Abstract
The authors operated on 22 patients with scapular body fractures, with a mean age of 35 years. The minimal follow-up was 12 months. All patients were treated from the Judet posterior approach. The study included 14 cases of an isolated body fracture, three of scapular body fracture combined with fracture of the scapular neck and five of glenoid fossa fracture. In all 14 cases where a 3D computed tomography (CT) reconstruction was performed prior to operation, intraoperative findings corresponded to this reconstruction. In eight cases without preoperative 3D CT reconstruction, the correct type of fracture was identified in only two cases. We also identified three basic types of fractures of the lateral border of the scapula. The anatomical relationship between the glenoid fossa and scapular body, congruency and stability of the shoulder joint was achieved in all cases. The average constant score was 94.
Introduction
Fractures of the scapular body have long been treated nonoperatively; however, ever since the work of Robert Judet [1], interest has been evolving in the indications and techniques of internal fixation of these fractures [2, 3]. Malunited scapular body fractures are now recognised as a source of glenohumeral discomfort and functional disability [3–9] and have stimulated a number of studies assessing the outcomes of operative treatment [10–16].
Material and method
Between April 2005 and July 2008, 22 displaced fractures of the scapular body were treated operatively. The patient cohort comprised 20 men and two women, with the mean age 35 (range 19–56) years. In four cases, the scapula fracture was associated with a fracture of the medial clavicle and in one case with acromioclavicular (AC) dislocation. In 19 patients, the fracture was the result of a traffic accident, one a fall from horse, one by a fall from scaffolding and one from a tree falling on the patient. The mean injury–operation interval was 11 (3–21) days. The average follow-up period was 26 (range 12–48) months; eight patients were followed up for more than three years (Table 1).
Table 1.
Overview of patients and their basic characteristics
| N | Gender | Age (Y) | Interval injury-surgery (D) | Fracture type | Type of later border fx | Injury of ipsilateral shoulder girdle | Site | Mechanism of injury | F-U (M) | ROM | Complications | Constant score |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | M | 25 | 7 | 2L | 1A | – | R | by falling tree | 48 | full | – | 100 |
| 2 | M | 45 | 21 | 2L | 1A | – | R | motorbike | 46 | full | – | 100 |
| 3 | M | 39 | 6 | 2L | 1A | clavicle | L | pedestrian hit by tram | 28 | full | – | 98 |
| 4 | M | 32 | 9 | 2L | 2B | – | R | cyclist | 16 | IR -15° | 93 | |
| 5 | M | 36 | 9 | 2L | 1B | clavicle, brachial plexus | R | pedestrian hit by car | 44 | restricted | persisting paresis of brachial plexus | 52 |
| 6 | M | 45 | 21 | 2H | 2A | – | R | fall from horse | 42 | IR -10° | – | 98 |
| 7 | M | 22 | 16 | 2H | 1A | – | L | car driver | 40 | full | – | 100 |
| 8 | F | 19 | 10 | 2H | 2A | clavicle | L | cyclist | 12 | full | – | 95 |
| 9 | M | 25 | 8 | 2H | 2B | clavicle | R | motorbike | 12 | IR -10° | – | 98 |
| 10 | M | 33 | 9 | 2H | 1A | – | L | cyclist | 12 | full | – | 100 |
| 11 | M | 21 | 15 | 3T | 2A | – | L | motorbike | 42 | full | hypertrophic scar | 100 |
| 12 | M | 42 | 19 | 3T | 1A | – | L | fall from height | 12 | full | – | 98 |
| 13 | M | 33 | 9 | Comm | 1B | – | L | motorbike | 18 | IR -10° | – | 96 |
| 14 | M | 38 | 11 | Comm | 1B | AC disloc. | R | motorbike | 20 | IR -15° | angulation of inferior angle | 91 |
| 15 | M | 56 | 13 | Combined 2H+SN | 1B | suprascapular nerve entrapment | R | cyclist | 30 | full | infraspinatus muscle atrophy | 90 |
| 16 | M | 31 | 3 | Combined 3T+SN | 1B | – | R | motorbike | 44 | full | – | 95 |
| 17 | M | 41 | 7 | Combined Comm+TrN | 1B | – | L | car driver | 38 | full | – | 95 |
| 18 | M | 30 | 6 | Combined 2H+G | 3 | – | R | cyclist | 15 | full | revised hematoma | 95 |
| 19 | M | 33 | 9 | Combined 2H+G | 3 | clavicle | L | motorbike | 16 | ER -10° | – | 91 |
