Abstract
Korean women with a history of gestational diabetes mellitus (GDM) have a 3.5 times greater risk of developing postpartum diabetes than the general population. The incidence of type 2 diabetes mellitus in early postpartum is reported as 10-15% in Korean women. A prospective follow-up study on Korean women with GDM showed that approximately 40% of women with previous GDM were expected to develop diabetes within 5 years postpartum. Independent risk factors for the development of diabetes in Korean women with previous GDM are pre-pregnancy body weight, gestational age at diagnosis, antepartum hyperglycemia on oral glucose tolerance test, low insulin response to oral glucose load, and family history of diabetes. Women with postpartum diabetes have greater body mass indexes, body weight, and waist circumferences than women with normal glucose tolerance. Multiple logistic regression analysis has revealed that waist circumference is the strongest obesity index along with systolic blood pressure and that triglyceride levels are a major independent risk factor for developing diabetes. These results in Korean women with previous GDM underline the importance of postpartum testing in Korean women diagnosed with GDM, and demonstrate that impaired B-cell function, obesity, and especially visceral obesity, are associated with the development of diabetes.
Keywords: Diabetes, gestational; Incidence; Postpartum diabetes; Risk factors
INTRODUCTION
Gestational diabetes mellitus (GDM) is defined as glucose intolerance of variable severity with onset or first recognition during pregnancy [1]. The prevalence of GDM is reported as ~14% of all pregnancies in the US [2], and has been increasing in multiethnic populations [3]. In Korea, 2% to 5% of all pregnant women reportedly develop GDM [4]. The clinical implications of GDM are primarily associated with adverse outcomes in pregnancy, such as preeclampsia, Cesarean delivery, macrosomia, and birth trauma [5]. In addition, women with GDM are at an increased risk for type 2 diabetes mellitus (T2DM) later in life [6].
Women with GDM during pregnancy have a greater risk for development of T2DM postpartum. An original study by O'Sullivan and Mahan [7] that produced criteria for the diagnosis of GDM, aimed to determine the level of glycemia during pregnancy that could identify subjects at risk for T2DM in the future. Although most women with GDM exhibit normal glucose tolerance (NGT) when tested several weeks postpartum, impaired B-cell function and/or increased insulin resistance has been reported in these women [8,9], and a substantial proportion of women with previous GDM will eventually develop T2DM [2,10,11].
In this article, I will discuss the prevalence and risk factors of postpartum glucose intolerance in women with GDM, especially in Korean women and summarize recent findings on prevention of T2DM in women with previous GDM.
INCIDENCE OF T2DM IN WOMEN WITH PREVIOUS GDM
Several studies from North America have reported postpartum T2DM rates ranging from 3% to 38% within 1 year after delivery, depending on ethnicity and the proportion of participants with severe hyperglycemia during pregnancy [12-15]. Within 1 year of delivery, a high incidence of diabetes (38%) in women with GDM has been reported in a mixed ethnic population [12]. Using National Diabetes Data Group (NDDG) criteria, Kjos et al. [13] found that 9% of predominantly Hispanic women with GDM developed T2DM in early postpartum. Catalano et al. [14] reported that 3% of subjects in a study population of predominantly white women developed diabetes postpartum. Furthermore, Dacus et al. [15] reported a 10% rate of developing diabetes in a population of predominantly black women with GDM, using the same diagnostic criteria.
A study of mixed ethnic populations in Chicago showed that the cumulative incidence of T2DM in women with previous GDM increased rapidly in the first 2 years after delivery, and approximately 50% of women with GDM progressed to T2DM within 5 years postpartum [10]. A systemic review on the development of diabetes in previous GDM cases by Kim et al. [2] demonstrated that the cumulative incidence of T2DM increased rapidly in the first 5 years after delivery and appeared to plateau after 10 years. The conversion rate to diabetes in women with previous GDM among ethnic groups becomes similar after adjusting for length of follow-up and proportion of participants in follow-up testing.
