Abstract
Patellofemoral disorders are common conditions seen in a knee clinic but can present a great diagnostic challenge to the orthopaedic surgeon. Combined single photon emission computerised tomography with conventional computer tomography (SPECT/CT) provides the clinician with precise anatomical and physiological information of the patellofemoral joint. We present a clinical review that highlights the value of SPECT/CT in patients with patellofemoral disorders, where other modalities such as radiographs, MRI, and conventional CT did not provide sufficient information. SPECT/CT has proven to be helpful for establishing the diagnosis and guidance for further treatment. SPECT/CT should be recognised as a valuable diagnostic tool in orthopaedic patients.
Introduction
Patellofemoral disorders are common clinical conditions encountered in the knee clinic and can present a great diagnostic challenge to the orthopedic surgeon [1–8]. Despite a detailed history and thorough clinical examination, in many patients with patellofemoral disorders it is difficult to precisely locate the origin of the pain, analyse the pathomorphology and subsequently establish the correct diagnosis [9]. It is even more difficult when the knee has previously been operated on. Radiological imaging such as radiographs, computerised tomography (CT), magnetic resonance imaging (MRI) and single photon emission computerised tomography (SPECT) are readily available investigations in most orthopaedic units and form part of the standard diagnostic armamentarium [7, 10–13].
The major disadvantage of conventional radiographs in diagnosing patellofemoral disorders is the poor correlation between radiographic abnormalities and patellofemoral pain [11, 12]. Due to non-standardised leg position and alignment at the time of radiographic imaging, measurements of the patellar height, position and tilt, as well as the shape of the trochlear groove are variable and only gross patellofemoral abnormalities can be detected and/or measured. Furthermore, the sensitivity and specificity of plain radiographs to detect grade 1 and 2 chondral abnormalities is low [13].
CT provides a more precise and comprehensive anatomical and mechanical view of the patellofemoral joint (PFJ), but its informative value is limited to osseous structures [12].
MRI allows detection of osteochondral lesions, osteoarthritic (OA) changes, tears of the menisci or synovial abnormalities. In the PFJ, however, the correlation between patients‘ symptoms and abnormal findings is low and the sensitivity to detect chondral lesions varies widely [10, 12].
Planar SPECT reflects serum markers of bone and cartilage metabolism such as cartilage oligomeric matrix protein (COMP), and bone sialoprotein (BSP) [7, 10, 14, 15]. As subchondral bone changes precede joint space narrowing, SPECT is able to detect disease earlier than radiographs in OA. In the knee, it can detect tibio-femoral osteoarthritis with extremely high sensitivity. In the PFJ, SPECT images are often ill defined and lack precise anatomical detail to provide useful information for further guidance of surgical management [10, 16].
Such limitations have been improved dramatically with the advent of hybrid SPECT/CT systems that can offer clear anatomical detail through high resolution CT imaging with bone physiological activity detected by SPECT study. It is also able to detect chondral and ligamentous damage with high sensitivity and specificity. There is currently no literature supporting the use of SPECT/CT in patients presenting with patellofemoral disorders. In the review presented below, we illustrate the scanning protocol available to perform SPECT/CT and four clinical scenarios that have helped determine an accurate diagnosis and plan further management in such cases.
All SPECT/CTs in our unit are performed using a hybrid system, Symbia T16, (Siemens, Erlangen, Germany) equipped with a pair of low energy, high-resolution collimators and a dual-head gamma camera with an integrated, 16 × 0.75 mm slice-thickness CT. Two hours after injection of 700 MBq Technetium-99m HPD (CIS Bio International Sur Yvette, France) a SPECT is performed with a frame matrix size of 128 × 128 with an angle step of 32°, and a time per frame of 25 seconds. Reconstructed data is displayed in transaxial, coronal and sagittal planes. Using this scanning protocol, this technology has assisted our diagnosis and management in the following situations.
