Abstract
Background and Objectives:
Anthropometric variables and their relation to conventional coronary artery disease (CAD) risk factors in railway employees have been inadequately studied in India. This cross-sectional survey was carried out in the Solapur division of the Central railway in the year 2004, to assess the anthropometric variables in railway employees and their relation to conventional CAD risk factors.
Materials and Methods:
A total of 995 railway employees, with 872 males and 123 females participated in this cross-sectional study. All subjects underwent anthropometric measurements, fasting lipid profile, and blood sugar level. Various anthropometric indices were calculated for body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), and abdominal volume index (AVI). Statistical analysis was done by EPI Info 6 statistical software.
Results:
Compared to all other obesity indices, WHtR was most prevalent in both genders. High WHtR was present in 699 (80.16%) males and 103 (83.73%) females. Age ≥45 years, high systolic BP, high diastolic BP, low HDL, high triglyceride, and diabetes mellitus were positively correlated with high BMI, high WC, high WHR, high WHtR, and high AVI. High BMI, high WC, high WHR, high WHtR, and high AVI were negatively associated with physical inactivity.
Conclusions:
Over all, anthropometric variables in both genders were significantly deranged in subjects with coronary risk factors. Compared to all other anthropometric variables, WHtR was statistically significantly associated with a majority of coronary artery risk factors. Hence we recommend inclusion of WHtR as a parameter of obesity to predict coronary artery disease risk factor along with WC, WHR, and BMI in epidemiologic studies.
Keywords: Anthropometric variables, abdominal volume index, body mass index, waist circumference, waist-to-hip ratio, waist-to-height ratio
INTRODUCTION
So far, anthropometric variables and their relation to conventional coronary risk factors in railway employees have been inadequately studied in India. To assess anthropometric variables and their relation to coronary risk factors, this cross-sectional survey was carried out in Solapur division of the Central railway in the year 2004. The purpose of this study was to examine the association of obesity with CAD risk factors by different anthropometric variables. This particular section of the population was selected, as it comprises all classes of employees, including both sexes, sedentary and nonsedentary job workers of various socioeconomic groups, religions, and from different parts of India.
MATERIALS AND METHODS
This study was designed to investigate conventional CAD risk factors and their relation to anthropometric variables among the Solapur division railway employees. This study was approved by the ethical committee of Dr. V.M. Medical College, Solapur, and Dr. Kotnis Memorial Railway Hospital, Solapur. This study was conducted among the railway employees of Solapur division of the Central railway.
A proforma was prepared that incorporated information regarding demography (age and sex), anthropometric (height in meter, weight in kilograms, waist and hip circumferences in centimeters) variables, occupation (sedentary or nonsedentary), physical examination (pulse, blood pressure), clinical data (history of diabetes hypertension, smoking, tobacco chewing, exercise), and biochemical investigations [fasting blood sugar level (BSL) and complete lipid profile]. Anthropometric variables were calculated by using the above measurements for body mass index (BMI), waist circumference (WC), waist-to-hip ratio (WHR), waist-to-height ratio (WHtR), and abdominal volume index (AVI). All the eligible employees of both sexes underwent physical, anthropometric examination, and biochemical investigations according to the standard guidelines used earlier.[1]
A total of 995 railway employees participated in this cross-sectional survey with age ≥ 30 and ≤ 60 years. Railway employees were chosen from railway stations, divisional railway mandal office, railway police force (RPF) and railway hospitals. According to the nature of their job, they were classified as sedentary and nonsedentary workers, including both males and females. Out of 995 subjects studied, 700 (70.35%) underwent biochemical investigations. There were 872 men of whom 484 (55.5%) were of age < 45 years and 388 (44.5%) were of age ≥ 45 years. A total of 123 were females, 58 (48%) were of age < 45 years and 65 (52%) were of age ≥ 45 years.
Blood pressure was measured using a standard mercury sphygmomanometer under standard conditions as mentioned in cardiovascular survey methods.[1] Biochemical investigations were performed on an automated analyzer by using the kit provided by Accurex Biomedical Pvt. Ltd. (ISO 13485: 2003, ISO 9001: 2008 & CE certified Mumbai, India). HDL cholesterol was calculated by phosphotungstate/MgCl 2 autozyme technique. The concentration of LDL cholesterol was calculated by using a formula of Friedewald. [LDL cholesterol = total cholesterol – (HDL + triglyceride/5)].[2] Total cholesterol (T-CHO) was measured by cholesterol oxidase (CHOD)– phenol + aminophenazone (PAP) enzymatic colorimetric technique. Triglyceride (TRG) was measured by glycerol-3-phosphate oxidase (GPO)– peroxidase (POD) enzymatic technique. BSL fasting was done by glucose oxidase (GOD) – peroxidase (POD) enzymatase by autoenzyme technique.
