Abstract
Introduction: Degenerative spine disorders are steadily increasing parallel to the aging of the population with considerable impact on cost and productivity. In this paper we study the prevalence and risk factors for multiple spine surgery and its impact on cost.
Methods: Data on 1,153 spine surgery inpatients operated between October 2005 and September 2008 (index spine surgery) in regard to the number of previous spine surgeries and location of surgeries (cervical or lumbar) were retrospectively collected. Additionally, prospective follow-up over a period of 2-5 years was conducted.
Results: Retrospectively, 365 (31.7%) patients were recurrent spine surgery patients while 788 (68.3%) were de novo spine surgery patients.
Nearly half of those with previous spine surgery (51.5%) were on different regions of the spine.
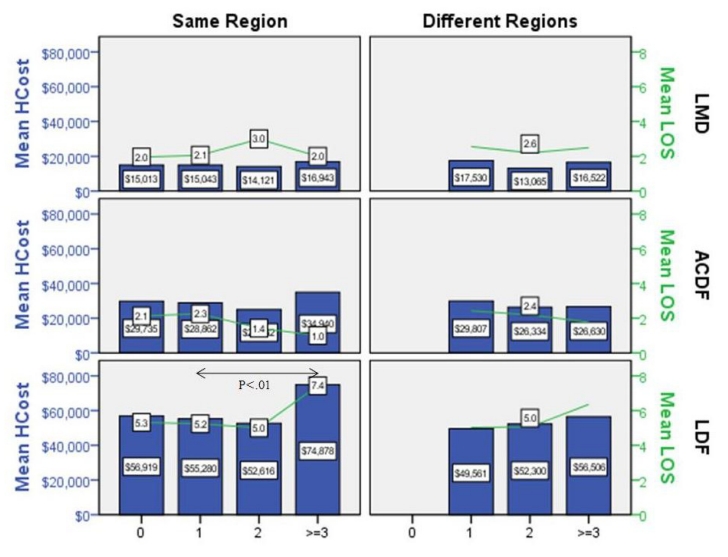
There were no significant differences in length of stay or hospital charges except in lumbar decompression and fusion (LDF) patients with multiple interventions on the same region of the spine. Significant differences (P<.05) in length of stay (5.4 days vs. 7.4 days) and hospital charges ($55,477 vs. $74,878) between LDF patients with one previous spine versus those with ≥3 previous spine surgeries on the same region were noted.
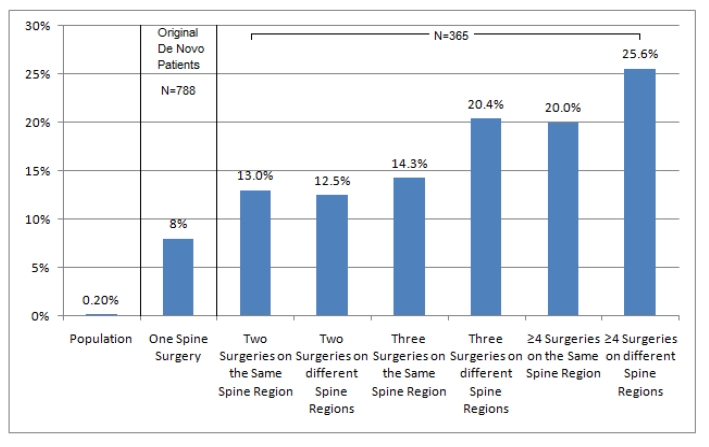
Prospectively, the overall reoperation rate was 10.4%. The risk of additional spine surgery increased from 8.0% in patients with one previous spine surgery (index surgery) to 25.6% in patients with ≥4 previous spine surgeries on different regions of the spine (including index surgery).
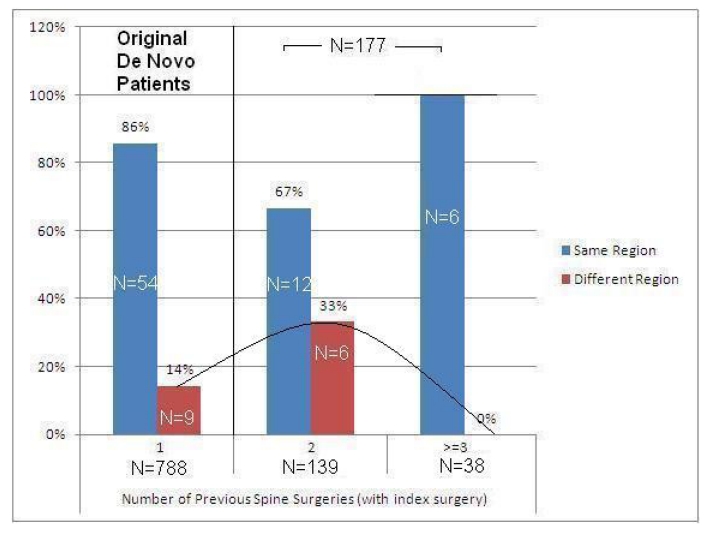
After excluding patients with previous spine surgeries on different regions of the spine, 17.2% of reoperated patients had additional spine surgery on a different spine region. The percentage of additional spine surgery on a distant spine region increased from 14.0% in patients with one spine surgery to 33.0% in patients with two spine surgeries on the same region. However, in patients with three or more spine surgeries on the same spine region there were no interventions on a distant spine region during the follow-up period.
