Abstract
The association between pancreatitis and primary hyperparathyroidism (PHPT) is controversial. We report a 32-year-old man who presented with recurrent episodes of acute pancreatitis. Primary hyperparathyroidism was diagnosed after the fourth episode of pancreatitis. He had no additional risk factors for pancreatitis. Eighteen months after successful parathyroid surgery, there has been no recurrence of abdominal pain and his serum calcium is within the normal range.
Keywords: Pancreatitis, primary hyperparathyroidism, parathyroid surgery
INTRODUCTION
Primary hyperparathyroidism (PHPT) syndrome is an endocrine disorder, characterized by excessive secretion of parathyroid hormone from one or more parathyroid glands.[1] The elevation of PTH usually leads to hypercalcemia and hypophosphatemia; patients may present with classic skeletal disease, recurrent nephrolithiasis, or be asymptomatic, detected on routine biochemical screening. A dramatic increase in the incidence of PHPT occurred in the late 1960s, due primarily to the introduction of the multichannel autoanalyzer. The clinical profile of PHPT in the western countries had shifted from a symptomatic disorder, toward a more asymptomatic state.[2] However, PHPT has a variable clinical expression and symptomatic PHPT is still the predominant form of disease in many developing countries, with skeletal manifestation (osteitis fibrosis cystica) being very common.[3] Earlier studies from India have attributed the greater severity of PHPT to delayed diagnosis and widely prevalent vitamin D deficiency.[4]
Hypercalcemia is considered to be a rare cause of pancreatitis but the true cause and effect relationship between PHPT and pancreatitis remains controversial. PHPT has been associated with different types of pancreatitis. Despite its rarity, a cause and effect relationship is still suggested by the fact that parathyroidectomy seems to prevent recurrence of pancreatitis.[5]
Some patients suffer from 2 or more attacks of pancreatitis before a diagnosis of PHPT is made. We present a patient who had repeated admissions for acute pancreatitis, 4 episodes over a period of 15 months. PHPT was diagnosed after the fourth episode.
CASE REPORT
A 32-year-old man was first admitted to a district hospital with an episode of acute pancreatitis. He had elevated serum amylase and computed tomography (CT) abdomen revealed diffusely enlarged pancreas with irregular outline with no calcification or dilatation of main pancreatic duct [Figure 1]. CT abdomen did not reveal gall stones or nephrolithiasis. Over the next 15 months, he suffered 3 more episodes of acute pancreatitis. During the second episode, CT abdomen revealed focal necrosis in the body (less than 30%).
Figure 1.
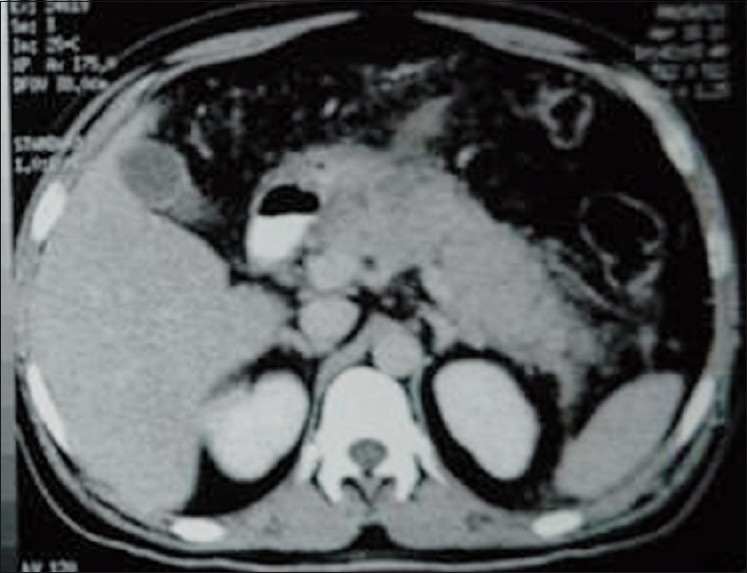
CT abdomen showing diffusely enlarged pancreas with irregular outline
For the fourth episode of acute pancreatitis, he was admitted in our institute. He denied any history of alcohol abuse and there was no family history of pancreatitis. Investigations revealed elevated serum amylase and lipase. Magnetic resonance cholangiopancreatography revealed diffusely edematous pancreas with no evidence of pancreatic divisum. Lipid profile was normal (total cholesterol 157 mg/dL, triglyceride 158 mg/dL, LDL cholesterol 85 mg/dL, and HDL cholesterol 40 mg/dL). The serum calcium was 10.4 mg/dL (normal range 8.8-10.5 mg/dl) and serum albumin was 4.6 g/dL. During the first 3 episodes of pancreatitis, the serum calcium was not estimated. The serum calcium at the upper limit of normal gave us clue that he may be having underlying hypercalcemic disorder.