Anthropometric measurements
Each person was examined for height, weight, WC, and hip circumference without shoes and chappals with minimal clothing as per cardiovascular survey methods.[1] BMI was calculated by formula of weight in kg/height m2. WHR was calculated by WC/HC in centimeters. WHtR was calculated by WC/height in centimeters. AVI was calculated using volume formulas for cylinder (V = πr2h) and vertical cone V = (1/3)πr2h. The formula developed was AVI = [2 cm (waist)2 + 0.7 cm (WC – HC)2]/1000, which estimates overall abdominal volume between symphysis of pubis and xiphoid appendix and theoretically includes intra-abdominal fat and adipose tissue volumes.[3]
Diagnostic criteria
A smoker in India consumes tobacco in the form of bidi/cigarettes and chewing tobacco. A person smoking one or more cigarettes or bidis per day at the time of study was considered as a smoker and one chewing tobacco currently, a tobacco chewer.[4] In the present study, tobacco consumption in the form of smoking and in the form of tobacco chewing were grouped separately.
-
Physical activity according to the type of job were classified as,
Nonsedentary job (moderate to heavy physical activity)
-
Sedentary job (low physical activity) Physical activity was classified into 2 levels,
Moderate to high physical activity was referred as nonsedentary (RPF, drivers, gangmen, and others)
Low physical activity referred (sedentary) to people involved in office work, research work, and so on.[5]
Cutoffs for high BMI were ≥25 for females and ≥27 for males.[6,7] Cutoffs for high WHR were ≥0.9 for males and ≥0.8 for females. Cutoffs for high WHtR were ≥0.45 for females and ≥0.48 for males. Cutoffs for high WC were >85 cm for females and >90 cm for males.[6] Cutoffs for high AVI was calculated by receiver-operator characteristic (ROC) curve 16.48 liter.
Diabetes mellitus (DM): If a subject is a known diabetic on treatment with any BSL or if fasting BSL (F-BSL) 126 mg/dL.[6] Dyslipidemia was defined as if, T-CHO ≥ 200 mg/dL, LDL, cholesterol ≥ 130 mg/dL, HDL, cholesterol 40 mg/dL, TRG ≥ 150 mg/dL.[6] Hypertension was labeled if blood pressure ≥ 140 mmHg SBP and ≥90 mmHg DBP or known to be hypertensive on treatment with any blood pressure.[8]
Statistical analysis
The data were pooled, computerized, and analyzed by evaluation version of EPI Info. 6 [( Epi Info is public domain statistical software for epidemiology developed by Centers for Disease Control and Prevention (CDC) in Atlanta, Georgia (USA)]. Prevalence rates were given in percentage. Various numbers are given as mean and standard deviation. Categorical variables have been compared by using χ2 (Chi-square) test. The Pvalue < 0.05 was considered as significant. Correlation of anthropometric variables and coronary risk factors in different age groups were determined using r2 and multiple linear regression analysis. ROC curve is used to find out the cutoff point for particular value of a test as a diagnostic test. Cutoff values of WHtR and AVI were calculated by using this curve as a tool for diagnosing central obesity.[9] Correlation (r): r = 0.8 (high correlation coefficient), r= 0.4–0.7 (moderate correlation), and r= 0.3 and above (low correlation coefficient).
RESULTS
A total of 872 (87.63%) were males and 123 (12.36%) were females. All of them underwent physical examination, and anthropometric measurements for Ht, Wt, HC, and WC, but only 605 males and 95 females underwent biochemical investigations with a response rate of 69.15%in males and 77.23% in females.
