Abstract
The purpose of this study was to investigate the influence of body function, activities and pain on the level of activity in adults with Kashin Beck Disease (KBD). Seventy-five KBD patients with a mean age of 54.8 years (SD 11.3) participated. Anthropometrics, range of joint motion (ROM) and muscle strength were measured as well as the time-up-and-go test and functional tests for the lower and upper extremities. Activity was assessed with the participation scale and the WHO DAS II. In the shoulder, elbow, hip and knee joints, a severe decrease in ROM and bilateral pain was noted. A decrease in muscle strength was observed in almost all muscles. The timed-up-and-go test scores decreased. No or mild restriction in activity was found in 35%, and 33% experienced a moderate restriction whereas 32% had severe to extreme restriction. Activities in the lower extremities were mildly to moderately correlated to ROM and muscle strength, whereas in the upper extremities activities were correlated to range of joint motion. Activity was significantly associated with ROM after correction for muscle strength, gender and age. Participation was borderline significantly associated with ROM after correction for muscle strength, gender, age and the activity time-up-and-go. In KBD adults, a severe decrease in activity is primarily caused by decrease in ROM. These findings have strong influence on rehabilitation and surgical intervention.
Introduction
Kashin Beck Disease (KBD) is a chronic joint disease with decreased health conditions causing major functional limitations and disability of unknown origin.
KBD has a typical crescent geographical distribution, primarily in agricultural regions of eastern Siberia, northern Korea and in the central regions of China. The disease is widely distributed in China, from Heilongjiang in the north-east to Sichuan and Tibet in the south-west where at least 1 million people are affected [1].
The prevalence varies, some villages are severely affected with 60–90% of children showing signs of KBD [1, 2].
The pathogenesis has not been fully unravelled yet, but the general presumption is that the aetiology is multi-factorial (combination of nutritional, environmental, immunological, genetic, and infectious factors). A possible relationship exists between KBD and osteoarthritis (OA) in their pathogenic pathways despite their different aetiology [3]. Nutritional deficiency (selenium and iodine) is present in KBD endemic rural areas. Also deficiencies in micro nutrients such as vitamin A, D, E, and calcium might play a role [1].
Another hypothesis is that KBD might be caused by mycotoxins, by which the proteoglycan synthesis is disturbed, leading to severe cartilage damage. The epiphyseal plate of cartilage from young and adolescent KBD patients shows necrosis and apoptosis in the hypertrophic layer near the adjacent subchondral bone [3, 4].
Researchers are pursuing new leads in genetics such as polygenetic inheritance. Genetic susceptibility accounts for one fourth of the risk factor for KBD, which might explain why certain population groups are more vulnerable, why boys are more affected than girls and why patients with KBD are more likely to have siblings with KBD [1, 5].
The clinical manifestations are related to decrease in growth and multiple joint damage. The worst form of the disease starts at childhood (age 2–3 years) and may result in dwarfism. Signs of symmetrical severe articular deformities caused by primary epiphyseal destruction are followed by severe cartilage destruction resulting in restriction of movements and metaphyseal enlargement. The distal joints of the upper and lower limbs are most often and most severely affected. Frequently involved joints are the ankle-, wrist-, knee- and elbow joint. Patients experience arthritic pain, morning stiffness, shortened fingers, deformed and/or enlarged joints, with limited motion in the extremities [2, 6, 7].
The severity of the disease varies from patient to patient, depending on the time of onset and level of intervention or treatment. The morbidity increases with ageing and is marked by reduced function of affected joints at a young age, reduced muscle strength, reduced range of joint motion (ROM), chronic pains, stunted growth and general fatigue. The diagnosis of KBD is based upon X-ray findings, and clinical criteria in three to four stages have been described [4, 7].
Most common KBD treatment strategies are palliative. Preventive and curative treatments attempted so far have been inconclusive.
Literature concerning conservative rehabilitation strategies in KBD is scarce. Mathieu et al. [8] performed clinical trials over a period of four years, regarding the effect of physiotherapy on improving joint mobility, pain and activity (ankles, knees and elbows) in 135 patients suffering from KBD. Results show that physiotherapy intervention does improve joint mobility.
General research on rehabilitation in KBD patients is primarily focussed on body functions and structures [8–10], whereas activities, pain and participation as well as their associations are seldom highlighted [11].
Our study was designed to add a wider and more comprehensive scope to rehabilitation strategies for KBD in an adult population.
This scope could be important to health professionals developing more evidence-based interventions or treatments. Moreover, it should urge rehabilitation not to focus on joints and muscles only, but also on more patient-relevant outcomes such as activity and pain.
Information on the associations between body function, structure measurements, activity and pain can be helpful when setting up appropriate rehabilitation intervention schemes and patient management programs.
The objective of this study was to assess clinical characteristics in an adult population with KBD. Clinical characteristics were studied in the domains of the International Classification of Functioning Disability and Health (ICF) [12]. Therefore, we studied cross-sectional outcome parameters in the body function and structure domain, as well as in the activity and participation domain. We also studied the associations between the domains, and the influence of body functions/structures and activities on the level of participation.
Patients
Our cross-sectional study was conducted in March 2009 in three mountain villages (Feng Mao, Luo Shan and Jiu Long) in Mao Xian County, Sichuan Province, China. The study protocol (designed by the authors AS, RE and RdV) was approved by the Sichuan Health Bureau, the Peking University Third Hospital, China and the University of Applied Sciences ‘Hogeschool van Amsterdam’, The Netherlands.
The International Classification of Functioning Disability and Health (ICF) [12] was used to reveal the clinical characteristics, outcome and associations in the different domains (body function and structures, activities and participation).
