight gain in Latina females.
Keywords: psychosocial, minority, youth, BMI, weight concerns, emotional eating, mediation, moderation
INTRODUCTION
Obesity in the adolescent population has reached epidemic proportions in the United States, with ethnic minorities the most affected group [1]. Recent data from the National Health and Nutrition Examination Survey indicate that 38.7% of non-Hispanic Blacks and 41.8% of Latinos ages 6–19 have a body mass index (BMI) ≥ 85th percentile [2]. In addition to having high rates of obesity, minority female youth are among the most sedentary groups in the United States [3] and have diets high in sugar that affect adiposity [4], putting them at increased health risk [5].
The majority of obesity interventions in youth have focused on modifying diet intake and/or levels of physical activity. However, diet and physical activity only partially account for obesity risk [6], thus contributions from other variables should be explored. Obesity has been shown to be associated with worse psychosocial functioning in youth [7]. Psychosocial variables may be important targets for obesity prevention because of their potential as modifiable mediators/moderators [8], and have been shown to impact obesity as well as obesity-related behaviors in youth [9]. However, these types of variables have been not been extensively studied in minority youth. Weight concerns and worries are examples of psychosocial variables that may impact weight status in this population.
There is some evidence indicating that weight concerns are positively associated with weight status in minority youth [10]. Haines et al. found that increased weight concerns were predictive of increased BMI in a longitudinal study of ethnically-diverse female youth [11]. Furthermore, weight concerns are pervasive, particularly in females, and can precede rather than result from obesity.
The construct of worries is a related psychosocial variable that encompasses weight concerns but covers a broader range of hassles. Worries, defined as “a chain of thoughts negatively affect-laden and relatively uncontrollable,” [12] have not been extensively studied in youth. Limited findings associate worries with poor sleep patterns, health complaints, and decreased psychological well-being in youth [13]. However, worries are conceptually distinct from related constructs such as generalized anxiety in that they focus on the perceived exposure to stressors and inner concerns [14]. Appearance-related worries have been related to other psychosocial constructs, such as emotional eating in youth [15].
Emotional eating stems from psychosomatic theory [16] which posits that humans use food as an emotional defense when faced with negative affect. Emotional eating is associated with increased fatty food intake [17] and higher BMI [18] in adults, however few studies have investigated the relationship between emotional eating and BMI in youth. Snoek et al. found no association between emotional eating and BMI in a sample of White female youth [19]. Conversely, Braet et al. reported that overweight females had higher emotional eating scores than normal weight females [20]. However, Nguyen-Rodriguez et al. found that emotional eating scores did not differ between normal weight and overweight minority youth [21]. Despite limited research, the findings have been conflicting and little research has focused on this construct in Latina youth, leaving a gap in the literature on psychosocial factors related to obesity in this population.
This study aims to elucidate the relationship between worries, emotional eating, weight concerns, and BMI in an ethnically diverse sample of females using two repeated measures taken six months apart. To our knowledge, no previous study has investigated whether emotional eating mediates or moderates the relationship between worries and BMI percentile in minority youth. We propose that the relationship between worries and weight status is influenced by emotional eating in this sample such that worries are associated with increased emotional eating, which is associated with increased BMI percentile. In addition, we aim to investigate the direct effect of worries on emotional eating, weight concerns, and BMI percentile. We propose that worries will be positively associated with emotional eating scores as youth may be more likely to eat when faced with generalized worries. Furthermore, worries may be related to health concerns, of which weight concerns is an example. Worries may also directly impact BMI percentile because increased negative affect has been associated with higher BMI percentile [22]. The main hypotheses are that (1) baseline worries will be associated with follow-up BMI percentile, emotional eating, and weight concerns; (2) the effect of baseline worries on follow-up BMI percentile will be mediated or moderated by emotional eating; and (3) follow-up BMI percentile, emotional eating, and weight concerns will be correlated.
METHODS
Participants & Procedures
Participants were recruited from seven middle schools in Los Angeles to participate in a physical activity intervention trial [23]. Baseline data collection took place in the fall prior to the intervention trial with those students who gave active personal assent and active parental consent, or whose parents did not give active refusal. By the third day of recruitment, if students were unable to provide active consent of the parents but did provide written personal assent, they were allowed to complete an abbreviated form of the survey if parents did not actively refuse participation. Students with passive parental consent filled out an abbreviated version of the survey. This consent procedure allows for maximum participation in the survey. Follow-up data were collected approximately six months later in the spring semester at one month post-intervention. All procedures were approved by the University of Southern California Institutional Review Board as well as the school districts and Archdiocese.
