Abstract
Patients with Down’s syndrome (DS) have an increased incidence of coxarthrosis which may become symptomatic with prolonged life expectancy. We present seven consecutive patients (nine hips) with DS who had primary total hip arthroplasty (THA). Average clinical and radiological follow-up was 9.9 ± 6.4 years (range 2–22.25). Harris hip scores (HHS) improved significantly (p < 0.01) from 41.1 (range 18.5–65) to 80.2 (range 67.5–91) at latest follow-up. Two patients required revision arthroplasty for stem loosening at 16 (osteolysis) and six years (trauma) following THA, respectively. Six of the THAs required a constrained liner. No dislocations or deep infections were encountered. We contend that THA is a reliable surgical intervention in patients with DS and may be performed in symptomatic patients.
Introduction
Down’s syndrome (DS) is the most common chromosomal disorder diagnosed between 1 in 650 to 1 in 1000 live births accounting for an estimated 550 infants births annually in the United States [1]. Apart from intellectual disability, patients with DS are prone to musculoskeletal disorders. Ligamentous hyperlaxity and muscle hypotonia cause instability, subluxation and dislocation affecting the cervical spine, knees and hips [2–4]. Hip abnormalities include coxa valga, capsular and ligamentous hyperlaxity and acetabular dysplasia [4]. Furthermore, DS is associated with a higher incidence of slipped capital epiphysis (1.3%), Perthes’ disease (2%) and hip dislocations (2.9%) leading to increased incidence of hip osteoarthritis [4].
With improved health care, life expectancy has increased from only 12 in 1949 [5] to an average of almost 60 years currently in developed countries [6–10]. Thus, disabling hip pain is now more frequently encountered and needs to be more definitively addressed. This suggests a greater role for total hip arthroplasty (THA). However, only limited data is available in the literature about the challenges of THA in DS patients and their clinical outcomes. Previous reports have indicated increased rates of instability (11%) and early aseptic loosening (11%) [11]. In addition, wound infections and lack of compliance are concerns, leading to recommendation for added precautions [11, 12].
Materials and methods
This study included seven consecutive patients (nine hips) with DS and symptomatic hip osteoarthritis. The patients were accompanied by their family members who described an ongoing deterioration in walking due to increased pain that interfered with their activities of daily living. In all patients primary THA was performed under the supervision of the senior author (AEG) over a period of two decades from March 1986 onwards.
Collarless, proximally porous coated, cementless femoral stems and hemispheric porous coated cementless cups secured with screws were used in all patients. Leg length was restored intraoperatively with the aid of a rigid measurement device fixed to the iliac wing routinely used in our institution. The distance from the iliac wing to a point in the femoral shaft was marked prior to hip dislocation. The components’ size and offset were determined in order to compensate for the pre-operative clinical and radiographic leg length discrepancy. If adequate stability could not be achieved despite restoration of leg length discrepancy and impingement was ruled out, then the patient was regarded as hyperlax. In six of the THAs a constrained liner was used to enhance stability due to soft tissue hyperlaxity and patients’ anticipated inability to adhere to postoperative hip precautions.
Patients’ medical records were reviewed after a specific approval of the institutional IRB was received.
Average age at surgery was 34.8 ± 7.5 years (range 25–47, median 35.4, Table 1). Coxarthrosis was secondary to developmental hip dysplasia (DDH) in six patients (Fig. 1) and slipped capital femoral epiphysis (SCFE) in one patient. Four patients (five hips) had at least one previous hip operation for their underlying condition (Table 1). Average follow-up was 9.9 ± 6.4 years (range 2–22.3, median 9.3, Table 1). Component design, use of constrained liner, surgical approach (trans gluteal, trochanteric slide) and use of supplementary aids to enhance postoperative stability were documented (Table 1).
Table 1.