The assessments were performed by a team of five members (AS, JG, MV, S de R and ZB) assisted by eight local health professionals. Before the start of our study a three-day workshop was provided to health professionals regarding physical assessment and proper use of the Participation Scale and WHO DAS II questionnaires and interview techniques. In this way it became possible to communicate with the community in their local dialect. On the last day of the training a pilot research was carried out after which the concept was evaluated and final adjustments were made.
KBD patients and the grade of severity were identified by local health key persons under supervision of the Centre for Disease Control and Prevention (CDC) and the local County Health Bureau. The study was carried out consulting the ethical committee in the Peking University Third Hospital in Beijing, China. Ethical clearance for the study was obtained through informed consent from participants before any activity was conducted.
Methods
Physical assessment was performed in the domain “body function and structures” of the ICF. Anthropometrics, range of joint motion, presence of pain and muscle strength were measured.
Anthropometrics
Standing- and sitting height were measured in a standardised method to the nearest centimetre. Joint deformities/malalignment of upper extremities (crooked fingers, short humerus), spine (scoliosis/kyphosis) or lower extremities (genu varus and valgus or pes planus) were measured.
Range of joint motion
Passive range of joint motion (ROM) was measured to assess the laxity of ligaments, and other collagen tissues' ROM was measured bilaterally to the nearest 2° with a standard two-legged transparent 20-cm arms 360-degrees ISOM (STFR) goniometer and a transparent finger ISO (STFR) goniometer using the ‘anatomical landmark’ method. ROM measurements were performed on the shoulder joint (abduction, elevation), elbow joint (flexion, extension), wrist joint (dorsal extension) and in the metacarpal-phalangeal and inter-phalangeal joint of the second ray (flexion and extension). In the lower extremities the passive ROM of the hip joint (flexion, extension), knee joint (flexion, extension) and ankle joint (dorsal extension) were measured. We summed up all ROM measurements to provide insights in the total range of joint motion [13]. Total ROM provides insights in the stiffness (amount of decrease in ROM) of a person.
Pain
After each task the patient was asked whether performing this task was painful or not. Totalling the number of painful tasks resulted in the pain score during activities.
Muscle strength
Muscle strength was assessed using the criteria of the Medical Research Council (MRC); the rating scale ranges from 0 to 5, where 0 indicates no contraction possible, and 5 is contraction possible against severe resistance [14]. In healthy adults, the muscle strength should be 5. The shoulder abductors, elbow flexors, hip flexors, knee extensors, and ankle dorsal- and plantar flexors were measured. The muscle strength of the hands was assessed (grip strength and three-point grip strength) using a hand-held dynamometer (Citec, Groningen, The Netherlands). Bilaterally, measurements were performed three times consecutively and the mean value was computed [15]. Data were compared with reference values for adults [16, 17]. Physical assessment was performed in the domain “activities” of the ICF. Daily activities in upper and lower extremities were measured, as well as the time-up-and-go test.
Daily activities
A list of ten daily activities linked with daily work in the upper and lower extremities, which were appropriate for the local situation, was composed. The composition was based on literature review and clinical expertise and was specifically designed for this study. Functional tests for the upper extremities were based on sequential occupational dexterity assessment (SODA) [18].
Upper extremities
The patient was seated on a chair at a table where the five different tasks were exhibited. The patient received verbal instructions concerning the task where bilateral and unilateral activities were performed.
Pick up three different-sized Chinese Yuan coins from the table (bilateral task) [18].
Open a PET bottle. One hand holds the bottle while the other hand unlocks it. The overall performance of the total task was scored.
Untighten two buttons of a shirt (unilateral task) [18].
Open the lid of a 500-ml thermos bottle (unilateral task) [18].
Pour water into a cup (unilateral task) [18].
Lift up a brick of 1.5 kg to shoulder level (bilateral task).
Lower extremities
The functional test for the lower extremities was based on those daily activities that include joints which might be influenced by KBD.
Squat to 70 degrees. The patient was asked to stand up with the feet 30 cm apart. From upright standing position the patient starts to squat by bending the knees until there is a 70-degree angle between femur and fibula and then hold this position for two seconds.
Deep squat. The patient was asked to perform a deep squat until the flexion angle between femur and fibula was more than 100 degrees.
Step up (15 cm).
Step down (15 cm).
The performance was scored according to the observation of the assessor (not possible = score 2, with compensation = score 1, possible = score 0).
Timed-up-and-go test (TUG)
The timed-up-and-go test (TUG) was performed in three runs and recorded in seconds [19]. Patients in the study population who normally walked with aids (13.3%) were allowed to use their walking stick during the timed-up-and-go test. All participants wore footwear.
Questionnaires were performed in the domain “participation” of the ICF.
Restrictions in participation were assessed using the participation scale (version 5.2; 18 items), which provided a quantitative measure of an individual’s perceived participation restrictions [20]. The participation scale was used in conjunction with the WHO DAS II (12 items), which provided a quantitative measure of limitations in function in the area of activities of daily living and participation level [21]. Items that were ambiguous were removed from the questionnaire (e.g. current marital status, cohabiting [WHODAS II], and religious affairs [participation scale Q7]).
Statistical analysis
Patient characteristics were analysed using a descriptive method. Anthropometrics were analysed using reference values for non affected Chinese people using one sampled t-test. For categorical data analysis, quantitative variables were tested for a normal distribution and were described as means and standard deviations. Variables that were not normally distributed were described as median and the interquartile range. Qualitative variables were described as percentages.
Differences between left and right (within patients) in joint mobility were analysed using the paired sampled t-test. Pearson’s and Spearman’s correlations were used to illustrate correlations between variables.
