Abstract
Background
Complicated Grief (CG) is under consideration as a new diagnosis in DSM5. We sought to add empirical support to the current dialogue by examining the commonly used Inventory of Complicated Grief (ICG) scale completed by 782 bereaved individuals.
Methods
We employed IRT analyses, factor analyses, and sensitivity and specificity analyses utilizing our full sample (n=782), and also compared confirmed CG cases (n=288) to non-cases (n=377). Confirmed CG cases were defined as individuals bereaved at least 6 months who were seeking care for CG, had an ICG ≥ 30, and received a structured clinical interview for CG by a certified clinician confirming CG as their primary illness. Non-cases were bereaved individuals who did not present with CG as a primary complaint (including those with depression, bipolar disorder, anxiety disorders and controls) and had an ICG<25.
Results
IRT analyses provided guidance about the most informative individual items and their association with CG severity. Factor analyses demonstrated a single factor solution when the full sample was considered, but within CG cases, six symptom clusters emerged: 1) yearning and preoccupation with the deceased, 2) anger and bitterness, 3) shock and disbelief, 4) estrangement from others, 5) hallucinations of the deceased, and 6) behavior change, including avoidance and proximity seeking. The presence of at least one symptom from three different symptom clusters optimized sensitivity (94.8%) and specificity (98.1%).
Conclusions
These data, derived from a diverse and predominantly clinical help seeking population, add an important perspective to existing suggestions for DSM5 criteria for CG.
Keywords: complicated grief, symptoms, grief, loss, DSM, diagnostic criteria, factor analyses, IRT
Complicated grief (CG) is a recently described syndrome currently being considered for inclusion in the DSM5. Criteria have been proposed [1] based upon data primarily from elderly white widows, and analysis of additional data sets is needed. Developers of DSM5 consider their highest priority goal that of usefulness to clinicians diagnosing and treating patients. This paper provides additional empirical evidence through analyses of CG symptoms in a large clinical data set consisting of bereaved individuals with CG, anxiety disorders, mood disorders, and healthy controls. Study participants received clinician administered structured diagnostic assessments in three clinical research institutions. All participants completed the Inventory of Complicated Grief [ICG: 2], one of the most widely used assessment instruments in this field [e.g. 3; 4–7]. While a statistical methodology cannot, by itself, determine criteria for diagnosing CG, we believe that exploring the dimensional structure of the ICG, particularly in samples that include CG cases, is useful because 1) examination in a diverse bereaved sample with and without bereavement related symptoms can provide evidence that CG is a single construct (consistent with prior work: [1; 8], and 2) as a second level step, examination within the subgroup of CG cases can identify clusters of symptoms that are more likely to co-occur within the construct of CG. Such symptom clusters can be used as meaningful ways of combining symptoms in order to develop parsimonious, coherent diagnostic criteria. We hypothesized that 1) CG would be identified as a single construct in a diverse, variably symptomatic bereaved sample and 2) individuals with clinically confirmed CG could be differentiated from non-CG cases based on ICG symptom clusters with improved sensitivity and specificity once optimal clustering was identified within CG cases through factor analyses. This paper describes our study samples, analytic methods and results. We present our proposed criteria and a discussion of the literature about CG as a potential new diagnosis in a companion paper.
Methods
Study Sample
The study sample included 782 individuals recruited through public advertisement or clinical referral to participate in research studies at Columbia University, the University of Pittsburgh or Massachusetts General Hospital who reported the death of a loved one. All studies were approved by the local Institutional Review Board. All participants provided informed consent prior to participation. Participants from Pittsburgh and New York were 304 individuals who presented with CG as a chief complaint, and were evaluated for participation in an NIMH-funded treatment study of CG. Participants from Boston (n=478) were enrolled in one of 3 protocols examining psychological characteristics and/or biological markers of primary bipolar disorder (n=103), unipolar major depressive disorder (n=64), anxiety disorders (n=87 with social anxiety disorder, n=49 with panic disorder, n=36 with generalized anxiety disorder, and n=30 with posttraumatic stress disorder), complicated grief (n=14) or participated as a healthy control (n=95). Healthy controls participants were defined as those with no current or lifetime DSM-IV Axis 1 disorders, with the exception of specific phobia and a past history of alcohol or substance use disorders in remission for at least 12 months.
All participants were at least 18 years of age. Age, gender, race and ethnicity of each study sample are provided in Table 1. Detailed information was obtained from individuals presenting for CG treatment in Pittsburgh and New York; mean time since the loss was 5.5 ± 8.3 years with the loss occurring 6–12 months prior to evaluation in21%, 1–2 years in 20%, 2–5 years in 30%, and more than 5 years in 28%. Of these patients, 32% lost their spouses or other romantic partner, 30% lost parents, 23% children, 6% siblings, and 9% other friends or family. Violent deaths (i.e. accidents, suicide, or murder) made up 27% of these losses. Complete data on loss characteristics were not available for the MGH sample.
Table 1.