Preoperative and intraoperative patient data
| Patient code | Follow-up (years) | Age at surgery (years) | Side | Hip pathology | aAcetabular dysplasia | Previous hip surgeries | Surgical approach | Constrained liner | Acetabular component design |
|---|---|---|---|---|---|---|---|---|---|
| 1 (L) | 5.8 | 25 | Left | DDH | Type 3 | 2 | Trochanteric slide | yes | Osteonics |
| 1 (R) | 5.0 | 26 | Right | DDH | Type 2 | 2 | Trochanteric slide | yes | Osteonics |
| 2 | 22.3 | 47 | Left | DDH | Type 3 | 0 | Transgluteal | yes | PCA (Howmedica) |
| 3 | 9.5 | 36 | Right | DDH | Type 2 | 0 | Transgluteal | no | PCA (Howmedica) |
| 4 | 5.8 | 43 | Left | DDH | Type 2 | 0 | Transgluteal | yes | Osteonics |
| 5 | 15.8 | 32 | Right | DDH | Type 2 | 1 | Transgluteal | no | Osteonics |
| 6 | 14.3 | 39 | Right | DDH | Type 2 | 3 | Trochanteric slide | no | PCA (Howmedica) |
| 7 (R) | 9.3 | 29 | Right | SCFE | Type 2 | 0 | Transgluteal | yes | Osteonics |
| 7 (L) | 2.0 | 36 | Left | SCFE | Type 2 | 1 | Transgluteal | yes | Trabecular Metal (Zimmer) |
| Average | 9.9 | 34.8 | |||||||
| Min | 2.0 | 25.0 | |||||||
| Max | 22.3 | 47.0 | |||||||
| Median | 9.3 | 35.4 | |||||||
| STDEV | 6.4 | 7.5 |
STDEV standard deviation, DDH developmental dysplasia of hip, SCFE slipped capital femoral epiphysis
a Type of acetabular dysplasia is according to Hartofilakidis et al. [13]
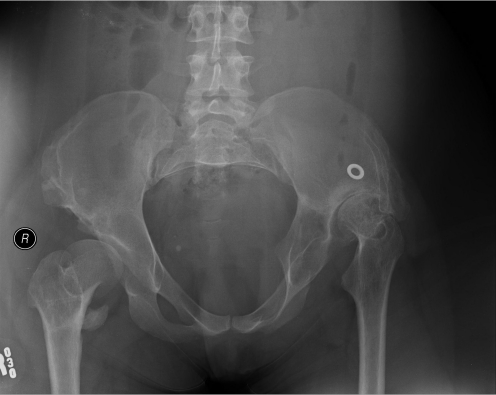
Fig. 1.
Preoperative X-ray of a patient with Down syndrome and bilateral developmental hip dysplasia (DDH)
Follow-up consisted of clinical and radiographic examination at standard postoperative intervals (preoperative, postoperatively at six weeks, six months, at one year and then annually). Clinical evaluations included leg length discrepancy (LLD) preoperatively and postoperatively. The Harris hip score (HHS) was recorded in the presence of accompanying family members or carers (Table 2) to confirm the validity of the data.
Table 2.
Harris hip scores (HHS) pre-operative and at postoperative follow-up
| Patient code | Presurgery | Six weeks | Six months | One year | Two years | Four years | Five years | Seven years | Eight years | Ten years | 15 years | 17 years |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 (L) | 46.5 | 60.5 | 76.5 | 79.5 | 91.0 | 91.0 | 90 | |||||
| 1 (R) | 21.5 | 65.5 | 72.5 | 80.0 | 91.0 | 91.0 | 91 | |||||
| 2 | 65.5 | 41.5 | 41.5 | 74.0 | 83.0 | 82.0 | 80 | 77 | 66.5 | 65.5 | 34 | |
| 3 | 31 | 74 | 86.5 | 86.5 | 93.5 | 82.5 | 82.5 | 80 | ||||
| 4 | 39.5 | 67 | 72.5 | 83.0 | 83.5 | 89.0 | 85.5 | |||||
| 5 | 18.5 | 60 | 65 | 75.5 | 83.5 | 80.0 | 71.5 | 69 | 69 | 67.5 | ||
| 6 | 45 | 51.5 | 55.5 | 91.0 | 91.5 | 93.0 | 90.5 | |||||
| 7 (R) | 50.5 | 51.5 | 56.5 | 68.0 | 67.0 | 70.0 | 67 | 67 | 68 | |||
| 7 (L) | 51.5 | 60 | 55.5 | 80.5 | 83.0 | |||||||
| Average | 41.1 | 59.1 | 64.7 | 79.8 | 85.2 | 84.8 | 77.3 | 71.0 | 70.9 | 65.5 | 34 | 67.5 |
| Min | 18.5 | 41.5 | 41.5 | 68.0 | 67.0 | 70.0 | 67.0 | 67.0 | 66.5 | 65.5 | 34.0 | 67.5 |
| Max | 65.5 | 74.0 | 86.5 | 91.0 | 93.5 | 93.0 | 90.5 | 77.0 | 80.0 | 65.5 | 34.0 | 67.5 |
| Median | 45.0 | 60.0 | 65.0 | 80.0 | 83.5 | 85.8 | 75.8 | 69.0 | 68.0 | 65.5 | 34.0 | 67.5 |
