Abstract
INTRODUCTION
Immediate breast reconstruction after mastectomy has known psychological and financial advantages but it is difficult to compare the outcome of various methods of reconstruction. Re-operation rates are an objective measure of surgical intervention required to attain and maintain acceptable cosmesis.
PATIENTS AND METHODS
A series of 95 patients (110 immediate reconstructions) was analysed for number of re-operations required within 5 years of initial surgery, magnitude of procedures, ‘survival’ of the reconstruction and effect of radiotherapy.
RESULTS
Although more intervention was seen in patients with implant-based reconstruction and the time-course over which autologous and implant-based reconstructions fail is different these did not reach statistical significance. Radiotherapy has a significant effect on failure of implant-based reconstruction.
CONCLUSIONS
Long-term, large studies of immediate reconstruction are required to assess adequately the impact of type of reconstruction on re-operation rates. The National Mastectomy and Breast Reconstruction Audit is ideally placed to provide answers to remaining questions about longevity of immediate breast reconstruction and the effect that late failure has on patient satisfaction.
Keywords: Immediate breast reconstruction, Re-operation rate, Outcome
The aim of immediate breast reconstruction is restoration of the breast mound at the time of mastectomy. The psychological and financial advantages have been reported.1,2 Immediate reconstruction has been facilitated by the development of skin-sparing mastectomy which has cosmetic advantages3 without detriment to the oncological outcome,4 but with some evidence that major complications are more common than for delayed reconstructions.5 Broadly, three techniques of reconstruction are widely available: (i) tissue expander/implant reconstruction; (ii) pedicled latissimus dorsi (LD) flap (with or without an implant); and (iii) transfer of abdominal fat in the form of a transverse rectus abdo-minis myocutaneous (TRAM) flap or a perforator flap using the same abdominal skin and fat but no muscle, based on deep inferior epigastic perforator vessels (DIEP). Alternative free flaps using buttock or thigh fat are offered in some centres.
Comparisons between techniques of reconstruction are few in number and have short follow-up.3,6 Longer term results are given in some series focusing on a single operative technique.7–9 Relevant outcome measures of immediate breast reconstruction include aesthetic results, patient satisfaction and re-operation rates, yet each measure has drawbacks. Patient satisfaction may be the ultimate end-point since the reason for reconstruction is the psychological well-being of the patient. However, patients cannot be entirely objective and this does not enable comparisons between techniques. Measurement of aesthetic result is complex and, although panel assessments can be reproducible, aesthetic appearance changes over time and the final result conceals the steps required to reach that appearance. Re-operations are an objective measure of surgical intervention required to attain and maintain acceptable cosmesis. No long-term comparative studies were found in the literature.
We investigated a series of patients who had undergone mastectomy and immediate breast reconstruction. Implant-based reconstructions (either tissue-expander/implant-only, or LD flap with implant) were compared with autologous reconstructions (LD without an implant or DIEP flap). The focus was on the number of re-operations within the first 5 years of follow-up and the time-course over which these took place. The aim of this study was to compare autologous with implant-based reconstruction in terms of the: (i) number of revision operations occurring in a 5-year follow-up period; (ii) rate of re-operation over time; (iii) time course of reconstructive failure; and (iv) impact of radiotherapy.
Patients and Methods
A prospectively-collected list of patients undergoing skin-sparing mastectomy with immediate reconstruction performed by one breast surgeon (DE) and one plastic surgeon (RW), i.e. a constant team, was consulted. Hospital notes were examined. Data on patient age at the time of reconstruction, smoking history, and mastectomy weight were noted. Likewise, pathological data including tumour size and type, nodal involvement, and use of adjuvant chemotherapy, radiotherapy and endocrine therapy were recorded. The type of reconstruction performed and number of re-operations were documented. The main focus of this study was on the number of re-operations that occurred as planned procedures and the time-course over which these occur.
If a reconstruction failed, requiring a different technique of reconstruction to be used, further surgery to revise the second reconstruction was not a direct result of the primary reconstruction. The patient was, therefore, ‘censored’ at the time of failure. Likewise, development of local or distant recurrent disease changes the threshold for cosmetic intervention so patients with recurrence were also censored.