There have been limited studies on postpartum glucose intolerance in Asian women with previous GDM. Kim et al. [16] in South Korea evaluated 211 women with GDM at 6 weeks postpartum and found that 9.5% had developed T2DM and 9% had impaired glucose tolerance (IGT). Another study from South Korea showed that incidences of T2DM and IGT were 15.1% and 23.2%, respectively, in 311 women with GDM at 2 months postpartum [11]. A study of 120 Chinese women with GDM diagnosed using World Health Organization (WHO) criteria showed that 13.3% of women had IGT (8.3%) or T2DM (5%) at 1 year following delivery [17]. Another study of 800 Chinese women in Hong Kong demonstrated that the incidences of diabetes and IGT were 13% and 22%, respectively, at 6 weeks postpartum [18].
The incidence of postpartum diabetes in Korean women with GDM is somewhat lower than described by Metzger et al. [12], but the proportion of GDM class A2 and B1 in this population is greater than in other Korean studies. In addition, the proportion of GDM class A2 and B1 in a study by Kim et al. [16] was 20%; lower than any other Korean study [11]. Thus, the difference in incidence of diabetes among ethnic groups at early postpartum may be affected by the proportion of participants with severe hyperglycemia during pregnancy.
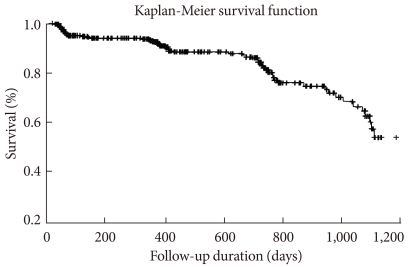
Cho et al. [19] performed a multi-center prospective study in South Korea to evaluate the incidence of diabetes in women with previous GDM. During the first 6 years after delivery (mean duration of follow-up, 2.1±1.8 years), 12.8% and 13.2% of 909 women with previous GDM who had not been diagnosed with T2DM at 6-8 weeks postpartum, developed either T2DM or IGT, respectively. Cumulative incidence of T2DM in these women is shown in Fig. 1. Cho et al. demonstrated that, when the data were analyzed using a 5-year postpartum survival analysis, the incidence rate of T2DM was approximately 41% in Korean women with previous GDM. A long-term follow-up study (median duration of follow-up, 8 years) of Chinese women with previous GDM in Hong Kong showed that 12% of 67 women had T2DM [20]. Differences in the incidence of postpartum diabetes between Korean and Chinese women might be attributable to differences in diagnostic methods and criteria for GDM. Another study of South Indian women reported that 37% of 35 women with previous GDM had T2DM 5 years after delivery [21].
Fig. 1.
Cumulative incidence of type 2 diabetes mellitus in 909 Korean women with previous gestational diabetes mellitus.
The Diabetes Prevention Program (DPP) demonstrated that women with a history of GDM had a 71% increased risk of developing T2DM, as compared with women without such a history [22]. In comparing the risk for developing diabetes in Korean women with previous GDM with the general population, or with women with NGT during pregnancy, Lee et al. [23] reported that Korean women with previous GDM had a 3.5 times greater risk for T2DM, and history of GDM was a greater risk factor than family history of diabetes or waist circumference. In other Asian studies, it was reported that the odds ratio (OR) for development of T2DM is 3.8 in Hong Kong [20] and 35.5 in South India [21]. A recent study from Australia showed that women with previous GDM had a 9.6 times greater risk for developing diabetes, and Asian women had a 2.1 times higher risk, as compared with Caucasian women [24]. Another recent study from the UK also demonstrated that South Asian women had a higher risk of developing diabetes, as compared with Caucasian women (48.6% vs. 25.0%), within a mean period of 4.38 years after delivery [25].
RISK FACTORS FOR T2DM IN WOMEN WITH GDM
Several investigators have performed multivariate analysis to identify independent factors associated with developing T2DM. Factors associated with developing diabetes included the degree of hyperglycemia (fasting glucose measured by oral glucose tolerance test [OGTT], area under the curve [AUC] using OGTT) during pregnancy, gestational age at diagnosis of GDM, insulin treatment during pregnancy, maternal age, and prepregnancy body mass index (BMI) [2]. A recent systemic review of a study that aimed to predict T2DM in women with previous GDM, demonstrated that fasting glucose levels measured with an antepartum diagnostic OGTT was the most significant predictor of T2DM (OR range, 11.1 to 21.0). Two-hour glucose levels (OR range, 1.02 to 1.03) and AUC on OGTT (OR range, 3.64 to 15) were also significant predictors [26].