| STDEV | 15.1 | 9.7 | 13.7 | 6.8 | 8.1 | 7.7 | 9.3 | 5.3 | 6.2 |
STDEV standard deviation
Routine hip radiographs (anterior-posterior [AP] view of the pelvis and anterior-posterior and lateral view of the affected hip) were taken to evaluate preoperative acetabular dysplasia (Fig. 1) [13]. The initial six-week postoperative series of radiographs served as the baseline to which all subsequent radiographs were compared. Radiographs were evaluated by two of the authors (A.E.G and Y.K) for evidence of component migration or loosening.
Acetabular migration was measured according to criteria published by Massin and Engh [14] and any radiolucent lines or osteolytic lesions measuring 1 cm2 or more in the zones described by DeLee and Charnley were recorded [15]. Acetabular component migration was deemed positive if >5 mm migration occurred or if the radiographs demonstrated circumferential radiolucent lines, including the area around the screws.
Loosening of the femoral stem was defined as progressive subsidence of >3 mm or varus-valgus shift of more than 3 degrees [16]. Stem subsidence was evaluated by measuring the distance from the tip of the greater trochanter and the upper margin of the lateral shoulder of the stem, and the distance between the most proximal medial part of the porous coated surface of the stem and the upper border of the lesser trochanter was measured. A femoral component was considered possibly loose when there was a complete radiolucent line surrounding the entire stem both on AP and lateral radiographs [17, 18].
One way ANOVA test was used to compare HHS at follow-up. For all statistical tests a P value < 0.05 was considered to be statistically significant.
Results
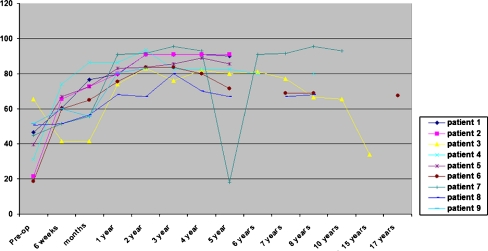
The average HHS improved from 41.1 ± 15.1 (range 18.5–65.5, median 45) preoperatively to 59.1 ± 9.7 (range 41.5–74, median 60) at six weeks postsurgery. Average HHS further improved at six months (64.7 ± 13.7, range 41.5–86.5, median 65), at one year (79.8 ± 6.8, range 68–91, median 80) and at two years (85.2 ± 8.1, range 67–93.5, median 83.5) following surgery. Postoperative HHS were found significantly improved at one-year (p < 0.05) and two-year (p < 0.01) follow-up compared to preoperative HHS (Table 2). HHS remained essentially unchanged (p = 0.43) at four-year (84.8.3 ± 7.7, range 70–93, median 85.8) and eight-year (70.9 ± 6.2, range 66.5–80, median 68) follow-up (Table 2, Fig. 3).
Fig. 3.
Harris hip scores (HHS) recorded at patient's follow-up visits. Please note that HHS reached a lasting plateau at one year after total hip arthroplasty (THA). THA 7 had a sudden drop in her HHS due to a periprosthetic fracture and returned to pre fracture levels after the revision THA. THA 3 had a gradual decline of his HHS in the last few years prior to his hip revision due to stem loosening
Seven out of the nine THAs were radiographically well fixed at the last follow-up. Two patients required revision arthroplasty for stem loosening at six and 16 years following THA, respectively. In both patients the acetabular component was well fixed and did not require a revision.