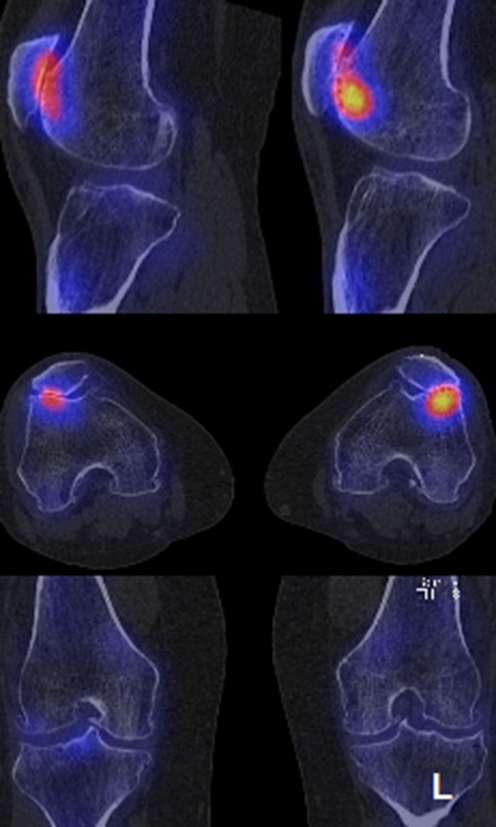
A 45-year-old male complained of left anterior knee pain, associated with instability and made worse by running. He was known to have bilateral bipartite patella, and a past history of minor injury to his left knee (seven and 23 years ago). Clinical examination was unremarkable with no tenderness in the knee and a full range of movement. Anteroposterior (AP), lateral and skyline radiographs revealed bilateral bipartite patella. There was no sign of degeneration of the retropatellar surface or femoro-tibial compartment. The skyline view of the patella demonstrated the main body of the patella to be satisfactorily seated in the trochlea, with an accessory lateral pole overhanging the lateral femoral condyle. The SPECT/CT revealed a degenerate pseudoarthrosis between the patella and its lateral pole with increased signal intensity (Fig. 1). The patient was treated by resection of the lateral pole of the bipartite patella with debridement of the medial facet. He made an uneventful recovery with full resolution of symptoms.
Fig. 1.
Combined single photon emission computerised tomography with conventional computer tomography (SPECT/CT) images (coronal, lateral and axial) of the left knee of a 45-year-old male patient showing an increased signal activity to the pseudoarthrosis between the main body of the patella and lateral pole
A 60-year-old female patient presented with bilateral knee pain, more severe on the left. There was no history of trauma. The knee was noted to swell and be most painful on walking and climbing stairs. Clinically, the left knee had a mild effusion and peripatellar tenderness. The AP and lateral weight-bearing radiographs showed isolated lateral patellofemoral OA of both knees, with largely preserved femoro-tibial joints. The radiographic changes appeared symmetrical. The SPECT/CT demonstrated activity to both patellofemoral joints. Images corresponded with the patient’s symptoms with signal intensity greatest from the lateral femoral condyle and PFJ (Fig. 2). The patient underwent PFJ arthroplasty with a resulting abatement in symptoms.
Fig. 2.
Combined single photon emission computerised tomography with conventional computer tomography (SPECT/CT) images of both knees of a 60-year-old female patient showing a localised area of increased tracer uptake to the lateral femoral condyle and patellofemoral joint (PFJ). The intensity is greatest on the left knee, corresponding with the patient’s symptoms
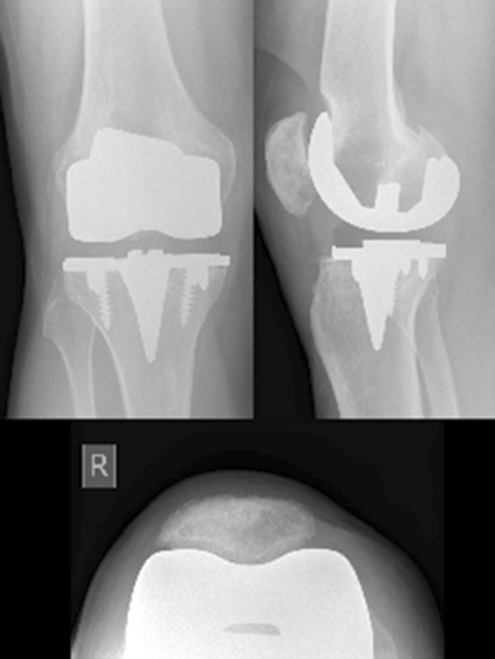
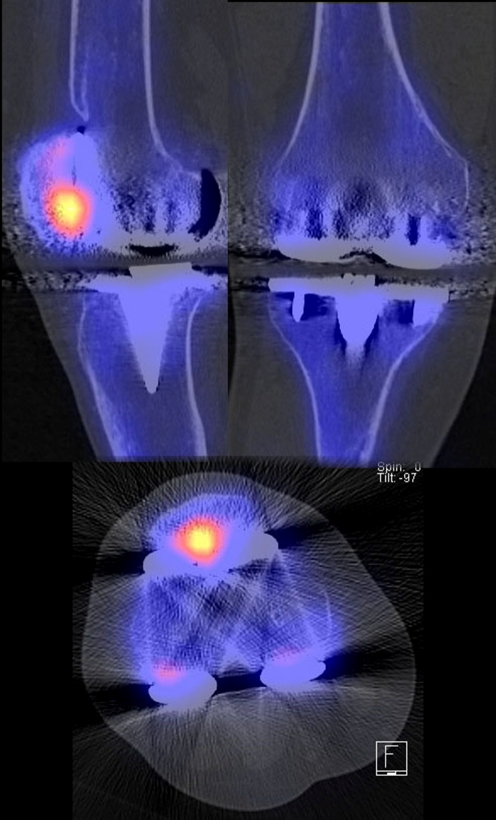
A 50-year-old male patient had undergone a patella sparing primary total knee arthroplasty (Natural Knee®, Zimmer Ltd., Münsingen, Switzerland) for post-traumatic bicompartmental osteoarthritis. Two and a half years after surgery the patient presented with activity-related anterior right knee pain. Clinical examination and blood tests, including infection screening, were normal. Radiographs showed an unchanged position of the total knee prosthesis but with some notching of the femur (Fig. 3). The patella was well seated in the trochlea with neither tilting or subluxation, nor degenerative changes. There appeared to be minor osteolysis underneath the tibial base plate. With the suspicion of tibial component loosening, a SPECT/CT was performed. To the surprise of the clinicians the PFJ was shown to be the source of the patient’s symptoms. There was no evidence of prosthesis loosening or infection (Fig. 4). Following patella resurfacing, the patient made a full recovery.