| IR-10° | ||||||||||||
| 20 | M | 55 | 11 | Combined 2H+G | 3 | – | L | cyclist | 12 | ER-10° | 96 | |
| IR-15° | ||||||||||||
| 21 | F | 19 | 12 | Combined 3Y+G | 3 | – | L | motorbike | 16 | full | 100 | |
| 22 | M | 40 | 13 | Combined Comm+G | 3 | – | R | cyclist | 12 | full | angulation of inferior angle | 95 |
Abbreviations: IR – internal rotation, ER – external rotation, R – right site, L – left site, (D) – days, (M) – months, (Y) – years, M – male patient, F – female patient, 2L – two-fragment low transverse fracture, 2H – two-fragment high transverse fracture, 3T – three-fragment T-shaped fracture, 3Y– three-fragment Y-shaped fracture, comm – comminuted fracture, SN – surgical neck fracture, TrN – transpinous neck fracture, G – fracture of glenoid fossa
Radiological imaging In all 22 patients, an anteroposterior view of the injured shoulder, Neer I and II Y views and 2D computed tomography (CT) scans were obtained prior to surgery. In 14 patients, 3D CT imaging were also obtained prior to operation.
Indication for operation In 17 cases of extra-articular fractures of the scapular body, the indication for operation was a marked displacement of fragments meeting at least the following two criteria [11]:
One hundred per cent translation of the lateral border fragments
Thirty-degree angular deformity of the lateral border and glenoid fossa
Fragment penetration in thoracic wall
In five cases, the indication was a displaced intra-articular fracture of the glenoid fossa associated with a markedly displaced fracture of the scapular body.
Surgical technique All patients were treated surgically in semiprone position via the Judet approach by the first author. During mobilisation of the infraspinatus, care was always taken to avoid injuring its neurovascular bundle at its location in the region of the spinoglenoidal sulcus. The main fracture fragments were carefully mobilised after clearing off haematoma and/or early callus. Skeletal reconstruction began with the lateral scapular border. For fractures involving the glenoid, the articular surface was initially reduced and secured with internal fixation. This was followed by reduction of the extra-articular fragments of the lateral border. For glenoid fragment fixation, we used L- and T-shaped 2.7-mm plates and 2.7-mm cortical screws followed by 3.5 dynamic compression plate (DCP), 3.5 DCP reconstructive or semitubular plates. In extra-articular fractures, the procedure was dependent on the type of fracture of the lateral border (see below). We fixed each of the main fragments using plates and a minimum of two screws. Where the fracture line ran immediately below the infraglenoid tubercle, the proximal fragment of the lateral border was too short for plate fixation by two screws. Therefore, in two cases, we placed a shaped reconstruction plate on the posterior aspect of the scapular neck and in three cases a straight plate on the posterior surface of the glenoid. It was critical to prevent screw penetration into the joint cavity (Fig. 1). The fracture of the medial border was further fixed in the spinomedial angle. In five cases, we used a contoured 3.5-mm semitubular plate, in three more muscular patients a 3.5-mm DCP reconstruction plate, in 11 cases an L-shaped 2.7-mm plate and in two cases wire cerclage. Major intercalary fragments from the central part of the infraspinatus fossa were fixed by straight or L-shaped 2.7-mm plates and screws. In two cases of an associated fracture of the surgical neck, the fragment formed by the glenoid fossa, neck and coracoid process was fixed by 3.5-mm cortical lag screws combined in one case with a wire cerclage. In one case of an associated trans-spinous scapular fracture, we performed internal fixation of the scapular spine with a 3.5-mm DCP plate. After accomplishing internal fixation, we inserted suction drainage, carefully reinserted the infraspinatus muscle and the spinal portion of the deltoid muscle and placed the extremity in a sling.
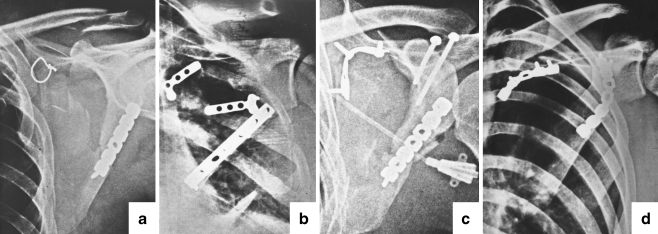
Fig. 1.
