Abstract
Aims: To examine whether individual changes in alcohol consumption among female alcoholics under treatment are predicted by level of and changes in depression and dysfunctional attitudes. Method: A total of 120 women who were treated for alcohol addiction at the Karolinska Hospital in Stockholm (Sweden) were assessed twice over a 2-year period using the Depression scale from the Symptom Checklist-90, the Alcohol Use Inventory and the Dysfunctional Attitude Scale (DAS). Latent growth curve analysis was used. Results: Decrease in alcohol consumption, depression and dysfunctional attitude variables were found at group level. The results also showed significant individual variation in change. Changes in alcohol consumption were predicted by baseline alcohol drinking, as well as by level and changes in depression. Stronger reduction in depression was related to higher level of depression at baseline, and with reduction in dysfunctional attitudes. Different DAS sub-scales resulted in different magnitude of the model relations. Good treatment compliance was related to lower baseline level in depression, but also with higher baseline level in dysfunctional attitudes, and predicted stronger reduction in alcohol consumption. Conclusion: This paper shows the importance of incorporating both individual level and change in depression as predictors of change in alcohol consumption among subjects treated for alcohol addiction. Also, dysfunctional attitudes are both indirectly and directly related to treatment outcome. By incorporating alcohol consumption, depression and dysfunctional attitudes as targets of intervention, treatment compliance and outcome may be enhanced.
INTRODUCTION
Alcohol problems manifest in several ways: in high level of alcohol consumption, harmful drinking patterns and relapse to alcohol drinking after treatment. Alcohol problems and depression co-vary in women, as assessed by cross-sectional and longitudinal epidemiological and clinical studies (Burns et al., 2005; Dixit and Crum, 2000; Haynes et al., 2005; Ramsey et al., 2005). Even if related, improvement in one disorder does not always reduce the other (Burns et al., 2005). Dysfunctional attitudes may interact with depression and thereby also with alcohol problems. The relation between depression and dysfunctional attitudes has mostly been analysed in the context of cognitive therapy studies, in which patients with alcohol addiction have usually been excluded (Oei and Free, 1995). The present study, which is related to an earlier study of the same sample (Haver and Gjestad, 2005), explores the relation between dysfunctional attitudes, depression and alcohol consumption, both at the group and individual level.
Changes in alcohol problems and depression
Changes in alcohol use disorders (AUDs) over time correlate with baseline levels of alcohol use (Dawson et al., 2007) and with major depression (Greenfield et al., 1998). Depression at intake, as measured by diagnosis or continuous measures of depression severity, predicts the alcohol outcome after treatment among women who suffer from AUDs (Charney et al., 1998; Zilberman et al., 2003). Measurement differences may partially explain different results of co-morbidity analyses, with strongest relations often found when using diagnostic categories of depression (Bradizza et al., 2006; Burns et al., 2005; Haynes et al., 2005). Depression is a strong predictor of relapse to alcohol drinking, with prolonged depression being a stronger predictor than the baseline level of depression (Bradizza et al., 2006; Haver and Gjestad, 2005). Thus, changes in depression are important for later alcohol consumption (Kodl et al., 2008). The latter study showed reduction in depression to occur both spontaneously and as a result of intervention. The degree of alcohol dependence and alcohol consumption at baseline did not correlate with alcohol measures at follow-up. A decrease in co-morbid depression may thus explain why higher levels of alcohol consumption and dependence at baseline do not always correlate with poor outcomes of addiction treatment. One study found an equal decrease in alcohol consumption over a 3-month period in men and women with or without current depression and/or anxiety (Burns et al., 2005). Changes in alcohol consumption and depression have also been studied using autoregressive models (Aneshensel and Huba, 1983; Peirce et al., 2000). The effect of depression on later residual change in alcohol use was of relatively short duration. Another study found that higher baseline depression levels were associated with a decrease in alcohol consumption at Year 1, and with an increase in alcohol consumption at Year 3, indicating a non-linear relation over time (Schutte et al., 1995, 1997). The close relation between alcohol consumption and depression over time was confirmed in one meta-analysis (Hartka et al., 1991), but not confirmed by others (Nolen-Hoeksema et al., 2006). More advanced statistical methods, such as multilevel modelling, are available for the analysis of change (Curran and Muthén, 1999; Singer and Willett, 2003). For example, one study reported an increase in alcohol consumption over time among clinically depressed patients (women and men) and community controls (Holahan et al., 2004).
These studies show that both the baseline level and especially changes in depression are important for prediction of changes in alcohol problems in general, and specifically in alcohol consumption. These relations will be influenced by the time between measurements, as well as types of measurements used.
Are dysfunctional attitudes related to the level and change in depression and alcohol consumption?
Dysfunctional attitudes, defined as rigidly and relatively stable over generalizations within the domains of perfectionism, performance, need for approval and love, omnipotence and autonomy, are related to depressed mood (Beevers and Miller, 2004; Kwon and Oei, 2003). Such attitudes contribute to a cognitive bias where information is processed in an unrealistically negative manner, which increases the risk for development of a negative mood (Beevers and Miller, 2004). Dysfunctional attitudes are seen as a stable vulnerability factor, and predict changes in depression, including onset and repeated relapses (Elkin et al., 2006; Furlong and Oei, 2002; Hamilton and Dobson, 2002; Weich et al., 2003). Conversely, dysfunctional attitudes may be mood dependent, as depression increases the tendency for negative cognitions (Beevers and Miller, 2004). Improvement in depression could thus be related to an attenuation of dysfunctional attitudes. Attitude changes have been found after various interventions in depressed patients and even in waiting list patients to a lesser degree (Oei and Free, 1995). A change in the Dysfunctional Attitude Scale (DAS) was associated with change in the depression score; thus, dysfunctional attitudes may be seen as a relatively stable parameter, but also as a changeable trait (Oei and Free, 1995). Cognitions have been found to directly predict stability and change in alcohol disorders if relevant cognitive items from existing measurements were selected (Ramsey et al., 2002). Another study found the dysfunctional attitudes scale to be related to later problem drinking in a college sample, even when controlling for level of alcohol consumption, gender, age and depression (Heinz et al., 2009). After controlling for cognitive factors, depressive symptoms were not a significant predictor of problem drinking. Thus, depression-specific dysfunctional attitudes relate to alcohol problems, also problematic alcohol consumption, directly or via the level of and changes in depression, and may be an important factor to include also in samples of problem drinkers.