The associations between the parameters in the different domains of the ICF were analysed with univariate and multivariate linear regression techniques adjusted for possible confounding factors. To resolve the primary research question, the participation score was defined as dependent variable and range of joint motion and muscle strength, as well as age, gender, presence of pain and TUG were defined as independent variables. Associations were expressed as regression coefficients with a 95% confidence interval (95% CI). P-value < 0.05 β was considered to be significant. Analyses were performed with the software package Statistical Package for Social Science (SPSS Inc., Chicago, IL) version 15.
Results
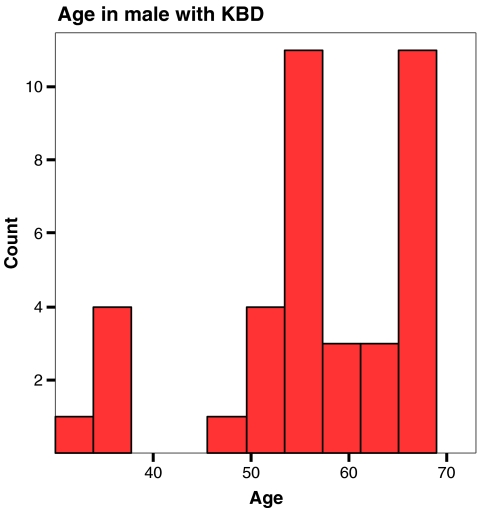
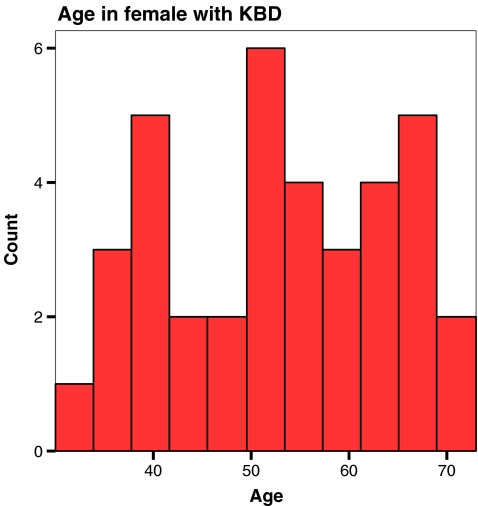
Patient characteristics are presented in Table 1. Seventy-five adults with a mean age of 54.8 (SD 11.3) years participated (50.7% male). Gender related age distribution is presented in Figs. 1 and 2. Eighty-eight percent of the population was married and 67% was employed, while 29% was unable to work for health reasons. Height and sitting height were significantly decreased compared to reference values of unaffected Chinese people [6] (mean height 1.53 versus 1.58 in the reference group; p-value < 0.001) [16, 22].
Table 1.
Patient characteristics
| Characteristic | Value |
|---|---|
| Age (mean, SD) | 54.83 (11.29) |
| Male | 50.7% |
| Female | 49.3% |
| Tribe (%) | |
| Qiang | 97.3 |
| Han | 2.6 |
| Height, cm (mean, SD) | |
| Male | 157 (7) |
| Female | 149 (9) |
| Arm span (mean, SD) | 156.4 (15) |
| Trunk height (mean, SD) | 79.4 (6) |
| Crooked fingers (%) | 79.7 |
| Enlarged finger joints (%) | 88.0 |
| Genu varus (%) | 45.3 |
| Genu valgus (%) | 12.0 |
| Pes planus (%) | 40.0 |
| Marital status (%) | |
| Married | 87.7 |
| Other than married | 12.3 |
| Main work status (%) | |
| Self employed | 67.1 |
| Retired | 1.4 |
| Unemployed due to health reasons | 28.8 |
Fig. 1.
Age distribution in males with Kashin Beck Disease (KBD)
Fig. 2.
Age distribution in female with Kashin Beck Disease (KBD)
Clinical characteristics are presented in Table 2. Axial malalignment was present in the lower extremities (genu varus/valgus) in 57% and in the upper extremities, especially in the finger joints (crooked fingers as well as enlarged finger joints) in 88%.
Table 2.