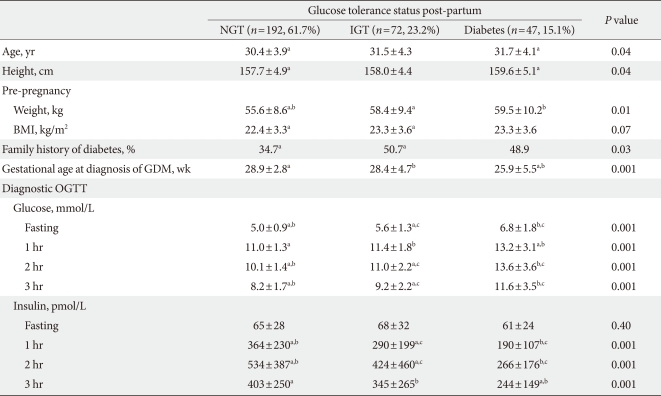
A study of Korean women with previous GDM found that age, height, and pre-pregnancy weight in women with postpartum diabetes were greater than in women with NGT (Table 1). Gestational age at diagnosis of GDM was lower in women with postpartum diabetes, as compared with women with NGT. Plasma glucose levels measured by a diagnostic OGTT were highest in women with postpartum diabetes and lowest in women with NGT. However, 1-, 2-, and 3-hour insulin levels showed a reverse trend. Women with postpartum NGT had the highest insulin levels. When multiple logistic regression analysis was applied to find independent risk factors for postpartum diabetes, pre-pregnancy weight, gestational age at diagnosis, 2-hour glucose levels, and 3-hour insulin concentrations using a diagnostic OGTT were independent predictors for developing T2DM [11]. Kim et al. [16] also demonstrated that the AUC on an antepartum OGTT, family history of diabetes, and gestational age at GDM diagnosis were independent predictors of both postpartum diabetes and postpartum IGT. Cho et al. [19], who performed a multi-center prospective study on Korean women with previous GDM, found that women with diabetes had greater BMI, body weight, and waist circumferences than women with NGT. Multiple logistic regression analysis revealed that waist circumference is the strongest obesity index, along with systolic blood pressure, and that triglyceride levels are the major independent risk factor for developing diabetes.
Table 1.
Antepartum clinical and metabolic characteristics of Korean women with GDM
GDM, gestational diabetes mellitus; NGT, normal glucose tolerance; IGT, impaired glucose tolerance; BMI, body mass index; OGTT, oral glucose tolerance test.
abcp < 0.05; values in each line that share the same symbol are significantly different.
The association between postpartum diabetes and the severity of hyperglycemia during pregnancy in women with previous GDM has also been documented in other ethnic groups [2,10,12-14,26,27]. Observations of impaired B-cell function as an independent predictor for T2DM in Korean women [11] is in agreement with several studies in the US [10,27,28]. Although pre-pregnancy weight and BMI in Korean women with GDM is typically considerably lower than in other study populations (especially in North American studies), pre-pregnancy weight and waist circumference have been found to be independent risk factors for postpartum diabetes in Korean women [11,19]. A study of Chinese women in Hong Kong also noted that maternal BMI was only marginally associated with postpartum diabetes in women with previous GDM. Several studies in North America have also revealed that maternal BMI is an independent risk factor for postpartum diabetes [10,29,30]. In particular, Metzger et al. [10] reported that women with previous GDM and diabetes in early postpartum had impaired B-cell function, and later onset of diabetes was independently associated with pre-pregnancy weight and impaired insulin secretion at diagnosis of GDM.