Demographic and Diagnostic Characteristics and Total ICG scores for the Full Bereaved Sample (n=782) and the Specific Subsamples Defined as Complicated Grief Cases (n=288) and Non-Cases (n=377)
| Full Bereaved Sample | Complicated Grief Cases | Non-Cases | ||
|---|---|---|---|---|
| n=782 | n=288 | n=377 | ||
| Gender | Male | 294 (38%) | 56 (20%) | 194 (51%) |
| Female | 482 (62%) | 231(80%) | 183 (49%) | |
| Missing n | 6 | 1 | 0 | |
| Race | Non-Hispanic White | 576 (77%) | 182 (70%) | 306 (82%) |
| Black/African | 108 (15%) | 63 (24%) | 35 (9%) | |
| American | ||||
| Asian | 5 (1%) | 4 (2%) | 1 (0.3%) | |
| Hispanic | 29 (4%) | 8 (3%) | 15 (4%) | |
| American Indian | 14 (2%) | 1 (0.4%) | 11 (3%) | |
| Other | 13 (2%) | 2 (1%) | 8 (2%) | |
| Missing n | 37 | 28 | 1 | |
| Age | Mean in years (SD) | 47.0 (14.6) | 52.7 (14.7) | 43.5 (13.2) |
| Missing n | 10 | 1 | 4 | |
| Primary Diagnosis | Complicated Grief | 318 (41%) | 288 (100%) | - |
| Bipolar | 103 (13%) | - | 79 (21%) | |
| GAD | 36 (5%) | - | 31 (8%) | |
| MDD | 64 (8%) | - | 48 (13%) | |
| PTSD | 30 (4%) | - | 17 (5%) | |
| Panic | 49 (6%) | - | 37 (10%) | |
| SAD | 87 (11%) | - | 74 (20%) | |
| No diagnosis | 95 (12%) | - | 91 (24%) | |
| Secondary Diagnoses for CG Cases | Bipolar | - | 3 (1%) | - |
| GAD | - | 60 (21%) | - | |
| MDD | - | 146 (51%) | - | |
| PTSD | - | 97 (34%) | - | |
| Panic | - | 30 (10%) | - | |
| SAD | - | 22 (8%) | - | |
| None of the above | - | 78 (27%) | - | |
| ICG Total score | Mean (SD) | 27.2(18.7) | 46.5 (9.3) | 10.2 (7.0) |
| [Min-Max] | [0–76] | [30–76] | [0–24] |
Assessments
Participants completed the 19-item Inventory of Complicated Grief [ICG: 2], a well validated measure with prior evidence for high internal consistency (Cronbach’s α = 0.94) and test-retest reliability [0.80: 2]. Symptoms related to the death of a loved one are rated as occurring 0=never, 1 = rarely, 2=sometimes, 3=often, 4=always. The mean and range of the ICG total scores for the study samples are provided in Table 1. Based on prior work [9–10], we dichotomized symptoms as present (often or always) or absent (not at all, rarely or sometimes) to best represent a clinically meaningful symptom level, and further to provide comparability of our results with other analyses performed on a similar set of symptoms [1]. Other psychiatric diagnoses were determined by experienced clinical interviewers certified as reliable in using the Structured Clinical Interview for DSM-IV [11], or the MINI International Neuropsychiatric Interview for DSM-IV [MINI Plus Version 5.0: 12].
Definition of Complicated Grief Cases and Non-cases
In order to devise CG criteria, an estimate of “caseness” was needed. As a first step, consistent with our prior treatment studies, we used a cut point of 30 or higher for the ICG total score (Shear et al 2005) and found n=362 CG cases based on this criterion alone. However, in order to focus on the most clinically meaningful group with additional evidence for CG, we ultimately defined “confirmed” CG cases as individuals who experienced the death of a loved one at least6 months earlier, scored 30 or higher on the ICG, self-identified with CG, and also had CG confirmed as their primary clinical problem in a structured clinical interview for CG by raters trained by KS. We compared these confirmed CG cases (n=288) to non-cases (n=377), defined as bereaved individuals who did not present with CG as a primary complaint (including those with depression, bipolar disorder, anxiety disorders and controls) and who scored less than 25 points on the ICG.
Statistical Methods
We first examined the underlying dimensional structure of the ICG across the full study population to determine whether CG emerges as a single disorder construct, and then separately within the subgroup of “confirmed” CG cases to determine how symptoms cluster within CG. To investigate the number of underlying dimensions, the magnitude of the eigenvalues associated with the tetrachoric correlation matrix of the 19 items was examined. The number of eigenvalues greater than 1 was identified and the associated percent of variability explained calculated. Exploratory factor analyses of dichotomous symptoms were performed using robust weighted least squares [WLSMV in Mplus 6.0: 13] and geomin orthogonal rotation, taking the number of factors to be equal to the respective number of eigenvalues greater than 1. Model adequacy (i.e. adequacy of the number of factors) was assessed using the chi-square goodness of fit test, CFI, and RMSEA and also importantly based on interpretability of the factors. Interpretation of the factor analysis results was guided by examining factor loadings relating each of the 19 symptoms to each of the underlying factors. To identify symptom clusters, we considered predominately the numerical results of the factor analyses and were further guided by content interpretability of the dimensions identified. Symptoms with a dominant loading (typically larger than 0.40) on just one factor were interpreted to be indicative of that factor. In instances where a symptom had multiple loadings larger than 0.40, or on the other extreme, no large loadings, content interpretation was used to guide the placement of the symptom into a symptom cluster [14]. In the full sample where a 1 factor model was adequate, we also fit the 2-parameter logistic item response theory (IRT) model and present estimates of the item discrimination and severity parameters, the item characteristic and information curves, as well as the predicted underlying trait. Factor analyses were conducted in Mplus 6.0 [15] and the IRT results were obtained using the latent trait modeling (“ltm”) in R2.10.1 [16].