Different types of internal fixation: a Patient 3 with low transverse fracture of the body; lateral border was fixed by a 3.5-mm reconstructive dynamic compression plate (DCP) plate, medial border by wire cerclage and the clavicle fracture healed without internal fixation; b Patient 2 with low transversal fracture of the scapular body and displaced large intercalary fragment; lateral border was fixed by 3.5-mm DCP plate, medial border by 2.7-mm L plate and intercalar fragment by 2.7-mm T plate; c Patient 15 with high transversal fracture of the scapular body and surgical neck; lateral border was fixed by a 3.5-mm reconstructive DCP plate, medial border by a shaped 3.5-mm semitubular plate and fracture of the neck by two lag 3.5-mm cortical screws; d Patient 7 with high transversal fracture of the scapular body; lateral border was fixed by 3.5-mm reconstructive DCP plate, medial border by shaped 3.5-mm reconstructive DCP plate
Postoperative treatment Passive motion exercises using a continuous passive motion (CPM) machine began immediately after the surgery. Active range of motion started at four weeks and muscle and shoulder girdle exercises at six weeks. Check radiographs (Neer I and II views) were taken at six weeks and three, six and 12 months.
Evaluation We evaluated the type of the scapular body fracture, the course of fracture lines, the type of fracture of the lateral column and associated fractures. We compared preoperative imaging and intraoperative findings, and we evaluated radiological outcomes, complications and functional results [17].
Results
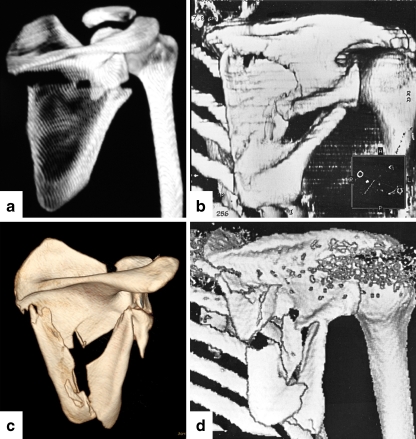
Type of fractures Fourteen cases were isolated scapular body fractures, in three the body fracture was combined with a scapular neck fracture and in five with a glenoid fossa fracture. In 14 cases, we identified a two-fragment transverse fracture of the scapular body, in four a three-fragment fracture and in four a comminuted fracture of the body (Fig. 2). Two-fragment, transverse fracture was characterised by a fracture line interrupting the lateral and medial borders of the carrying triangle. The fracture line started in the upper half of the lateral border and ran across the infraspinous fossa towards the spinomedial angle. In nine cases, the fracture line began at the lateral border close below the glenoid. We classified these fractures as high transverse fractures (Fig. 2a). In five cases, the fracture line started at ≥3 cm distal to the inferior rim of the glenoid fossa. These fractures we called low transverse fractures (Fig. 2b). In ten cases, the transverse fracture was isolated; in one it was combined with fracture of the surgical neck; and in three it was associated with fracture of the glenoid fossa.Three-fragment fracture interrupted the sides of the body in three locations, namely, in the upper half of the lateral border, in the spinomedial angle and in the area of the inferior angle (Fig. 2c). The horizontal line split the scapula body into proximal and distal fragments, whereas the vertical line split the distal fragment into medial and lateral. In two cases, the scapular body fracture was isolated and in one it was associated with fracture of the surgical neck and in one with fracture of the glenoid fossa.Comminuted fracture comprised four or more major fragments (Fig. 2d). In two cases, it was an isolated fracture of the scapular body, in one a combination with a trans-spinous fracture of the neck and in one a combination with fracture of the glenoid fossa.
Fig. 2.