The first patient (patient code 6, Table 2) was doing very well with a HHS over 90 in the first five years after surgery. During the sixth year she sustained a periprosthetic fracture (B3 according to the Vancouver Classification [19, 20]) following a fall. Her stem was revised with a modular tapered stem (ZMR, Zimmer, Warsaw, Indiana) along with a strut bone graft to support the proximal femur. Surgical approach was through an extended trochanteric osteotomy to the fracture. At seven years post revision she walked without aids. Her HHS at last follow-up was 91.
The second patient (patient code 2, Table 2) had loosening of the femoral stem. Due to proximal femoral osteolysis the surgical approach was through a trochanteric osteotomy that maintained the continuity of the abductors, greater trochanter bony shell and vastus lateralis. The patient had fibrous nonunion of the osteotomy. At 6.1 years post revision he ambulated with a walker. His HHS at six-year follow-up was 73.5. At 22.3 years after index hip reconstruction there was no sign of failure of the shelf autograft that had been used to augment the superolateral acetabulum.
Another patient has used a cane since surgery. None of the other patients were using walking aids at the last follow-up.
Operated leg LLD was altered by an average of 1.7 ± 1.1 cm (range 0.5–4, median 1.5, Table 3). In eight of the nine (88.8%) hips LLD was reduced. One of the patients with a high dislocated hip, grade 3 dysplasia [13], was lengthened by 4 cm without neurological compromise. However, in one patient, during THA of the contralateral hip, LLD was increased from 0 to 0.5 cm.
Table 3.
Postoperative functional outcome (LLD, use of walking aids)
| Patient code | Side | LLD presurgery | LLD postsurgery | ∆ LLD (cm) | Use of walking aids |
|---|---|---|---|---|---|
| 1 (L) | Left | 2 cm short | 0 | 2 | No aids |
| 1 (R) | Right | 0 | 0.5 cm long | 0.5 | No aids |
| 2 | Left | 5 cm long | 1 cm short | 4 | Walker |
| 3 | Right | 2 cm short | 0.5 cm short | 1.5 | No aids |
| 4 | Left | 2.5 cm short | 1 cm short | 1.5 | No aids |
| 5 | Right | 1 cm long | 0 | 1 | No aids |
| 6 | Right | 4 cm short | 2.5 cm short | 1.5 | Cane |
| 7 (R) | Right | 4 cm short | 1.5 cm short | 2.5 | No aids |
| 7 (L) | Left | 1.5 cm short | 1 cm short | 0.5 | No aids |
| Average | 1.7 | ||||
| Min | 0.5 | ||||
| Max | 4.0 | ||||
| Median | 1.5 | ||||
| STDEV | 1.1 |
LLD leg length discrepancy, STDEV standard deviation
No dislocations, superficial or deep infections were encountered in any of the patients. There were no complications related to anaesthesia. At the last follow-up, all patients were fully mobile. There was no clinical evidence of discomfort and range of motion was satisfactory in all patients.
Discussion
Hip osteoarthritis is a significant problem in DS patients with a prevalence of 8–28% [4, 21]. However, there are few reports of treatment options in this group of patients. Gill et al. reported on the possible causes for surgeons’ reluctance to perform THA in these patients, including anticipated aggressive behaviour and non-compliance which may lead to increased rates of dislocations [22].
Despite the very favourable results which we report in this study, several medical conditions such as upper cervical spine instability, cardiac anomalies, susceptibility to infections and early development of Alzheimer’s should be taken into account during the preoperative evaluation of these patients [5–9].
Preoperative lateral flexion/extension radiographs of the cervical spine are required to rule out upper cervical instability [2]. Congenital cardiac anomalies are present in about 40% and require appropriate cardiac work-up. Although abnormalities of the immune system are common, wound infection rates were not found to be increased in our patients or in previous reports of DS patients undergoing THA [11, 12].