Fig. 3.
Anteroposterior, lateral and skyline radiographs of the right knee of a 50-year-old male patient taken 2.5 years after primary total knee arthroplasty
Fig. 4.
Combined single photon emission computerised tomography with conventional computer tomography (SPECT/CT) images of the right knee of a 50-year-old male patient showing a focal increased activity at the retro patellar surface with otherwise unsuspicious knee after total knee arthroplasty
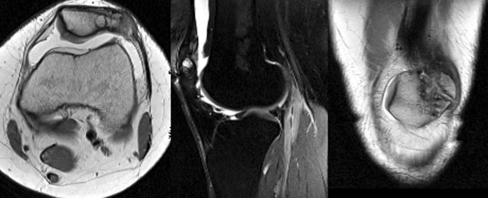
A 35-year-old female patient presented with acute left anterior knee pain and swelling, worse after episodes of running. Examination revealed palpable patellofemoral crepitus, with lateral parapatellar and joint line tenderness. Twenty years earlier, she had undergone microfracture of the retropatellar surface for osteochondritis dissecans. She had made a successful recovery and was able to perform to a high level of activity. Radiographs demonstrated disruption of the lateral patella facet with a possible osteochondral defect, which we postulated was a chronic injury from the time of previous microfracture and underlying osteochondritis dissecans. MRI confirmed damage to the lateral patella facet, a grade 3–4 PFJ chondromalacia with a lateral meniscal lesion (Fig. 5). The SPECT/CT study displayed increased signal activity in the lateral patella facet (Fig. 6). The patient underwent arthroscopic debridement and partial resection of her lateral patella. She made a full recovery from her symptoms and was able to return to running.
Fig. 5.
MRI of left knee joint of a 35-year-old female patient
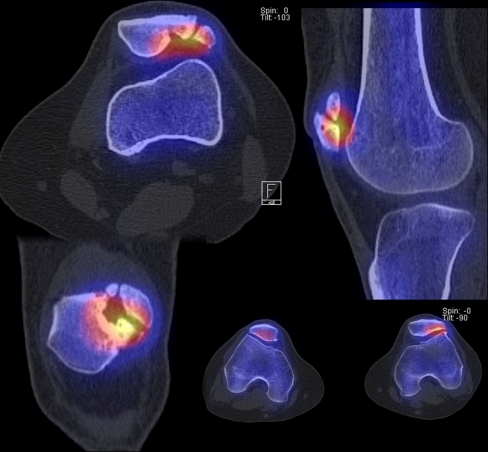
Fig. 6.
Combined single photon emission computerised tomography with conventional computer tomography (SPECT/CT) images of the left knee of a 35-year-old female patient showing the former osteochondritis dissecans lesion 20 years after microfracturing. The increased tracer activity in combination with the osteoarthritic changes clearly indicated the patellofemoral osteoarthritis as cause of the anterior knee pain
Discussion
Hybrid SPECT/CT systems have been available for clinical use for over a decade [17–22], but appear not to have entered the common orthopaedic consciousness as a helpful investigative tool. The major advantage of this modality remains the high diagnostic yield available from combining the detection of abnormal bone metabolism with SPECT, with the precise anatomical detail available in high resolution CT [21, 23]. There is a paucity of literature regarding the use of SPECT/CT in knee disorders and the patellofemoral joint in particular. With the presented scenarios, we endeavor to illustrate the clinical value we have found using this tool to make a firm diagnosis in patients with patellofemoral disorders, where standard imaging techniques such as radiographs or MRI have failed to give a conclusive answer for the patient’s symptoms.