Basic types of scapula body fractures: a High transverse; b low transverse; c three-fragment. pf proximal fragment, dmf distomedial fragment, dlf distolateral fragment; d comminuted fracture
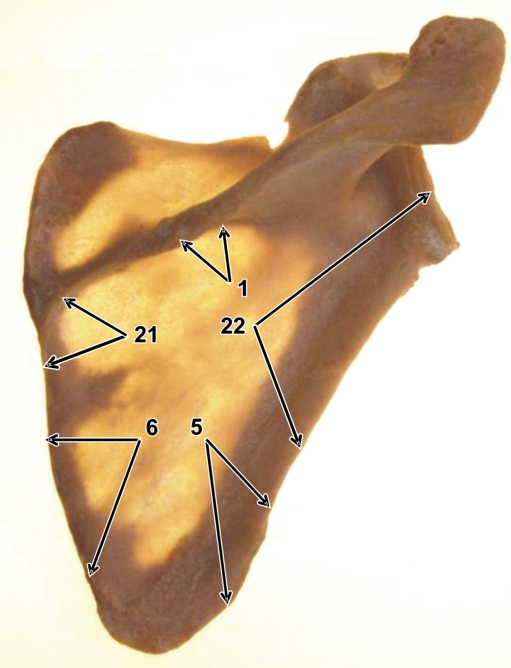
Localisation of fracture lines The upper part of the lateral border of the scapula body was affected in 21 cases. Only once in a case of a comminuted fracture of the body associated with a fracture of the glenoid fossa did the fracture line pass through the distal part of the glenoid fossa. In all 22 cases, the fracture line ran from the lateral border to the spinomedial angle where the medial border of the scapular body was fractured (Fig. 3). The medial or lateral border of the inferior angle was fractured in eight patients, namely, in a three-fragment or comminuted fracture of the scapula body. The fracture line never ran through the centre of the inferior angle. Only once, in a comminuted fracture of the body associated with a trans-spinous fracture of the neck, did the fracture line pass across the scapular spine.
Fig. 3.
Distribution of fracture lines
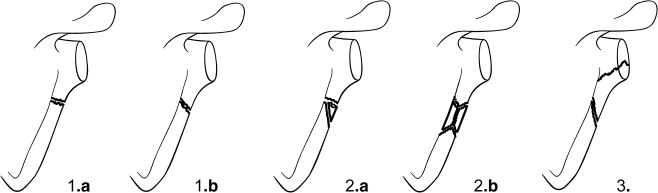
Fracture of the lateral border of the scapula According to the number of fragments, the course of fracture line and glenoid fossa involvement, we identified three basic fracture types of the lateral border of the scapula (Fig. 4). Simple two-fragment fractures of lateral border were identified in 11 cases. In seven of them, the fracture line ran across the lateral border and reduction of fragments was stable (Type 1a). In five cases the fracture line passed obliquely and reduction was unstable (Type 1b). Therefore we fixed both fragments with a short “intramedullary” peg made from a K-wire [18]. Only then it was possible to fix the lateral border using a 3.5 DCP or 3.5 DCP reconstruction plate.Fracture of lateral border with interfragment was encountered in five cases, of which twice it was a case of a small lateral hemifragment broken off the distal fragment (Type 2a). After this hemifragment was fixed to the distal fragment, reduction of the fracture of the lateral border was stable and it was possible to finalise internal fixation by a 3.5 DCP or reconstruction plate.In three cases a complete interfragment of the full width of the lateral border was broken off (Type 2b). This interfragment was always markedly angulated, displaced by pull of the muscles and split into two parts. In one case, the larger part of the interfragment was firmly stuck in the chest wall and in two cases in the surrounding muscles. Both parts of the interfragment had to be released from soft tissues, connected with two lag screws and attached with another two lag screws to the main distal fragment, in order to restore the original length of the lateral border. In the next step the interfragment and proximal fragment were reduced and bridged by a plate (Fig. 5). Fracture of lateral border with involvement of the glenoid fossa was recorded in five cases (type 3). Of these, in three cases, it was only a simple fracture of the inferior part of the glenoid fossa involving the lateral border. In the other two cases, this fracture was combined with an interfragment broken off the lateral border close below the glenoid. Reduction of these interfragments was anatomical. We used lag screws and a T- or L-shaped 2.7-mm plate. Final stabilisation was performed by 3.5-mm DCP or semitubular plate.
Fig. 4.
Classification of fractures of the lateral border. 1a simple stable fracture, 1b simple unstable fracture, 2a fracture with partial interfragment, 2b fracture with full-width interfragment, 3 fracture with involvement of glenoid fossa
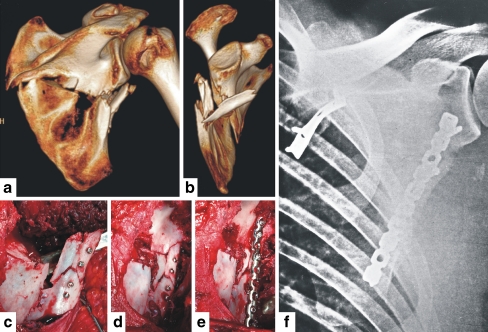
Fig. 5.