Research problems and hypotheses
In this study, alcohol consumption was used as a continuous indicator of alcohol problem severity. The use of a continuous alcohol use variable increases the statistical power and possibilities when analysing multivariate statistical models. This study does not take the clinical cut-off between the presence of a clinical diagnostic condition and the non-clinical condition into consideration. However, non-dependent sub-threshold levels of drinking among depressed patients are suggested to be clinically important (Ramsey et al., 2005). On the basis of the literature, we expected changes in alcohol consumption to be predicted by its baseline level and by the level of and changes in depression. In addition, it was hypothesized that changes in depression should be predicted by changes in dysfunctional attitudes. The baseline dysfunctional attitudes score is supposed to be related to the baseline level of depression, and thus being indirectly related to changes in depression. Because of the depression-related content of dysfunctional attitudes, we expected dysfunctional attitudes as a total scale to predict changes in depression exclusively and thereby moderate changes in alcohol consumption indirectly. This would show dysfunctional attitudes to be of clinical importance for alcohol consumption. Sub-dimensions of the total DAS were tested in separate models to explore potential differences in strengths of the predictors. These constructs measured ‘need for other's approval’, ‘need for love’, ‘need for perfection’ and autonomy. Dysfunctional attitudes directly relevant to alcohol problems could relate to alcohol consumption directly (Ramsey et al., 2002). Since the measurement of dysfunctional attitude never was developed to measure relevant attitudes for alcohol problems, dysfunctional attitudes at indicator level were explored as direct predictors of alcohol consumption. Both baseline-change and change-follow-up level models were specified. These models controlled for age (Hamilton and Dobson, 2002; Manninen et al., 2006). These are prediction models and no conclusions about causes and effects can be made, as this would require more measurement points to test competing models (Bollen, 1989; Bollen and Curran, 2006).
MATERIALS AND METHODS
Participants
The Early Treatment of Women with Alcohol Addiction (EWA) treatment project started in 1981 at the Karolinska Hospital in Stockholm, Sweden. This project included 420 women who entered treatment consecutively. The first sub-sample (pilot study) was included between 1981 and 1982 (n = 100), the second group (n = 200) was included during 1983–1984 and the third group of 120 women during 1991–1994. The study of the second group compared EWA treatment with treatment as usual. The present study involves the last 120 women. The focus in this part of the EWA project was the study of co-morbidity factors at intake and at 2-year follow-up. This last sub-sample was quite similar to the two first sub-samples with respect to drinking and socio-demographic variables, although some changes were found, reflecting what had taken place in the Swedish society in general during the time-frame of the study. A somewhat higher general level of unemployment, more beer consumption and less spirits were found among the last sub-sample. However, all women preferred to drink wine (Haver et al., 2009). Median age at intake was 44 years (range 23–63). Educational and occupational level, marital status and number of children were representative of the women in the general population. Almost all women (96%) suffered from a DSM-III-R diagnosis of alcohol dependence (Haver et al., 2001), and had an average alcohol consumption ∼130 g of alcohol on days with heavy drinking. Only women not previously treated for alcohol abuse were included in the EWA study; however, about half the sample had received psychiatric treatment. Increased levels were found with regard to depression and other mental health dimensions compared with a general population control sample (Haver, 2003). Attrition: of the 120 women enrolled, 98 were studied at the 2-year follow-up (82%). Three women died during the study period (from cancer and alcohol-related causes) and 19 women either refused to participate or could not be located. These 19 women differed statistically from women contributing to the last measurement in baseline measures on some relevant variables, with lower scores on alcohol consumption measured by three different alcohol consumption variables, lower prevalence of psychiatric diagnoses in general and depression diagnoses specifically, but higher scores on failing in goal achievements. Thus, the missingness was probably not at random (Bollen and Curran, 2006), and women with baseline data only were therefore excluded from the analyses (list-wise deletion) instead of imputing follow-up scores.
Intervention
The psychotherapy focused mainly on alcohol-related problems with a reduction of harmful drinking or total abstinence as the intervention goal; however, pharmacological treatment was also given for alcohol addiction and psychiatric disorders. Further descriptions of the sample, treatment and measurements were reported earlier (Haver, 2003; Haver et al., 2001). The study was approved by the Stockholm Regional Ethical Review Board and by the Swedish Data Inspection Board.
Measures
The instruments used were Swedish versions of the Alcohol Use Inventory (AUI; Berglund et al., 1988; Wanberg et al., 1977), a 25-item version of the DAS-25 (Weich et al., 2003) and the Depression scale from the Symptom Checklist-90 (SCL-90; Derogatis and Cleary, 1977; Zack et al., 1998). The instruments were administered twice, at intake after the abstinence phase and at the 2-year follow-up.
The AUI measures used were maximum alcohol consumption on any drinking day in grams of alcohol, average consumption on drinking days and average daily consumption over 1 week. Maximum consumption on any drinking day was used as the main alcohol variable. The two other indicators were also tested in similar models. The variables were normally (or nearly normally) distributed.