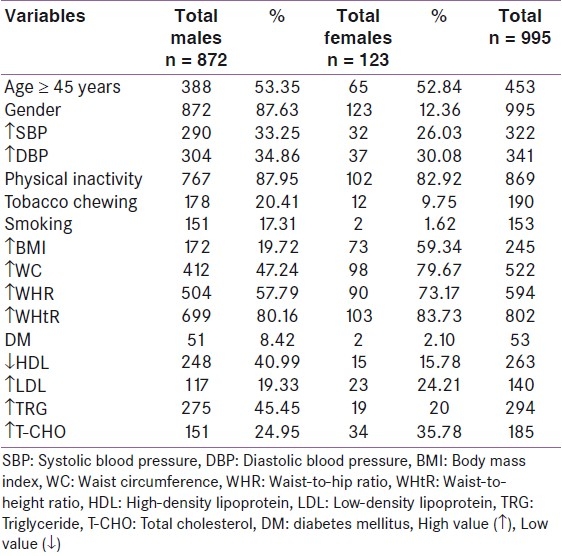
The subjects were ≥45 years of age; 388 (53.35%) males and 65 (52.84%) females. High SBP was present in 290 (33.25%) males and 32 (26.03%) females. High DBP was present in 304 (34.86%) males and 37 (30.08%) females. Physical inactivity was present in 767 (87.95%) males and 102 (82.92%) females. Tobacco chewing was present in 178 (20.41%) males and 12 (9.75%) females. Smoking was present in 151 (17.31 %) males and 2 (1.62%) females. High BMI was present in 172 (19.72%) males and 73 (59.34%) females. High WC was present in 412 (47.24%) males and 98 (79.67%) females. High WHR was present in 504 (57.79%) males and 90 (73.17%) females. High WHtR was present in 699 (80.16%) males and 103 (83.73%) females. High AVI was present in 359 (41.16%) males and 35 (28.45%) females. DM was present in 51 (8.42%) males and 2 (2.10%) females. Low HDL was present in 248 (40.99%) males and 15 (15.78%) females. High LDL was present in 117 (19.33%) males and 23 (24.21%) females. High T-CHO was present in 151 (24.95%) males and 34 (35.78%) females. High TRG was present in 275 (45.45%) males and 19 (20%) females [Table 1].
Table 1.
Prevalence of coronary artery disease risk factors
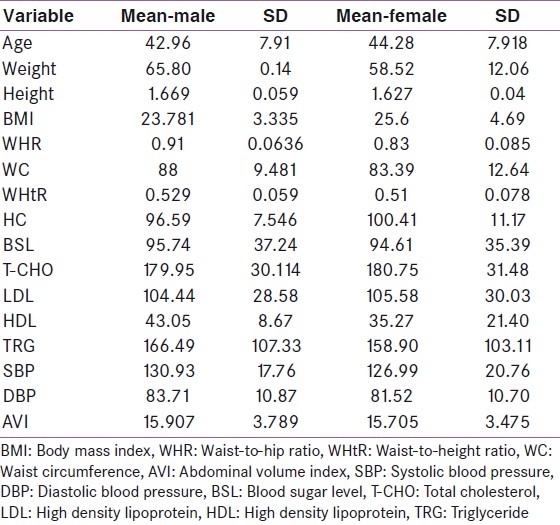
In both males and females, all the anthropometric variables were high. Most prevalent obesity index in male population was high WHtR. In female population, the most prevalent obesity index was high WHtR. Prevalence of overall and central obesity was comparatively more in female population for all the variables as shown in Table 2. Mean age, BMI, and low HDL levels were comparatively higher in females, whereas mean SBP, DBP, TRG, WHR, WC, and WHtR were comparatively higher in males. Standard deviation values of quantitative data in male and female population are shown in Table 3.
Table 2.
Prevalence of obesity indices
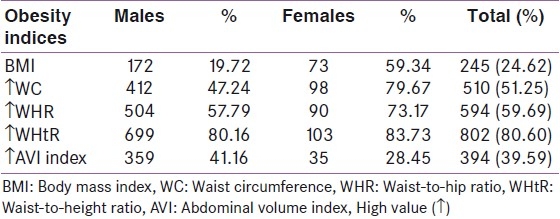
Table 3.
Standard deviation values of quantitative data in male and female population
Total 65 females were with age ≥ 45 years and 58 with age < 45 years. In female population, high WHR in age ≥ 45 years was present in 58 (47.15%). High BMI in age ≥ 45 years was present in 46 (37.39%). High WC in age ≥ 45 years was present in 57 (46.34%). High WHtR in age ≥ 45 years was present in 54 (43.90%). High AVI in age ≥ 45years was present in 25 (20.32%). In females only high BMI was statistically significant in age ≥ 45 years with P value < 0.001.
Males totalling 388 were of the age ≥ 45 years and 484 females were < 45 years of age. In male population, ≥45 years of age, a high WHR was present in 262 (30.04%). A high BMI in age ≥ 45 years was present in 90 (10.32%). A high WC in age ≥ 45 years was present in 207 (23.73%). High WHtR in age ≥ 45 years was present in 332 (38.07%). High AVI in age ≥ 45 years was present in 279 (31.99%). In males, all anthropometric variables, such as WHR, WHtR, BMI, WC, and AVI, were significantly raised, in the age group ≥ 45 years with P value < 0.001.