Trained data collectors administered the questionnaire using scripts and a manual of procedures in order to standardize the collection technique. Students in the 6th – 8th grades filled out a confidential psychosocial questionnaire (identified only by a unique ID number) that assessed dietary and physical activity habits. Height and weight measurements were taken by trained data collectors on all study participants.
At baseline, 207 male and 459 female students completed surveys. Because this study was developed to understand weight concerns and related behaviors in populations of predominantly Latina females, this analysis focused on females only. Of the 459 females with baseline data, 35 were excluded because they were categorized as underweight, and 20 were excluded due to missing data. Thus, 404 female participants were included in this analysis, of which 27% took part in the physical activity intervention.
Instruments
Worries
Worries were assessed using a 19-item scale [14]. Participants were asked how much they worried about items in the previous month. Items related to several issues pertinent to adolescent life including self-image, relationships, and school. Examples of items are: “My future” and “My family or friends health”. Answer categories were on a four-point Likert scale: “I never worry about this”, “I worry about this a little”, I worry about this sometimes”, and “I worry about this a lot”. The mean score of the items was used to determine how worried the participants felt. Cronbach’s alpha for this scale at baseline was 0.87.
Emotional Eating Scale
Emotional eating was assessed using the 13-item Emotional Eating subscale of the Dutch Eating Behavior Questionnaire (DEBQ) [24]. The questions prompted the participants to “think about how you usually feel before you start eating” and to check the answer that matches how often the participant agreed with that behavior. Examples of the behavior items are: “Nothing to do” and “Something unpleasant happens”. Responses were rated on a five-point Likert scale: “never”, “rarely”, “sometimes”, “often”, and “very often”. The mean score of all the items was used to assess emotional eating and Cronbach’s alpha for this subscale at follow-up was 0.94.
Weight Concerns
A seven-item weight concerns scale was used to assess how much participants worried about or felt negatively/positively about their body or looks [25]. The questions asked, “In the past year how often have you…” and then provided seven items. Examples of the items are: “Thought about wanting to be thinner” and “Weight made difference in how you feel about yourself”. Responses were rated on a four-point Likert scale: “never”, “sometimes”, “often”, and “very often”. The mean score of all the items was used to assess weight concerns and the Cronbach’s alpha for the scale at follow-up was 0.79.
Weight Status
BMI (kg/m2) was calculated using weight (in kg) and height (in cm) measured by the Tanita body composition analyzer (TBF-300A) and a stadiometer, respectively. In order to take into account age and gender during childhood when growth is still occurring, BMI percentile was calculated with SPSS code from the Centers for Disease Control and Prevention (CDC) [26]. The age- and gender- specific thresholds for weight status are as follows: normal-weight is defined as 5th to <85th percentile, overweight is defined as between the 85th to <95th percentile, and obese is defined as ≥95th percentile.
Demographic Variables
Age (in years) was determined from the school records. An ethnicity scale was used to assess ethnic background [27]. Participants were asked to “mark all that apply” for the ethnicity categories and those that checked more than one category were considered “Multi-ethnic”. The original scale had 10 categories that later were collapsed into 5 categories for the regression analysis: Latina, Multi-Ethnic, Asian/Pacific Islander, White and Other.
Data Analysis
Data collected at baseline and follow-up were used in the analyses to establish time precedence. Only female participants with complete data were included (N= 404). Complete data was defined as having non-missing demographic, BMI percentile, and psychosocial data for both baseline and follow-up. Means and frequencies were calculated to describe the study sample. Intervention status was controlled for in all analyses. Partial correlations controlling for age, and ethnicity were used to determine the associations between the independent and multiple dependent variables. Paired t-tests were used to provide descriptive information on baseline and follow-up scores for emotional eating, weight concerns, and BMI percentile.