Recently, Xiang et al. [31] studied 72 Hispanic women to identify prognostic factors associated with postpartum diabetes up to 12 years following delivery. They found that low insulin sensitivity and impaired B-cell function (low B-cell compensation for insulin resistance) at baseline were independently associated with the development of diabetes. In the follow-up period, body weight (fat) gain and rates of decline in beta cell compensation were significantly associated with postpartum diabetes. Lim et al. [32] performed a case-control study on Korean women with previous GDM to investigate insulin sensitivity and body composition (especially visceral fat at the postpartum evaluation) as contributors to the development of impaired glucose metabolism after delivery. They found that visceral fat was greater in women with IGT than in age- and BMI-matched women with NGT or normal control women. The insulin sensitivity index was lower in women with IGT than those with NGT or normal control women. B-cell function, as measured by the acute insulin response to glucose, was also lower in women with IGT. They concluded that visceral obesity and a low insulin response to glucose might contribute simultaneously to the development of impaired glucose metabolism in Korean women with previous GDM.
In summary, Korean women with previous GDM had a similar incidence of postpartum diabetes and the risk factors for development of diabetes in these women were also similar to those found in North American women.
POSTPARTUM SCREENING AND PREVENTION OF DIABETES IN WOMEN WITH PREVIOUS GDM
The American Diabetes Association (ADA) recommends screening for diabetes in women with GDM at 6-12 weeks postpartum by measuring fasting plasma glucose or with a 75 g OGTT [33]. Women should then be reevaluated every 3 years if their glucose tolerance status is NGT. The American College of Obstetrics and Gynecology (ACOG) suggests that postpartum screening for T2DM be performed at the first postpartum visit [34]. ACOG does not recommend but suggests postpartum screening in women with GDM, citing the lack of longterm studies that support the benefits of testing. However, a survey of ACOG Fellows in 2004 found that 75% of participants performed routine postpartum screening, and 51% used the 75 g OGTT [35].
Both the ADA and ACOG recommend that women with previous GDM be educated or counseled about lifestyle changes including diet, exercise, and weight reduction [33,34].
Several studies have revealed that lifestyle intervention is effective in the prevention or delay of developing T2DM in high risk populations [36-38]. The DPP demonstrated that lifestyle intervention reduces the incidence of T2DM by 58% (95% confidence interval [CI], 48% to 66%) and metformin by 31% (95% CI, 17% to 43%) in diverse ethnic people with IGT, as compared with a placebo [36]. An ancillary study by the DPP enrolled women with a history of GDM and demonstrated that lifestyle intervention reduced the rate of development of T2DM by 53.4% and 49.2% in women with or without a GDM history, respectively, as compared with women in a placebo group. This reduction occurred even though the women with a history of GDM lost less weight than the women without a GDM history (1.60±0.80 kg vs. 4.03±0.40 kg at year 3, respectively) during a lifestyle intervention [22]. This study also showed that metformin treatment was 3 times more effective in reducing the incidence of diabetes in women with a GDM history than in those without a GDM history.
The Troglitazone in the Prevention of Diabetes (TRIPOD) study demonstrated a 55% risk reduction in developing T2DM with troglitazone treatment [37], which was comparable with reductions of 53.4% for lifestyle intervention and 50.4% for metformin treatment in women with previous GDM in the DPP study.
An observational study of Korean women with previous GDM showed that a weight loss of approximately 4 kg to 5 kg within 3 years postpartum has a significant impact on the development of diabetes (Jang HC, Park HK, Cho NH. Gestational diabetes in Korea: postpartum weight change and development of type 2 diabetes [unpublished data]). When women with previous GDM were stratified into 3 groups based on tertiles of BMI changes, the frequency of postpartum diabetes was 11.5% at baseline, but only 5.4% at end of the follow-up period in women who lowered their BMI by ≥3.8% (weight change, -4.8±3.0 kg).
In conclusion, Korean women with previous GDM had a similar incidence of postpartum diabetes, even though their BMI was relatively lower compared to Western women. Reduction of body weight or body fat might be also effective on prevention of T2DM in Korean women with previous GDM. Further studies on clinical trial for diabetes prevention in Korean women with previous GDM is needed.
ACKNOWLEDGMENT
This research was supported by a research grant (02-2010-013) from the Seoul National University Bundang Hospital, a Clinical Research Award from the Korean Diabetes Association, and a grant (00-PJ3-PG6-GN07-001) from the Korea Health 21 R&D Project, Ministry of Health and Welfare, Republic of Korea.