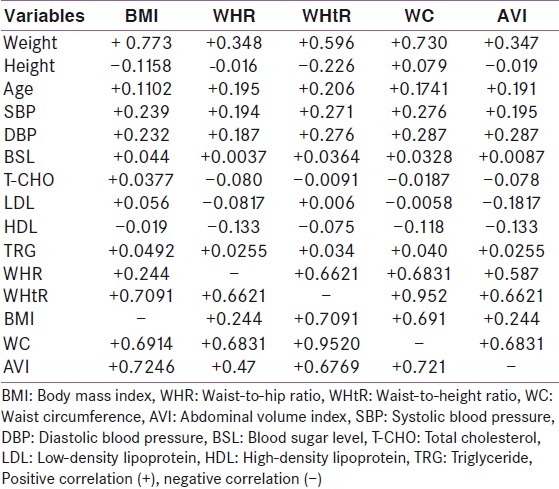
Correlation of anthropometric indices to coronary artery disease risk factors
BMI had partial positive correlation (moderate to low) with coronary risk factors, such as age weight, SBP, DBP, F-BSL, T-CHO, LDL cholesterol, TRG, and other anthropometric variables. WHR had partial positive correlation (moderate to low) with coronary risk factors, such as age, height, weight, SBP, DBP, F-BSL, total, TRG, and other anthropometric variables. WHtR had partial positive correlation (moderate to low) with coronary risk factors, such as age, weight, SBP, DBP, F-BSL, LDL cholesterol, TRG, and other anthropometric variables. WC had partial positive correlation (moderate to low) with coronary risk factors, such as age, weight, height, SBP, DBP, F-BSL, TRG, and other anthropometric variables. AVI had partial positive correlation (moderate to low) with coronary risk factors, such as age, weight, height, SBP, DBP, F-BSL, TRG, and other anthropometric variables [Table 4]. In male population, age ≥ 45 years had odds ratio of 2.15 with WHtR and 1.95 with AVI. Sedentary job had an odds ratio of 1.402 with BMI. Officers had an odds ratio of 4.69 with BMI and 1.552 with AVI. BSL had an odds ratio of 1.457 with WC and 3.66 with BMI. T-CHO had odds ratio of 2.11 with BMI. LDL cholesterol had an odds ratio of 2.47 with BMI. Low HDL cholesterol had an odds ratio of 1.67 with WC. TRG had an odds ratio of 1.271 with WC and 1.32 with AVI. SBP had an odds ratio of 2.0 with BMI, 1.47 with WC, and 1.48 with AVI. DBP had an odds ratio of 1.79 with BMI and 1.59 with WC.
Table 4.
Correlation of anthropometric indices with coronary artery disease risk factors
In female population, age ≥ 45 years had an odds ratio of 1.673 with BMI. Sedentary job had an odds ratio of 2.0 with WHR, 1.86 with WC, and 1.79 with WHtR. T-CHO had an odds ratio of 1.45 with WC. TRG had an odds ratio of 1.329 with AVI. SBP had an odds ratio of 1.48 with AVI and DBP had an odds ratio of 1.34 with WC.
We have correlated all anthropometric indices with CAD risk factors considering the overall population. We have found that age ≥ 45 years was better correlated with high values of BMI, WC, WHR, WHtR, and AVI. High SBP, high DBP, and sedentary job were significantly and positively correlated with high values of BMI, WC, WHR, WHtR and AVI. Officers were positively correlated with high values of BMI, WHtR, and AVI. High values of BMI, WC, WHR, WHtR, and AVI were negatively associated with physical inactivity. Tobacco and smoking were negatively correlated with high values of BMI, WC, WHR, and WHtR. DM was statistically significant and positively associated with high values of BMI, WC, WHR, WHtR, and AVI. In dyslipidemia low HDL was correlated with high values of WHR, WHtR, and AVI, whereas LDL cholesterol, T-CHO, and TRG were correlated only with high BMI and high WHtR in this population [Table 4].
In multiple regression analysis a model was utilized that included age, BMI, WHR, WHtR, WC, AVI, SBP, DBP, plasma T-CHO, TRG, and smoking. This revealed age, WHtR, and WHR as an independent determinant of most of the CAD risk factors in both genders. Multiple regression analysis for WHtR and WHR showed that both of them were significantly associated with most of the CAD risk factors, such as age ≥ 45 years, high SBP, high DBP, DM, low HDL, high LDL, high T-CHO, and high TRG [Table 5].