Figure 1 presents the model tested in this analysis. To control for effect students nested within schools, multi-level modeling was used to test the predictive relationship between baseline worries scores and follow-up BMI percentile, emotional eating, and weight concerns. Baseline worries was the independent variable in all models while school was treated as a class-level variable with a random intercept and the test visit (baseline or follow-up) was treated as a repeated measure with unstructured covariance. School intervention status, age, and ethnicity were included as covariates in all regression models given precedence in the literature.
Figure 1.
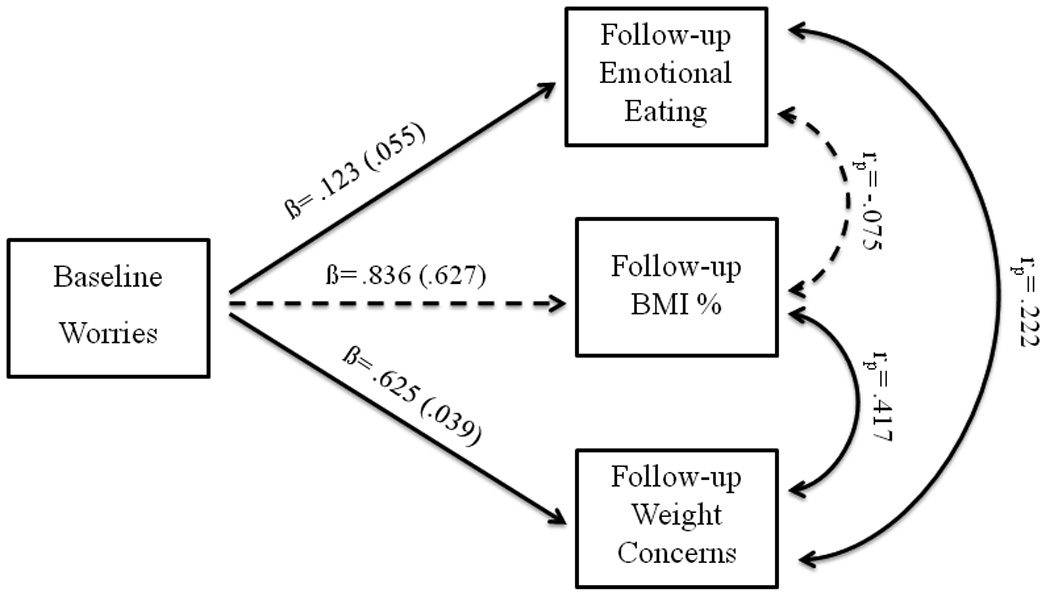
1Values are betas (standard errors); covariates are age, ethnicity, and intervention status.
2Solid lines represent significant pathways & dashed lines represent non-significant pathways.
The mediation model can be found in Figure 2. Mediation was tested using the method described by Baron and Kenny [28] and Sobel’s test was used to determine statistical significance [29]. In these tests, baseline worries was the independent variable, weight status at follow-up was the dependent variable, and emotional eating at follow-up was the proposed mediator. Moderation effects were tested for low versus high emotional eating scores. The sample was stratified based on the sample mean emotional eating scores and multilevel modeling was used to determine whether a significant association existed between baseline worries and follow-up BMI percentile in those with “low” versus “high” emotional eating scores. Although a cut point exists for the emotional eating scale, it was developed in a White sample. The mean score was used as a cut point in this minority sample. Data analysis was conducted using SAS v9.1 (SAS Institute, Inc., Cary, NC) and significance was set at alpha= 0.05.
Figure 2.
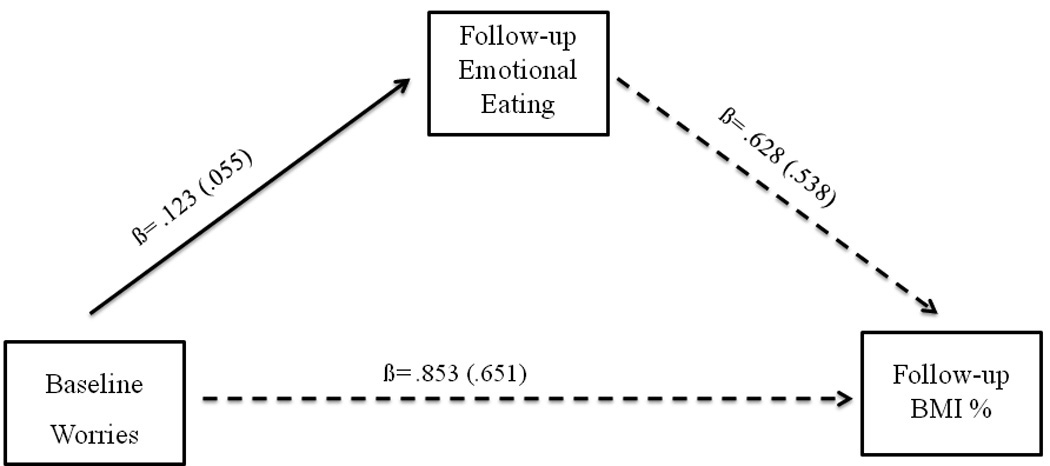
1Values are betas (standard errors)
2Solid lines represent significant pathways & dashed lines represent non-significant pathways.