Clinical characteristics: ROM (degrees), muscle strength and presence of uni- and bilateral pain
| Range of motion (degrees) | Mean (SD) | No pain % | Unilateral pain % | Bilateral pain % |
|---|---|---|---|---|
| Shoulder joint | ||||
| Abduction | 107.3 (23.1) | 10.7 | 6.7 | 82.7 |
| Elbow joint | ||||
| Flexion | 126.6 (23.2) | 10.7 | 9.3 | 80.0 |
| Extension | −23.5 (20.2) | 14.3 | 15.7 | 65.3 |
| Wrist joint | ||||
| Dorsal flexion | 52.8 (20.0) | 9.3 | 12.0 | 78.7 |
| MCP joint | ||||
| Flexion | 61.6 (18.4) | 8.2 | 12.3 | 79.5 |
| Extension | 18.1 (14.8) | 15.3 | 5.6 | 79.2 |
| PIP joint | ||||
| Flexion | 68.7 (20.9) | 18.9 | 13.5 | 67.6 |
| Extension | −0.9 (9.1) | 18.9 | 16.2 | 64.9 |
| DIP joint | ||||
| Flexion | 53.2 (14.1) | 29.2 | 13.9 | 56.9 |
| Extension | −0.5 (10.7) | 23.3 | 17.8 | 58.9 |
| Hip joint | ||||
| Flexion | 76.6 (24.8) | 11.0 | 5.5 | 83.6 |
| Extension | −8.4 (4.6) | 15.6 | 6.2 | 78.1 |
| Knee joint | ||||
| Flexion | 112.1 (27.4) | 8.1 | 9.5 | 82.4 |
| Extension | −11.1 (22.0) | 4.1 | 10.8 | 85.1 |
| Ankle joint | ||||
| Dorsal flexion | 9.6 (8.1) | 12.3 | 9.6 | 78.1 |
| Muscle strength (range 0–5) | Median (P50) (P25–75) | No pain % | Unilateral pain % | Bilateral pain % |
|---|---|---|---|---|
| Shoulder | ||||
| Abduction | 4 (3–5) | 13.3 | 8.0 | 78.7 |
| Elbow | ||||
| Flexion | 4.5 (3–5) | 6.7 | 6.7 | 86.7 |
| Hip | ||||
| Flexion | 4.5 (3–5) | 13.5 | 13.5 | 73.0 |
| Knee | ||||
| Extension | 4.5 (3.5–5) | 1.4 | 6.8 | 91.8 |
| Ankle | ||||
| Dorsal flexion | 4.5 (2.5–5) | 13.5 | 2.7 | 83.8 |
| Plantar flexion | 4.5 (3–5) | 12.2 | 8.1 | 79.7 |
| Muscle strength (hand-held myometry) (N) | Left mean (SD) | Right mean (SD) | ||
|---|---|---|---|---|
| Three point grip | 48.3 (26.) | 46.8 (27.3) | ||
| Fist grip | 75.5 (48.6) | 72.6 (44.6) |
| Muscle strength (range 0–5) | Median (P50) (P25–75) | No pain % | Unilateral pain % | Bilateral pain % |
|---|---|---|---|---|
| Shoulder | ||||
| Abduction | 4 (3–5) | 13.3 | 8.0 | 78.7 |
| Elbow | ||||
| Flexion | 4.5 (3–5) | 6.7 | 6.7 | 86.7 |
| Hip | ||||
| Flexion | 4.5 (3–5) | 13.5 | 13.5 | 73.0 |
| Knee | ||||
| Extension | 4.5 (3.5–5) | 1.4 | 6.8 | 91.8 |
| Ankle | ||||
| Dorsal flexion | 4.5 (2.5–5) | 13.5 | 2.7 | 83.8 |
| Plantar flexion | 4.5 (3–5) | 12.2 | 8.1 | 79.7 |
| Muscle strength (hand-held myometry) (N) | Left mean (SD) | Right mean (SD) | ||
|---|---|---|---|---|
| Three point grip | 48.3 (26.) | 46.8 (27.3) | ||
| Fist grip | 75.5 (48.6) | 72.6 (44.6) |
In the shoulder-, elbow-, hip- and knee joint a severe decrease in ROM was present both in flexion and extension, whereas in the distal joints the decrease in range of joint motion was less marked. Compared to age-related reference values [6], a significant decrease was present in all joint movements except for flexion in the MCP joint (p-value 0.8) and extension in the DIP joint (p-value 0.7). In almost all joints, bilateral pain was present.
A decrease in muscle strength was observed in almost all muscles (median score 4.5; interquartile range 2.5–5), whereas in healthy adults a median score of 5 should be present. Mean three-point grip was 46.8 N (SD 27.3) versus 105.5 N (SD 19.6) in healthy controls (p = 0.006), whereas mean grip strength was significantly reduced in both males and females compared to healthy controls (p = 0.000) [16, 17, 22]. The mean (SD) time of standing up (TUG) was 12.3 s (SD 4.7) in males and 12.8 s (SD 6.8) in females, whereas in healthy individuals of at least 60 years of age the mean (95% CI) TUG time was 9.4 (range 8.9–9.9) [23].
Standing for a long period was possible without any problems or mild problems in 15%, with moderate problems in 17%, while 68% had severe problems or were not able to stand at all. Walking for a long distance for more than 500 metres was possible without any problems to mild problems in 36%, moderate problems in 19%, while 42% had severe problems or were not able at all. Squatting was possible in 37%, possible with assistance in 29% and impossible in 32%, whereas deep squatting was possible in 15%, possible with assistance in 16% and impossible in 68%.
No or mild restriction in participation was found in 35.6% of the study population, whereas 32.9% had moderate restrictions in activity and 31.5% had severe to extreme restriction. Participation on item level is presented in Table 3. Participation scored using the WHO DAS II revealed medium and large problems (>50%) in the items “finding work”, “working as hard”, “contributing to the household”, “making visits outside the village”; whereas in social and cognitive items no severe problems were reported.
Table 3.
