Abstract
Total fat replacement of the pancreas is rare. Focal fatty replacement is the most common degenerative lesion of pancreas. Focal fatty deposits have no major clinical significance; however, extreme fat replacement is of pathologic significance, as it is associated with marked reduction in exocrine function of pancreas, resulting in malabsorption due to pancreatic enzyme insufficiency.
Keywords: Computed tomography, malabsorption, pancreatic lipomatosis
INTRODUCTION
Fatty replacement of exocrine pancreas, also known as fatty infiltration, lipomatosis, adipose atrophy, or lipomatous pseudohypertrophy is a well-documented benign entity of speculative origin.[1] We present a case of total pancreatic lipomatosis with malabsorption and low serum amylase. In our case, chronic pancreatic duct obstruction by calculus proved to be the sole etiologic factor.
CASE REPORT
A 25-year-old woman presented to the hospital with a complaint of amenorrhea for 2 years, increased frequency of fatty stools, and decreased appetite for 6 months, generalized body swelling of 2 months duration, fever of 1 month duration, pain abdomen off and on. Physical examination revealed pallor and pitting edema of bilateral lower limbs. Respiratory and cardiovascular system examination revealed no abnormality. No past history of tuberculosis, diabetes mellitus, or hypertension. Ascitic tap revealed clear fluid (transudate). Laboratory investigations revealed decreased total protein, 4.4 g/dL (normal 6–8 g/dL); reduced albumin, 1.9 g/dL (normal 3.5—5 g/dL); and low serum amylase, 8 somogyi units (normal 20–200 somogyi units). Routine blood tests and liver and renal function tests were normal. Chest X-ray revealed left-sided pleural effusion. Ultrasound abdomen revealed hyperreflective pancreas [Figure 1a], free fluid within the pelvic cavity, and mildly dilated small bowel loops with thickened wall. Computed tomography revealed atrophic pancreas with complete fatty infiltration (attenuation value = –120 HU), and no demonstrable normal pancreatic parenchyma [Figure 1b and c]. Solitary calculus was noted within the pancreatic duct near the ampulla of Vater without pancreatic duct dilatation [Figure 1d]. There was no dilatation of intrahepatic biliary radicals or common bile duct. Small bowel wall thickening with increased intraluminal fluid and dilution of contrast medium was also evident [Figure 1e]. On the basis of the above-mentioned findings, the diagnosis of diffuse pancreatic lipomatosis (secondary to chronic pancreatic duct obstruction by calculus) leading to malabsorption, subsequently fatty steatorrhea, hypoproteinemia, and retention of fluid within the body was made.
Figure 1.
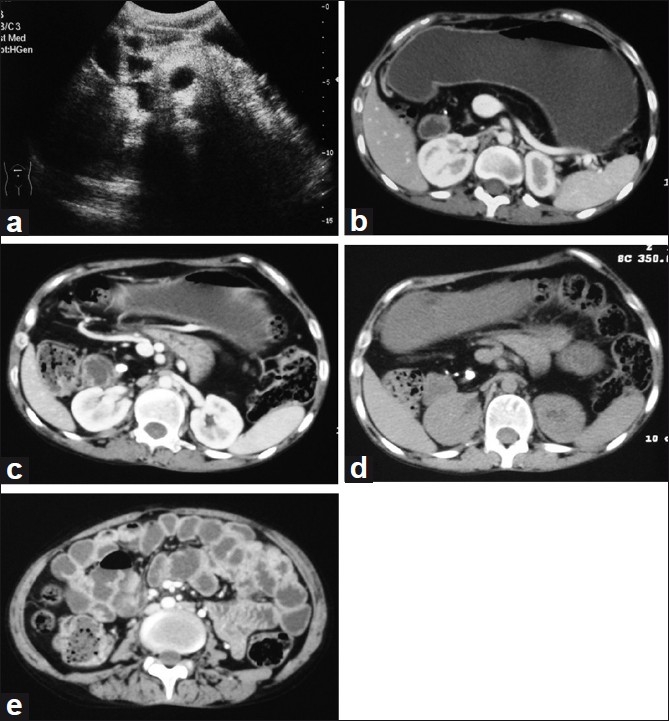
(a) Ultrasound abdomen demonstrates hyperreflective pancreas, indistinguishable from normal retroperitoneal fat; (b and c) contrastenhanced axial CT images demonstrate atrophic pancreas with total fat replacement. The entire pancreas has low attenuation value (HU = –120). Main pancreatic duct appears to be stenotic (rather than dilated), suggesting chronic severe obstruction; (d) noncontrast axial CT image shows solitary calculus in distal pancreatic duct near the ampulla of Vater; and (e) contrastenhanced axial CT image demonstrates mildly dilated small bowel loops with wall thickening and dilution of contrast medium
DISCUSSION
Recognition of total fatty replacement of pancreas is important for radiologists as it results in malabsorption due to pancreatic exocrine insufficiency.[2] The role of ultrasound in the diagnosis of pancreatic steatosis is very limited; first, because the overlying bowel gas causes obscuration of the pancreas and second, the fatty infiltration results in increased echogenicity of the pancreatic tissue making its differentiation difficult from normal retroperitoneal fat. However, cross-sectional imaging, namely, CT and MRI has an important role in the evaluation of pancreatic disease. CT is particularly useful in detecting specific etiologies, for example, pancreatic duct obstruction by the calculus or tumor. Unenhanced CT has negative attenuation value of pancreatic tissue replaced by the fat, therefore can reliably diagnose diffuse fatty change involving the pancreas. However, focal fatty change cannot be diagnosed confidently with CT alone, as on postcontrast images the normal pancreatic parenchyma entrapped between fatty replacement area shows contrast enhancement simulating a true mass.[3] Chemical shift MRI has advantage over CT in confirming the presence of focal fatty replacement of the pancreas. A characteristic loss of signal intensity on opposed-phase T1-weighted gradient-echo image as compared with corresponding in-phase image confirms the presence of microscopic lipid within the focal pancreatic mass detected on CT.[4] MRCP/ERCP demonstrates the status of pancreatic duct and the biliary tree. Selective pancreatic angiography is especially useful in differentiating pancreatic lipomatosis from dorsal agenesis by showing the pancreatic circulation.[5]