3Covariates: school intervention status, age, and ethnicity
RESULTS
Descriptives
The sample characteristics are presented in Table 1. There were no statistically significant differences in ethnicity, worries, emotional eating, weight concerns, and BMI percentile between participants with complete data and those with missing data. The participants with missing data were younger than those without missing data (12.2±0.7 vs. 12.5±0.6, respectively; p= 0.049). The study sample was 67.1% Latina, had a mean age of 12.5 (±0.6) years, and 60.6% were classified as normal weight. There was a significant increase in mean emotional eating scores between baseline and follow-up (p= 0.017). Mean BMI percentile also significantly increased from baseline to follow-up (p= 0.036).
Table 1.
Characteristics of the analyzed sample (N= 404)
| Baseline | Follow-up | ||||
|---|---|---|---|---|---|
| Variable | Mean (±SD) | Range | Mean (±SD) | Range | p value |
| Age (years) | 12.5 (±0.6) | 11 – 14 | |||
| BMI percentile | 68.5 (±27.9) | 5.7 – 99.6 | 69.4 (±26.7) | 5.8 – 99.6 | 0.036 |
| Ethnicity (N, (%)) | |||||
| Latina | 271 (67.1) | ||||
| Asian/PI | 51 (12.6) | ||||
| Multi-Ethnic | 48 (11.9) | ||||
| Other | 24 (5.9) | ||||
| White | 10 (2.5) | ||||
| Weight Status1,2 (N, (%)) | |||||
| Normal Weight | 245 (60.6) | 5th to <85th | 241 (59.7) | 5th to <85th | 0.524 |
| Overweight | 75 (18.6) | 85th to < 95th | 81 (20.0) | 85th to < 95th | 0.392 |
| Obese | 84 (20.8) | ≥ 95th | 82 (20.3) | ≥ 95th | 0.774 |
| Worries Scale | 2.3 (±0.7) | 1 – 4 | 2.4 (±0.6) | 1 – 4 | .076 |
| Weight Concerns Scale | 2.4 (±0.6) | 1 – 4 | 2.4 (±0.7) | 1 – 4 | 0.525 |
| Emotional Eating Scale | 1.8 (±0.8) | 1 – 5 | 1.9 (±0.9) | 1 – 5 | 0.017 |
Weight status defined using the CDC age and gender-specific guidelines [31].
Differences in proportions from baseline to follow-up calculated using McNemar’s test; differences in means from baseline to follow-up calculated using paired t-test.
Partial Correlations
The baseline and follow-up psychosocial scores were significantly correlated, and baseline BMI percentile explained 95.1% of the variance in follow-up BMI percentile (partial r= −0.95, p< 0.001). At follow-up, emotional eating was positively correlated with weight concerns (partial r= 0.22, p< 0.001) and weight concerns were positively correlated with BMI percentile (partial r= 0.42, p< 0.001). There was a non-statistically significant negative correlation at follow-up between emotional eating and BMI percentile (partial r= −0.08, p= 0.133).
Regressions
The results from the multi-level model can be found in Table 2 and a conceptual model is presented in Figure 1. After controlling for the random school-level effect, age, ethnicity, and school intervention status, baseline worries was significantly associated with emotional eating (β= 0.12, p= 0.027) and weight concerns (β= 0.63, p< 0.001) at follow-up. Baseline worries were not significantly related to BMI percentile at follow-up (β= 0.84, p= 0.183). There were no ethnic or age differences for any model covariates, nor were there any significant differences in the school random effect for any covariates.