Table 5.
Relation of anthropometric variables and coronary artery disease risk factors in males and females
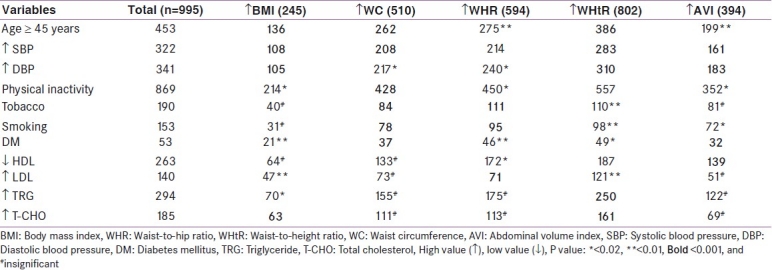
Furthermore, the WHR was the single independent variable to all or most of the CAD risk factors by multiple regression analysis. Multiple logistic regression analysis revealed WHtR and WHR were significantly associated with age (P < 0.001), BMI (P < 0.001) DM (P = 0.005), SBP (P < 0.001), DBP (P < 0.001), low HDL in females, and high TRG in males (P < 0.001) [Figure 1].
Figure 1.
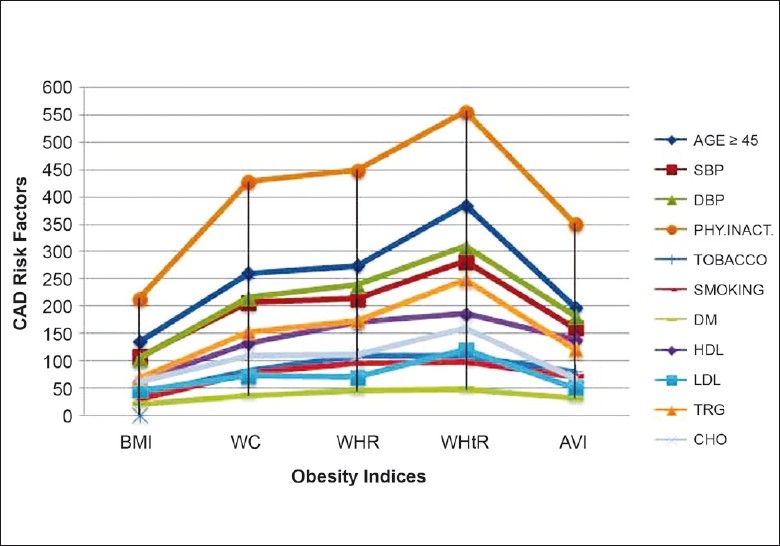
Relation of anthropometric variables to coronary artery disease risk factors
DISCUSSION
Anthropometric variables were raised in the Solapur Division railway employees. Both overall and central obesity were highly prevalent in both male and female population. Conventional CAD risk factors, such as physical inactivity, central obesity, hypertension, low HDL, age ≥ 45 years, and hypertriglyceridemia were highly prevalent in males, whereas physical inactivity, central obesity, hypertension, age ≥ 45 years, and hypercholesterolemia were highly prevalent in female population. WHtR was statistically significantly associated with majority of CAD risk factors. Compared to overall obesity, central obesity was better correlated with most of the CAD risk factors. WHtR was better predictive of CAD risk factors than WC and WHR in present study. Cutoff value for WHtR has not been calculated for the Indian population, hence further studies are required for calculation in the Indian context. In the present study, WHtR was a powerful predictor of most of the CAD risk factors, whereas WHR, WC, and AVI were next to it in a decreasing order. We have compared our results with various studies in which Lin et al in a general population study reported that, WHtR is a better indicator for predicting CVD risk factors than the other 3 indices (BMI, WC, and WHR) in Taiwan, which is comparable with our study.[10] Lin et al[10] and Hsieh et al[11,12] also stated that WHtR is a better predictor of most of the CAD risk factors than WHR, WC, and BMI. Huang et al[13] in a general population study in Taiwan found that the 4 anthropometric indices (BMI, WC, WHR, and WHtR) are closely related to cardiovascular risk factors, which is comparable with our study. The results of Misra et al[14] indicated a high prevalence of diabetes, obesity, and dyslipidemia in urban slum population in northern India in middle age, particularly in females, which is comparable with our study. Guerrero-Romero et al[3] in their study of 746 men and nonpregnant women randomly recruited from Durango City in northern Mexico, stated that AVI is reliable and shown to be strongly related to IGT and DM, which is comparable with our study, but they have not correlated the association with other CAD risk factors, such as hypertension, dyslipidemia, and physical inactivity. In Southern Andhra Pradesh, India, a study of randomly selected urban and rural population by Venkatramana et al[15] suggested that BMI and WC are better indicators of CAD risk factors, which is partially comparable with our study as other anthropometric variables have not been used in their study. Reeder et al[16] in 5 Canadian provinces (Alberta, Manitoba, Ontario, Quebec, and Saskatchewan) general population study, found that WC was the measure of abdominal obesity most highly correlated with cardiovascular disease risk factors, which is partially comparable with our study. In Omani population Al-Riyami and Afifi,[17] in their study among male adults aged 20 years and above in a community-based survey as a part of the National Health Survey, reported that current smokers were of low BMI compared with nonsmokers and exsmokers and currently light smokers