Statistical analysis
The focus of this study was the number of re-operations occurring for each patient. In order to eradicate the effect of different duration of follow-up in the two groups, a 5-year follow-up period was selected. The number of re-operations required by each group were compared using the Mann-Whitney test. The Mann-Whitney test was also used to examine the effect of radiotherapy on re-operation rates. These analyses were undertaken on a per-patient basis (having first established that there was no difference between unilateral and bilateral cases).
Since our second hypothesis was that the time-course over which re-operations occur is different in the two groups, the rate (number of patients having surgery in a year divided by the number of uncensored patients in that year of follow-up) was calculated and depicted graphically.
Completion of 5 years of follow-up was required for inclusion in the comparison of long-term rates of re-operation. This overlooks patients whose reconstruction fails within that time. However, reconstructive failure is a very important measure. This was compared on a ‘per breast’ basis using a Kaplan-Meier analysis with a log rank test for heterogeneity of the groups.
Results
Demographics
Ninety-five patients were identified. Fifteen cases were bilateral, thus 110 breast reconstructions were included in this study. The mean age of patients was 46.5 years (range, 22–67 years). Eighty (73%) were therapeutic mastectomies and 30 (27%) were risk-reducing. Thirty-seven reconstructions were DIEP flaps, 13 autologous latissimus dorsi myocutaneous flaps, 43 LD with implant and 17 tissue-expander/implant only reconstructions. Seven cases were done for local recurrence. Eleven patients had previously had unilateral breast radiotherapy (i.e. prior to mastectomy and immediate breast reconstruction) and 26 patients had unilateral post-reconstruction adjuvant radiotherapy. Sixty-nine reconstructions did not receive radiotherapy. Radiotherapy data were not available for four patients. The median duration of follow-up for the whole cohort was 4.4 years (interquartile range, 2.1–7.1 years).
Histology and adjuvant treatment
The mean invasive tumour size was 23 mm (range, 1–120 mm). Twenty-two were invasive ductal carcinoma, eight were invasive lobular and seven were mixed. Thirty-six of the 80 patients undergoing therapeutic mastectomy had extensive DCIS. Of the 80 therapeutic mastectomy cases, 16 had positive nodes.
Number of re-operations in the first 5 years after immediate reconstruction
Among the 35 patients with a full 5 years of follow-up (i.e. reached 5 years with no recurrence and no reconstructive failure), the median number of re-operations was 1.0 and the mean 1.65. Table 1 summarises the data by reconstruction type. Overall, 75% of autologous reconstruction patients and 87% of implant-based reconstruction patients underwent at least one operation. Using the Mann-Whitney test, no statistically significant difference was found between the number of re-operations in the autologous and implant-based groups (P = 0.20). The mean number of re-operations is higher in the implant-based reconstructions than autologous reconstructions and it is likely that this study lacks the power to detect a significant difference. A power calculation based on our data suggests that 176 patients would be needed to give an 80% power to detect a difference in the number of re-operations at 5 years at the 0.05 level.
Table 1.
Number of re-operations for the 35 patients with a full 5 years of follow-up
| Number | Mean | SD | LQ | Median | UQ | |
|---|---|---|---|---|---|---|
| Autologous | 12 | 1.33 | 1.37 | 0.75 | 1.00 | 2.00 |
| Implant-based | 23 | 1.83 | 1.40 | 1.00 | 2.00 | 2.00 |
SD, standard deviation; LQ, lower quartile; UQ, upper quartile.
No significant difference P= 0.20
Rate of re-operation varies with type of reconstruction and time
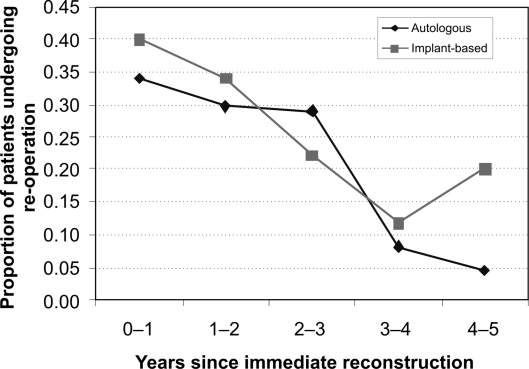
The rate of re-operation following both autologous and implant-based reconstruction was very similar, both showing a decreasing trend with time. Neither group reached zero by years 4–5 (Fig. 1).