Participation scores overall and per individual items
| Restriction | Participation overall | |||
|---|---|---|---|---|
| No significant restriction | 8.2% | |||
| Mild restriction | 27.4% | |||
| Moderate restriction | 32.9% | |||
| Severe restriction | 27.4% | |||
| Extreme restriction | 4.1% | |||
| Participation scale | Equal/ irrelevant (%) | No problem (%) | Small problem (%) | Medium problem (%) | Large problem (%) |
|---|---|---|---|---|---|
| To have equal opportunity as peers to find work | 32.9 | 0.0 | 2.7 | 16.4 | 47.9 |
| To work as hard as peers do | 21.9 | 0.0 | 2.7 | 31.5 | 43.8 |
| To contribute to the household economically in a similar way to your peers | 49.3 | 0.0 | 0.0 | 20.5 | 30.1 |
| To make visits outside the village as much as peers do | 30.1 | 0.0 | 11.0 | 31.5 | 27.4 |
| To take part in major festivals as peers do | 56.2 | 1.4 | 4.1 | 19.2 | 19.2 |
| To take as much part in social activities as peers | 46.6 | 4.1 | 16.4 | 23.3 | 9.6 |
| To be as socially active as peers are | 68.5 | 1.4 | 4.1 | 16.4 | 9.6 |
| To have the same respect in the community as peers | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| To have opportunity to take care of yourself (appearance, health, nutrition) | 72.6 | 0.0 | 2.7 | 11.0 | 13.7 |
| To visit people in the community as often as other people do | 43.1 | 1.4 | 11.1 | 25.0 | 19.4 |
| To move around the village just as other people do | 67.1 | 1.4 | 9.6 | 16.4 | 5.5 |
| To visit public places in the village as often as other people do | 39.7 | 5.5 | 13.7 | 24.7 | 16.4 |
| To do household work at home | 58.9 | 1.4 | 4.1 | 11.0 | 24.7 |
| Opinion count in family discussions | 83.6 | 2.7 | 2.7 | 6.8 | 4.1 |
| Eating utensils are kept in the same drawer as the rest of the household | 91.7 | 0.0 | 1.4 | 1.4 | 5.6 |
| To help other people | 65.8 | 0.0 | 4.1 | 12.3 | 17.8 |
| To be comfortable meeting other people | 49.3 | 11.0 | 9.6 | 23.3 | 6.8 |
| To feel confident to try to learn new things | 67.1 | 0.0 | 1.4 | 9.6 | 21.9 |
| Participation scale | Equal/ irrelevant (%) | No problem (%) | Small problem (%) | Medium problem (%) | Large problem (%) |
|---|---|---|---|---|---|
| To have equal opportunity as peers to find work | 32.9 | 0.0 | 2.7 | 16.4 | 47.9 |
| To work as hard as peers do | 21.9 | 0.0 | 2.7 | 31.5 | 43.8 |
| To contribute to the household economically in a similar way to your peers | 49.3 | 0.0 | 0.0 | 20.5 | 30.1 |
| To make visits outside the village as much as peers do | 30.1 | 0.0 | 11.0 | 31.5 | 27.4 |
| To take part in major festivals as peers do | 56.2 | 1.4 | 4.1 | 19.2 | 19.2 |
| To take as much part in social activities as peers | 46.6 | 4.1 | 16.4 | 23.3 | 9.6 |
| To be as socially active as peers are | 68.5 | 1.4 | 4.1 | 16.4 | 9.6 |
| To have the same respect in the community as peers | 100.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| To have opportunity to take care of yourself (appearance, health, nutrition) | 72.6 | 0.0 | 2.7 | 11.0 | 13.7 |
| To visit people in the community as often as other people do | 43.1 | 1.4 | 11.1 | 25.0 | 19.4 |
| To move around the village just as other people do | 67.1 | 1.4 | 9.6 | 16.4 | 5.5 |
| To visit public places in the village as often as other people do | 39.7 | 5.5 | 13.7 | 24.7 | 16.4 |
| To do household work at home | 58.9 | 1.4 | 4.1 | 11.0 | 24.7 |
| Opinion count in family discussions | 83.6 | 2.7 | 2.7 | 6.8 | 4.1 |
| Eating utensils are kept in the same drawer as the rest of the household | 91.7 | 0.0 | 1.4 | 1.4 | 5.6 |
| To help other people | 65.8 | 0.0 | 4.1 | 12.3 | 17.8 |
| To be comfortable meeting other people | 49.3 | 11.0 | 9.6 | 23.3 | 6.8 |
| To feel confident to try to learn new things | 67.1 | 0.0 | 1.4 | 9.6 | 21.9 |
Correlations between the measurements in the domains “body function and structure” and “activities” of the ICF are presented in Table 4.
Table 4.
Correlations between body functions/structures, activities and participation
| Correlations between body functions /structures and activities | r | r-square | p-value | |
|---|---|---|---|---|
| Squatting | Pain | 0.12 | 0.01 | 0.290 |
| ROM lower extremity | 0.54 | 0.29 | 0.000 | |
| MRC lower extremity | 0.48 | 0.23 | 0.000 | |
| Step up | Pain | 0.03 | 0.00 | 0.809 |
| ROM lower extremity | 0.43 | 0.18 | 0.001 | |
| MRC lower extremity | 0.48 | 0.23 | 0.000 | |
| Step down | Pain | 0.04 | 0.00 | 0.734 |
| ROM lower extremity | 0.23 | 0.05 | 0.074 | |
| MRC lower extremity | 0.45 | 0.20 | 0.000 | |
| Standing for a long time | ROM | 0.23 | 0.05 | 0.072 |
| MRC | 0.16 | 0.03 | 0.201 | |
| Walking distance | ROM | 0.36 | 0.13 | 0.005 |
| MRC | 0.38 | 0.14 | 0.004 | |
| Time-up-and-go test | ROM lower extremity | 0.34 | 0.12 | 0.005 |
| MRC | 0.35 | 0.12 | 0.005 | |
| Opening a bottle | Pain | 0.30 | 0.09 | 0.009 |
| ROM arm and hand | 0.49 | 0.24 | 0.000 | |
| MRC upper extremity | 0.32 | 0.10 | 0.004 | |
| Lifting up a brick | Pain | 0.18 | 0.03 | 0.107 |
| ROM arm and hand | 0.41 | 0.17 | 0.000 | |
| MRC upper extremity | 0.33 | 0.11 | 0.004 | |
| ROM | MRC | 0.47 | 0.22 | 0.000 |
| Correlations between body functions /structures, activities and participation | r | r-square | p-value | |
|---|---|---|---|---|
| Participation scale | Overall health | 0.44 | 0.19 | 0.000 |
| Standing for a long time | 0.28 | 0.09 | 0.014 | |
| Walking long distances | 0.55 | 0.30 | 0.000 | |
| Squatting | 0.40 | 0.02 | 0.000 | |
| Timed-up-and-go | 0.21 | 0.04 | 0.012 | |
| Step up | 0.43 | 0.18 | 0.000 | |
| Step down | 0.30 | 0.09 | 0.009 | |
| Pain | 0.02 | 0.00 | 0.906 | |
| ROM total | 0.46 | 0.21 | 0.000 | |
| MRC total | 0.42 | 0.18 | 0.000 | |
ROM range of joint motion, MRC muscle strength measurements
Total ROM and total muscle strength were moderately correlated (Spearman correlation coefficient 0.47; p <0.001). Activities in the lower extremities were mildly to moderately correlated to range of joint motion and muscle strength, whereas in the upper extremities activities were primarily correlated to range of joint motion.