Worthy of great appreciation are Drs. Soo Lim, Sung Hee Choi, Soo Heon Kwak, Young Min Cho, Kyong Soo Park, and Nam H. Cho for collecting data and providing thoughtful comments, as well as Ms. Ye Jin Lee for her technical assistance.
References
- 1.Metzger BE. Summary and recommendations of the Third International Workshop-Conference on Gestational Diabetes Mellitus. Diabetes. 1991;40(Suppl 2):197–201. doi: 10.2337/diab.40.2.s197. [DOI] [PubMed] [Google Scholar]
- 2.Kim C, Newton KM, Knopp RH. Gestational diabetes and the incidence of type 2 diabetes: a systematic review. Diabetes Care. 2002;25:1862–1868. doi: 10.2337/diacare.25.10.1862. [DOI] [PubMed] [Google Scholar]
- 3.Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS Kaiser Permanente of Colorado GDM Screening Program. Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care. 2005;28:579–584. doi: 10.2337/diacare.28.3.579. [DOI] [PubMed] [Google Scholar]
- 4.Jang HC, Cho YM, Park KS, Kim SY, Lee HK, Kim MY, Yang JH, Shin SM. Pregnancy outcome in Korean women with gestational diabetes mellitus diagnosed by the Carpenter-Coustan criteria. J Korean Diabetes Assoc. 2004;28:122–130. [Google Scholar]
- 5.Jovanovic L, Pettitt DJ. Gestational diabetes mellitus. JAMA. 2001;286:2516–2518. doi: 10.1001/jama.286.20.2516. [DOI] [PubMed] [Google Scholar]
- 6.O'Sullivan JB. Body weight and subsequent diabetes mellitus. JAMA. 1982;248:949–952. [PubMed] [Google Scholar]
- 7.O'Sullivan JB, Mahan CM. Criteria for the oral glucose tolerance test in pregnancy. Diabetes. 1964;13:278–285. [PubMed] [Google Scholar]
- 8.Buchanan TA, Metzger BE, Freinkel N, Bergman RN. Insulin sensitivity and B-cell responsiveness to glucose during late pregnancy in lean and moderately obese women with normal glucose tolerance or mild gestational diabetes. Am J Obstet Gynecol. 1990;162:1008–1014. doi: 10.1016/0002-9378(90)91306-w. [DOI] [PubMed] [Google Scholar]
- 9.Ryan EA, Imes S, Liu D, McManus R, Finegood DT, Polonsky KS, Sturis J. Defects in insulin secretion and action in women with a history of gestational diabetes. Diabetes. 1995;44:506–512. doi: 10.2337/diab.44.5.506. [DOI] [PubMed] [Google Scholar]
- 10.Metzger BE, Cho NH, Roston SM, Radvany R. Prepregnancy weight and antepartum insulin secretion predict glucose tolerance five years after gestational diabetes mellitus. Diabetes Care. 1993;16:1598–1605. doi: 10.2337/diacare.16.12.1598. [DOI] [PubMed] [Google Scholar]
- 11.Jang HC, Yim CH, Han KO, Yoon HK, Han IK, Kim MY, Yang JH, Cho NH. Gestational diabetes mellitus in Korea: prevalence and prediction of glucose intolerance at early postpartum. Diabetes Res Clin Pract. 2003;61:117–124. doi: 10.1016/s0168-8227(03)00110-4. [DOI] [PubMed] [Google Scholar]
- 12.Metzger BE, Bybee DE, Freinkel N, Phelps RL, Radvany RM, Vaisrub N. Gestational diabetes mellitus: correlations between the phenotypic and genotypic characteristics of the mother and abnormal glucose tolerance during the first year postpartum. Diabetes. 1985;34(Suppl 2):111–115. doi: 10.2337/diab.34.2.s111. [DOI] [PubMed] [Google Scholar]
- 13.Kjos SL, Buchanan TA, Greenspoon JS, Montoro M, Bernstein GS, Mestman JH. Gestational diabetes mellitus: the prevalence of glucose intolerance and diabetes mellitus in the first two months post partum. Am J Obstet Gynecol. 1990;163(1 Pt 1):93–98. doi: 10.1016/s0002-9378(11)90676-0. [DOI] [PubMed] [Google Scholar]