In the first scenario, the patient with bipartite patellae, SPECT/CT imaging was clearly able to discriminate between pain arising from the retropatellar surface or the bipartite patella. Management was targeted towards the lateral pole of the patella, demonstrated specifically by the increased activity of the SPECT/CT.
In our second scenario, the patient presented with a symmetrical pattern of PFJ osteoarthritis. The increased tracer activity to the left knee corresponded with the patient’s symptomology. We suggest that SPECT/CT may play a role in investigating the progression of disease in particular morphological patterns of osteoarthritis in the PFJ. This finding, if proved by larger-scaled studies, could guide orthopaedic surgeons to a more specific treatment for osteoarthritis.
The third scenario presented a patient with anterior knee pain after knee arthroplasty, a presentation sometimes seen following surgery. Often the exact cause of the pain is difficult to establish as being related solely to the PFJ. In our case, the patella appeared to be well seated in the trochlea with no obvious clinical or (standard) radiological evidence of maltracking or degenerative disease. In this cohort of patients, the decision to proceed to patella resurfacing is difficult without clear clinical evidence. SPECT/CT not only excluded infection and loosening of the femoro-tibial components, but clearly identified the PFJ as the source of the patient’s symptoms. The anatomical location of greatest metabolic activity is demonstrated on SPECT/CT, whereas on plain CT, metal artifacts alter the image quality and render the investigation as redundant.
The fourth scenario of a patient 20 years after micro-fracture of the PFJ emphasises the clinical value of SPECT/CT in the follow-up of patients after surgical treatment for patellofemoral problems. Although MRI revealed a lateral meniscal lesion and cystic degenerate change to the patella, SPECT/CT specifically demonstrated the latter to be the main cause of symptoms. The increased tracer activity was seen only on the PFJ and not the lateral tibial plateau.
This small series highlights the potential that SPECT/CT provides in establishing a firm diagnosis in often ambiguous clinical situations. The conclusions we can draw are limited by the small sample. Indeed the value in patellofemoral pain needs to be addressed with further research and large-scaled studies. We advocate the use of SPECT/CT in establishing the diagnosis and guidance of further treatment in cases with patellofemoral problems and encourage fellow orthopaedic surgeons to consider employing this valuable diagnostic tool.
Acknowledgments
Conflict of interest The authors declare that they have no conflicts of interest.
References
- 1.Fulkerson JP (1983) The etiology of patellofemoral pain in young, active patients: a prospective study. Clin Orthop Relat Res:129–133 [PubMed]
- 2.Fulkerson JP. Patellofemoral pain disorders: evaluation and management. J Am Acad Orthop Surg. 1994;2:124–132. doi: 10.5435/00124635-199403000-00006. [DOI] [PubMed] [Google Scholar]
- 3.Fulkerson JP. Diagnosis and treatment of patients with patellofemoral pain. Am J Sports Med. 2002;30:447–456. doi: 10.1177/03635465020300032501. [DOI] [PubMed] [Google Scholar]
- 4.Gerbino PG, 2nd, Griffin ED, D’Hemecourt PA, Kim T, Kocher MS, Zurakowski D, et al. Patellofemoral pain syndrome: evaluation of location and intensity of pain. Clin J Pain. 2006;22:154–159. doi: 10.1097/01.ajp.0000159583.31912.1d. [DOI] [PubMed] [Google Scholar]
- 5.LaBella C. Patellofemoral pain syndrome: evaluation and treatment. Prim Care. 2004;31:977–1003. doi: 10.1016/j.pop.2004.07.006. [DOI] [PubMed] [Google Scholar]
- 6.Lowry CD, Cleland JA, Dyke K. Management of patients with patellofemoral pain syndrome using a multimodal approach: a case series. J Orthop Sports Phys Ther. 2008;38:691–702. doi: 10.2519/jospt.2008.2690. [DOI] [PubMed] [Google Scholar]