Figure 1.
Rate of re-operations over time since primary reconstruction. The table reports the number of patients ‘at risk’ for each year of follow-up.
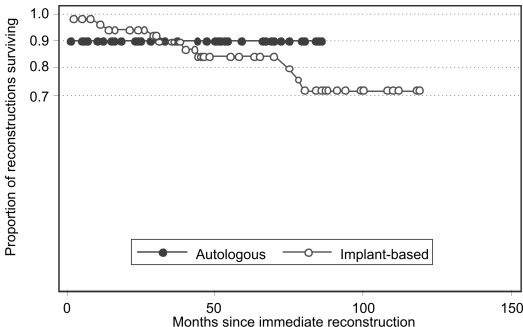
Time-course of failure varies with type of reconstruction
The re-operation data presented so far censors patients at the time of failure of the reconstruction or diagnosis of recurrent disease. However, failure requiring secondary reconstruction is an important element of re-operation after immediate reconstruction. None of the autologous LD flaps failed. All DIEP failures occurred within the first postoperative week, while implant-based reconstructions suffered from a gradual attrition up to, and including, the sixth year offollow-up (Fig. 2). Using the log-rank test for heterogeneity, the difference between reconstruction types was not statistically significant (P = 0.58). This lack of statistical significance may reflect a lack of power in this study but, importantly, the difference may still be clinically and financially significant.
Figure 2.
Kaplan-Meier curve of survival of autologous and implant-based breast reconstruction.
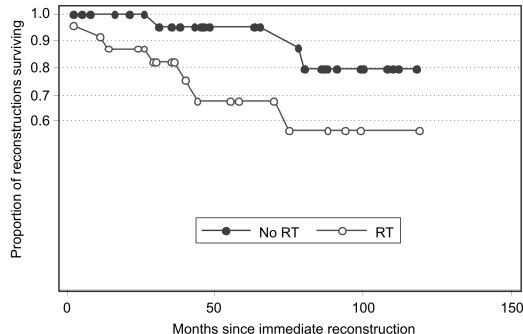
Radiotherapy affects survival of implant-based immediate reconstruction
In this series, implant-based reconstructions were classified according to whether they had or had not received radiotherapy. All breasts which had radiotherapy prior to mastectomy and immediate reconstruction were grouped together with those who received adjuvant post-mastectomy radiotherapy and compared with those who had never been irradiated. Donor site operations were excluded. There was no statistically significant difference between the radiotherapy and no radiotherapy groups in the number of re-operations required in the first 5 years after reconstruction (P = 0.83, Mann-Whitney test). However, the pattern of loss of implant-based reconstruction over time was significantly different according to exposure to radiotherapy (P = 0.04, log-rank test; Fig. 3). Autologous reconstructions were excluded from this analysis as failure occurs early (prior to post-mastectomy radiotherapy).
Figure 3.
Kaplan–Meier graph of survival of implant-based reconstruction according to exposure to radiation. RT, prior radiotherapy or adjuvant irradiation; no RT, no irradiation.
Discussion
The assessment of outcome of breast reconstruction is complex. Interpretation of the literature is complicated by analysis of series including both immediate and delayed reconstructions. In a prospective cohort study of 326 patients, Alderman et al.5 showed that immediate reconstructions have significantly higher total as well as major complication rates. Our study focuses purely on immediate reconstructions and uses operative intervention as an outcome measure as this encompasses complications, patient satisfaction and cosmetic outcome.
Comparisons of re-operations can be problematic because different authors define these differently. For example, Gabriel et al.9 studied 217 women who had an implant-based breast reconstruction. They included anticipated, staged procedures, together with those done because the patient requested a size change or aesthetic improvement but differentiated from those which had at least one clinical indication (defined by the authors as a complication).