Table 2.
Results from the multi-level model 1
| Multi-Level Model | Baseline Worries | |
|---|---|---|
| Standard β (std error) | p value | |
| Follow-up EE | .12 (.06) | 0.027 |
| Follow-up Weight Concerns | .63 (.04) | 0.001 |
| Follow-up BMI Percentile | .84 (.63) | 0.183 |
All betas are adjusted for age, ethnicity, intervention status, and random effect of school.
BMI= body mass index; EE=emotional eating
The mediation model is presented in Figure 2. The purpose of this model was to determine if baseline worries was operating through an internal psychosocial variable (emotional eating) to impact BMI percentile at follow-up. Baseline worries did not statistically significantly predict follow-up BMI percentile (p= 0.183) thereby failing the first criteria for mediation and precluding further mediation analyses.
The moderation model is presented in Table 3. There were significant moderating effects of baseline emotional eating on the relationship between baseline worries and follow-up BMI percentile (β= 2.13, p= 0.003). After stratifying the sample by the mean emotional eating score, there was a significant positive relationship between worries and BMI percentile in females with “high” emotional eating scores (β= 2.77, p= 0.009) but not in those with “low” emotional eating scores (β= 0.01, p= 0.986).
Table 3.
Relationship among worries, emotional eating, & BMI percentile1
| Multi-Level Model | Follow-up BMI Percentile | |
|---|---|---|
| Standard β (std error) | p value | |
| Baseline Worries | −2.86 (1.40) | 0.042 |
| Baseline EE | −5.77 (1.83) | 0.002 |
| Worries*EE | 2.13 (0.70) | 0.003 |
| Stratified analysis | ||
| Low EE score | 0.01 (0.79) | 0.986 |
| High EE score | 2.77 (1.05) | 0.009 |
All betas are adjusted for age, ethnicity, intervention status, random effect of school, & baseline BMI percentile.
BMI= body mass index; EE= emotional eating
DISCUSSION
The purpose of this analysis was to evaluate the impact of worries on emotional eating, BMI percentile, and weight concerns in minority youth. The first hypothesis that baseline worries are associated with emotional eating, weight concerns, and BMI percentile at follow-up was only partially confirmed. Baseline worries was significantly associated with emotional eating and weight concerns but not BMI percentile at follow-up. Previous research indicates that decreased psychological well-being is associated with higher BMI [30]. However, one typical reaction to stress is under-eating [31]. Therefore, this predominantly normal weight sample may not exhibit the more atypical overeating response to stress. Also, baseline BMI percentile accounted for 95% of the variance in follow-up BMI percentile, leaving only 5% of the variance to be explained by other variables. Although mean BMI percentile did significantly change over time, the increase was small and may have been due to seasonal fluctuations [32]. A longer follow-up may be needed to see the effects of long-term emotional eating on BMI percentile changes.
The second hypothesis that emotional eating mediated or moderated the relationship between worries and BMI percentile was partially supported. While emotional eating did not mediate the relationship between baseline worries and follow-up BMI percentile, there was clear evidence for moderation. There was a positive association between worries and BMI percentile in females with “high” emotional eating scores indicating that worries only affect BMI percentile in those with a propensity to emotionally eat. Some evidence supports a relationship between emotional eating and BMI percentile [20,21]; however the majority of studies have examined differences in emotional eating between normal weight and overweight participants as separate groups. Thus, this was a novel finding of this analysis and adds to the literature base on emotional eating and weight status in minority females. Future work should extend these findings in a longitudinal study design that permits causal associations in normal and overweight youth.
The findings partially supported the third hypothesis; follow-up emotional eating and weight concerns, and weight concerns and BMI percentile were significantly correlated (p< .001 for both). Follow-up emotional eating and BMI percentile were not significantly correlated (p= .133). The positive correlation between BMI percentile and weight concerns is consistent with previous work conducted in ethnically diverse populations that have found increases in weight concerns with increases in BMI percentile [33,34]. The significant relationship between emotional eating and weight concerns in a heterogeneous weight sample suggests that normal weight females are also negatively affected by weight concerns that may be influencing emotional eating behavior. Interventions focused on alleviating weight concerns may be instrumental in improving the psychological well-being of youth and reducing risk for obesity.