The next step in our analyses was to assess sensitivity and specificity of different criteria in differentiating CG cases from non-cases. Individual symptoms on the ICG, clusters of symptoms identified by the factor analyses, and different rules based on counts of symptoms or symptom clusters were all examined. Sensitivity was calculated as the prevalence of the particular criteria in the confirmed CG cases (n=288) and specificity was calculated as one minus the prevalence of the particular criteria in the CG non-cases (n=377). The likelihood ratio of test positive, which indicates how many times more likely it is to see the criteria in the cases than in the non-cases, was calculated by taking the sensitivity divided by 1-sensitivity.
Results
Factor Analyses for the Full Bereaved Sample (n=782)
Eigenvalues associated with the tetrachoric correlation matrix for the ICG in the full sample yielded 3 values larger than 1:12.16, 1.28, and 1.02. The outlying large first eigenvalue indicates 64% (12.2/19) of the variability in the data can be explained with just one dimension, while 71% and 76% can be explained with the addition of 2 and 3 dimensions respectively. Results for the 1 through 3 factor analysis models are shown in Table 2, and indicate a single dimension measured simultaneously by all symptoms is empirically the best way to describe differences across the full sample. Also included in Table 2 are the item parameters for the 1 factor model corresponding to the IRT parameterization. The item with the largest discrimination parameter in the IRT (and likewise the largest factor loading in the one factor model) is “I feel that life is empty without the person who died” and the relatively lowest is “I have pain in the same area of my body as the person who died”. In IRT, items with larger discrimination parameters are interpreted as more reliable measures for the underlying trait at the specific location of the severity parameter. Of note, many of the discrimination parameters are extremely large; for example, because they are on the logit scale, a value of 4.2 indicates that the emptiness symptom has 66 times the odds of being reported for a person one standard deviation higher on the attribute scale. The corresponding item characteristic and information curves are shown in Figure 1.
Table 2.
Prevalence of Symptoms, Factor Analysis and IRT Parameter Estimates for Full Bereaved Sample (n=728)
| Prevalence | Factor analysis parametersa | IRT parametersb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1-factor | 2-factors | 3-factors | Severity | Discrimination | Imax | |||||
| 1 | 1 | 2 | 1 | 2 | 3 | |||||
| 13. I feel that life is empty without the person who died | 0.36 | 0.95 | 0.95 | . | 0.92 | . | . | 0.44 | 4.20 | 1.00 |
| 19. I feel lonely a great deal of the time ever since he/she died | 0.38 | 0.95 | 0.95 | . | 0.92 | . | . | 0.40 | 4.03 | 0.92 |
| 8. I feel stunned or dazed over what happened | 0.33 | 0.94 | 0.89 | . | 0.91 | . | . | 0.55 | 3.45 | 0.67 |
| 3. I feel I cannot accept the death of the person who died | 0.32 | 0.89 | 0.88 | . | 0.89 | . | . | 0.58 | 3.38 | 0.65 |
| 7. I feel disbelief over what happened | 0.36 | 0.95 | 0.91 | . | 0.92 | . | . | 0.44 | 3.36 | 0.64 |
| 4. I feel myself longing for the person who died | 0.47 | 0.92 | 0.93 | . | 0.90 | . | . | 0.11 | 3.32 | 0.62 |
| 1. I think about this person so much, it’s hard to do the things I normally do | 0.26 | 0.86 | 0.86 | . | 0.85 | . | . | 0.77 | 3.10 | 0.54 |
| 17. I feel bitter over this person’s death | 0.28 | 0.87 | 0.86 | . | 0.89 | . | . | 0.71 | 2.93 | 0.49 |
| 2. Memories of the person who died upset me | 0.42 | 0.86 | 0.87 | . | 0.87 | . | . | 0.26 | 2.85 | 0.46 |
| 16. I feel that it is unfair that I should live when this person died | 0.17 | 0.80 | 0.80 | . | 0.79 | . | . | 1.15 | 2.57 | 0.37 |
| 6. I can’t help feeling angry about his/her death | 0.32 | 0.85 | 0.84 | . | 0.86 | . | . | 0.61 | 2.54 | 0.37 |
| 10. Ever since he/she died I have lost the ability to care about other people | 0.22 | 0.79 | 0.79 | 0.43 | 0.77 | . | 0.47 | 0.99 | 2.20 | 0.27 |
| 9. Ever since he/she died it is hard for me to trust people | 0.24 | 0.73 | 0.73 | 0.41 | 0.73 | . | 0.51 | 1.00 | 1.83 | 0.19 |
| 15. I see the person who died stand before me | 0.04 | 0.64 | 0.62 | . | 0.58 | 0.53 | . | 2.44 | 1.76 | 0.18 |
| 18. I feel envious of others who have not lost someone close | 0.22 | 0.69 | 0.70 | . | 0.70 | . | . | 1.11 | 1.73 | 0.17 |
| 14. I hear the voice of the person who died speak to me | 0.04 | 0.61 | 0.60 | . | 0.55 | 0.55 | . | 2.54 | 1.72 | 0.17 |
| 5. I feel drawn to places and things associated with the person who died | 0.26 | 0.64 | 0.64 | . | 0.62 | . | . | 1.00 | 1.45 | 0.12 |
| 12. I go out of my way to avoid reminders of the person who died | 0.15 | 0.59 | 0.59 | . | 0.60 | . | . | 1.61 | 1.41 | 0.11 |
| 11. I have pain in the same area of my body as the person who died | 0.07 | 0.53 | 0.54 | . | 0.52 | . | . | 2.41 | 1.37 | 0.11 |
| Test Statistics | Chi-square | 671 | 426 | 223 | ||||||
| Df | 152 | 134 | 117 | |||||||
| Pvalue | <.0001 | <.0001 | <.0001 | |||||||
| RMSEA | 0.066 | 0.053 | 0.034 | |||||||
| CFI | 0.982 | 0.990 | 0.996 | |||||||
All factor loadings smaller than 0.40 are suppressed for ease of interpretation.