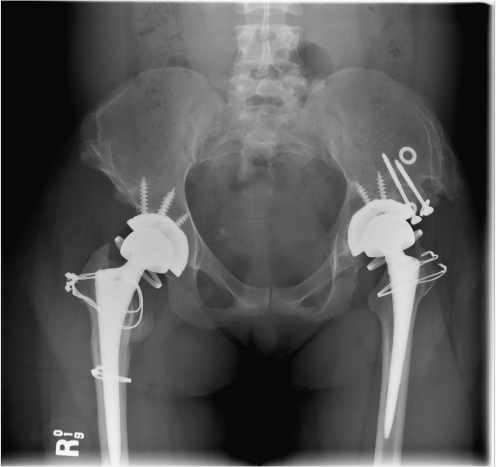
Possible orthopaedic challenges which need to be addressed include acetabular dysplasia, deformed femoral neck, narrow femoral canal and postoperative ligamentous hyperlaxity with higher susceptibility to dislocation. Kioschos et al. reported good results of THA in nine hips in six patients with an average follow up of 7.75 years [11]. They report use of reamed bipolar arthroplasty in three of their patients, a technique in which the acetabulum is reamed to bone and articulates directly with a bipolar femoral head. Moreover, they used adjunctive precautions such as spica cast (three patients) and abduction braces (two patients) in order to address postoperative instability. One patient with a reamed bipolar prosthesis dislocated in the early postoperative period (day 5) and was treated by an open reduction. Another patient was revised due to aseptic loosening attributed to cup malposition and impingement at 7.8 years after surgery. In our study, constrained liners were used in six hips as ancillary measures to ensure adequate stability (Fig. 2). The authors prefer using constrained liners since it is our opinion that they provide more reliable pain relief as there is no motion between the metal head on the acetabular bone. The decision to use constrained liners was based on intraoperative evaluation of soft tissue laxity and the anticipated inability of the patient to adhere to standard postoperative hip precautions. Although none of the patients in our study required cup revision during the follow-up period, Trabecular Metal (Zimmer, Warsaw, Indiana) cups with constrained liners may be an option to enhance cup fixation and longevity. Larger femoral heads may not provide supplementary stability as they mainly address impingement rather than hyperlaxity. No additional precautions such as bracing or spica casts were used in any of the patients.
Fig. 2.
Postoperative X-ray of the patient. Total hip arthroplasty (THA) was performed through a modified trochanteric slide bilaterally. A shelf autograft was performed to support the left dysplastic acetabulum. Trochanteric slides had a bony union bilaterally
A modified trochanteric slide (Fig. 2) as described by the senior author was used in two patients (three hips) who had two or more previous operations around the hip (Table 1); a lateral transgluteal approach was used in the remaining patients [23, 24]. In all three primary THAs, the osteotomies healed well without complications.
Two patients required femoral stem revision. Both patients’ HHS demonstrate their clinical course (Fig. 3). The first patient (patient code 7) was doing very well clinically with HHS over 90 in her annual follow-up visits, without any clinical symptoms indicative of stem loosening. Unfortunately, she sustained a severe fall leading to a Vancouver type-B3 periprosthetic femoral fracture accompanied by premature stem loosening and considerable proximal femoral bone loss [20]. This data was retrieved from the operative note as the X-rays documenting the fracture are unavailable. A modular tapered stem was used to provide distal fixation (ZMR, Zimmer, Warsaw, Indiana). Due to the proximal bone loss, a strut bone graft was used to provide proximal support and reduce the load from the prosthetic modular junction. The patient recovered well from her revision, and at seven years after revision THA her HHS returned to over 90 and she walked without aids. Radiographs taken at the last follow-up demonstrate a healed extended osteotomy with well fixed femoral and acetabular implants. It is reasonable to assume that without the fall, the stem was not loose as her HHSs were consistently high.
The second patient (patient code 3) had stem loosening due to osteolysis. His HHS gradually declined in the 10–15 years follow-up period (Fig. 3). The femoral stem was revised through a trochanteric osteotomy preserving the continuity of the hip abductors, greater trochanter bony shell and vastus lateralis to prevent uncontrolled fracture of the greater trochanter. Unlike the modified trochanteric osteotomies used for the primary THA, this patient had fibrous non union of the osteotomy with proximal migration of the greater trochanter. The broken wires caused no irritation and were left in situ. At 6.1 years after revision he ambulated with a walker. HHS at six-year follow-up was 73.5. At 22.3 years post primary THA there was no sign of failure of the shelf autograft that had been used to augment the superolateral acetabulum. In both of these patients the acetabular components were well fixed and were left in situ during the revision. At the last follow-up 14.4 and 22.3 years post primary THA there was no evidence of excessive osteolysis around the acetabulum.