The DAS-25 is a valid and frequently used instrument of depression-related cognitions (Nelson, 1992; Oei and Free, 1995; Ramsey et al., 2002). The items are within the domain of approval, love, achievement, perfectionism, entitlement, omnipotence and autonomy. The internal consistency (Cronbach's alpha) for DAS was 0.91 at baseline and 0.90 at follow-up. In explorative bivariate analyses, some follow-up DAS indicators predicted follow-up level in alcohol consumption. These items indicated a need of achievement to gain respect, difficulty taking risks because of fearing the consequences, experiencing inferiority if not succeeding as well as others, afraid of losing others’ respect, the need of expecting success before making any effort to solve problems, problems of trusting others because of being afraid to be hurt, believing that happiness is more dependent on other persons than oneself and a belief that problems will disappear without any effort. These items were grouped as a scale [here called alcohol-related DAS (DAS-ALC)] to explore the relations within the model with the follow-up level specified as the intercept factors for DAS-ALC and alcohol consumption.
The SCL-90 Depression scale is a symptom measure of depression. Depression as a theoretical construct is related to observed indicators, both within the diagnostic and dimensional diagnostic perspective (Borsboom, 2008). In this paper, we used the term ‘Depression’ as the label of the continuous latent underlying variable being reflected by the SCL-90 symptom indicators. Even if these symptom indicators would be related to the diagnosis of depression, this measure is not a measure of clinical diagnosis. As for the alcohol measure, a continuous measure was best suited for the research problems in this study. The internal consistency for this scale was 0.90 and 0.93 at baseline and follow-up, respectively. On the basis of the internal consistency results, the latent depression variable was corrected for measurement error in the variables (Stoolmiller, 1995).
Although it is not possible to determine how much of the change was caused by the intervention, some treatment variables were added in the model. Treatment compliance was indicated by still being in treatment or having terminated in accordance with the treatment staff. About 59% women confirmed this kind of compliance. Other variables were number of visits at the EWA centre during intervention years 1 and 2, number of months participating in treatment and number of days in inpatient treatment.
Analyses
Our study was based on a one-group pre- post design, which may be described as a longitudinal design (Rogosa, 1995). Problems related to the use of difference score models have been debated, but nevertheless described as relevant for longitudinal analyses (Rogosa et al., 1982). Although two observations do not reveal the nature or shape of change, they provide information about the amount of change (Duncan et al., 2006). Inclusion of a reference group would have enhanced the possibility of using latent growth curve (LGC) modelling to compare the different sources of changes (Muthén and Curran, 1997). However, as this part of the EWA treatment project was the study of psychiatric co-morbidity and intervention effects were studied prior to this phase, decreases and increases in variables may reflect both intervention effects and other causes.
The analyses used were descriptive statistics, reliability (Cronbach's alpha) and t-test for dependent samples testing of group means over time. Structural Equation Modelling (SEM) was used to test confirmatory factor analysis (CFA) models and LGC models of the level and change in the variables.
A CFA of the depression sub-scale did not support the fact that this scale represented one dimension. Eleven residual co-variances had to be estimated to achieve an acceptable fit between model and data, which indicates several dimensions. This probably reflects some heterogeneity in the scale content and an underrepresentation of the depression construct. Owing to low sample size, the DAS could not be tested with CFA.
LGC models take into account not only group mean differences, but also individual differences in change. LGC is well suited for longitudinal data (Bollen and Curran, 2006), and is preferred over traditional longitudinal analyses (e.g. repeated ANOVA), as it is more flexible regarding complexity in model testing and is the only method that may be used to control for measurement error. On the basis of two measurement points, this model is a difference score model with latent variables (Duncan et al., 2006; Raykov, 1993). Ideally, measurement should be analysed with latent variables reflected by several observed indicators. However, this procedure places demands on the sample size. In this study, the sample size did not allow for such estimation. An approximation of the measurement model could be to pre-specify measurement errors in the models based on Cronbach's alpha (Stoolmiller, 1995). Beyond these restrictions, our analyses follow general guidelines for LGC models within the SEM literature (Bollen and Curran, 2006; Duncan and Duncan, 2004; Willett and Keiley, 2000).
The models were step-wise analysed, separate growth models first, followed by complete models. Based on the hypotheses, the tested structure was tentatively specified. Then non-significant parameters were removed and the model re-estimated. This analytic strategy, which is both confirmatory and exploratory, is described as a model-generating procedure (Jöreskog, 1993). The relation between the level and change in DASs, and change in depression, was analysed with the baseline level of depression entered as a predictor and not as a residual covariance. This strategy was used to control for a possible confounding effect between depression and DASs.
The estimation method was Full Information Maximum Likelihood, which uses information from all cases, even if some data are missing (Arbuckle, 2007). These results were compared with Maximum Likelihood on a total imputed sample with Expectation Maximization imputation for missing data. The two estimation methods produced similar results.
We used χ2 with the significance test, Comparative Fit Index (CFI), Normed Fit Index (NFI), Non-Normed Fit Index (NNFI) and Root Mean Square Error of Approximation (RMSEA) with confidence intervals to evaluate model fit. Ideally, CFI, NFI and NNFI should be beyond 0.90, and RMSEA should be below 0.08 or preferably 0.05 (close fit) (Bollen and Curran, 2006; Kline, 2005). SPSS 15 and AMOS 16 were used for analyses, and Microsoft Excel to compute predicted estimates and generate plots. Plots were estimated at the mean level to describe group baseline and change means, but also at plus/minus one standard deviation to show individual variation around this group level.
RESULTS
Table 1 lists the descriptive statistics obtained from the DAS, SCL-90 Depression scale and AUI Maximum alcohol consumption in grams. All group level changes from baseline (T1) to follow-up (T2) were statistically significant. AUI Maximum alcohol consumption and DAS did not correlate at intake, nor did AUI Maximum and SCL-90 Depression. At follow-up, there was a statistically significant correlation between AUI Maximum alcohol consumption and SCL-90 Depression (r = 0.36, P < 0.05). The correlation between DAS and Depression was stronger at the baseline (r = 0.53, P < 0.05) than at the follow-up (r = 0.36, P < 0.05). Analyses of time-lagged correlations were stronger with DAS (r = 0.54, P < 0.05) and weaker with AUI Maximum alcohol consumption (r = 0.34, P < 0.05).