The Severity parameter represents the location (on the standardized trait scale) where the prevalence of the item is expected to be 0.5 which also corresponds to the location of maximum item information. The Discrimination parameter is directly proportional to the maximum item information (i.e., precision) for measuring the one underlying trait. Imax is the relative item information as compared to the overall most informative item (Q13: I feel that life is empty without the person who died)
Figure 1.
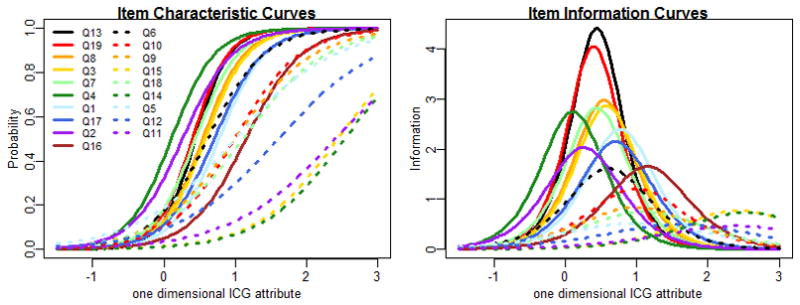
Figures below are based on analyses from the full sample n=728, and display IRT curves based on estimated item parameters presented in Table 2. Item characteristic curves show the probability of reporting the symptom at different levels of the underlying trait, and directly related to this, the item information curves show the precision with which the symptom measures the underlying trait at different levels of the trait (higher information indicates higher precision)
It was expected based on previous research [1] that a single dimension would emerge for the full sample. Within a sample population that exhibits a broad range of a given trait (e.g. ranging from none to many symptoms), it is common to empirically identify just one dominant dimension (i.e. one large eigenvalue) that characterizes an overall measure of low to high values of the trait. A large number of individuals (n=264: 34%) from the full bereaved sample exhibited none of the 19 symptoms with a rather normal and diverse distribution for the remaining number of symptoms. Furthermore we found that the IRT predicted trait level is highly correlated with the simple count of the number of symptoms (Pearson correlation = 0.98).
Factor Analyses for the “Confirmed” CG Case Sample (n=288)
We next examined the dimensional symptom structure in a targeted sample of people likely to have complicated grief. If the singular dimension for the attribute underlying the ICG found for the full sample were universally true, it would also hold for this upper end of the trait. Factor analyses repeated with identical methods revealed the first 6 eigenvalues were greater than 1: 5.4, 2.4, 2.2, 1.7, 1.4, 1.2, suggesting that 28%, 41%, 53%, 62%, 69%, and 75% of the variability could be explained by the first 6 dimensions respectively. There is substantial evidence just based on these eigenvalues that 1 dimension is not adequate to describe differences amongst these CG cases; thus, the singular dimension for the CG trait found for the full sample appears to not be universally true. The goodness of fit statistics for the 6 factor model were very good at CFI = 0.99, RMSEA = 0.022, Chi-square = 82.4 on df = 72 with a p-value = 0.19, but were also considered good for the 5 factor model CFI=0.98, RMSEA = 0.03, Chi-square = 108.4 on df = 86 with a p-value = 0.05. After examination of the specific items and factor loadings for both the 5 and 6 factor model, the 6 factor model appeared to provide the best interpretable fit to the underlying dimensions. These factors and items are described in Tables 3 and 4. Symptom clusters corresponding to the 6 factors were formed almost entirely based on empirically driven results motivated by clearly large loadings relating symptoms to factors. Two symptoms required investigator decision making to choose the most coherent cluster. ICG item 18 (“I feel envious of others who have not lost someone close”) did not show a strong loading with any factor and was placed into a cluster based on conceptually meaningful factor configuration. Item 2 (“memories of the person who died upset me”) had a loading of 0.42 with items 9 and 10, but also cross loaded with item 12 which loaded more heavily on factor 6 and ultimately was placed in the factor 6 cluster.
Table 3.
Exploratory Factor Analysis with Clinically Confirmed CG Cases (n=288). Factor loadings for 6-factor solution.