After the episode of pancreatitis subsided, serum biochemical parameters were repeated. Repeat serum calcium was 13.1 mg/dL, phosphate 2.0 mg/dL, albumin 4.8 g/dL, and serum alkaline phosphatase was 284 U/L. Serum 25-hydroxyvitamin D was 10.31 ng/mL and serum iPTH was 610.7 pg/mL. On the basis of biochemical parameters a diagnosis of PHPT was made. Ultrasonography neck revealed a hypoechoic lesion 2.1 × 1.2 cm at the lower pole of left lobe of thyroid. Left inferior parathyroid adenoma was localized on a radionuclide parathyroid scan (99mTC MIBI) [Figure 2]. He denied any history of bone pains, bone fractures, neuropsychiatric symptoms, or muscle weakness.
Figure 2.
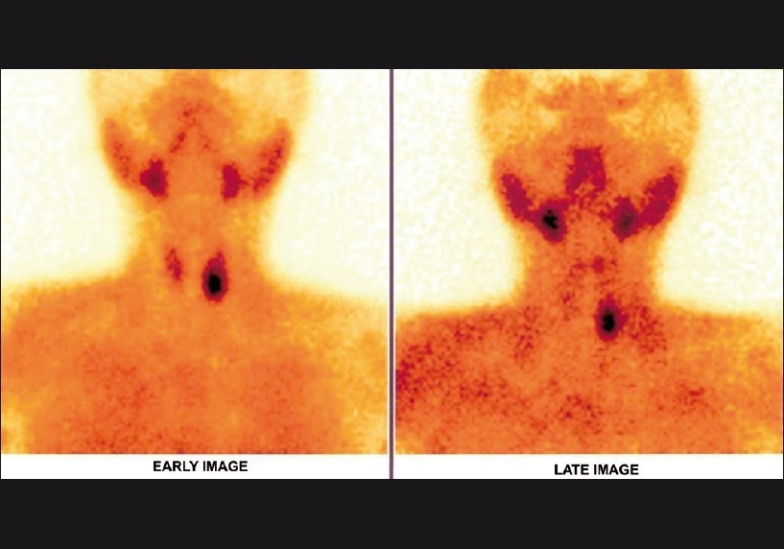
Radionuclide parathyroid scan (99mTC MIBI) showing left inferior parathyroid adenoma
Parathyroid adenoma was removed. The postoperative period was uneventful. Eighteen months after successful parathyroid surgery, there has been no recurrence of abdominal pain and his serum calcium is within the normal range. His current biochemical parameters are serum calcium 8.2 mg/dL; serum phosphorus 3.9 mg/dL; iPTH 32 pg/mL, and 25(OH) D3 29.33 pg/mL.
DISCUSSION
The association between pancreatitis and PHPT is controversial. The first report of PHPT associated with pancreatic lithiasis was published in 1947.[6] The Mayo Clinic experience between 1950 and 1975 found that out of 1153 patients with PHPT, only 17 (1.5%) had coexisting pancreatitis, and alternative explanations for pancreatitis were found for several patients.[7] But several studies have suggested a causal association between pancreatitis and PHPT.[8] The prevalence of acute pancreatitis in PHPT has been estimated to be between 1.5% and 13%.
PHPT has been associated with different types of pancreatitis, such as acute, subacute, or chronic calcifying pancreatitis.[9] A study involving 83 cases of pancreatitis combined with PHPT found that about 70% of the patients suffered from acute relapsing or chronic pancreatitis.[10] Some patients suffer from 2 or more attacks of pancreatitis before a diagnosis of PHPT is made. In a study from India, pancreatitis was associated in 6 of 87 patients (6.8%) with PHPT. Pancreatitis was the presenting symptom in 5 patients. All patients with a past history of pancreatitis had suffered two or more attacks.[11] In our patient there was a delay of 15 months before the diagnosis of PHPT was established. Serum calcium estimation after the first episode of pancreatitis would have eliminated this delay.. It is important to estimate serum calcium after an episode of unexplained pancreatitis. This will minimize the delay before the diagnosis of PHPT is made.