were also of low BMI compared with exsmokers, which is comparable with our study. In the railway employees cohort, smoking was negatively associated only with BMI. Ledoux et al,[18] in a Canadian general population study stated that the WC and BMI correlate most closely with blood pressure and plasma lipids, which is comparable with the present study. Onat et al,[19] in a random sample of Turkish general adult population, observed that the WC and WHR were strongly associated with BMI and DBP and plasma TRG in Turkish women, which is similar to and comparable with our results. Hsieh et al,[20] in a study found that, the WHtR and WHR increased with age in both the genders, which is comparable with our results.
Rosmond et al,[21] in a selected population study, reported that obesity (BMI) and centralization of body fat stores (WHR) are differently associated with occupational factors as well as leisure time activities. Hu et al[22] reported that television watching and other sedentary behaviors are related to risk of obesity and type 2 DM in women. Both these studies are comparable with the current study. Slattery et al[23] in a study of the US Railroad population quoted that occupationally and leisure time physically inactive employees are at a higher risk of developing CAD risk factors and cardiovascular death, which is consistent with the current study. Several studies[17,24] showed that smokers have, on an average, lower BMI than nonsmokers and that smoking cessation is often associated with weight gain.
In the present study, WHtR has been found to be significantly and positively associated with most of the CAD risk factors, hence WHtR can be used routinely as an anthropometric tool for prediction of CAD risk factors in epidemiologic studies.[25–29]
The other parameters of coronary artery risk [C-reactive protein (CRP), homocysteine, and others] have not been done in the present study because of limitations of study to conventional CAD risk factors and resource limitations.
Other CAD risk factors, such as hyperhomocysteinemia, have not shown a robust utility in CHD risk stratification, and there are no clinical trial data showing that intervention to lower homocysteine levels reduces CHD events. Measurement of homocysteine levels should be reserved for individuals with atherosclerosis at a young age or out of proportion to established risk factors. Elevations in acute-phase reactants, such as fibrinogen or CRP, may reflect overall atherosclerotic burden or extravascular inflammation that could potentiate atherosclerosis or its complications. CRP measured by high-sensitivity assay, adds predictive information to that derived from established coronary artery risk factors, such as cholesterol. Elevated levels of the acute-phase reactant CRP and fibrinogen may merely reflect ongoing inflammation rather than a direct etiologic role for CRP in CAD.
In the present study, the prevalence of metabolic syndrome (using ATP III criteria modified for Indians) was 25.17% in males and 27.35% in females. Among all the components of metabolic syndrome, high WC was most prevalent in females and systolic hypertension in males.
SUMMARY AND CONCLUSION
In the current study, the most common CAD risk factor was truncal obesity in the Solapur division railway employees. Generalized obesity, overweight, and central obesity problem was more prevalent in subjects with age ≥ 45 years, sedentary job, physical inactivity, and female gender. There was a significant lack of physical activity and exercise among sedentary job workers, leading to overweight and obesity. Generalized obesity, overweight, and central obesity were significantly correlated with CAD risk factors, such as age ≥ 45 years, dyslipidemia, hypertension, DM, and physical inactivity.