Table 1.
Descriptive statistics (mean, SD) at baseline and at the 2-year follow-up for AUI Maximum consumption on any drinking day, DAS and SCL-90 Depression scale (n = 98)
| Baseline (T1) |
Follow-up (T2) |
|||||
|---|---|---|---|---|---|---|
| Variable | Mean | SD | Mean | SD | Change | t-test |
| AUI Max alcohol cons | 150.92 | 70.86 | 91.39 | 70.12 | 59.53 | 6.95* |
| DAS | 85.94 | 25.65 | 79.81 | 24.47 | 6.13 | 2.54* |
| SCL-90 Depression | 1.28 | 0.80 | 0.90 | 0.86 | 0.38 | 4.18* |
*P < 0.05.
Separate LGC analyses
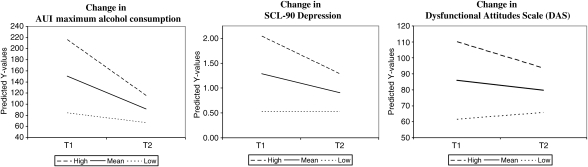
The results of separate growth analyses were used to estimate the predicted time scores, as presented in Fig. 1. A mean group decrease was found for all three variables even though considerable variation in both the baseline level and the change was found.
Fig. 1.
Model-generated growth plots for AUI Maximum consumption on any drinking day, SCL-90 Depression and DAS. Plots show the baseline level at mean and ±1 SD score and predicted change.
The relation between baseline level and change was negative for all variables, indicating that most reduction occurs among those subjects displaying the highest baseline level, while lower baseline levels were associated with a less pronounced decrease and thus increased stability. The depression measure showed more stability than alcohol consumption. The other two alcohol variables showed similar results, with some minor differences regarding the decrease and co-variance between baseline levels and changes. Low DAS levels at baseline were, however, associated with an increase in scores over time.
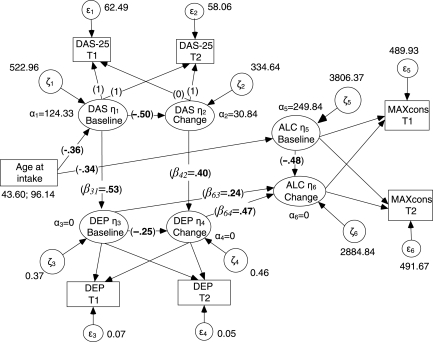
Prediction of changes in alcohol consumption
Figure 2 shows the final model, which reached a close fit between the model and data (χ2 = 11.37, df = 15, P = 0.73, CFI = 1.00, NFI = 0.93, NNFI = 1.06, RMSEA = 0.00, RMSEAc.i. = 0.00–0.07, RMSEAε<0.05 = 0.88). Prediction of change in Maximum alcohol consumption was more strongly related to change in SCL-90 Depression than baseline depression level.
Fig. 2.
Growth model with changes in AUI Maximum alcohol consumption on any drinking day (ALC) predicted by its baseline level (T1), and by baseline level and changes in SCL-90 Depression (DEP). Depression is predicted by DAS. Intercept (α) and variance (ζ) values for baseline levels and changes are presented. Standardized structural parameter values (β) are presented in bold. Measurement errors (ε) are pre-specified.
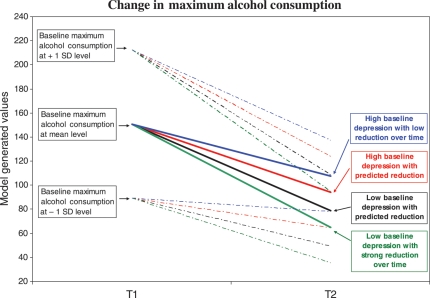
SCL-90 Depression scores at intake were statistically significantly predicted by DAS scores at intake. The model also showed that the DAS change predicted SCL-90 Depression changes. A plot based on these structural equations is presented in Fig. 3. As the AUI Maximum alcohol consumption and the DAS at the baseline level were predicted by age at treatment intake, this plot represents a scenario for women at the mean age. The model-generated results showed younger or older women to have similar changes over time; they would, however, exhibit higher or lower levels. Age did not predict the baseline level of depression and changes over time for any of these three variables.
Fig. 3.
Model-generated plot of the baseline levels and changes in AUI Maximum alcohol consumption on any drinking day. Predictors of change were baseline level of maximum alcohol consumption, and levels and changes in SCL-90 Depression score. All factors were controlled for measurement errors. The figure shows the estimated changes at the baseline mean level and ±1 SD level.
The model-generated estimates in Fig. 3 shows that women with an elevated baseline level of SCL-90 depression decreased their maximum alcohol consumption to a lesser extent than women with a low baseline level of depression. The figure shows two other conditions. Women with lower baseline level of depression and a decrease during the study exhibited the strongest decrease in maximum alcohol consumption. A much less pronounced change in maximum alcohol consumption was related to a higher baseline level of depression and an ongoing high level over time. The figure also shows that the degree of change was dependent on the baseline level of maximum alcohol consumption. This illustrates the importance of building the relation between depression level and change into the model. Dysfunctional attitudes were related to the relation between depression and alcohol consumption, as decrease in the DAS was associated with a greater decrease in depression. Both level and change in dysfunctional attitudes moderated changes in alcohol consumption through the level of and changes in depression. Models using changes in average consumption on drinking days and average daily consumption over 1 week yielded almost identical structural parameter values and goodness-of-fit results.
DAS sub-scales showed differences in parameter values for the prediction of depression, both the relation between baseline levels and the relation between changes in these two factors. Such findings indicate that the scale content is important for prediction strengths. Table 2 shows the ‘need of approval’ factor to be associated with strongest values, while the achievement scale did not result in a well-fitted model. In this last model, the regression effect of age was not statistically significant.
Table 2.