| 1 |
2 |
3 |
4 |
5 |
6 |
|
|---|---|---|---|---|---|---|
| 13. I feel that life is empty without the person who died. | 0.86 | 0.00 | 0.05 | 0.01 | 0.03 | 0.06 |
| 19. I feel lonely a great deal of the time ever since he/she died. | 0.85 | 0.09 | −0.06 | 0.24 | 0.11 | 0.02 |
| 4. I feel myself long for the person who died. | 0.83 | −0.02 | 0.08 | −0.38 | 0.02 | −0.12 |
| 1. I think about this person so much that it’s hard for me to do things I normally do. | 0.46 | −0.08 | 0.34 | 0.24 | 0.31 | −0.12 |
| 16. I feel that it is unfair that I should live when this person died. | 0.62 | 0.22 | 0.25 | 0.03 | −0.01 | −0.05 |
| 6. I can’t help feeling angry about his/her death. | −0.03 | 0.79 | 0.51 | 0.02 | 0.10 | 0.04 |
| 17. I feel bitter over this person’s death. | 0.12 | 0.77 | 0.36 | 0.12 | 0.04 | 0.06 |
| 7. I feel disbelief over what happened. | 0.30 | −0.02 | 0.94 | −0.22 | −0.07 | −0.02 |
| 8. I feel stunned over what happened. | 0.25 | 0.07 | 0.80 | −0.10 | 0.02 | −0.08 |
| 3. I feel I cannot accept the death of the person who died. | 0.31 | 0.01 | 0.65 | 0.03 | 0.11 | 0.09 |
| 10. Ever since he/she died, I feel like I have lost the ability to care about other people or I feel distant from people I care about. | 0.34 | 0.16 | 0.00 | 0.81 | −0.03 | −0.03 |
| 9. Ever since he/she died, it is hard for me to trust people. | 0.06 | 0.31 | −0.05 | 0.71 | −0.10 | −0.19 |
| 18. I feel envious of others who have not lost someone close. | 0.38 | 0.21 | 0.00 | 0.08 | −0.02 | 0.27 |
| 14. I hear the voice of the person who died speak to me. | 0.28 | 0.22 | −0.03 | 0.01 | 0.81 | −0.02 |
| 15. I see the person who died stand before me. | 0.28 | 0.03 | 0.22 | −0.07 | 0.78 | 0.16 |
| 11. I have pain in the same area of the body or have some of the same symptoms as the person who died. | 0.13 | 0.02 | 0.07 | 0.35 | 0.42 | 0.04 |
| 12. I go out of my way to avoid reminders of the person who died. | −0.03 | 0.09 | 0.30 | 0.46 | 0.17 | 0.52 |
| 2. Memories of the person who died upset me. | 0.31 | −0.10 | 0.29 | 0.42 | 0.01 | 0.15 |
| 5. I feel drawn to places and things associated with the person who died. | 0.25 | 0.00 | 0.19 | 0.02 | 0.36 | −0.51 |
All loadings > 0.4 are highlighted in bold..
Table 4.
ICG Symptom Clusters in Confirmed CG Cases Based on Six Factor Model
SYMPTOM CLUSTER 1: “Yearning and preoccupation with the deceased”
|
SYMPTOM CLUSTER 2: “Anger and bitterness”
|
SYMPTOM CLUSTER 3: “Shock and disbelief”
|
SYMPTOMCLUSTER 4:”Estrangement from others”
|
SYMPTOM CLUSTER 5: “Hallucinations of the deceased”
|
SYMPTOM CLUSTER 6: “Behavior change, including avoidance or proximity seeking”
|
Item 18 did not empirically load highly with any factors but was chosen to group in Symptom Cluster4 because it was conceptually most meaningful there.. Item 2 empirically loaded more strongly with Factor 4, but due to its cross loading also with 12 and because of conceptual interpretability, it is included in Symptom Cluster 6.
Sensitivity and Specificity Analyses
Table 5 shows sensitivity and specificity for each ICG symptom, ordered from most to least sensitive for discriminating CG cases from non-cases. Longing (item 4) was the most sensitive item, though this item alone failed to capture 11.5% of the confirmed CG cases, and was reported by 9.3% of non-cases. All items showed specificity above 90%, with 2 items present only in CG cases (“I feel that it is unfair that I should live when this person died” and “I hear the voice of the person who died speak to me”).
Table 5.
Sensitivity and Specificity of ICG Items in Complicated Grief Cases vs. Non-cases
| Prevalence in cases (n=288) | Prevalence in non-cases (n=377) | Specificity (1-false positive rate) | Likelihood ratio of test positive | |
|---|---|---|---|---|
| Sensitivity (true positive rate) | False positive rate | |||
| 4. I feel myself longing for the person who died | 88.5% | 9.3% | 90.7% | 9.5 |
| 2. Memories of the person who died upset me | 81.9% | 7.2% | 92.8% | 11.4 |
| 19. I feel lonely a great deal of the time ever since he/she died | 80.9% | 2.4% | 97.6% | 33.9 |
| 13. I feel that life is empty without the person who died | 80.2% | 1.9% | 98.1% | 43.2 |
| 7. I feel disbelief over what happened | 76.4% | 3.7% | 96.3% | 20.6 |
| 8. I feel stunned or dazed over what happened | 71.2% | 1.9% | 98.1% | 38.3 |
| 3. I feel I cannot accept the death of the person who died | 70.1% | 1.9% | 98.1% | 37.8 |
| 6. I can’t help feeling angry about his/her death | 64.6% | 3.7% | 96.3% | 17.4 |
| 1. I think about this person so much, it’s hard to do the things I normally do | 61.1% | 1.3% | 98.7% | 46.1 |
| 17. I feel bitter over this person’s death | 61.1% | 2.1% | 97.9% | 28.8 |
| 9. Ever since he/she died it is hard for me to trust people | 49.0% | 2.4% | 97.6% | 20.5 |
| 10. Ever since he/she died I have lost the ability to care about other people | 47.9% | 1.6% | 98.4% | 30.1 |
| 5. I feel drawn to places and things associated with the person who died | 46.5% | 5.3% | 94.7% | 8.8 |
| 18. I feel envious of others who have not lost someone close | 45.1% | 2.7% | 97.3% | 17.0 |
| 16. I feel that it is unfair that I should live when this person died | 40.6% | 0.0% | 100.0% | *9999 |
| 12. I go out of my way to avoid reminders of the person who died | 32.3% | 2.4% | 97.6% | 13.5 |
| 11. I have pain in the same area of my body as the person who died | 12.8% | 1.3% | 98.7% | 9.7 |
| 15. I see the person who died stand before me | 10.8% | 0.3% | 99.7% | 40.6 |
| 14. I hear the voice of the person who died speak to me | 9.7% | 0.0% | 100.0% | *9999 |
Values of 9999 are given for those cases where the ratio is estimated to be infinite (due to a zero false positive rate in the non-case group).