Central obesity measured by WHtR was strongly correlated with majority of CAD risk factors than WHR, WC, and AVI. These observations serve to underline the central role of overweight/obesity and the additive deleterious effects of abdominal obesity in the pathogenesis of lipid and carbohydrate metabolism, leading to CHD and type 2 DM, and hypertension. The present study shows a disturbing burden of coronary risk factors mainly truncal obesity, physical inactivity, hypertension in a sample population of railway employees. There is an urgent need to undertake population-based measures to reverse the trend. Out of all the anthropometric variables, WHtR was significantly and positively associated with most of the CAD risk factors, hence WHtR can be used routinely as an anthropometric tool for prediction of CAD risk factors in epidemiologic studies. By preventing obesity and overweight, a substantial part of CHD mortality may be prevented because a majority of the CAD risk factors are strongly correlated with anthropometric indices. We concluded that weight control should be an integral part of the prevention of cardiovascular disease. The “U” turn in obesity express highway probably lies in lifestyle modifications, going back to a traditional lifestyle with a judicious use of modern technology. There is a pressing need for primordial prevention of obesity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Rose GA, Blackburn H, Gillum RF, Prineas RJ. WHO monograph series no. 56. 2nd ed. Geneva: World Health Organization; 1982. Cardiovascular survey methods.2nd ed. [PubMed] [Google Scholar]
- 2.Friedewald WT, Levx RI, Frederickson DS. Estimation of concentration of LDL cholesterol in plasma without use of ultra: Centrifuge. Clin Chem. 1972;18:499–507. [PubMed] [Google Scholar]
- 3.Guerrero-Romero F, Rodríguez-Morán M. Abdominal volume index: An anthropometry-based index for estimation of obesity is strongly related to impaired glucose tolerance and type 2 diabetes mellitus. Arch Med Res. 2003;34:428–32. doi: 10.1016/S0188-4409(03)00073-0. [DOI] [PubMed] [Google Scholar]
- 4.Walia M. Prevalence of coronary risk factors in NIDDM. J Assoc Physicians India. 1999;47:1052. [PubMed] [Google Scholar]
- 5.Paffenbarger R, Hyde R, Wing A, Lee I, Jung D, Kampert J. The association of changes in physical activity level and other lifestyle characteristics with mortality among men. N Engl J Med. 1993;328:538–45. doi: 10.1056/NEJM199302253280804. [DOI] [PubMed] [Google Scholar]
- 6.Gupta R, Majumdar S. Correlation of waist-hip ratio with coronary heart disease and risk factor prevalence in a rural male population. Indian Heart J. 1994;46:145–8. [PubMed] [Google Scholar]
- 7.Executive summary of third report of the cholesterol education program (NECP) Expert panel of detection, Evaluation, and treatment of high blood cholesterol In Adults. (Adult Treatment Panel III) JAMA. 2001;285:2486–97. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 8.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure.JNC VII Report. JAMA. 2003;289:2560–71. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 9.Fletcher RH, Fletcher SW, Wagner EH. 3rd ed. Baltimore: Williams & Wilkins; 1996. Clinical epidemiology.The essentials. [Google Scholar]
- 10.Lin WY, Lee LT, Chen CY, Lo H, Hsia HH, Liu IL, et al. Optimal cut off values for obesity to predict CAD risk factor in Taiwan. Int J Obes Relat Metab Disord. 2002;26:1232–8. doi: 10.1038/sj.ijo.0802040. [DOI] [PubMed] [Google Scholar]
- 11.Hsieh SD, Yoshinaga H, Muto T. Waist-to-height ratio, a simple and practical index for assessing central fat distribution and metabolic risk in Japanese men and women. Int J Obes Relat Metab Disord. 2003;27:610–6. doi: 10.1038/sj.ijo.0802259. [DOI] [PubMed] [Google Scholar]
- 12.Hsieh SD, Yoshinaga H. Abdominal fat distribution and coronary heart disease risk factors in men-waist/height ratio as a simple and useful predictor. Int J Obes Relat Metab Disord. 1995;19:585–9. [PubMed] [Google Scholar]