Prediction relations between baseline (T1) levels and changes in DAS and SCL-90 Depression (DEP)
| DAS scales | DAST1 ↓ DEPT1 | DASChange ↓ DEPChange | Model fit: RMSEA | RMSEAε<0.05 |
|---|---|---|---|---|
| Total | 0.53* | 0.40* | 0.000 | 0.88 |
| Approval | 0.61* | 0.51* | 0.000 | 0.92 |
| Perfectionism | 0.60* | 0.21* | 0.040 | 0.53 |
| Love | 0.41* | 0.13* | 0.010 | 0.67 |
| Achievement | 0.66* | 0.32* | 0.137 | 0.00 |
Different DAS scales are analysed: total score, ‘Need of approval’, ‘Need for perfectionism’, ‘Need for love’ and ‘Need for achievement’. Parameter values are standardized
*P < 0.05.
A model with the empirically derived alcohol-related DAS scale (DAS-ALC) showed that follow-up in DAS-ALC predicted follow-up alcohol consumption (standardized β = 0.21), even after controlling for the relation between change in depression and follow-up alcohol consumption (β = 0.37). As before, change in depression was related to change in alcohol consumption (β = 0.23). In addition, the depression baseline level was related to both changes (−0.44) and the follow-up level in DAS-ALC (0.37). Changes in DAS-ALC was related to changes in depression (β = 0.34). All parameter values were statistically significant and the model fitted the data well (χ2 = 5.84, df = 7, P = 0.56, CFI = 1.00, NFI = 0.95, NNFI = 1.02, RMSEA = 0.00, RMSEAc.i. = 0.00–0.07, RMSEAε<0.05 = 0.70).
The treatment compliance variable was added to the original model presented in Fig. 2. Compliance was predicted both by the DAS (0.27, P < 0.05) and depression (−0.34, P < 0.05) baseline factors, with higher levels of the DAS and lower levels of depression being associated with the presence of compliance. The direct relation between the baseline symptom level of depression and changes in alcohol consumption was not supported in this model. Also, the compliance variable predicted changes in alcohol consumption (standardized β = −0.20, P < 0.05), that is, greater reduction in alcohol consumption among compliant women. The model fitted the data very well (χ2 = 14.89, df = 19, P = 0.73, CFI = 1.00, NFI = 0.91, NNFI = 1.06, RMSEA = 0.00, RMSEAc.i. = 0.00–0.07, RMSEAε<0.05 = 0.89). Other treatment variables did not give similar results.
DISCUSSION
Many alcohol-addicted women coming for treatment showed symptoms of depression, with related dysfunctional attitudes as well. Changes in alcohol consumption, symptoms of depression and dysfunctional attitudes were found over time, both at group and individual levels. Some of the strong reductions that were associated with high baseline levels could represent a regression to the mean effect (Finney, 2008; Gmel et al., 2007). Even though women with highest problem scores at the baseline also experienced most reduction over time, the results confirmed the findings of Dawson et al. (2007) that higher levels of alcohol consumption at the baseline were associated with higher alcohol consumption later on.
Level and change in depression predicted changes in alcohol consumption
Our findings based on latent growth models have no direct counterparts in previous studies, as these studies have used other types of analyses, different ways of operationalization of the constructs and different time intervals. The number of time points may also be an important factor contributing to differences (Schutte et al., 1997). Nevertheless, the present findings support the hypothesis that both initial and prolonged elevated levels of depression is an important determinant of whether alcohol problems decrease over time or not (Bradizza et al., 2006; Charney et al., 1998; Greenfield et al., 1998; Kodl et al., 2008; Ramsey et al., 2005). The estimated model showed changes in depression symptoms more strongly to predict changes in alcohol consumption than did the baseline level in such depression symptoms. This confirms later alcohol consumption to be more strongly related to changes in depression than previously elevated levels of alcohol consumption and depression (Hartka et al., 1991). Thus, a prolonged level of depression may explain the apparent stability or even the increase in alcohol consumption and other alcohol-related problems over time (Driessen et al., 2001). These results may also suggest why alcohol abstinence at a later point in time is not necessarily predicted by baseline alcohol consumption and severity of dependence (Kodl et al., 2008). Even if no differences with regard to decrease in alcohol consumption between groups with or without baseline depression or anxiety were found (Burns et al., 2005), our results could indicate that this could be due to a decrease in depressive symptoms among subjects in the co-morbid group. Our results are also in agreement with a study showing that depressed patients are at risk for increased alcohol consumption over time (Holahan et al., 2004). These patients were at risk for increased negative events, less social support and greater levels of dysfunctional coping. Obtaining help for coping with depression and other-related factors may, therefore, also enhance the therapeutic effects on alcohol problems, for example, a reduction in harmful alcohol consumption. Our study showed that higher levels of alcohol consumption and depression at intake were associated with a greater decrease in alcohol consumption, given the expected changes in depression. This shows how changes in the outcome variable are moderated by the predictors, which indicates interaction effects (Bollen and Curran, 2006). The present investigation therefore extends earlier findings, as both the level of and change in depression contributed to the magnitude of change in alcohol consumption. These findings illustrate some of the shortcomings of traditional analyses of change, especially when using categorized variables. In sum, these findings underscore the importance of reducing both depression level and alcohol consumption among women who present with this co-morbidity.