Likelihood ratio of test positive= sensitivity/(1-specificity).
We next examined sensitivity and specificity of the presence of at least one symptom from each cluster, as well as sensitivity and specificity of different numbers of symptom clusters required. The results, shown in Table 6, indicate that the presence of at least one symptom from items representing the “yearning and preoccupation” cluster would have the greatest sensitivity, capturing 96.9% of CG cases, with a specificity of 88.3%. The most specific cluster was Symptom Cluster5 (items 11, 14, 15: “hallucinations of the deceased”), with a specificity of 98.4%, but sensitivity of only 24%. For each of the remaining 4 clusters, the presence of at least one threshold level symptom was highly prevalent in cases (range 72.6%to 92.4%) with excellent specificity (range 86.2%to 94.7%).
Table 6.
Sensitivity and Specificity of Symptom Clusters and of Numbers of Clusters in Confirmed CG Cases vs. Non-Cases
| Prevalence in cases (n=288) | Prevalence in non-cases (n=377) | . | . | |
|---|---|---|---|---|
| Sensitivity | False positive | Specificity | lrpositive | |
| Symptom Clusters | ||||
| 1. Yearning and preoccupation with the deceased | 96.9% | 11.7% | 88.3% | 8.30 |
| 2. Anger and bitterness | 72.6% | 5.3% | 94.7% | 13.68 |
| 3. Shock and disbelief | 87.2% | 6.1% | 93.9% | 14.29 |
| 4. Estrangement from others | 76.7% | 5.8% | 94.2% | 13.15 |
| 5. Hallucinations of the deceased | 24.0% | 1.6% | 98.4% | 15.05 |
| 6. Behavior change, including avoidance or proximity seeking | 92.4% | 13.8% | 86.2% | 6.70 |
| Number of Symptom Clusters | ||||
| At least1 | 100.0% | 31.0% | 69.0% | 3.22 |
| At least2 | 99.3% | 11.1% | 88.9% | 8.91 |
| At least3 | 94.8% | 1.9% | 98.1% | 51.05 |
| At least4 | 86.5% | 0.3% | 99.7% | 325.95 |
| At least5 | 54.9% | 0.0% | 100.0% | *9999 |
| All 6 | 14.2% | 0.0% | 100.0% | *9999 |
| Symptom Cluster1 And | ||||
| At least 1 from 2–6 | 96.5% | 6.1% | 93.9% | 15.82 |
| At least 2 from 2–6 | 93.8% | 1.3% | 98.7% | 70.69 |
| At least 3 from 2–6 | 85.8% | 0.3% | 99.7% | 323.33 |
| At least 4 from 2–6 | 54.9% | 0.0% | 100.0% | *9999 |
| All 5 from 2–6 | 14.2% | 0.0% | 100.0% | *9999 |
Values of 9999 are given for those cases where the ratio is estimated to be infinite (due to a zero false positive rate in the non-case group).
Lrpositive= likelihood ratio of test positive= sensitivity/(1-specificity).
When different combinations of symptom clusters were considered together, requiring a larger number of clusters be present resulted in higher specificity but lower sensitivity. For example, 100% of the CG cases had a threshold symptom in at least one cluster, but the false positive rate was 31%. At the other end of the spectrum, no non-cases had a threshold symptom in 5 or more clusters, but sensitivity dropped to 54.9% for cases. A requirement of symptoms from at least 3 different symptom clusters optimized both sensitivity (94.8%) and specificity (98.1%). Given the proposal by Prigerson’s group for an anchor criterion that focuses on yearning, we performed conditional analyses examining how many additional clusters optimize sensitivity and specificity when at least one symptom from the “yearning and preoccupation” cluster is required. Results indicated sensitivity of 93.8% and a specificity of 98.7% with at least 2 additional symptom clusters endorsed.
Discussion
These data indicate how CG symptoms cluster in a large clinical sample of patients with CG, and how such clusters can be employed to optimize sensitivity and specificity for identification of CG cases. Our results resemble prior work showing that a single factor solution fits best in a sample of bereaved individuals with a wide range of grief related symptom severity [1; 8]. This result provides support for a general construct of CG that discriminates people with no symptoms from those with increasing numbers of symptoms. Indeed, a large number of individuals (n=264: 34%) did not endorse any of the ICG items at the level of often or more, and the single factor IRT model predicted CG trait levels to be highly correlated with the simple count of number of symptoms present. The symptoms found to best discriminate between individuals across the single general construct of CG were similar to those previously reported in bereaved populations [1; 8]. Loneliness and feeling life is empty were the most discriminating (i.e. most informative), but all of the symptoms were highly informative for the general construct of CG, as is indicated by all discrimination parameters being larger than 1.