- 7.Naslund JE, Odenbring S, Naslund UB, Lundeberg T. Diffusely increased bone scintigraphic uptake in patellofemoral pain syndrome. Br J Sports Med. 2005;39:162–165. doi: 10.1136/bjsm.2004.012336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brushoj C, Holmich P, Nielsen MB, Albrecht-Beste E. Acute patellofemoral pain: aggravating activities, clinical examination, MRI and ultrasound findings. Br J Sports Med. 2008;42:64–67. doi: 10.1136/bjsm.2006.034215. [DOI] [PubMed] [Google Scholar]
- 9.Pagenstert GI, Bachmann M. Clinical examination for patellofemoral problems. Orthopade. 2008;37(9):890–895. doi: 10.1007/s00132-008-1296-3. [DOI] [PubMed] [Google Scholar]
- 10.Lorberboym M, Ami DB, Zin D, Nikolov G, Adar E. Incremental diagnostic value of 99mTc methylene diphosphonate bone SPECT in patients with patellofemoral pain disorders. Nucl Med Commun. 2009;24(4):403–410. doi: 10.1097/00006231-200304000-00010. [DOI] [PubMed] [Google Scholar]
- 11.Kijowski R, Blankenbaker D, Stanton P, Fine J, Smet A. Correlation between radiographic findings of osteoarthritis and arthroscopic findings of articular cartilage degeneration within the patellofemoral joint. Skeletal Radiol. 2006;35(12):895–902. doi: 10.1007/s00256-006-0111-7. [DOI] [PubMed] [Google Scholar]
- 12.Elias DA, White LM. Imaging of patellofemoral disorders. Clin Radiol. 2004;59(7):543–557. doi: 10.1016/j.crad.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 13.Carson WG, Jr, James SL, Larson RL, Singer KM, Winternitz WW. Patellofemoral disorders: physical and radiographic evaluation. Part II: radiographic examination. Clin Orthop Relat Res. 1984;185:178–186. [PubMed] [Google Scholar]
- 14.Hejgaard N, Diemer H. Bone scan in the patellofemoral pain syndrome. Int Orthop. 1987;11(1):29–33. doi: 10.1007/BF00266055. [DOI] [PubMed] [Google Scholar]
- 15.Dye S, Chew MH. The use of scintigraphy to detect increased osseous metabolic activity about the knee. J Bone Joint Surg. 1993;75:1388–1406. [Google Scholar]
- 16.Collier BD, Johnson RP, Carrera GF, Isitman AT, Veluvolu P, Knobel J, et al. Chronic knee pain assessed by SPECT: comparison with other modalities. Radiology. 1985;157(3):795–802. doi: 10.1148/radiology.157.3.3877315. [DOI] [PubMed] [Google Scholar]
- 17.Even-Sapir E, Keidar Z, Bar-Shalom R. Hybrid imaging (SPECT/CT and PET/CT) improving the diagnostic accuracy of functional/metabolic and anatomic imaging. Semin Nucl Med. 2009;39(4):264–275. doi: 10.1053/j.semnuclmed.2009.03.004. [DOI] [PubMed] [Google Scholar]
- 18.Breunung N, Barwick T, Fernando R, Gnanasegaran G, Vijayanathan S, Hosahalli M, et al. Additional benefit of SPECT-CT in investigating heel pain. Clin Nucl Med. 2008;33(10):705–706. doi: 10.1097/RLU.0b013e318184b987. [DOI] [PubMed] [Google Scholar]
- 19.Roarke MC, Nguyen BD, Pockaj BA. Applications of SPECT/CT in nuclear radiology. AJR Am J Roentgenol. 2008;191(3):W135–W150. doi: 10.2214/AJR.07.3564. [DOI] [PubMed] [Google Scholar]
- 20.Hirschmann MT, Iranpour F, Davda K, Rasch H, Hugli R, Friederich NF (2010) Combined single-photon emission computerized tomography and conventional computerized tomography (SPECT/CT): clinical value for the knee surgeons? Knee Surg Sports Traumatol Arthrosc 18(3):341–345 [DOI] [PubMed]
- 21.Scharf S. SPECT/CT imaging in general orthopedic practice. Semin Nucl Med. 2009;39(5):293–307. doi: 10.1053/j.semnuclmed.2009.06.002. [DOI] [PubMed] [Google Scholar]
- 22.Knupp M, Pagenstert GI, Barg A, Bolliger L, Easley ME, Hintermann B. SPECT-CT compared with conventional imaging modalities for the assessment of the varus and valgus malaligned hindfoot. J Orthop Res. 2009;(27)11:1461–1466. doi: 10.1002/jor.20922. [DOI] [PubMed] [Google Scholar]
- 23.Hirschmann MT, Iranpour F, Konala P, Kerner A, Rasch H, Cobb JP, Friederich NF (2010) A novel standardized method for evaluating patients after total knee arthroplasty using combined single photon emission tomography and conventional computerized tomography (SPECT/CT). Knee Surg Sports Traumatol Arthrosc (accepted January 2010) [DOI] [PubMed]