Dysfunctional attitudes predicted changes in alcohol consumption indirectly and directly
Changes in dysfunctional attitudes were evident, even though these were more stable than the levels of depression and alcohol consumption. These findings were as expected (Elkin et al., 2006; Furlong and Oei, 2002; Hamilton and Dobson, 2002; Oei and Free, 1995). Earlier studies indicate that pre-treatment dysfunctional attitudes are predictive of depression treatment response and depression relapse (Elkin et al., 2006; Hamilton and Dobson, 2002). In addition to the different analytic approaches used, the inclusion of the DAS change factor in addition to the baseline level could explain this difference in findings. Nevertheless, the baseline dysfunctional attitudes score is related to changes in depression indirectly via its relation to the depression baseline level. The growth curve analysis without a specified measurement error showed a statistically significant relation between the baseline level of dysfunctional attitudes and changes in depression. However, when measurement errors in the variables were accounted for, this direct relation was not supported. Reduction in dysfunctional attitudes was related to reduction in depression levels, a finding confirming previous findings (Beevers and Miller, 2004; Brown and Ramsey, 2000; Furlong and Oei, 2002; Kwon and Oei, 2003). Reduction in alcohol consumption was indirectly related to a lower baseline level of and reduction over time in dysfunctional attitudes. The DAS as a total scale did not predict alcohol consumption directly. However, some DAS items at follow-up predicted alcohol consumption at follow-up. This confirms that cognitions may be directly related to alcohol problems if relevant cognitions are measured (Heinz et al., 2009; Ramsey et al., 2002). These findings show how a possible direct relation between a DAS and alcohol consumption may not be found if this scale consists of heterogeneous items only partially relevant to drinking. Differences in the magnitude of the predictor relations were found to be dependent on which DAS sub-scales were analysed. This illustrates the importance of using conceptually homogeneous scales in analyses (Smith et al., 2009). Preliminary analyses also link increases in dysfunctional attitudes to mortality in this group of women, while no such results were found for changes in depression and alcohol consumption. Integrating different dimensions of dysfunctional attitudes into the model gives additional understanding of this co-morbidity between alcohol addiction and depression over time.
Treatment compliance
Compliance was predicted by baseline levels in dysfunctional attitudes and depression, and it predicted changes in alcohol consumption. The direct relation between the baseline level in depression and changes in alcohol consumption was not maintained when compliance was included in the model. However, this relation may be partially covered by the indirect relations between baseline depression and changes in alcohol consumption through the compliance variable. The relation between baseline dysfunctional attitudes and compliance was positive, whereas the relation with depression at the baseline was negative. Even if this finding is not easily interpreted, it is an interesting possibility that such dysfunctional attitudes may be related to the perceived need and motivation for treatment, while depression symptoms not covered by such attitudes might be associated with decreased motivation and passivity.
Limitations of the study
The generalizability of our findings is limited to a population of women being able to contribute at both measurements points, since missing data analysis indicated differences between those lost to follow-up and the rest of the group studied. Another sample limitation is linked to the model estimation with this sample size. Even if the results indicated close fit, some instability was also found. The model should therefore be replicated in samples of greater size. Although the Depression scale of SCL-90 has been widely used, its validity has been questioned (Cyr et al., 1985; Schmitz et al., 2000; Zack et al., 1998). Our analyses confirm that this scale is encumbered with some validity problems, which indicate that SCL-90 should be revised to achieve more homogeneous, distinct and meaningful dimensions. However, this measurement problem perhaps applies to diagnoses in general (Smith et al., 2009).
CONCLUSIONS
This growth curve analysis of the co-morbidity of level and changes in alcohol consumption and depression describes a clinical picture that both confirms and expands earlier findings, suggesting that both the baseline level of and changes in depression are related to changes in alcohol consumption over time. The inclusion of dysfunctional attitudes moderates the relation between depression and alcohol consumption; however, to different degrees depending on the individual dysfunctional attitude items included for the analysis. In addition, a DAS sub-scale directly related to alcohol consumption at follow-up. Lastly, intervention compliance was found as a mediating factor between the baseline level in these factors and changes in alcohol consumption. These findings have implications for treatment of co-morbid depression and alcohol addiction.
Funding
The project was funded by the Norwegian Research Foundation (NFR), The Swedish Research Council (grant 14645), the Alcohol Research Council of the Swedish Retail Monopoly and Alcohol and Drug Research Western Norway.
Acknowledgements
The assistance of Dr Staffan Lindberg and Ms Irma Bergerson is gratefully acknowledged.
REFERENCES
- Aneshensel CS, Huba GJ. Depression, alcohol use, and smoking over one year: a four-wave longitudinal causal model. J Abnorm Psychol. 1983;92:134–50. doi: 10.1037//0021-843x.92.2.134. [DOI] [PubMed] [Google Scholar]