The time-course over which re-operations have been reported also varies from paper to paper. For example, Malyon et al.6 reported their data with a mean follow-up of 10 months, while the Clough et al.7 series of implant reconstructions had a median follow-up of 4.2 years. With improving survival rates, long-term maintenance of good cosmesis becomes more important. We have, very deliberately, reported our re-operation data for patients who have completed 5 years of follow-up without developing local or distant recurrence and without changing the type of reconstruction.
We have also examined results by reconstruction type. These data could be useful to patients selecting the best reconstructive option for them. Such a comparison between reconstruction types was not truly possible in the studies of Kroll and Baldwin3 or Malyon et al.6 because of a varying proportion of immediate and delayed reconstructions and differences in follow-up period between the reconstruction types. These differences could have accounted for some of the differences in re-operation rates.
Numbers of operations at 5 years
The re-operation rates that we report are higher than we had anticipated and higher than other series. This emphasises the value of self-audit. In comparison with our data, Malyon et al.6 report lower median re-operation numbers. However, inclusion of delayed reconstructions and only 10-month mean follow-up precludes comparison of their data with ours. In particular, in our series many patients underwent revision surgery greater than 2 years after their primary reconstruction suggesting that other series might not have measured the full impact of additional surgery. Clough et al.7 presented data on the longevity of good cosmesis after immediate reconstruction using implants. The revisional surgery rate was 30.2% over a median follow-up period of 4.2 years. This is the proportion of patients who have undergone further surgery, the numbers of operations per patient are not reported. The equivalent proportion for our implant-based reconstruction group is 87% over a longer time-course of 5 years.
It is important to note that many of the implant-only reconstructions were performed almost 10 years ago and, at that time, many were sited in a dual-plane, part submuscu-lar, part subcutaneous pocket. Many of this now historical series received radiotherapy, unlike Clough's series (only 8%). Likewise, the DIEP flaps with more than 5 years of follow-up time are those performed early in our series and their problems may represent learning curve issues.
Though not statistically significant, the mean number of re-operations required by patients with implant-based reconstructions is higher than autologous reconstructions. As demonstrated earlier, the number of reconstructions in each group is insufficient to allow an important clinical difference to reach statistical significance. Furthermore, these patients who reached 5 years from their initial reconstruction are likely to be a selected subgroup who had not had complications or required adjustments. The patients whose reconstruction failed within the 5-year period might have had several attempts at salvage before conceding that an alternative method of reconstruction was required.
In addition to number, the magnitude of the re-operations varies greatly between groups (data not shown). This is hard to quantify, but liposuction and excision of donor site dog ears as commonly required after DIEP or autologous LD reconstructions constitute a minor burden of operating time, in-patient days and patient recovery time. Implant-based reconstructions commonly require capsulectomy and implant exchange, which not only impact more on resources, but also risk significant complications.
Rate of re-operation changes with time
The annual rate of re-operation is previously unreported. Both types of reconstruction required early re-operations (e.g. to improve the contour of the reconstructed breast or to exchange tissue expander for definitive implant). Once these are done, the rate falls, but not to zero. This has implications for patients, both psychologically and physically, and for resource management.
Time scale of failure of reconstruction (Kaplan–Meier ‘survival’ analysis)
As outlined above, the patients included in the 5-year follow-up of re-operation numbers were, by definition, those whose reconstruction did not fail within the first 5 years. However, to present 5-year data alone would be misleading. Lower re-operation rates for successful autologous reconstruction could hide a higher failure rate. For this reason, we also present data on failure of reconstruction. For DIEP flaps, this was flap failure and occurred within the first postoperative week as would be expected. None of the autologous LD flaps failed. Implant-based reconstructions fail over a longer time-course. While these differences did not reach statistical significance, implant-based reconstructions remained at risk of failure throughout the study period, with a gradual attrition.
Symmetrisation surgery
Of the 80 patients undergoing unilateral mastectomy and reconstruction, 26 (33%) had a symmetrising procedure (data not shown). Contralateral surgery does contribute to overall aesthetic outcome but is an additional potential source of morbidity. Furthermore, it impacts on work load, requiring operating time and follow-up. Similarly, nipple reconstruction and areola tattooing are a matter of patient preference and have an impact on workload.
