THE ORIGINAL ‘HEARTSINK’ STUDY
In his 1988 paper ‘Five years of heartsink patients in general practice’,1 Tom O'Dowd is said to have coined the term ‘heartsink’. In that paper O'Dowd refers to a publication in which the term ‘heartsink’ had been employed 2 years previously, but in which the author, CG Ellis, preferred ‘dysphoria’ to describe:
‘the feelings felt in the pit of your stomach when their [the patients’] names are seen on the morning's appointment list’.2
O'Dowd believed that Ellis's ‘pit of your stomach’ definition had ‘an intuitive ring about it’; he quoted it and attached it to the term ‘heartsink’, a term which, according to O'Dowd, ‘more clearly refers to the doctor's emotions which are triggered by certain patients’.1
O'Dowd's paper described a study of 28 patients ‘considered to be heartsink’ in his practice. Over 6 months, these patients were discussed by practice staff at a series of lunchtime meetings. The stated function of these discussions was to share information, define problems, formulate management plans, and provide support for the GP assigned to each patient. We are not told whether the discussions elicited heartsink-type feelings among attendees, but, tellingly: ‘the meetings stopped after 6 months because of pressure of time and doubt that the effort was worth while’.1 When the meetings ceased only nine of the 28 heartsink patients had been discussed. O'Dowd determined that: ‘Inadvertently this has provided two comparison groups: one group who had a management plan and one whose care was unplanned and reactive’. Five years later, O'Dowd compared these two groups using outcome measures such as frequency of attendance and whether or not the patients were still ‘considered to be heartsink’.
O'Dowd's study contained several significant weaknesses: unclear entry criteria; questionable comparison groups; ill-defined and inadequately-described interventions; follow-up that was very incomplete; and outcomes that are difficult to interpret. Arguably, the greatest flaw is the failure to disentangle the doctor and their feelings from the patient and their presentations. O'Dowd recognised that the doctors’ experience was subjective, but perceived the problem and its solution to lie in his patients. The phrase ‘heartsink patient’ captures this ambiguity perfectly: it is the doctor's heart that sinks, but it is the patient who receives the label. O'Dowd was conscious that his problem remained unresolved and ended his paper with a call for assistance: ‘we need help with this problem because we are part of it and thus find understanding it difficult’.
IMPACT OF THE HEARTSINK STUDY
Irrespective of the study's limitations, the perceived problem and the term used to describe it evidently resonated with readers. Heartsink-titled editorials citing O'Dowd appeared in Australian and Canadian primary care journals the following year.3,4 The terminology was taken up in different specialities also, with citations of O'Dowd subsequently occurring in journals of neurology, rheumatology, ophthalmology, diabetology, psychiatry, psychology, sociology, social science, and public health, as well as the journals of Quality & Safety in Healthcare, Management Learning, Pain, and Sex Roles.
The inception of heartsink within the medical literature and its increase in use over time can be demonstrated. The academic search engine Google Scholar was employed to identify uses of the term heartsink each year in journal articles and books within the fields of medicine, pharmacy, and veterinary medicine for the 30 years from 1980 to 2009. To ensure that any witnessed change in heartsink references did not simply reflect changes in total references over time, the number of heartsink references each year was divided by the total number of Google Scholar references for that year, to give an index of heartsink references per Google Scholar reference per year (Figure 1).
Figure 1.
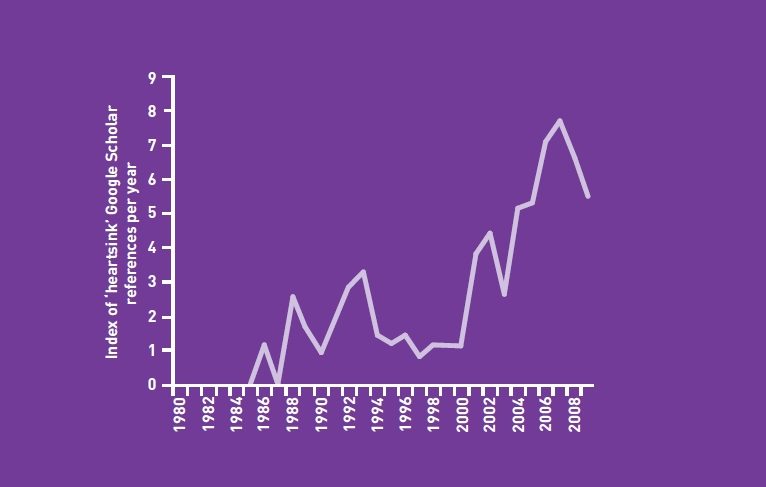
Google Scholar ‘heartsink index’ 1980–2009.