Despite its rarity, a cause and effect relationship is still suggested by the fact that parathyroidectomy seems to prevent recurrence of pancreatitis. Nearly 100% improvement in pancreatitis symptoms after the cure of PHPT has been reported.[12]
There are 2 mechanisms of hypercalcemia-induced pancreatitis. Hypercalcemia can lead to de novo activation of trypsinogen to trypsin, resulting in autodigestion of the pancreas and subsequent pancreatitis. Another explanation is that hypercalcemia leads to the formation of pancreatic calculi, ductal obstruction, and subsequent attacks of acute or chronic pancreatitis. Also, genetic risk factors may predispose patients with PHPT to pancreatitis. The calcium level is probably of major importance in the development of pancreatitis. The mean calcium values among patients with PHPT and pancreatic disease have been reported to be significantly higher than those in patients with PHPT without pancreatic involvement.[8]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bilezikian JP, Brandi ML, Rubin M, Silverberg SJ. Primary hyperparathyroidism: New concepts in clinical, densitometric and biochemical features. J Intern Med. 2005;257:6–17. doi: 10.1111/j.1365-2796.2004.01422.x. [DOI] [PubMed] [Google Scholar]
- 2.Mundy GR, Cove DH, Fisken R. Primary hyperparathyroidism changes in the pattern of clinical presentation. Lancet. 1980;1:1317–20. doi: 10.1016/s0140-6736(80)91783-3. [DOI] [PubMed] [Google Scholar]
- 3.Silverberg SJ, Sahne E, Dempster DW, Bilezikian JP. The effect of vitamin D insufficiency in patients with primary hyperparathyroidism. Am J Med. 1999;107:561–7. doi: 10.1016/s0002-9343(99)00294-6. [DOI] [PubMed] [Google Scholar]
- 4.Arya V, Bhambri R, Godbole MM, Mithal A. Vitamin D status and its relationship with bone mineral density in healthy Asian Indians. Osteoporos Int. 2004;15:56–61. doi: 10.1007/s00198-003-1491-3. [DOI] [PubMed] [Google Scholar]
- 5.Prinz RA, Aranha GV. The association of primary hyperparathyroidism and pancreatitis. Am Surg. 1985;51:325–9. [PubMed] [Google Scholar]
- 6.Martin L, Canseco JD. Pancreatic calculosis. JAMA. 1947;135:1055. doi: 10.1001/jama.1947.02890160013005. [DOI] [PubMed] [Google Scholar]
- 7.Bess MA, Edis AJ, van Heerden JA. Hyperparathyroidism and pancreatitis: Chance or a causal association? JAMA. 1980;243:246–7. [PubMed] [Google Scholar]
- 8.Jacob JJ, John M, Thomas N, Chacko A, Cherian R, Selvan B, et al. Does Hyperparathyroidism cause pancreatitis.A south Indian experience and a review of published work? ANZ J Surg. 2006;76:740–4. doi: 10.1111/j.1445-2197.2006.03845.x. [DOI] [PubMed] [Google Scholar]
- 9.Carnaille B, Oudar C, Pattou F, Combemale F, Rocha J, Proye C. Pancreatitis and Primary hyperparathyroidism: Forty cases. Aust N Z J Surg. 1998;68:117–9. doi: 10.1111/j.1445-2197.1998.tb04719.x. [DOI] [PubMed] [Google Scholar]
- 10.Terrise JF. Perparathyroidie et atteinte pancreatique. Thesis: Lyon, No. 89. 1968 [Google Scholar]
- 11.Agarwal A, George RK, Gupta SK, Mishra SK. Indian J Gastroenterol. 2003;22:224–5. [PubMed] [Google Scholar]
- 12.Mixter CG, Jr, Keynes WM, Cope O. Further experience with pancreatitis as a diagnostic clue to hyperparathyroidism. N Engl J Med. 1962;266:265–72. [Google Scholar]