This study failed to find a significant association between emotional eating and BMI, which has been reported in White youth. It is possible that emotional eating may not yet be associated with BMI in early adolescence. To our knowledge, no other study has examined this relationship in Latinas and our findings do not support a significant relationship in this population. This finding may be explained by the lack of cultural sensitivity of the measure. Also, cultural differences may exist in reactions t o worries and Latinas may employ different coping strategies than Whites or not identify their food intake as emotion-driven. For example, they may be external eaters (i.e. people who eat as a result of being over-responsive to environmental cues), which is a distinct construct from emotional eating [35] that was not measured in this study due to spatial restrictions on the survey. The lack of studies on emotional eating in Latinas is a void in the literature and warrants future research. This study attempted to address this literature gap, however the findings warrant future research as there are conflicting results and a dearth of knowledge on this topic in minority females.
Several limitations should be considered. Only female participants were included in this analysis thereby prohibiting any study of gender differences in our model. However, van Strien et al. did not find gender-based emotional eating differences in a sample of youth [36]. Also, psychosocial data is vulnerable to self-report bias [37]. BMI percentile is considered a proxy measure of adiposity in adolescents, but has been shown to be significantly correlated with percent body fat in youth [38] and is considered a feasible adiposity measure in large studies [39]. This study is also limited by the repeated measures design, which precludes analyzing causal pathways between the variables and understanding the contribution of natural growth (i.e.: puberty) on BMI percentile. Future studies should assess the longitudinal association between emotional eating and weight status as well as the effects worries can have on long-term BMI changes. These data were collected as part of a larger physical activity intervention, which may have influenced the psychosocial variables in this analysis. For example, overweight adolescent females are more likely to engage in physical activity as a weight control behavior and have more weight concerns than normal weight females [40]. Although intervention status was controlled for in the analysis, future work may want to assess the effects of physical activity on these psychosocial variables in order to understand how these relationships work.
CONCLUSIONS
The findings demonstrate the inter-relationships among psychosocial variables and weight status and related behaviors. Worries predicted emotional eating and weight concerns, suggesting that worries impact psychological well-being and behavior. Future studies should aim to employ longitudinal designs that will help determine the direction of the associations among psychosocial variables on BMI percentile in adolescent populations. Future interventions may want to target improving psychological well-being in those with higher emotional eating scores as a means of impacting future weight status. Worries may play a larger role in the lives of adolescents than previously thought and very little is known about its psychological and behavioral contributions to the obesity epidemic in ethnically diverse populations. Future research should determine the specific worries that are impacting the psychological well-being of youth.
Acknowledgments
This research was supported by NIDDK KO1D-K59293 (Spruijt-Metz, PI) and the NCI-funded USC Center for Transdisciplinary Research on Energetics and Cancer (U54CA 116848)(Spruijt-Metz, Project Leader and Core Co-Director)
We would like to acknowledge Dolly Yang who managed this project, the many undergraduate students who assisted in data collection, and the students and schools who welcomed us into their classrooms.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
REFERENCES