In all patients a relatively gradual yet consistent improvement in HHS after surgery was found, reaching a plateau at one year throughout follow-up (Fig. 3). Surgeons, patients and their families should be aware of this postoperative course. It should be discussed well beforehand in order to match patient-family-surgeon expectations.
LLD in these patients can be minimised and often restored. None of the patients in the study required any walking aids at ten years post THA. Patient number 5 started to use a cane at ten years after primary THA and patient number 3 required a walker only after his revision THA.
Patients with DS require careful medical, social and orthopaedic preoperative evaluation and preparation. THA in these patients may be relatively more demanding surgically due to the presence of bony deformities typical of DDH affecting both acetabulum and femur. In addition, soft tissue hyperlaxity may compromise postoperative stability, especially if smaller sized femoral heads are to be used.
Thus, appropriate THA designs including smaller sized stems to fit the narrow femoral canal and metallic augmentations or structural bone autograft to support the acetabular cup should be available in order to allow the surgeon to address these challenges. In complex cases, a modified trochanteric slide to facilitate surgical exposure is advised. Constrained liners can be used to enhance stability especially when tissue hyperlaxity is encountered in less compliant patients. External stabilisers such as spica or abduction braces are not required.
Based on these results we contend that THA is a reliable surgical intervention in patients with DS and symptomatic coxarthrosis. With appropriate patient selection this group can be expected to have long-term pain relief and good mobility following THA.
Acknowledgements
The authors would like to thank Matthew Macdonald at the Mount Sinai Orthopedic Department for his support in statistical analysis and data collection for our study.
References
- 1.Stoll C, Alembik Y, Dott B, Roth MP. Study of Down syndrome in 238,942 consecutive births. Ann Genet. 1998;41:44–51. [PubMed] [Google Scholar]
- 2.Kriss VM. Down syndrome: imaging of multiorgan involvement. Clin Pediatr. 1999;38:441–449. doi: 10.1177/000992289903800801. [DOI] [PubMed] [Google Scholar]
- 3.Nance WE, Engel E. Human cytogenetics: a brief review and presentation of new findings. J Bone Joint Surg Am. 1967;49:1436–1454. [PubMed] [Google Scholar]
- 4.Shaw ED, Beals RK. The hip joint in Down's syndrome. A study of its structure and associated disease. A study of its structure and associated disease. Clin Orthop Relat Res. 1992;278:101–107. [PubMed] [Google Scholar]
- 5.Penrose LS. The incidence of mongolism in the general population. J Ment Sci. 1949;95:685–688. doi: 10.1192/bjp.95.400.685. [DOI] [PubMed] [Google Scholar]
- 6.Bittles AH, Glasson EJ. Clinical, social, and ethical implications of changing life expectancy in Down syndrome. Dev Med Child Neurol. 2004;46:282–286. doi: 10.1111/j.1469-8749.2004.tb00483.x. [DOI] [PubMed] [Google Scholar]
- 7.Friedman JM. Radical disparities in median age at death of persons with Down syndrome. United States, 1968–1997. MMWR Morb Mortal Wkly Rep. 2001;50:463–465. [PubMed] [Google Scholar]
- 8.Glasson EJ, Sullivan SG, Hussain R, Petterson BA, Montgomery PD, Bittles AH. The changing survival profile of people with Down's syndrome: implications for genetic counselling. Clin Genet. 2002;62:390–393. doi: 10.1034/j.1399-0004.2002.620506.x. [DOI] [PubMed] [Google Scholar]