A richer understanding of the nature of CG emerged when we repeated our analyses in clinically “confirmed” CG cases alone. Six distinct clinically meaningful dimensions emerged from the factor analysis including: 1) yearning and preoccupation with the deceased, 2) anger and bitterness, 3) shock and disbelief, 4) estrangement from others, 5) hallucinations of the deceased, and 6) behavior change, including avoidance and proximity seeking. This factor analytic approach can guide parsimonious inclusion of symptoms as diagnostic criteria. For example, although longing was the most commonly reported symptom (88.5% in CG cases), it was not found to be unique, but rather clustered with other symptoms of separation distress: loneliness, preoccupation with the loved one, feeling life is now empty, and feeling it is unfair to live while the loved one died. This cluster of symptoms measuring separation distress yielded very good sensitivity (96.9%) and specificity (88.3%). Bitterness and anger also clustered, were present in nearly three quarters of CG cases, and yielded high specificity (94.7%). Symptoms of shock and disbelief together were highly prevalent (87.2%) with good specificity (93.9%). Interpersonal symptoms of “estrangement from others” emerged as a cluster as well, with at least one symptom present in more than three quarters of cases (76.7%), again with good specificity (94.2%). Avoidance of reminders clustered with distress about memories and proximity seeking (symptom cluster6), with a sensitivity of 92.4% and specificity of 86.2%.
In criteria development, empirical data should be considered alongside other available research and clinical experience; as an example, avoidance is understood to be a difficult construct to assess since people avoid thinking about things they avoid. Nevertheless, studies confirm that avoidance is important in CG [17], and psychotherapy for CG targets this symptom [17–20]. Further, our clinical experience with CG patients is consistent with the co-occurrence of compulsive proximity seeking behaviors (e.g. compulsively viewing photos, or refraining from washing things that belonged to the deceased to retain their smell) and avoidance behaviors (e.g. avoidance of favorite places shared with the deceased, unwillingness to alter areas of the house).
Another finding that emerged from our factor analysis was the clustering of “hallucinatory” symptoms. While these symptoms were not among the more common or most informative according to item IRT analyses, or even as a cluster (25%prevalence), they were highly specific (less than 2% of non-CG bereaved individuals reported at least one of them)and also mapped to the highest levels of CG severity in the IRT analysis. Thus, this symptom cluster may be considered a marker for a more severe CG diagnosis. Similar results were observed by Boelen et al, who also suggested that these symptoms be candidates for diagnostic criteria [8].
This study has a number of strengths that increase confidence in the findings. All subjects were well characterized, including structured psychiatric diagnostic assessment by certified experienced clinical raters. The sample includes a wide range of ages and has a moderate degree of racial/ethnic diversity. Further, the sample includes a large group of individuals who self-identified as having CG, had a high level of ICG symptoms and were confirmed by an experienced clinician to have CG. Losses in this “confirmed” CG case cohort include parents and children in addition to romantic partners, and include death by homicide, suicide, accident and natural causes. In addition, there is a large group of bereaved individuals with a mood or anxiety disorder, as well as those without disorder.
There are also some weaknesses of our sample. In order to optimize the sample size and include a wide range of individuals, we combined data across three sites from different studies, and there was thus a lack of systematic recruitment resulting in a lack of complete data about the characteristics of the loss and a much smaller proportion of CG treatment seeking individuals in the MGH sample. We were also limited to the use of only a few clinical research based sites (MGH, University of Pittsburgh and NYSPI), somewhat limiting generalizability to community settings. Selection of the6 factor model in the CG cases, as well as the placement of items 2 and 18 were based on clinical interpretation, a procedure that is consistent with standard practice in factor analysis [14] and with recommendations by Kraemer and colleagues [21] regarding collaborations between clinicians and statisticians in the interpretation of data informing DSM diagnoses. Finally, findings are limited by the questions asked in the ICG itself.
In conclusion, these data add an important perspective to existing suggestions for DSM5 criteria for CG. Ideally, diagnostic criteria should discriminate ill from not ill people, including both healthy controls and patients with other psychiatric disorders. However, this is not the only goal of the criteria. A second goal is to provide away for clinicians to understand the syndrome of CG and where a given patient fits within the spectrum of people with CG. Our analyses of CG symptom frequency and clustering, derived from a large, diverse and predominantly clinical help-seeking population who underwent rigorous evaluation procedures, provide one example of how empirical data can offer guidance for DSM criteria development. Additional investigation including replication of our analyses, field testing and biological, clinical and epidemiologic research is needed to further test and refine the diagnosis of CG.
Acknowledgments
This study was supported by a Massachusetts General Hospital Claflin Distinguished Scholar Award (NS), a National Institute of Mental Health Grant 1R01MH077700(NS), and funding from the Highland Street Foundation (MGH). The present study was also supported by two National Institute of Mental Health grants awarded to Dr. Shear, MH60783and MH70741.
Footnotes
Conflicts of Interest: Naomi Simon: Research grants (American Foundation for Suicide Prevention, Astra Zeneca, Cephalon, Highland Street Foundation, Forest Laboratories, NARSAD, NIMH, Glaxo SmithKline, Janssen, Lilly, Pfizer, Sepracor, UCB-Pharma), payment for manuscript preparation (Astra Zeneca), payment for the development of educational presentations (Pfizer),
Melanie Wall: None
Aparna Keshaviah: None
M. Taylor Dryman: None
Nicole LeBlanc: None
M. Katherine Shear: Research grants (NIH), support for travel (NIH), and payment for the development of educational materials (ADEC webinar, the University of Manitoba, Winnipeg, & the University of Memphis).