- 14.Catalano PM, Vargo KM, Bernstein IM, Amini SB. Incidence and risk factors associated with abnormal postpartum glucose tolerance in women with gestational diabetes. Am J Obstet Gynecol. 1991;165(4 Pt 1):914–919. doi: 10.1016/0002-9378(91)90438-w. [DOI] [PubMed] [Google Scholar]
- 15.Dacus JV, Meyer NL, Muram D, Stilson R, Phipps P, Sibai BM. Gestational diabetes: postpartum glucose tolerance testing. Am J Obstet Gynecol. 1994;171:927–931. doi: 10.1016/s0002-9378(94)70060-5. [DOI] [PubMed] [Google Scholar]
- 16.Kim YL, Cho YW, Park SW, Lee SK, Ahn IS, Na BW, Lee J, Cho YK, Lee HY, Lee SJ. Antepartum characteristics predicting persistent postpartum glucose lntolerance in the patients with gestational diabetes mellitus (GDM) J Korean Diabetes Assoc. 2000;24:46–59. [Google Scholar]
- 17.Lam KS, Li DF, Lauder IJ, Lee CP, Kung AW, Ma JT. Prediction of persistent carbohydrate intolerance in patients with gestational diabetes. Diabetes Res Clin Pract. 1991;12:181–186. doi: 10.1016/0168-8227(91)90075-o. [DOI] [PubMed] [Google Scholar]
- 18.Ko GT, Chan JC, Tsang LW, Li CY, Cockram CS. Glucose intolerance and other cardiovascular risk factors in Chinese women with a history of gestational diabetes mellitus. Aust N Z J Obstet Gynaecol. 1999;39:478–483. doi: 10.1111/j.1479-828x.1999.tb03138.x. [DOI] [PubMed] [Google Scholar]
- 19.Cho NH, Jang HC, Park HK, Cho YW. Waist circumference is the key risk factor for diabetes in Korean women with history of gestational diabetes. Diabetes Res Clin Pract. 2006;71:177–183. doi: 10.1016/j.diabres.2005.06.003. [DOI] [PubMed] [Google Scholar]
- 20.Tam WH, Yang XL, Chan JC, Ko GT, Tong PC, Ma RC, Cockram CS, Sahota D, Rogers MS. Progression to impaired glucose regulation, diabetes and metabolic syndrome in Chinese women with a past history of gestational diabetes. Diabetes Metab Res Rev. 2007;23:485–489. doi: 10.1002/dmrr.741. [DOI] [PubMed] [Google Scholar]
- 21.Krishnaveni GV, Hill JC, Veena SR, Geetha S, Jayakumar MN, Karat CL, Fall CH. Gestational diabetes and the incidence of diabetes in the 5 years following the index pregnancy in South Indian women. Diabetes Res Clin Pract. 2007;78:398–404. doi: 10.1016/j.diabres.2007.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Ratner RE, Christophi CA, Metzger BE, Dabelea D, Bennett PH, Pi-Sunyer X, Fowler S, Kahn SE Diabetes Prevention Program Research Group. Prevention of diabetes in women with a history of gestational diabetes: effects of metformin and lifestyle interventions. J Clin Endocrinol Metab. 2008;93:4774–4779. doi: 10.1210/jc.2008-0772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lee H, Jang HC, Park HK, Metzger BE, Cho NH. Prevalence of type 2 diabetes among women with a previous history of gestational diabetes mellitus. Diabetes Res Clin Pract. 2008;81:124–129. doi: 10.1016/j.diabres.2008.02.017. [DOI] [PubMed] [Google Scholar]
- 24.Lee AJ, Hiscock RJ, Wein P, Walker SP, Permezel M. Gestational diabetes mellitus: clinical predictors and long-term risk of developing type 2 diabetes--a retrospective cohort study using survival analysis. Diabetes Care. 2007;30:878–883. doi: 10.2337/dc06-1816. [DOI] [PubMed] [Google Scholar]