- Arbuckle JL. Amos 16.0 User's Guide. Chicago, SPSS inc., Amos Development Corporation; 2007. [Google Scholar]
- Beevers CG, Miller IW. Depression-related negative cognition: mood-state and trait dependent properties. Cognit Ther Res. 2004;28:293–307. [Google Scholar]
- Berglund M, Bergman H, Swenelius T. The Swedish Alcohol Use Inventory (AVI), a self-report inventory for differentiated diagnosis in alcoholism. Alcohol Alcohol. 1988;23:173–8. [PubMed] [Google Scholar]
- Bollen KA. Structural Equations with Latent Variables. New York: Wiley; 1989. [Google Scholar]
- Bollen KA, Curran PJ. Latent Curve Models: a Structural Equation Perspective. Hoboken, NJ: Wiley-Interscience; 2006. [Google Scholar]
- Borsboom D. Psychometric perspectives on diagnostic systems. J Clin Psychol. 2008;64:1089–108. doi: 10.1002/jclp.20503. [DOI] [PubMed] [Google Scholar]
- Bradizza CM, Stasiewicz PR, Paas ND. Relapse to alcohol and drug use among individuals diagnosed with co-occurring mental health and substance use disorders: a review. Clin Psychol Rev. 2006;26:162–78. doi: 10.1016/j.cpr.2005.11.005. [DOI] [PubMed] [Google Scholar]
- Brown RA, Ramsey SE. Addressing comorbid depressive symptomatology in alcohol treatment. Prof Psychol Res Pr. 2000;31:418–22. [Google Scholar]
- Burns L, Teesson M, O'Neill K. The impact of comorbid anxiety and depression on alcohol treatment outcomes. Addiction. 2005;100:787–96. doi: 10.1111/j.1360-0443.2005.001069.x. [DOI] [PubMed] [Google Scholar]
- Charney DA, Paraherakis AM, Negrete JC, et al. The impact of depression on the outcome of addictions treatment. J Subst Abuse Treat. 1998;15:123–30. doi: 10.1016/s0740-5472(97)00183-9. [DOI] [PubMed] [Google Scholar]
- Curran PJ, Muthén BO. The application of latent curve analysis to testing developmental theories in intervention research. Am J Community Psychol. 1999;27:567–95. doi: 10.1023/A:1022137429115. [DOI] [PubMed] [Google Scholar]
- Cyr JJ, McKenna-Foley JM, Peacock E. Factor structure of the SCL-90-R: is there one? J Per Assess. 1985;49:571–8. doi: 10.1207/s15327752jpa4906_2. [DOI] [PubMed] [Google Scholar]
- Dawson DA, Goldstein RB, Grant BF. Rates and correlates of relapse among individuals in remission from DSM-IV alcohol dependence: a 3-year follow-up. Alcohol Clin Exp Res. 2007;31:2036–45. doi: 10.1111/j.1530-0277.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL-90: a study in construct validation. J Clin Psychol. 1977;33:981–9. [Google Scholar]
- Dixit AR, Crum RM. Prospective study of depression and the risk of heavy alcohol use in women. Am J Psychiatry. 2000;157:751–8. doi: 10.1176/appi.ajp.157.5.751. [DOI] [PubMed] [Google Scholar]
- Driessen M, Meier S, Hill A, et al. The course of anxiety, depression and drinking behaviours after completed detoxification in alcoholics with and without comorbid anxiety and depressive disorders. Alcohol Alcohol. 2001;36:249–55. doi: 10.1093/alcalc/36.3.249. [DOI] [PubMed] [Google Scholar]
- Duncan TE, Duncan SC. An introduction to latent growth curve modeling. Behav Ther. 2004;35:333–63. [Google Scholar]
- Duncan TE, Duncan SC, Strycker LA. An Introduction to Latent Variable Growth Curve Modeling: Concepts, Issues and Applications. London: Lawrence Erlbaum; 2006. [Google Scholar]
- Elkin I, Falconnier L, Martinovich Z, et al. Therapist effects in the National Institute of Mental Health Treatment of Depression Collaborative Research Program. Psychother Res. 2006;16:144–60. [Google Scholar]
- Finney JW. Regression to the mean in substance use disorder treatment research. Addiction. 2008;103:42–52. doi: 10.1111/j.1360-0443.2007.02032.x. [DOI] [PubMed] [Google Scholar]
- Furlong M, Oei TPS. Changes to automatic thoughts and dysfunctional attitudes in group CBT for depression. Behav Cogn Psychother. 2002;30:351–60. [Google Scholar]
- Gmel G, Wicki M, Rehm J, et al. Estimating regression to the mean and true effects of an intervention in a four-wave panel study. Addiction. 2007;103:32–41. doi: 10.1111/j.1360-0443.2007.02034.x. [DOI] [PubMed] [Google Scholar]
- Greenfield SF, Weiss RD, Muenz LR, et al. The effect of depression on return to drinking: a prospective study. Arch Gen Psychiatry. 1998;55:259–65. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- Hamilton KE, Dobson KS. Cognitive therapy of depression: pretreatment patient predictors of outcome. Clin Psychol Rev. 2002;22:875–93. doi: 10.1016/s0272-7358(02)00106-x. [DOI] [PubMed] [Google Scholar]
- Hartka E, Johnstone B, Leino EV, et al. A meta-analysis of depressive symptomatology and alcohol consumption over time. Addiction. 1991;86:1283–98. doi: 10.1111/j.1360-0443.1991.tb01704.x. [DOI] [PubMed] [Google Scholar]
- Haver B. Comorbid psychiatric disorders predict and influence treatment outcome in female alcoholics. Eur Addict Res. 2003;9:39–44. doi: 10.1159/000067735. [DOI] [PubMed] [Google Scholar]
- Haver B, Gjestad R. Phobic anxiety and depression as predictor variables for treatment outcome. a LISREL analysis on treated female alcoholics. Nord J Psychiatry. 2005;59:25–30. doi: 10.1080/08039480510018797. [DOI] [PubMed] [Google Scholar]
- Haver B, Dahlgren L, Willander A. A 2-year follow-up of 120 Swedish female alcoholics treated early in their drinking career: prediction of drinking outcome. Alcohol Clin Exp Res. 2001;25:1586–93. [PubMed] [Google Scholar]
- Haver B, Gjestad R, Lindberg S, et al. Mortality risk up to 25 years after initiation of treatment among 420 Swedish women with alcohol addiction. Addiction. 2009;104:413–9. doi: 10.1111/j.1360-0443.2008.02479.x. [DOI] [PubMed] [Google Scholar]
- Haynes JC, Farrell M, Singleton N, et al. Alcohol consumption as a risk factor for anxiety and depression: results from the longitudinal follow-up of the National Psychiatric Morbidity Survey. Br J Psychiatry. 2005;187:544–51. doi: 10.1192/bjp.187.6.544. [DOI] [PubMed] [Google Scholar]