Fracture of lateral border of the right scapula with full width interfragment – type 2b. a – 3D CT posterior view, b – 3D CT lateral view, c – fixation of interfragment to distal fragment of lateral border by two lag screws, d – reconstruction of lateral border, e –final fixation by 3.5 DCP plate, f – postoperative radiograph
Types of associated fractures There were two associated fractures of the surgical neck and one trans-spinous fracture of the neck. In both fractures of the surgical neck, the fracture line started at the lateral border of the body close below the inferior rim of the glenoid and ran through the spinoglenoidal sulcus to the suprascapular notch. In one case, the suprascapular nerve was entrapped in the fracture line. In the trans-spinous fracture of the neck, the fracture line passed from the lateral border of the scapular body over the middle part of the scapular spine towards the superior border of the scapula, i.e. medial to the suprascapular notch. In the five cases of associated fractures of the glenoid fossa, the separated fragment carried the distal third or two thirds of the glenoid fossa, the superior part of which always remained intact.
Comparison of preoperative imaging and intraoperative findings In all fourteen cases in which 3D CT reconstruction was performed prior to operation, the intraoperative findings corresponded to this reconstruction. In the ten cases without preoperative 3D CT reconstruction, the type of fracture was correctly determined only twice (transverse low isolated fracture of the scapular body). In six cases, the transverse fracture was considered a fracture of the scapular neck.
Radiological and functional results Minimum follow-up was 12 months and maximum 48 months; eight patients were followed up for more than three years. In all patients, primary bone union was achieved and anatomical relationship between the glenoid and scapular body restored. In two cases with comminuted fractures of the scapular body (patients 14 and 22), the residual angulation ≤10° of inferior angle was recorded. Functional results and complications are shown in Table 1. We recorded four intraoperative and one postoperative complication. In patients 14 and 22, it was a case of insufficient reduction of the inferior angle. In patient 15, we found intraoperative entrapment of the suprascapular nerve in the fracture line of the surgical neck. Postoperatively, complete atrophy of the infraspinatus muscle developed. Despite this, the patient has a full range of movement. In patient 5, we could not perform open reduction internal fixation (ORIF) due to a sudden worsening of the patient’s general condition. In patient 18, revision surgery was required due to haematoma in the surgical site two weeks after primary operation.In 13 of 14 patients with isolated scapula body fractures, we consider the results very good. The only exception was patient 5, a uncooperative alcoholic who had in addition to the scapula fracture a clavicle fracture and incomplete paresis of the brachial plexus. Only in four cases did we record limitation of internal rotation. In patients with associated fracture of the scapular neck, the range of motion was fully restored after operation, despite injury to the suprascapular nerve (patient 15) and complete atrophy of the infraspinatus muscle. In patients with a combined fracture, the results were worse in case of associated glenoid fracture. Only three younger patients (18, 21 22) of five patients had a full range of motion in the shoulder.
Discussion
Some authors classify fractures of the scapular body according to the direction of fracture lines and others according to the number of fragments [12]. Ideberg [19], Goss [20] and Mayo et al. [21] evaluate fractures of the body within classification of fractures of the glenoid. Only the Orthopaedic Trauma Association classification distinguishes between two types of isolated fractures of the scapular body, namely, 14A3.1 – noncomminuted and 14A3.2 comminuted fractures and one type of combined fracture of the scapular body and the glenoid fossa 14C3 [22].
Most intraoperatively identified types of scapular body fractures did not fit into these classifications. The main reason in our view is that the existing classifications [19–23] were developed on the basis of plain radiographs or 2D CT scans. Only a few of these fractures were treated operatively, mostly from limited surgical approaches. As a result, a correct classification of the fracture was very difficult or even impossible. The importance of 3D CT reconstructions for a correct diagnosis of scapular fractures was proved by Bartoníček et al. [24]. However, these 3D reconstructions must cover the scapula from the anterior, posterior, medial and lateral views as well as the scapula with subtraction of the proximal humerus and clavicle.