Correlations between the measurements in the domains “body function and structure”, “activities” as well as “participation” are presented in Table 4.
Overall health, walking long distances, squatting, timed-up-and-go, step up, step down, reduced ROM and reduced muscle strength were mildly to moderately correlated to activity.
The association between the overall participation score and range of joint motion, muscle strength as well as age and gender is presented in Table 5.
Table 5.
Univariate regression analysis between the overall participation score and range of joint motion, muscle strength, age, gender, pain and TUG
| Variable | β | 95%CI |
|---|---|---|
| ROM totala | 0.029 | 0.044–0.014 |
| MRC totala | −1.02 | −1.590 to −0.458 |
| Age | 0.14 | −0.12–4.0 |
| Gender | −0.4 | −6.2–5.4 |
| Pain | 0.16 | −0.44–0.75 |
| TUG | 0.43 | −0.56–0.92 |
ROM total summation of all range of joint motion measurements, MRC total summation of all muscle strength measurements, TUG time-up-and-go
a Significant associations
Univariate regression analysis revealed a significant association between activity and range of joint motion and muscle strength.
Multivariate regression analysis revealed that participation was significantly associated with range of joint motion after correction for confounders including muscle strength, gender and age (regression coefficient 0.021; 95% CI 0.041 to 0.001; p = 0.038).
Activity was borderline significantly associated with range of joint motion after correction for muscle strength, gender, age and the presence of pain (regression coefficient −0.020; 95% CI−0.041 to 0.000; p = 0.054).
Activity was borderline significantly associated with range of joint motion after correction for muscle strength, gender, age and the activity time-up-and-go (regression coefficient −0.020; 95 % CI −0.04 to 0.000; p = 0.051).
Discussion
In KBD adults, a severe decrease in activity is primarily caused by decrease in ROM and malalignment, and not primarily by age, gender, muscle strength nor by pain.
These findings may have strong influence on rehabilitation and surgical intervention. Since these observations are treatable problems, physical assessment and treatment of KBD should focus more on these aspects to improve socio-economical participation.
As shown in previous studies, the main physical characteristics of KBD are reduced range of motion of multiple joints, joint deformities, stunted growth and severe arthritic pains [2, 7, 8]. Literature regarding the associations between these characteristics and socio-economic participation had not been investigated in detail.
Our study has intrinsic limitations. First, the study was executed under rather difficult circumstances. The survey area was still suffering seriously in many ways (security, infrastructure, human resources and aftershocks) after the Sichuan earthquake in May 2008. Also, environmental circumstances such as cold temperatures at high altitude (2300–2700 m) with lack of heated investigation rooms at the time of the study might influence the results. Assessments were often performed while covering patients with clothes to prevent them from getting too cold. Therefore, hand held dynamometry was only performed in the hand and not in all tested muscles.
Second, the design of the study was only possible in a cross-sectional fashion. KBD may occur at young age, and therefore young people ought to be included in the study.
In general, most of the deformities are established at the age of 15 years. So the mechanical overload is generated by the unbalance of the joint, which rapidly aggravates the joint function with increasing pain and limitation of motion due to secondary osteoarthritis. The cross-sectional sampling of our study does not allow observation of this evolution.
As a result of the Chinese migration policy all children and young adults had been moved out of the endemic KBD area, attending boarding schools elsewhere. Thus, the study population was relatively healthy and ambulant. All were able to walk (with difficulty) from their home to the survey station. For safety reasons we were not allowed to conduct home visits to the less ambulant KBD patients in the area.
Third, the validity of the western measurement scales might be skewed due to cultural perception. Certain issues seem quite important from a Euro-centric perspective, but might be irrelevant to people in less developed parts of China.
Cultural behaviour also plays a strong role in the perception of pain behaviour, which is influenced by a complex of interaction of attitudes, beliefs, psychosocial and emotional factors. The survey team was to a limited extent sensitive to such influences in the assessment of KBD patients. In our study, the mean age of 54.8 years is significantly “old” for the studied population; therefore, in the participation domain, the items “finding work” and “working as hard” should be adjusted accordingly.
Fourth, all measurements were performed under supervision of an experienced examiner. A brief training period of three days seemed sufficient for the relatively inexperienced local examiners to reach a level of reliability comparable to that of an experienced professional. This can, however, not be stated with certainty.
In general, decreased ROM in arthritic painful joints is coupled with decreased muscle strength, leading to decrease in functional ability and problems in participation like social and physical (e.g. farming) activities.
Decreased muscle strength of upper and lower extremities was also observed in this study, especially pronounced in the extrinsic and intrinsic muscles of the hand, illustrated by the grip strength and three-point grip strength measurements. This might be caused by the experienced pain (more than 70% of all adults) and the malfunction of the fingers due to contractures and crooked fingers.