Conclusions
Patients selecting immediate reconstructions often do so because they desire ‘one operation’ to replace the breast mound and believe that an immediate reconstruction will allow them to move on psychologically. Their decision about the type of reconstruction could be affected by the understanding of a possible requirement for revision surgery for many years to come. A frank discussion is essential during the counselling and consent phase to ensure that patients have a realistic view of the medium-to-long term need for revision.
Although not a perfect measure, we believe that data on re-operations should be collected prospectively to allow comparison between types of reconstruction within an institution. These data also provide useful information about the workload associated with ‘maintenance’ of an immediate reconstruction. This additional workload is often overlooked when planning workforce needs and operating time requirements.
In the light of this and other studies, it may be that the results of the National Mastectomy and Breast Reconstruction Audit10 will contribute, but not be sufficient, to answer questions about patient satisfaction with immediate reconstruction. Patient satisfaction at 3 and 18 months are short-term measures and many of these women are young (mean age in our study was 47 years), likely to survive free of disease (92% in this study) and will, therefore, live with their choice of breast reconstruction for many years. Perhaps, the notes of a subset of patients from the National Audit could be reviewed over time to build up a larger scale picture of the implications of different reconstruction types for re-operation rates and, thus, theatre time and in-patient days incurred by maintenance surgery and failure rates in the long term.
References
- 1.Khoo A, Kroll SS, Reece GP, Miller MJ, Evans GR, et al. A comparison of resource costs of immediate and delayed breast reconstruction. Plast Reconstr Surg. 1998;101:964–8. doi: 10.1097/00006534-199804040-00011. discussion 969-70. [DOI] [PubMed] [Google Scholar]
- 2.Wellisch DK, Schain WS, Noone RB, Little 3rd JW. Psychosocial correlates of immediate versus delayed reconstruction of the breast. Plast Reconstr Surg. 1985;76:713–8. doi: 10.1097/00006534-198511000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Kroll SS, Baldwin B. A comparison of outcomes using three different methods of breast reconstruction. Plast Reconstr Surg. 1992;90:455–62. doi: 10.1097/00006534-199209000-00015. [DOI] [PubMed] [Google Scholar]
- 4.Greenway RM, Schlossberg L, Dooley WC. Fifteen-year series of skin-sparing mastectomy for stage 0 to 2 breast cancer. Am J Surg. 2005;190:918–22. doi: 10.1016/j.amjsurg.2005.08.035. [DOI] [PubMed] [Google Scholar]
- 5.Alderman AK, Wilkins EG, Kim HM, Lowery JC. Complications in postmastectomy breast reconstruction: two-year results of the Michigan Breast Reconstruction Outcome Study. Plast Reconstr Surg. 2002;109:2265–74. doi: 10.1097/00006534-200206000-00015. [DOI] [PubMed] [Google Scholar]
- 6.Malyon AD, Husein M, Weiler-Mithoff EM. How many procedures to make a breast? Br J Plast Surg. 2001;54:227–31. doi: 10.1054/bjps.2000.3538. [DOI] [PubMed] [Google Scholar]
- 7.Clough KB, O'Donoghue JM, Fitoussi AD, Nos C, Falcou MC. Prospective eval uation of late cosmetic results following breast reconstruction: I. Implant reconstruction. Plast Reconstr Surg. 2001;107:1702–9. doi: 10.1097/00006534-200106000-00010. [DOI] [PubMed] [Google Scholar]
- 8.Clough KB, O'Donoghue JM, Fitoussi AD, Vlastos G, Falcou MC. Prospective evaluation of late cosmetic results following breast reconstruction: II. Tram flap reconstruction. Plast Reconstr Surg. 2001;107:1710–6. doi: 10.1097/00006534-200106000-00011. [DOI] [PubMed] [Google Scholar]
- 9.Gabriel SE, Woods JE, O'Fallon WM, Beard CM, Kurland LT, Melton 3rd LJ. Complications leading to surgery after breast implantation. N Engl J Med. 1997;336:677–82. doi: 10.1056/NEJM199703063361001. [DOI] [PubMed] [Google Scholar]
- 10. National Mastectomy and Breast Reconstruction Audit, second report. 2009 < http://www.ic.nhs.uk/mbr>.