Division of transverse fracture of the scapular body into a high and low types has a practical implication. In the low type, the lateral rim of the proximal fragment was long enough for fixation of the plate minimally using two screws. In the high type, it was necessary to place the plate as far as the posterior surface of the glenoid or use a reconstruction plate bent towards the posterior surface of the scapular neck. When applying the plate on the posterior surface of the glenoid, there is danger of incorrect screw insertion into the joint line. In the classification developed by Ada and Miller [10], the high type of transverse fracture is designated as fracture of the neck inferior to scapular spine type IIC. This may be misleading, although it has been used by other authors. The reason is that on plain radiographs, the transverse fracture of the scapular body often imitates a fracture of the surgical neck. The course of fracture lines we identified and distribution of vulnerable areas of the scapular body complies with the study by Armitage et al. [25].
The lateral border of the scapula is the key structure for reduction and internal fixation of the scapular body [1–3, 18]. However, we did not find in the literature any classification of its fractures. Only Hardagger [3] mentioned “burst” fractures of the lateral border, when a sharp spike may enter the joint capsule. The classification of fractures of the lateral border that we use has proved to be a good guideline in reduction and internal fixation.
Our main goal of operating on patients with scapular body fractures was to restore the anatomical relationship of the glenoid and the scapular body and congruency between the anterior aspect of the scapular body and chest wall, permitting smooth movement of scapula on thorax. In cases associated with fractures of the glenoid fossa, we had to restore congruency and stability of the shoulder joint. All these factors we consider as prerequisites for normal long-term function of the shoulder. Stable fixation of the lateral border was in our cases the primary step to anatomical reconstruction of a fractured scapula. Fixation of the medial border in the following step was aimed particularly at neutralising the shear and rotation forces.
The disadvantage of our study is the fact that it is a retrospective study in which there is no comparison with a similar group of patients treated nonoperatively. We based our indications on criteria reported in the literature [11–16] and on the poor outcomes of nonoperatively treated scapular fractures [4–8]. We consider the value of this study to be in the fact that in each patient, the fracture type of the scapular body was described and the functional result classified. Determination of the exact type of fracture of the scapular body and fragment displacement was possible only with 3D CT imaging. The radiological and functional results of the operative treatment achieved are encouraging. Nevertheless, comparison with a control group will be necessary to make indication for operative treatment of these fractures more precise.
Acknowledgment
The authors thank J. Jupiter, M.D. for his assistance in the preparation of the manuscript.
Contributor Information
Jan Bartoníček, Phone: +420-2-67162431, FAX: +420-2-67313372, Email: bartonicek.jan@seznam.cz.
Vladimír Frič, Phone: +420-2-67162430, FAX: +420-2-67313372, Email: fric@fnkv.cz.
References
- 1.Judet R. Traitement chirurgical des fractures de l´omoplate. Acta Orthop Belg. 1964;30:673–678. [PubMed] [Google Scholar]
- 2.Magerl F. Osteosynthesen im Bereich der Schulter. Helv Chir Acta. 1974;41:225–232. [PubMed] [Google Scholar]
- 3.Hardegger F, Simpson LA, Weber BG. The operative treatment of scapula fractures. J Bone Joint Surg Br. 1984;66-B:725–731. doi: 10.1302/0301-620X.66B5.6501369. [DOI] [PubMed] [Google Scholar]
- 4.Armstrong CP, Spuy J. The fractures scapula: Importance and management based on series of 62 patients. Injury. 1984;15:324–329. doi: 10.1016/0020-1383(84)90056-1. [DOI] [PubMed] [Google Scholar]