The graph adequately demonstrates a rise in the use of heartsink over time in the literature of medicine, pharmacology, and veterinary medicine. During the early years of the 1980s there were no uses of heartsink found in the Google Scholar database. Five references in 1986 (Google Scholar heartsink index value 1.24) correspond to publication of Ellis's dysphoria article in that year; 12 references (index value = 2.62) occur in 1988, the year of O'Dowd's work; the rise continues sporadically thereafter.
The science citation website ISI Web Of Knowledge provides evidence that it was O'Dowd's paper and not Ellis's that directly impacted the growth of heartsink in the literature. Ellis's paper ’ containing the first published appearance of heartsink as well as the ‘feelings felt in the pit of your stomach’ definition — has only five subsequent Web Of Knowledge citations; O'Dowd's paper has 87. Despite his own citing of Ellis and his acknowledgement that heartsink had been in use before he arrived at his practice, several papers are explicit in crediting O'Dowd with having coined the term heartsink.5–7 Many more imply this by superscripting a citation of O'Dowd after using the term.
However, reviewing the uses of heartsink found in Google Scholar for the year 2010 reveals how the term has shifted far from O'Dowd's work, not only geographically and contextually, but semantically (Box 1). A commercial herbalist in New Zealand suggests a disease can create heartsink; an American dermatologist asserts that both his colleagues and patients can perceive a heartsink disease; an English ear, nose, and throat surgeon refers to iatrogenic surgical complications as heartsink cases; whole housing estates and towns become ‘heartsink’ in a letter to a journal; and a vet suggests a typology of heartsink pet-owners.
Box 1.
Google Scholar citations for ‘heartsink’ occurring in 2010 among medicine, pharmacology, and veterinary science references
The eight citations are listed in order of their consecutive appearance on the Google Scholar website.
-
New Zealand website promoting wheatgrass products for medicinal purposes.
‘Osteitis Pubis … creates heartsink for doctors.’
-
Letter bemoaning the exclusive appearance of professors in nominations for the BMJ Group's lifetime achievement award.
‘… the doctor who achieves most in life is probably an unknown general practitioner quietly improving the life and health of the population of a heartsink estate in a heartsink town.’
Bisset DL. Professors need only apply? BMJ 2010; 340: c280.
-
Paper on Hidradenitis Suppurativa claiming patients use the term to describe their condition.
‘… both patients and dermatologists describe HS as a “heart-sink disease”.’
Adams DR, et al. Treatment of Hidradenitis Suppurativa with etanercept injection. Arch Dermatol 2010; 146: 501–504.
-
A rheumatologist asserting that some patients are conscious of their label.
Patients with chronic widespread pain and fibromyalgia ‘often get to recognize that they are regarded as “difficult” or ‘heart-sink” patients.’
Shipley M. Chronic widespread pain and fibromyalgia syndrome. Medicine 2010; 38(4): 202–204.
-
An English homeopath describing the levels of increasing ‘depth’ that homeopathic practitioners engage with:
‘Symptoms at the deeper levels can sometimes define the heart sink patient as they do not sit easily in a conventional framework but are often experienced vividly by the patient.’
Thompson EA. Alternative and complementary therapies for the menopause: a homeopathic approach. Maturitas 2010; 66: 350–354.
-
An ear, nose, and throat surgeon discussing infected cochlear implants:
‘These are heart sink cases for the implant surgeon, worse if attributable to some aspect of surgery or hospital care.’
Gray RF. Surgical challenges in cochlear implants. Cochlear Implants Int 2010; 11(Suppl 2): 12–19.