Several activities are severely decreased with consequences for functional ability. In Chinese culture, people routinely squat for many activities of daily life: in leisure time (having a meal, a drink, a cup of tea, smoking, chatting), at work (e.g. farming, building, carpentry) and in domestic life there is the squat toilet. In the study group it was impossible for 32% of KBD patients to perform squats, while 68% could not perform a full squat. Ability to perform a full squat, standing for a long time, and walking long distances were significantly limited correlating to joint mobility and/or malalignment of the joints. KBD patients do encounter social and economic problems in many daily activities. This study confirms a moderate correlation of the total range of motion and the total muscle strength in all domains of ICF interfering in daily activity and participation.
The study was not designed to provide a comprehensive overview of problems in all age categories and in all areas of life. Additional in-depth interviews would be needed to make a comprehensive assessment of all problems to be addressed [20]. This study provides valid information for an adult patient population in which joint stiffness was present and without any rehabilitation activities or surgical interventions having been undertaken.
This study provided evidence that joint mobility is not the only parameter to consider in rehabilitation in order to improve functionality and (thus) participation. Adequate muscle strength is another criterion for maintaining stabilisation, endurance and function [7].
KBD appears to have a different aetiology when compared to osteoarthritis but it does have similar pathological outcome. It involves cartilage matrix degradation leading to joint destruction with restricted range of joint motion and reduced muscle strength. KBD often occurs in children with the breakdown of cartilage with severe multiple joint deformities during development [6], while OA is a degenerative joint disorder that predominantly occurs in older people. All study subjects were adults with KBD symptoms that appeared at young (adolescent) age, which confirms that KBD is a chronic disease with cumulative incidence over time [8]. This study suggests that joint mobility and muscle strength are associated with activity. Recommendations for treatment of KBD should concentrate on early detection of reduced range of joint motion and/or malalignment with additional attention to reduced muscle strength and endurance.
Once deformities are present, rehabilitation should focus on restoring functional recovery (maintain mobility and muscle strength) with or without supportive devices (braces, orthoses) [24, 25]. Surgical intervention (osteotomy) offers a good solution for advanced cases with severe joint deformities and malalignment [10, 26]. It is a valuable treatment with beneficial effects on pain and function of the affected joint. It also benefits neighbouring joints such as spine, pelvis and feet resulting in improvement in ability and capacity for self support.
The literature illustrates that after a surgical re-alignment patients have less pain and improved joint function [10]. Operative interventions should not only focus on the impairment and functional level, but should also recognise and affirm the value of inclusion of socio-economical participation.
Conclusion
In KBD adults, a severe decrease in activity is primarily caused by a decrease in range of joint motion and not by age, gender, muscle strength and the presence of pain. These findings have strong influence on rehabilitation and surgical intervention. Since these observations are treatable problems, physical assessment and treatment of KBD should focus more on these aspects to eventually improve socio-economical participation.
Acknowledgements
This study was conducted in collaboration with the Dutch University of Applied Sciences ‘Hogeschool van Amsterdam’, the Chinese educational organisation ‘Peking University Third Hospital’, the Dutch ‘Enraf Nonius’ Company and the Chinese Beijing Health East Technology Development Co. Ltd.
The study has been awarded with an Asia Facility Grant by the Dutch Government under contract agreement with executive authority of the Ministry of Economic Affairs. We thank Mr. Rolf Hoogland for organising the contract agreement.
The successful completion of this study would not have been possible without the highly valued cooperation of the Mao Xian Hospital (Dr Zou, Mr. Yan, Mr Sun), Mao Xian County Health Bureau (Mr. Zuo, Mr. Zhang, Mr. Li) and Mao Xian Center for Disease Control and Prevention (Mr. Zhang, Mr He), for providing excellent logistics and sharing extensive knowledge and information about the population and the study area. We also thank all Chinese health professionals with whom we worked closely together in this survey including Miss Chen, Mrs. Jian, Miss Wang, Mrs. Wu, Miss Li, Mr. He, Mr. Luo and Mr. An. Also, we acknowledge the community members of the three rural villages for being willing to share information, respond to the many questions of the survey and undergo a physical assessment and functional tests. We thank Dr. Chen Yaping and Mrs. Zhang Yan for playing a key role in terms of logistics, planning and operational management before and during the survey.
We are also grateful to the survey team members Mr. Jan Giesen, Mr. Zhao Bingnan Sander de Rapper who contributed in their unique ways towards the successful completion of the survey.