- 9.Glasson EJ, Sullivan SG, Hussain R, Petterson BA, Montgomery PD, Bittles AH. Comparative survival advantage of males with Down syndrome. Am J Hum Biol. 2003;15:192–195. doi: 10.1002/ajhb.10132. [DOI] [PubMed] [Google Scholar]
- 10.Janicki MP, Dalton AJ, Henderson CM, Davidson PW. Mortality and morbidity among older adults with intellectual disability: health services considerations. Disabil Rehabil. 1999;21:284–294. doi: 10.1080/096382899297710. [DOI] [PubMed] [Google Scholar]
- 11.Kioschos M, Shaw ED, Beals RK. Total hip arthroplasty in patients with Down's syndrome. J Bone Joint Surg Br. 1999;81:436–439. doi: 10.1302/0301-620X.81B3.9452. [DOI] [PubMed] [Google Scholar]
- 12.Skoff HD, Keggi K. Total hip replacement in Down's syndrome. Orthopedics. 1987;10:485–489. doi: 10.3928/0147-7447-19870301-15. [DOI] [PubMed] [Google Scholar]
- 13.Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N. Congenital hip disease in adults. Classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg Am. 1996;78:683–692. doi: 10.2106/00004623-199605000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Massin P, Schmidt L, Engh CA. Evaluation of cementless acetabular component migration. An experimental study. J Arthroplasty. 1989;4:245–251. doi: 10.1016/S0883-5403(89)80020-8. [DOI] [PubMed] [Google Scholar]
- 15.DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976;121:20–32. [PubMed] [Google Scholar]
- 16.Kim YH. The results of a proximally-coated cementless femoral component in total hip replacement: a five- to 12-year follow-up. J Bone Joint Surg Br. 2008;90:299–305. doi: 10.1302/0301-620X.90B3.20096. [DOI] [PubMed] [Google Scholar]
- 17.Engh CA, Jr, Culpepper WJ, Engh CA. Long-term results of use of the anatomic medullary locking prosthesis in total hip arthroplasty. J Bone Joint Surg Am. 1997;79:177–184. doi: 10.1302/0301-620X.79B2.7640. [DOI] [PubMed] [Google Scholar]
- 18.Kim YH, Kim JS, Oh SH, Kim JM. Comparison of porous-coated titanium femoral stems with and without hydroxyapatite coating. J Bone Joint Surg Am. 2003;85:1682–1688. doi: 10.1302/0301-620X.85B2.13289. [DOI] [PubMed] [Google Scholar]
- 19.Kellett CF, Boscainos PJ, Maury AC, Pressman A, Cayen B, Zalzal P, Backstein D, Gross A. Proximal femoral allograft treatment of Vancouver type-B3 periprosthetic femoral fractures after total hip arthroplasty. Surgical technique. J Bone Joint Surg Am. 2007;89:68–79. doi: 10.2106/JBJS.F.01047. [DOI] [PubMed] [Google Scholar]
- 20.Maury AC, Pressman A, Cayen B, Zalzal P, Backstein D, Gross A. Proximal femoral allograft treatment of Vancouver type-B3 periprosthetic femoral fractures after total hip arthroplasty. J Bone Joint Surg Am. 2006;88:953–958. doi: 10.2106/JBJS.E.00120. [DOI] [PubMed] [Google Scholar]
- 21.Hresko MT, McCarthy JC, Goldberg MJ. Hip disease in adults with Down syndrome. J Bone Joint Surg Br. 1993;75:604–607. doi: 10.1302/0301-620X.75B4.8331117. [DOI] [PubMed] [Google Scholar]
- 22.Gill CE, Taylor HM, Lin KT, Padaliya BB, Newman WJ, Abramovitch AI, Richardson CR, Charles PD. Difficulty in securing treatment for degenerative hip disease in a patient with Down syndrome: the gap remains open. J Natl Med Assoc. 2006;98:93–96. [PMC free article] [PubMed] [Google Scholar]
- 23.Goodman S, Pressman A, Saastamoinen H, Gross A. Modified sliding trochanteric osteotomy in revision total hip arthroplasty. J Arthroplasty. 2004;19:1039–1041. doi: 10.1016/j.arth.2004.03.023. [DOI] [PubMed] [Google Scholar]
- 24.Gross AE, Goodman S. The current role of structural grafts and cages in revision arthroplasty of the hip. Clin Orthop Relat Res. 2004;429:193–200. doi: 10.1097/01.blo.0000149822.49890.5e. [DOI] [PubMed] [Google Scholar]