-
A qualitative investigation of GPs’ experiences of palliative care patients in out-of-hours settings implies that the context creates the ‘heartsink patient’.
‘GP9 went as far as stating that the time-pressure factor meant that palliative care patients out-of-hours were “heart sinks” for her.’
Taubert M, Nelson A. ‘Oh God, not a Palliative’: out-of-hours general practitioners within the domain of palliative care. Palliat Med 2010; 24: 501–509.
-
A textbook of veterinary skills:
‘A common “heart-sink” type of client for veterinary surgeons is the angry client.’
Gray C, Moffett J. Handbook of veterinary communication skills. Chichester, Wiley-Blackwell. 2010: 115.
Viewed retrospectively, the significance of O'Dowd's paper appears to lie less in its drawing attention to the challenges of certain doctor–patient relationships in general practice and its defining of these challenges as within the scope of scientific study, and more in its popularisation of the term heartsink and its legitimisation of use of the term within the scientific literature.
PSYCHODYNAMIC POTENTIAL
Current use of the term heartsink has clearly moved beyond reference to O'Dowd's paper and the ‘problem’ that he perceived. None of the references in Box 1 cites O'Dowd and none of them upholds O'Dowd's patient-specific and specific-patient meaning of heartsink. Moreover, the phrase ‘heartsink patient’ has come under attack: branded ‘derogatory, unhelpful and inaccurate’ by the author of Using CBT in General Practice.8 She instead advocated reference to heartsink ‘reactions’ or ‘responses’ with the assertion that these responses were wholly the responsibility of the GP, ‘rather than being an inherent characteristic of any particular patient’. This re-formulation usefully facilitates contemplation of coping mechanisms that can be used in practice. It also sensibly challenges ill-considered labelling of patients. However, in discouraging reference to ‘heartsink patients’ there is a risk of permitting, even encouraging, less reflection-provoking labels (‘difficult patient’, ‘challenging patient’, etcetera) that concretise the externalisation of a problem. A powerful reflective imperative implied by O'Dowd's phrase is lost when heartsink is allowed to stray from its reference to patients.
O'Dowd's chosen term, in combining two common words to convey an intuitive understanding and elicit an emotional response, lies emphatically within the Freudian tradition.9 Furthermore, his favouring of an ‘intuitive’, ‘gut feeling’ definition to describe ‘the doctor's emotions which are triggered by certain patients’ represents an acknowledgement and frank expression of unconscious unresolved feelings within the doctor–patient relationship. In O'Dowd's formulation of that relationship, although the patient is implicated, so too is the doctor: it is, after all, the doctor's heart that sinks. Thus heartsink has a clear relation to established psychodynamic concepts of transference (the unconscious transfer of feelings from a relationship in the past to one in the present) and countertransference (the emotions evoked — here, within the doctor — by the transference of another — here, the patient).10,11 Indeed, an associated concept is ‘hate in the countertransference”: the title of an essay by physician and psychoanalyst Donald Winnicott in which a case is made for personal therapy or, by the extension of the editors of a recent volume in which the essay is republished, a contention:
‘that all staff working in this field should be offered, at a minimum, reflective space and supervision to explore negative feelings about service users openly and objectively.’12
Heartsink then becomes an appeal for a more reflective practice; for the use of psychodynamic perspectives and Balint groups.13 To this end, and to overcome our wariness of subjective patient labels, it may be more useful to talk of ‘heartsink relationships’.