The exact etiopathogenesis behind fatty replacement is not known; however, several predisposing factors have been suggested. These include obesity, diabetes mellitus, chronic pancreatitis, hereditary pancreatitis, pancreatic duct obstruction by calculus or tumor, and cystic fibrosis.[6] Marked pancreatic lipomatosis with atrophy has been observed in adult patients secondary to pancreatic duct obstruction by calculi or carcinoma.[7] Under these circumstances, the obstructed pancreatic duct is stenotic rather than dilated, and typically has a smooth wall. Important differentials in case of stenotic pancreatic duct include dorsal agenesis of pancreas, pancreatic carcinoma and chronic pancreatitis.[7] In our case, chronic pancreatic duct obstruction by calculus was the sole etiologic factor responsible for severe degeneration of the pancreatic tissue. We found that the obstructed pancreatic duct was stenotic rather than dilated; and the complete fatty replacement of the pancreatic bed had resulted in severe pancreatic enzyme insufficiency, subsequently causing malabsorption, fatty steatorrhea, hypoproteinemia, and retention of fluid. Extensive fatty replacement of pancreas has been reported in past by few authors. Patel et al, demonstrated lipomatous pseudohypertrophy of pancreas with dilated pancreatic duct due to obstructing calculus in distal pancreatic duct.[8] Haunz et al reported fat replacement in tail and pancreas in a clinical study of 80 cases of carcinoma head of pancreas.[9] Pancreatic lipomatosis with stenotic pancreatic duct, secondary to pancreatic head adenocarcinoma after neoadjuvant chemoradiotherapy has been reported by Makay et al.[10]
Patients with total pancreatic lipomatosis have poor outcomes, and control of symptoms due to malabsorption has a major impact on the quality of life of these patients. Pancreatic enzyme supplementation in combination with dietary counseling is the mainstay of the treatment in these patients.
CONCLUSION
Clinicians must keep total pancreatic lipomatosis as a differential in a patient with malabsorption. CT can reliably exclude the disease.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Patel S, Bellon EM, Haaga J, Park CH. Fat replacement of the exocrine pancreas. AJR Am J Roentgenol. 1980;135:843–5. doi: 10.2214/ajr.135.4.843. [DOI] [PubMed] [Google Scholar]
- 2.Walters MN. Adipose atrophy of the pancreas. J Pathol Bacterial. 1966;92:547–57. doi: 10.1002/path.1700920232. [DOI] [PubMed] [Google Scholar]
- 3.Matsumoto S, Mori H, Miyake H, Takaki H, Maeda T, Yamada Y, et al. Uneven fatty replacement of the pancreas: Evaluation with CT. Radiology. 1995;194:453–8. doi: 10.1148/radiology.194.2.7824726. [DOI] [PubMed] [Google Scholar]
- 4.Kim HJ, Byun JH, Park SH, Shin YM, Kim PN, Ha HK, et al. Focal fatty replacement of the pancreas: Usefulness of chemical shift MRI. AJR Am J Roentgenol. 2007;188:429–32. doi: 10.2214/AJR.05.1095. [DOI] [PubMed] [Google Scholar]
- 5.Baek SY, Lee SC, Kim MY, Lee MG, Cho KS, Auh YH. CT findings of pancreas lipomatosis and associated diseases. J Korean Radiol Soc. 1992;28:749–53. [Google Scholar]
- 6.Soyer P, Spelle L, Pelage JP, Dufresne AC, Rondeau Y, Gouhiri M, et al. Cystic fibrosis in adolescents and adults: Fatty replacement of the pancreas- CT evaluation and functional correlation. Radiology. 1999;210:611–5. doi: 10.1148/radiology.210.3.r99mr08611. [DOI] [PubMed] [Google Scholar]
- 7.Nakamura M, Katada N, Sakakibara A. Huge lipomatou pseudohypertrophy of the pancreas. Am J Gastroenterol. 1979;72:171–4. [PubMed] [Google Scholar]
- 8.Patel S, Bellon EM, Hagga J, Park CH. Fat replacement of the exocrine pancreas. AJR Am J Roentgenol. 1980;135:843–5. doi: 10.2214/ajr.135.4.843. [DOI] [PubMed] [Google Scholar]
- 9.Haunz EA, Baggenstoss AH. Carcinoma of head of the pancreas. Arch Pathol. 1950;49:367–86. [Google Scholar]
- 10.Makay O, Kazimi M, Aydin U, Nart D, Yilmaz F, Zeytunlu M, et al. Fat replacement of the malignant pancreatic tissue after neoadjuvant therapy. Int J Clin Oncol. 2010;15:88–92. doi: 10.1007/s10147-009-0001-9. [DOI] [PubMed] [Google Scholar]