- Heinz AJ, Veilleux JC, Kassel JD. The role of cognitive structure in college student problem drinking. Addict Behav. 2009;34:212–8. doi: 10.1016/j.addbeh.2008.10.011. [DOI] [PubMed] [Google Scholar]
- Holahan CJ, Moos RH, Holahan CK, et al. Unipolar depression, life context vulnerabilities, and drinking to cope. J Consult Clin Psychol. 2004;72:269–75. doi: 10.1037/0022-006X.72.2.269. [DOI] [PubMed] [Google Scholar]
- Jöreskog KG. Testing structural equation models. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park, Calif: Sage; 1993. pp. 294–314. [Google Scholar]
- Kline RB. Principles and Practice of Structural Equation Modeling. New York: Guilford Press; 2005. [Google Scholar]
- Kodl MM, Fu SS, Willenbring ML, et al. The impact of depressive symptoms on alcohol and cigarette consumption following treatment for alcohol and nicotine dependence. Alcohol Clin Exp Res. 2008;32:92–9. doi: 10.1111/j.1530-0277.2007.00556.x. [DOI] [PubMed] [Google Scholar]
- Kwon SM, Oei TP. Cognitive change processes in a group cognitive behavior therapy of depression. J Behav Ther Exp Psychiatry. 2003;34:73–85. doi: 10.1016/s0005-7916(03)00021-1. [DOI] [PubMed] [Google Scholar]
- Manninen L, Poikolainen K, Vartiainen E, et al. Heavy drinking occasions and depression. Alcohol Alcohol. 2006;41:293–9. doi: 10.1093/alcalc/agh246. [DOI] [PubMed] [Google Scholar]
- Muthén BO, Curran PJ. General longitudinal modeling of individual differences in experimental designs: a latent variable framework for analysis and power estimation. Psychol Methods. 1997;2:371–402. [Google Scholar]
- Nelson LD. The Dysfunctional Attitude Scale: how well can it measure depressive thinking? J Psychopathol Behav Assess. 1992;14:217–23. [Google Scholar]
- Nolen-Hoeksema S, Wong MM, Fitzgerald H, et al. Depressive symptoms over time in women partners of men with and without alcohol problems. J Abnorm Psychol. 2006;115:601–9. doi: 10.1037/0021-843X.115.3.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oei TPS, Free ML. Do cognitive behaviour therapies validate cognitive models of mood disorders? A review of the empirical evidence. Int J Psychol. 1995;30:145–79. [Google Scholar]
- Peirce RS, Frone MR, Russell M, et al. A longitudinal model of social contact, social support, depression, and alcohol use. Health Psychol. 2000;19:28–38. doi: 10.1037//0278-6133.19.1.28. [DOI] [PubMed] [Google Scholar]
- Ramsey SE, Brown RA, Stuart GL, et al. Cognitive variables in alcohol dependent patients with elevated depressive symptoms: changes and predictive utility as a function of treatment modality. Subst Abus. 2002;23:171–82. doi: 10.1080/08897070209511487. [DOI] [PubMed] [Google Scholar]
- Ramsey SE, Engler PA, Stein MD. Alcohol use among depressed patients: the need for assessment and intervention. Prof Psychol Res Pr. 2005;36:203–7. doi: 10.1037/0735-7028.36.2.203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raykov T. On estimating true change interrelationships with other variables. Qual Quant. 1993;27:353–70. [Google Scholar]
- Rogosa D. Myths and methods: ‘Myths about longitudinal research’ plus supplemental questions. In: Gottman JM, editor. The Analysis of Change. Hillsdale, NJ: Lawrence Erlbaum Associates; 1995. [Google Scholar]
- Rogosa D, Brandt D, Zimovski M. A growth curve approach to the measurement of change. Psychol Bull. 1982;92:726–48. [Google Scholar]
- Schmitz N, Hartkamp N, Kiuse J, et al. The Symptom Check-List-90-R (SCL-90-R): a German validation study. Qual Life Res. 2000;9:185–93. doi: 10.1023/a:1008931926181. [DOI] [PubMed] [Google Scholar]
- Schutte KK, Moos RH, Brennan PL. Depression and drinking behavior among women and men: a three-wave longitudinal study of older adults. J Consult Clin Psychol. 1995;63:810–22. doi: 10.1037//0022-006x.63.5.810. [DOI] [PubMed] [Google Scholar]
- Schutte K, Hearst J, Moos RH. Gender differences in the relations between depressive symptoms and drinking behavior among problem drinkers: a three-wave study. J Consult Clin Psychol. 1997;65:392–404. doi: 10.1037//0022-006x.65.3.392. [DOI] [PubMed] [Google Scholar]
- Singer JD, Willett JB. Applied Longitudinal Data Analysis: Modeling Change and Event Occurrence. New York: Oxford University Press; 2003. [Google Scholar]
- Smith GT, McCarthy DM, Zapolski TCB. On the value of homogeneous constructs for construct validation, theory testing, and the description of psychopathology. Psychol assess. 2009;21:272–84. doi: 10.1037/a0016699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoolmiller M. Using latent growth curve models to study developmental processes. In: Gottman JM, Collins JM, editors. The Analysis of Change. Vol. 20. New Jersey: Lawrence Erlbaum Associates; 1995. pp. 104–38. [Google Scholar]
- Wanberg KW, Horn JL, Foster FM. A differential assessment model for alcoholism. The scales of the Alcohol Use Inventory. J Stud Alcohol. 1977;38:512–43. doi: 10.15288/jsa.1977.38.512. [DOI] [PubMed] [Google Scholar]
- Weich S, Churchill R, Lewis G. Dysfunctional attitudes and the common mental disorders in primary care. J Affect Disord. 2003;75:269–78. doi: 10.1016/s0165-0327(02)00053-8. [DOI] [PubMed] [Google Scholar]
- Willett JB, Keiley MK. Using covariance structure analysis to model change over time. In: Tinsley HEA, Brown SD, editors. Handbook of Applied Multivariate Statistics and Mathematical Modeling. San Diego: Academic Press; 2000. pp. 665–93. [Google Scholar]
- Zack M, Toneatto T, Streiner DL. The SCL-90 factor structure in comorbid substance abusers. J Subst Abuse. 1998;10:85–101. doi: 10.1016/s0899-3289(99)80143-6. [DOI] [PubMed] [Google Scholar]
- Zilberman ML, Tavares H, Blume SB, et al. Substance use disorders: sex differences and psychiatric comorbidities. Can J Psychiatry. 2003;48:5–13. doi: 10.1177/070674370304800103. [DOI] [PubMed] [Google Scholar]