Significantly, this psychodynamic framing of heartsink leaves still unanswered some philosophical questions raised by O'Dowd's paper: questions about the legitimacy of accepting or dismissing psychological, social or spiritual problems as being within or beyond the remit of a doctor;5 and about the relative validity of the biomedical and biopsychosocial paradigms we may uphold in perceiving and understanding our patients.14
If, over time, the term heartsink has become merely another pejorative label, it may reflect our own failings and/or those of our profession: the adoption of O'Dowd's terminology without the effort and/or without the ‘reflective space and supervision’ that is required to resolve the problems that he struggled to understand. It is striking that, of the 87 above-referred-to citations of O'Dowd in the scientific literature, few (half a dozen at most) offer his subject matter a psychodynamic rendering and none consider the psychodynamic potential implicit in his terminology. In recent months, GPs have described how psychodynamic work within general practice is perceived to be challenged by evidence-based medicine,15 the Quality and Outcomes Framework,16 and Darzi Centres.17 This is lamentable because, in the context of such fast-shifting paradigms and increasing pressures in practice, performance assessment, service provision, and, lately, patient choice, the difficulties unresolved within ourselves and within our professional role have arguably never been greater. Reflective work has therefore never been more important (that it may never have been more challenging might prompt contemplation of our unconscious work-avoidance). Undertaking that important reflective work may help us in determining the most useful developments for our profession and may aid our personal growth as practitioners; eventually, perhaps, shoring our hearts from sinking.
Acknowledgments
Thanks to Nia Roberts who assisted with the citation searches and to Jeremy Howick and Kay Wang who read drafts of this paper. Thanks also to Richard James who provided extensive comment.
Provenance
Freely submitted; not externally peer reviewed.
REFERENCES
- 1.O'Dowd TC. Five years of heartsink patients in general practice. BMJ. 1988;297(6647):528–530. doi: 10.1136/bmj.297.6647.528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ellis CG. Making dysphoria a happy experience. BMJ. 1986;293(6542):317–318. doi: 10.1136/bmj.293.6542.317. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Colquhoun JP. Heartsink — yet another challenge. Austral Fam Physician. 1989;18:559–561. [PubMed] [Google Scholar]
- 4.Dixon T. Heartsink. Can Fam Physician. 1989;35:2381–2386. [PMC free article] [PubMed] [Google Scholar]
- 5.Butler CC, Evans M. The ‘heartsink’ patient revisited. The Welsh Philosophy and General Practice Discussion Group. Br J Gen Pract. 1999;49:230–233. [PMC free article] [PubMed] [Google Scholar]
- 6.Gray DP, Evans P, Sweeney K, et al. Towards a theory of continuity of care. J R Soc Med. 2003;96:160–166. doi: 10.1258/jrsm.96.4.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grant N, Gibbs T. Heartsink relationships: paradox as paradigm. Br J Gen Pract. 2009;59:136–137. [Google Scholar]
- 8.David L. Banbury: Scion Publishing Ltd; 2006. Using CBT in general practice: the 10 minute consultation. [Google Scholar]
- 9.Bettelheim B. New York, NY: Alfred A Knopf; 1982. Freud and man's soul. [PubMed] [Google Scholar]
- 10.Hughes P, Kerr I. Transference and countertransference in communication between doctor and patient. Adv Psychiatr Treat. 2000;6:57–64. [Google Scholar]
- 11.Goldberg PE. The physician–patient relationship: three psychodynamic concepts that can be applied to primary care. Arch Fam Med. 2000;9:1164–1168. doi: 10.1001/archfami.9.10.1164. [DOI] [PubMed] [Google Scholar]
- 12.Winnicott DW. Hate in the countertransference. Int J Psychoanal. 1949;30:69–74. [Google Scholar]
- 13.Kjeldmand D, Holmström I. Balint groups as a means to increase job satisfaction and prevent burnout among general practitioners. Ann Fam Med. 2008;6:138–145. doi: 10.1370/afm.813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilson HJ. The myth of objectivity: is medicine moving towards a social constructivist medical paradigm? Fam Pract. 2000;17:203–209. doi: 10.1093/fampra/17.2.203. [DOI] [PubMed] [Google Scholar]
- 15.Davidsen AS. To survive, general practice needs to reintroduce the psychodynamic dimension. Psychodynamic Practice. 2010;16:451–461. [Google Scholar]
- 16.Edgcumbe D. But there are no QOF points for Balint work! Its place in modern practice. Br J Gen Pract. 2010;60:858–859. doi: 10.3399/bjgp10X539380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stevens R. What Lord Darzi doesn't know: the role of psychodynamic factors in health. Psychodynamic Practice. 2010;16:445–450. [Google Scholar]