- 25.Oldfield MD, Donley P, Walwyn L, Scudamore I, Gregory R. Long term prognosis of women with gestational diabetes in a multiethnic population. Postgrad Med J. 2007;83:426–430. doi: 10.1136/pgmj.2006.056267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Golden SH, Bennett WL, Baptist-Roberts K, Wilson LM, Barone B, Gary TL, Bass E, Nicholson WK. Antepartum glucose tolerance test results as predictors of type 2 diabetes mellitus in women with a history of gestational diabetes mellitus: a systematic review. Gend Med. 2009;6(Suppl 1):109–122. doi: 10.1016/j.genm.2008.12.002. [DOI] [PubMed] [Google Scholar]
- 27.Buchanan TA, Xiang A, Kjos SL, Lee WP, Trigo E, Nader I, Bergner EA, Palmer JP, Peters RK. Gestational diabetes: antepartum characteristics that predict postpartum glucose intolerance and type 2 diabetes in Latino women. Diabetes. 1998;47:1302–1310. doi: 10.2337/diab.47.8.1302. [DOI] [PubMed] [Google Scholar]
- 28.Buchanan TA, Xiang AH, Kjos SL, Trigo E, Lee WP, Peters RK. Antepartum predictors of the development of type 2 diabetes in Latino women 11-26 months after pregnancies complicated by gestational diabetes. Diabetes. 1999;48:2430–2436. doi: 10.2337/diabetes.48.12.2430. [DOI] [PubMed] [Google Scholar]
- 29.Coustan DR, Carpenter MW, O'Sullivan PS, Carr SR. Gestational diabetes: predictors of subsequent disordered glucose metabolism. Am J Obstet Gynecol. 1993;168:1139–1144. doi: 10.1016/0002-9378(93)90358-p. [DOI] [PubMed] [Google Scholar]
- 30.Kaufmann RC, Schleyhahn FT, Huffman DG, Amankwah KS. Gestational diabetes diagnostic criteria: long-term maternal follow-up. Am J Obstet Gynecol. 1995;172(2 Pt 1):621–625. doi: 10.1016/0002-9378(95)90582-0. [DOI] [PubMed] [Google Scholar]
- 31.Xiang AH, Kjos SL, Takayanagi M, Trigo E, Buchanan TA. Detailed physiological characterization of the development of type 2 diabetes in Hispanic women with prior gestational diabetes mellitus. Diabetes. 2010;59:2625–2630. doi: 10.2337/db10-0521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lim S, Choi SH, Park YJ, Park KS, Lee HK, Jang HC, Cho NH, Metzger BE. Visceral fatness and insulin sensitivity in women with a previous history of gestational diabetes mellitus. Diabetes Care. 2007;30:348–353. doi: 10.2337/dc06-1405. [DOI] [PubMed] [Google Scholar]
- 33.American Diabetes Association. Gestational diabetes mellitus. Diabetes Care. 2004;27(Suppl 1):S88–S90. doi: 10.2337/diacare.27.2007.s88. [DOI] [PubMed] [Google Scholar]
- 34.American College of Obstetricians and Gynecologists Committee on Practice Bulletins--Obstetrics. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 30, September 2001 (replaces Technical Bulletin Number 200, December 1994). Gestational diabetes. Obstet Gynecol. 2001;98:525–538. [PubMed] [Google Scholar]
- 35.Gabbe SG, Gregory RP, Power ML, Williams SB, Schulkin J. Management of diabetes mellitus by obstetrician-gynecologists. Obstet Gynecol. 2004;103:1229–1234. doi: 10.1097/01.AOG.0000128045.50439.89. [DOI] [PubMed] [Google Scholar]
- 36.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997;20:537–544. doi: 10.2337/diacare.20.4.537. [DOI] [PubMed] [Google Scholar]
- 38.Tuomilehto J, Lindstrom J, Eriksson JG, Valle TT, Hamalainen H, Ilanne-Parikka P, Keinanen-Kiukaanniemi S, Laakso M, Louheranta A, Rastas M, Salminen V, Uusitupa M Finnish Diabetes Prevention Study Group. Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med. 2001;344:1343–1350. doi: 10.1056/NEJM200105033441801. [DOI] [PubMed] [Google Scholar]