- 5.Nordqvist A, Petersson C. Fractures of the body, neck, or spine of the scapula. Clin Orthop Relat Res. 1992;283:139–144. [PubMed] [Google Scholar]
- 6.Romero J, Schai O, Imhoff AB. Scapula neck fracture: the influence of permanent malalignment of the glenoid neck on clinical outcome. Arch Orthop Trauma Surg. 2001;121:313–316. doi: 10.1007/s004020000224. [DOI] [PubMed] [Google Scholar]
- 7.Pace AM, Stuart R, Brownlow H. Outcome of glenoid neck fractures. J Shoulder Elbow Surg. 2005;14:585–590. doi: 10.1016/j.jse.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Bozkurt M, Can F, Kirdemir V, Erden Z, Demirkale I, Bosbozkurt M. Conservative treatment of scapula neck fracture: the effect of stability and glenopolar angle on clinical outcome. Injury. 2006;36:1176–1181. doi: 10.1016/j.injury.2004.09.013. [DOI] [PubMed] [Google Scholar]
- 9.Bauer G, Fleuschmann W, Dussler E. Displaced scapula fractures: indication and long-term results of open reduction and internal fixation. Arch Orthop Trauma Surg. 1995;114:215–219. doi: 10.1007/BF00444266. [DOI] [PubMed] [Google Scholar]
- 10.Ada JR, Miller ME. Scapula fractures. Analysis of 113 cases. Clin Ortop Relat Res. 1991;269:174–180. [PubMed] [Google Scholar]
- 11.Cole PA. Scapula fractures. Orthop Clin N Amer. 2002;33:1–18. doi: 10.1016/S0030-5898(03)00069-5. [DOI] [PubMed] [Google Scholar]
- 12.Bartoníček J, Cronier P. History of treatment of scapula fractures. Arch Orthop Trauma Surg. 2010;130:83–92. doi: 10.1007/s00402-009-0884-y. [DOI] [PubMed] [Google Scholar]
- 13.Hersovici D, Roberts CS. Scapula fractures: to fix or not to fix? J Orthop Trauma. 2006;20:227–229. doi: 10.1097/00005131-200603000-00012. [DOI] [PubMed] [Google Scholar]
- 14.Lantry JM, Roberts CS, Giannoudis PV. Operative treatment of scapular fractures: a systematic review. Injury. 2008;39:271–283. doi: 10.1016/j.injury.2007.06.018. [DOI] [PubMed] [Google Scholar]
- 15.Nork SE, Barei DP, Gardner MJ, Schildhauer TA, Mayo KA, Benirschke SK. Surgical exposure and fixation of displaced type IV, V and VI glenoid fractures. J Orthop Trauma. 2008;22:487–493. doi: 10.1097/BOT.0b013e31817d5356. [DOI] [PubMed] [Google Scholar]
- 16.Herrera DA, Anavian J, Tarkin IS, Armitage BA, Chroder LK, Cole PA. Delayed operative management of fractures of the scapula. J Bone Joint Surg Br. 2009;91-B:619–626. doi: 10.1302/0301-620X.91B5.22158. [DOI] [PubMed] [Google Scholar]
- 17.Constant CR, Murley AH. Clinical method of functional asesment of the shoulder. Clin Orthop Relat Res. 1987;214:160–164. [PubMed] [Google Scholar]
- 18.Bartoníček J, Frič V, Tuček M. Intra-operative reduction of the scapular body - A technical trick. J Orthop Trauma. 2009;23:294–298. doi: 10.1097/BOT.0b013e31819f1dad. [DOI] [PubMed] [Google Scholar]
- 19.Ideberg R, Grevsten S, Larsson S. Epidemiology of scapula fractures. Acta Orthop Scand. 1995;66:395–397. doi: 10.3109/17453679508995571. [DOI] [PubMed] [Google Scholar]
- 20.Goss TP. Scapula fractures and dislocations: diagnosis and treatment. J Am Acad Orthop Surg. 1995;3:22–33. doi: 10.5435/00124635-199501000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Mayo KA, Benirschke SK, Mast JW. Displaced fractures of the glenoid fossa. Clin Orthop Relat Res. 1998;346:122–130. [PubMed] [Google Scholar]
- 22.Association OT. Fracture and dislocation compendium. Scapula fractures. J Orthop Trauma. 2007;21(Suppl 1):S68–S71. [Google Scholar]
- 23.Euler E, Habermeyer P, Kohler W, Schweiberer L. Skapulafrakturen - Klassifikation und Differentialtherapie. Orthopäde. 1992;21:158–162. [PubMed] [Google Scholar]
- 24.Bartoníček J, Frič V, Tuček M. Radiographic evaluation of scapula fractures. Rozhl Chir. 2009;88:84–88. [PubMed] [Google Scholar]
- 25.Armitage BM, Wijdicks CA, Tarkin IS, Schroder LK, Marek DJ, Zlowodzki M, Cole PA. Mapping of scapular fractures with three-dimensional computed tomography. J Bone Joint Surg Am. 2009;91:2222–2228. doi: 10.2106/JBJS.H.00881. [DOI] [PubMed] [Google Scholar]