- 1.Wang Y, Beydoun MA. The obesity epidemic in the United States--gender, age, socioeconomic, racial/ethnic, and geographic characteristics: A systematic review and meta-regression analysis. Epidemiologic Reviews. 2007 doi: 10.1093/epirev/mxm007. [DOI] [PubMed] [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of high body mass index in us children and adolescents, 2007–2008. JAMA. 303(3):242–249. doi: 10.1001/jama.2009.2012. [DOI] [PubMed] [Google Scholar]
- 3.Troiano RP, Berrigan D, Dodd KW, et al. Physical activity in the united states measured by accelerometer. Med Sci Sports Exerc. 2008;40(1):181–188. doi: 10.1249/mss.0b013e31815a51b3. [DOI] [PubMed] [Google Scholar]
- 4.Davis JN, Alexander KE, Ventura EE, et al. Associations of dietary sugar and glycemic index with adiposity and insulin dynamics in overweight latino youth. American Journal of Clinical Nutrition. 2007;86(5):1331. doi: 10.1093/ajcn/86.5.1331. [DOI] [PubMed] [Google Scholar]
- 5.Cook S, Auinger P, Li C, et al. Metabolic syndrome rates in united states adolescents, from the national health and nutrition examination survey, 1999–2002. The Journal of Pediatrics. 2008;152(2):165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 6.McAllister EJ, Dhurandhar NV, Keith SW, et al. Ten putative contributors to the obesity epidemic. Critical reviews in food science and nutrition. 2009;49(10):868. doi: 10.1080/10408390903372599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wardle J, Cooke L. The impact of obesity on psychological well-being. Best Pract Res Clin Endocrinol Metab. 2005;19(3):421–440. doi: 10.1016/j.beem.2005.04.006. [DOI] [PubMed] [Google Scholar]
- 8.Baranowski T, Jago R. Understanding the mechanisms of change in children' s physical activity programs. Exerc Sport Sci Rev. 2005;33(4):163–168. doi: 10.1097/00003677-200510000-00003. [DOI] [PubMed] [Google Scholar]
- 9.Falkner NH, Neumark-Sztainer D, Story M, et al. Social, educational, and psychological correlates of weight status in adolescents. Obes Res. 2001;9(1):32–42. doi: 10.1038/oby.2001.5. [DOI] [PubMed] [Google Scholar]
- 10.Vander Wal JS. Eating and body image concerns among average-weight and obese african american and hispanic girls. Eating Behaviors. 2004;5(2):181–187. doi: 10.1016/j.eatbeh.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 11.Haines J, Neumark-Sztainer D, Wall M, et al. Personal, behavioral, and environmental risk and protective factors for adolescent overweight. Obesity (Silver Spring) 2007;15(11):2748–2760. doi: 10.1038/oby.2007.327. [DOI] [PubMed] [Google Scholar]
- 12.Borkovec TD, Robinson E, Pruzinsky T, et al. Preliminary exploration of worry: Some characteristics and processes. Behav Res Ther. 1983;21(1):9–16. doi: 10.1016/0005-7967(83)90121-3. [DOI] [PubMed] [Google Scholar]
- 13.Brosschot JF, van der Doef M. Daily worrying and somatic health complaints: Testing the effectiveness of a simple worry reduction intervention. Psychology & Health. 2006;21(1):19–31. [Google Scholar]
- 14.Spruijt-Metz D, Spruijt RJ. Worries and health in adolescence: A latent variable approach. Journal of Youth and Adolescence. 1997;26(4):485–501. [Google Scholar]
- 15.Washington TD. Psychological stress and anxiety in middle to late childhood and early adolescence: Manifestations and management. Journal of Pediatric Nursing. 2009;24(4):302–313. doi: 10.1016/j.pedn.2008.04.011. [DOI] [PubMed] [Google Scholar]
- 16.Bruch H. Eating disorders. New York: Basic Books; 1973. [Google Scholar]
- 17.Cartwright M, Wardle J, Steggles N, et al. Stress and dietary practices in adolescents. Health Psychol. 2003;22(4):362–369. doi: 10.1037/0278-6133.22.4.362. [DOI] [PubMed] [Google Scholar]
- 18.Konttinen H, Männistö S, Sarlio-Lähteenkorva S, et al. Emotional eating, depressive symptoms and self-reported food consumption: A population-based study. Appetite. 2010 doi: 10.1016/j.appet.2010.01.014. In Press, Accepted Manuscript. [DOI] [PubMed] [Google Scholar]
- 19.Snoek HM, van Strien TJ, anssens JM, et al. Emotional, external, restrained eating and overweight in dutch adolescents. Scand J Psychol. 2007;48(1):23–32. doi: 10.1111/j.1467-9450.2006.00568.x. [DOI] [PubMed] [Google Scholar]
- 20.Braet C, Claus L, Goossens L, et al. Differences in eating style between overweight and normal-weight youngsters. J Health Psychol. 2008;13(6):733–743. doi: 10.1177/1359105308093850. [DOI] [PubMed] [Google Scholar]