References
- 1.Prigerson HG, Horowitz MJ, Jacobs SC, et al. Prolonged grief disorder: Psychometric validation of criteria proposed for DSM-IV and ICD-11. PLoS Medicine. 2009;6(8):e1000121. doi: 10.1371/journal.pmed.1000121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Prigerson HG, Maciejewski PK, Reynolds CF, III, et al. Inventory of Complicated Grief: A scale to measure maladaptive symptoms of loss. Psychiatry Research. 1995;59(1–2):65–79. doi: 10.1016/0165-1781(95)02757-2. [DOI] [PubMed] [Google Scholar]
- 3.Ott CH. The impact of complicated grief on mental and physical health at various points in the bereavement process. Death Studies. 2003;27(3):249–272. doi: 10.1080/07481180302887. [DOI] [PubMed] [Google Scholar]
- 4.Mitchell AM, Kim Y, Prigerson HG, Mortimer MK. Complicated grief and suicidal ideation in adult survivors of suicide. Suicide and Life-Threatening Behavior. 2005;35(5):498–506. doi: 10.1521/suli.2005.35.5.498. [DOI] [PubMed] [Google Scholar]
- 5.Simon NM, Pollack MH, Fischmann D, et al. Complicated Grief and Its Correlates in Patients With Bipolar Disorder. Journal of Clinical Psychiatry. 2005;66(9):1105–1110. doi: 10.4088/jcp.v66n0903. [DOI] [PubMed] [Google Scholar]
- 6.Kersting A, Kroker K, Horstmann J, et al. Association of MAO-A variant with complicated grief in major depression. Neuropsychobiology. 2007;56(4):191–196. doi: 10.1159/000120624. [DOI] [PubMed] [Google Scholar]
- 7.Keesee NJ, Currier JM, Neimeyer RA. Predictors of grief following the death of one’s child: The contribution of finding meaning. Journal of Clinical Psychology. 2008;64(10):1145–1163. doi: 10.1002/jclp.20502. [DOI] [PubMed] [Google Scholar]
- 8.Boelen PA, Hoijtink H. An item response theory analysis of a measure of complicated grief. Death Studies. 2009;33(2):101–129. doi: 10.1080/07481180802602758. [DOI] [PubMed] [Google Scholar]
- 9.Prigerson HG, Shear MK, Jacobs SC, et al. Consensus criteria for traumatic grief: A preliminary empirical test. British Journal of Psychiatry. 1999;174:67–73. doi: 10.1192/bjp.174.1.67. [DOI] [PubMed] [Google Scholar]
- 10.Prigerson HO, Jacobs SC. Traumatic grief as a distinct disorder: A rationale, consensus criteria, and a preliminary empirical test. In: Stroebe MS, Hansson RO, Stroebe W, Schut H, editors. Handbook of bereavement research: Consequences, coping, and care. Washington, DC US: American Psychological Association; 2001. pp. 613–645. [Google Scholar]
- 11.First MB, Spitzer RL, Gibboon M, Williams JBW. Structured Clinical Interview for DSM IV Axis I Disorders. New York, NY: New York State Psychiatric Institute; 1994. [Google Scholar]
- 12.Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. Journal of Clinical Psychiatry. 1998;59(Suppl 20):22–33. [PubMed] [Google Scholar]
- 13.Flora DB, Curran PJ. An Empirical Evaluation of Alternative Methods of Estimation for Confirmatory Factor Analysis With Ordinal Data. Psychological Methods. 2004;9(4):466–491. doi: 10.1037/1082-989X.9.4.466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nunnally JC, Bernstein IH. Psychometric Theory. New York, NY: McGraw-Hill Series in Psychology; 1994. [Google Scholar]
- 15.Muthen LK, Muthen BO. Mplus User’s Guide. Los Angeles, CA: Muthen & Muthen; 1998–2010. [Google Scholar]
- 16.Rizopoulos D. An R package for latent variable modeling and item response theory analyses. Jounral of Statistical Software. 2006;17(5):1–25. ltm. [Google Scholar]
- 17.Shear K, Monk T, Houck P, et al. An attachment-based model of complicated grief including the role of avoidance. European Archives of Psychiatry and Clinical Neuroscience. 2007;257(8):453–461. doi: 10.1007/s00406-007-0745-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shear K, Frank E, Houck PR, Reynolds CF., III Treatment of Complicated Grief: A Randomized Controlled Trial. JAMA: Journal of the American Medical Association. 2005;293(21):2601–2608. doi: 10.1001/jama.293.21.2601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Boelen PA, van den Hout MA. The role of threatening misinterpretations and avoidance in emotional problems after loss. Behavioural and Cognitive Psychotherapy. 2008;36(1):71–87. [Google Scholar]
- 20.Boelen PA, van den Bout J, van den Hout MA. A prospective examination of catastrophic misinterpretations and experiential avoidance in emotional distress following loss. Journal of Nervous and Mental Disease. 2010;198(4):252–257. doi: 10.1097/NMD.0b013e3181d619e4. [DOI] [PubMed] [Google Scholar]
- 21.Kraemer HC, Shrout PE, Rubio-Stipec M. Developing the Diagnostic and Statistical Manual V: What will ‘statistical’ mean in DSM-V? Social Psychiatry and Psychiatric Epidemiology. 2007;42(4):259–267. doi: 10.1007/s00127-007-0163-6. [DOI] [PubMed] [Google Scholar]