- 13.Huang B, Rodreiguez BL, Burchfiel CM, Chyou PH, Curb JD, Sharp DS. Associations of adiposity with prevalent coronary heart disease among elderly men: The Honolulu Heart Program. Int J Obes Relat Metab Disord. 1997;21:340–8. doi: 10.1038/sj.ijo.0800410. [DOI] [PubMed] [Google Scholar]
- 14.Misra A, Pandey RM, Devi JR, Sharma R, Vikram NK, Khanna N. High prevalence of diabetes, obesity and dyslipidaemia in urban slum population in northern India. Int J Obes Relat Metab Disord. 2002;26:1281. doi: 10.1038/sj.ijo.0801748. [DOI] [PubMed] [Google Scholar]
- 15.Venkatramana P, Reddy PC. Association of overall and abdominal obesity with coronary heart disease risk factors: Comparison between urban and rural Indian men. Asia Pac J Clin Nutr. 2002;11:66–71. doi: 10.1046/j.1440-6047.2002.00250.x. [DOI] [PubMed] [Google Scholar]
- 16.Reeder BA, Senthilselvan A, Despres JP, Angel A, Liu L, Wang H, et al. The association of cardiovascular disease risk factors with abdominal obesity in Canada.Canadian Heart Health Surveys Research Group. CMAJ. 1997;157:S39–45. [PubMed] [Google Scholar]
- 17.Al-Riyami AA, Afifi MM. The relation of smoking to body mass index and central obesity among Omani male adults. Saudi Med J. 2003;24:875–80. [PubMed] [Google Scholar]
- 18.Ledoux M, Lambert J, Reeder BA, Despres JP. A comparative analysis of weight to height and waist to hip circumference indices as indicators of the presence of cardiovascular disease risk factors. Canadian Heart Health Surveys Research Group. CMAJ. 1997;157:S32–8. [PubMed] [Google Scholar]
- 19.Onat A, Sansoy V, Uysal O. Waist circumference and waist-to-hip ratio in Turkish adults: interrelation with other risk factors and association with cardiovascular disease. Int J Cardiol. 1999;70:43–50. doi: 10.1016/s0167-5273(99)00049-2. [DOI] [PubMed] [Google Scholar]
- 20.Hsieh SD, Yoshinaga H, Muto T, Sakurai Y. Anthropometric obesity indices in relation to age and gender in Japanese adults. Tohoku J Exp Med. 2000;191:79–84. doi: 10.1620/tjem.191.79. [DOI] [PubMed] [Google Scholar]
- 21.Rosmond R, Lapidus L, Bjorntorp P. The influence of occupational and social factors on obesity and body fat distribution in middle-aged men. Int J Obes Relat Metab Disord. 1996;20:599–607. [PubMed] [Google Scholar]
- 22.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA. 2003;289:1785–91. doi: 10.1001/jama.289.14.1785. [DOI] [PubMed] [Google Scholar]
- 23.Slattery ML, Jacobs DR, Jr, Nichaman MZ. Leisure time physical activity and coronary heart disease death. The US Railroad study. Circulation. 1989;79:304–11. doi: 10.1161/01.cir.79.2.304. [DOI] [PubMed] [Google Scholar]
- 24.Jousilahti P, Tuomilehto J, Vartiainen E, Pekkanen J, Puska P. Body weight, cardiovascular risk factors, and coronary mortality.15-year Follow-up of middle-aged men and women in eastern Finland. Circulation. 1996;93:1372–9. doi: 10.1161/01.cir.93.7.1372. [DOI] [PubMed] [Google Scholar]
- 25.Hsieh SD, Muto T. The superiority of waist-to-height ratio as an anthropometric index to evaluate clustering of coronary risk factors among non-obese men and women. Prev Med. 2005;40:216–20. doi: 10.1016/j.ypmed.2004.05.025. [DOI] [PubMed] [Google Scholar]
- 26.Hsieh SD, Ashwell M, Muto T, Tsuji H, Arase Y, Murase T. Urgency of reassessment of role of obesity indices for metabolic risks. Metabolism. 2010;59:834–40. doi: 10.1016/j.metabol.2009.09.032. [DOI] [PubMed] [Google Scholar]
- 27.Mombelli G, Zanaboni AM, Gaito S, Sirtori CR. Waist-to-height ratio is a highly sensitive index for the metabolic syndrome in a Mediterranean population. Metab Syndr Relat Disord. 2009;7:477–84. doi: 10.1089/met.2008.0101. [DOI] [PubMed] [Google Scholar]
- 28.Bosy-Westphal A, Geisler C, Onur S, Korth O, Selberg O, Schrezenmeir J, et al. Value of body fat mass vs anthropometric obesity indices in the assessment of metabolic risk factors. Int J Obes (Lond) 2006;30:475–83. doi: 10.1038/sj.ijo.0803144. [DOI] [PubMed] [Google Scholar]
- 29.Lee CM, Huxley RR, Wildman RP, Woodward M. Indices of abdominal obesity are better discriminators of cardiovascular risk factors than BMI: A meta-analysis. J Clin Epidemiol. 2008;61:646–53. doi: 10.1016/j.jclinepi.2007.08.012. [DOI] [PubMed] [Google Scholar]