- 21.Nguyen-Rodriguez ST, Chou CP, Unger JB, et al. Bmi as a moderator of perceived stress and emotional eating in adolescents. Eat Behav. 2008;9(2):238–246. doi: 10.1016/j.eatbeh.2007.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koch FS, Sepa A, Ludvigsson J. Psychological stress and obesity. J Pediatr. 2008;153(6):839–844. doi: 10.1016/j.jpeds.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 23.Spruijt-Metz D, Nguyen-Michel ST, Goran MI, et al. Reducing sedentary behavior in minority girls via a theory-based, tailored classroom media intervention. Int J Pediatr Obes. 2008;3(4):240–248. doi: 10.1080/17477160802113415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.van Strien T, Frijters JER, Bergers GPA, et al. The dutch eating behavior questionnaire for assessment of restrained, emotional, and external eating behavior. International Journal of Eating Disorders. 1986;5(2):295–315. [Google Scholar]
- 25.Tomeo CA, Field AE, Berkey CS, et al. Weight concerns, weight control behaviors, and smoking initiation. Pediatrics. 1999;104(4):918–924. doi: 10.1542/peds.104.4.918. [DOI] [PubMed] [Google Scholar]
- 26.Kuczmarski RJ, Ogden CL, Guo SS, et al. 2000 cdc growth charts for the united states: Methods and development. Vital Health Stat. 2002;11(246):1–190. [PubMed] [Google Scholar]
- 27.Phinney JS. The multigroup ethnic identity measure: A new scale for use with diverse groups. Journal of Adolescent Research. 1992;7(2):156–176. [Google Scholar]
- 28.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 29.Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociological methodology. 1982;13:290–312. [Google Scholar]
- 30.Storch E, Milsom V, DeBraganza N, et al. Peer victimization, psychosocial adjustment, and physical activity in overweight and at-risk-for-overweight youth. Journal of Pediatric Psychology. 2007;32(1):80. doi: 10.1093/jpepsy/jsj113. [DOI] [PubMed] [Google Scholar]
- 31.Gold PW, Chrousos GP. Organization of the stress system and its dysregulation in melancholic and atypical depression: High vs low crh/ne states. Mol Psychiatry. 2002;7(3):254–275. doi: 10.1038/sj.mp.4001032. [DOI] [PubMed] [Google Scholar]
- 32.von Hippel PT, Powell B, Downey DB, et al. The effect of school on overweight in childhood: Gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007;97(4):696–702. doi: 10.2105/AJPH.2005.080754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lee K, Sohn H, Lee S, et al. Weight and bmi over 6 years in korean children: Relationships to body image and weight loss efforts. Obesity Res. 2004;12(12):1959–1966. doi: 10.1038/oby.2004.246. [DOI] [PubMed] [Google Scholar]
- 34.Sweeting H, Wright C, Minnis H. Psychosocial correlates of adolescent obesity, `slimming down' and `becoming obese'. Journal of Adolescent Health. 2005;37(5) doi: 10.1016/j.jadohealth.2005.01.008. 409.e409-409.e417. [DOI] [PubMed] [Google Scholar]
- 35.van Strien T, Oosterveld P. The children' s debq for assessment of restrained, emotional, and external eating in 7- to 12-year-old children. Int J Eat Disord. 2008;41(1):72–81. doi: 10.1002/eat.20424. [DOI] [PubMed] [Google Scholar]
- 36.van Strien T, Bazelier FG. Perceived parental control of food intake is related to external, restrained and emotional eating in 7–12-year-old boys and girls. Appetite. 2007;49(3):618–625. doi: 10.1016/j.appet.2007.03.227. [DOI] [PubMed] [Google Scholar]
- 37.Lissner L. Measuring food intake in studies of obesity. Public Health Nutr. 2002;5(6A):889–892. doi: 10.1079/phn2002388. [DOI] [PubMed] [Google Scholar]
- 38.Pietrobelli A, Faith MS, Allison DB, et al. Body mass index as a measure of adiposity among children and adolescents: A validation study. Journal of Pediatrics. 1998;132(2):204. doi: 10.1016/s0022-3476(98)70433-0. [DOI] [PubMed] [Google Scholar]
- 39.Dietz WH, Robinson TN. Use of the body mass index (bmi) as a measure of overweight in children and adolescents. Journal of Pediatrics. 1998;132(2):191. doi: 10.1016/s0022-3476(98)70426-3. [DOI] [PubMed] [Google Scholar]
- 40.Neumark-Sztainer D, Story M, Hannan PJ, et al. Weight-related concerns and behaviors among overweight and nonoverweight adolescents: Implications for preventing weight-related disorders. Arch Pediatr Adolesc Med. 2002;156(2):171–178. doi: 10.1001/archpedi.156.2.171. [DOI] [PubMed] [Google Scholar]