The World Health Organisation in Geneva provided permission for using the WHO DAS II.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
References
- 1.Malaisse F, Mathieu F. Big Bone Disease. A multidisciplinary approach of KBD in Tibet Autonomous Region (P.R. China) Les Presses Agronomiques de Gembloux, ASBL (Belgium) 2008;15:70–78. [Google Scholar]
- 2.Mathieu F, Begaux F, Lan ZY, Suetents C, Hinsenkamp M. Clinical manifestations of Kashin-Beck disease in Nyemo Valley, Tibet. Int Orthop. 1997;21:151–156. doi: 10.1007/s002640050139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cao J, Li S, Shi Z, Yue Y, Sun J, Chen J, Fu Q, Hughes CE, Caterson B. Articular cartilage metabolism in patients with Kashin Beck Disease: an endemic osteoarthropathy in China. Osteoarthr Cartilage. 2008;16:680–688. doi: 10.1016/j.joca.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 4.Pasteels JL, Liu FD, Hinsenkamp M, Rooze M, Mathieu F, Perlimutter N. Histology of Kashin-Beck lesions. Int Orthop. 2001;25:151–153. doi: 10.1007/s002640000190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Suetens C, Moreno-Reyes R, Chasseur C, Mathieu F, Begaux F, Haubruge E, Durand MC, Neve J, Vanderpas J. Epidemiological support for a multifactorial aetiology of Kashin-Beck disease in Tibet. Int Orthop. 2001;25:180–187. doi: 10.1007/s002640100247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mathieu F, Begaux F, Suetens C, De Maertelaer V, Hinsenkamp M. Anthrometry and clinical features of Kashin Beck disease in Central Tibet. Int Orthop. 2001;25:138–141. doi: 10.1007/s002640000192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Xiong G. Diagnostic, clinical and radiological characteristics of Kashin Beck disease in Shaanxi Province, PR China. Int Orthop. 2001;25:147–150. doi: 10.1007/s002640100248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mathieu F, Suetens C, Begaux F, de Maertelaer V, Hinsenkamp M. Effects of physical therapy on patients with Kashin-Beck disease in Tibet. Int Orthop. 2001;25:191–193. doi: 10.1007/s002640000206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hinsenkamp M, Ryppens F, Begaux F, Mathieu F, de Maertelaer V, Lepeire M, Haubruge E, Chasseur C, Stallenberg B. The anatomical distribution of radiological abnormalities in Kashin Beck disease in Tibet. Int Orthop. 2001;25(3):142–147. doi: 10.1007/s002640100236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Liu FD, Wang ZL, Hinsenkamp M. Osteotomy at the knee for advanced cases of Kashin-Beck disease. Int Orthop. 1998;22:87–91. doi: 10.1007/s002640050215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hinsenkamp M, Mathieu F, Claus W, Collard JF, de Maertelaer V. Effects of physical environment on the evolution of Kashin Beck disease in Tibet. Int Orthop. 2009;33:1085–1088. doi: 10.1007/s00264-009-0738-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.WHO (1980) International classification of functioning, disability and health. World Health Organisation, Geneva
- 13.Hogeweg JA, Langereis MJ, Bernards ATM, Faber JAJ, Helders PJM. Goniometry—variability in the clinical practice of a conventional goniometer in healthy subjects. Eur J Phys Med Rehabil. 1994;4:2–7. [Google Scholar]
- 14.Medical Research Council . Aids to the investigation of peripheral nerve injuries. War memorandum. 2. London: HMSO; 1943. [Google Scholar]
- 15.Beenakker EAC, van der Hoeven JH, Fock JM, Maurits NM. Reference values of maximum isometric muscle force obtained in 270 children aged 4–16 years by hand-held dynamometry. Neuromusc Dis. 2001;11(5):441–446. doi: 10.1016/S0960-8966(01)00193-6. [DOI] [PubMed] [Google Scholar]
- 16.Mathiowetz V, Kashman N, Volland G, Weber K, Dowe M, Rogers S. Grip and pinch strength: normative data for adults. Arch Phys Med Rehabil. 1985;66:69–72. [PubMed] [Google Scholar]
- 17.Windt A, Takken T, Helders PJM, Engelbert RHH. Is grip strength a predictor for total muscle strength in healthy children, adolescents and young adults? Eur J Ped. 2010;169(3):281–287. doi: 10.1007/s00431-009-1010-4. [DOI] [PubMed] [Google Scholar]
- 18.van Lankveld W, Van’t Pad Bosch P, Bakker J, Terwindt S, Franssen M, van Riel P. Sequential occupational dexterity (SODA): a new test to measure hand disability. J Hand Ther USA. 1996;9(1):27–32. [PubMed] [Google Scholar]
- 19.Steffen TM, Hacker TA, Mollinger L. Age- and gender-related test performance in community-dwelling elderly people: six-minute walk test, berg balance scale, timed up & go test, and gait speeds. Phys Ther. 2002;82(2):128–137. doi: 10.1093/ptj/82.2.128. [DOI] [PubMed] [Google Scholar]
- 20.van Brakel WH, Anderson AM, Mutatkar RK, Bakirtzief Z, Nicholls PG, Raju MS, Das-pattanayak RK. The participation scale: measuring a key concept in public health . Dis Rehabil. 2006;28(4):193–203. doi: 10.1080/09638280500192785. [DOI] [PubMed] [Google Scholar]
- 21.WHO (2000) WHO DASII, disability assessment schedule, training manual WHO classification, assessment and survey team. World Health Organisation, Geneva, pp 1–12
- 22.van der Ploeg RJO, Fidler V, Oosterhuis HJGH. Hand held myometry: reference values. J Neurol Neurosurg Psych. 1991;54:244–247. doi: 10.1136/jnnp.54.3.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bohannon RW. Reference values for the timed up and go test: a descriptive meta-analysis. J Ger Phys Ther. 2006;29(2):64–68. doi: 10.1519/00139143-200608000-00004. [DOI] [PubMed] [Google Scholar]
- 24.Brouwer RW, van Raaij TM, Jakma TT, Verhagen AP, Verhaar JAN, Bierma-Zeinstra SMA (2005) Braces and orthoses for treating osteoarthritis of the knee. Cochrane Database Syst Rev (1):CD004020 [DOI] [PubMed]
- 25.Hernández-Molina G, Reichenbach S, Zhang B, Lavalley M, Felson DT. Effect of therapeutic exercise for hip osteoarthritis pain: results of a meta-analysis. Arthritis Rheum. 2008;59:1221–1228. doi: 10.1002/art.24010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brouwer RW, Raaij van TM, Bierma-Zeinstra SMA, Verhagen AP, Jakma TT, Verhaar JAN (2009) Osteotomy for treating knee osteoarthrosis. Cochrane Database Syst Rev (3):CD0040199 [DOI] [PubMed]