Conclusion: De novo spine surgery is associated with an increased incidence of additional spine surgery at the same or distant spine regions. Large prospective studies with extended follow-up periods and multifaceted cost-outcome analysis are needed to refine the appropriateness of spine surgery.
Keywords: multiple spine surgery, spine region, cost
Abstract
Einführung: Wirbelsäulenerkrankungen nehmen parallel zur Alterung der Bevölkerung ständig zu mit beachtlichen Auswirkungen auf Kosten und Produktivität. In diesem Artikel werden die Prävalenz und die Risikofaktoren für mehrfache Wirbelsäulenoperationen und ihr Einfluss auf die Folgekosten untersucht.
Methoden: Eine retrospektive Analyse von 1.153 Krankenhauspatienten nach Wirbelsäulenoperationen im Zeitraum von Oktober 2005 bis September 2008 auch in Bezug auf vorausgegangene Wirbelsäulenoperationen und deren Lokalisation (Hals- oder Lendenwirbelsäule) wurde erstellt. Zusätzlich wurden die Nachuntersuchungen über 2–5 Folgejahre erfasst.
Ergebnisse: Rückblickend hatten 365 (31,7%) der Patienten wiederholte chirurgische Eingriffe an der Wirbelsäule, während bei 788 (68,3%) Patienten der operative Eingriff erstmalig erfolgte. Etwa bei der Hälfte (51,5%) der Patienten mit wiederholten Wirbelsäulenoperationen wurden diese in verschiedenen Bereichen durchgeführt.
Es gab keine signifikanten Unterschiede bei der Dauer des Klinikaufenthaltes oder bei den Klinikkosten außer bei Patienten mit lumbaler Dekompression und Fusion (LDF) mit mehrfachen Eingriffen im gleichen Operationsbereich. Signifikante Unterschiede (P<0,05) wurden gefunden beim Dauer des Klinikaufenthalts (5,5 Tage versus 7,4 Tage) und bei den Krankenhauskosten (55.477 $ versus 77.877 $) zwischen LDF-Patienten mit einer vorherigen Wirbelsäulenoperation verglichen mit Patienten mit drei und mehr vorausgegangenen Operationen in demselben Wirbelsäulenbereich.
Prospektiv lag die Häufigkeit erneuter Operationen durchschnittlich bei 10,4%. Das Risiko einer zusätzlichen Wirbelsäulenoperation stieg von 8,0% bei Patienten mit einer vorausgegangenen Wirbelsäulenoperation (Indexoperation) auf 25,6% bei Patienten mit 4 und mehr chirurgischen Eingriffen an verschiedenen Regionen der Wirbelsäule (incl. Indexoperation).
Nach Ausschluss aller Patienten mit vorausgegangenen Wirbelsäulenoperationen in verschiedenen Wirbelsäulenbereichen hatten 17,2% der erneut operierten Patienten eine zusätzliche Operation in einem anderen Wirbelsäulenbereich. Der Prozentsatz der zusätzlichen chirurgischen Eingriffe in einem entfernten Wirbelsäulenbereich lag bei Patienten mit einer Wirbelsäulenoperation bei 14% und stieg auf 33% bei Patienten mit zwei Operationen im selben Bereich. Jedoch gab es bei Patienten mit drei und mehr chirurgischen Eingriffen in der gleichen Wirbelsäulenregion während der Beobachtungsperiode keine weiteren Operationen in einer anderen Region.
Schlussfolgerung: Eine Erstoperation an der Wirbelsäule ist assoziiert mit einer erhöhten Häufigkeit von weiteren Wirbelsäulenoperationen im gleichen oder einem anderen Wirbelsäulenbereich. Große prospektive Studien mit längeren Beobachtungsperioden und Kosten-Nutzen-Analysen sind erforderlich, um die Angemessenheit von Wirbelsäulenoperationen in geeigneter Form bewerten zu können.
Introduction
Vertebral column difficulties are an ubiquitous penalty for the upright posture of our species. Increasingly aggressive surgical intervention has been introduced to ameliorate such difficulties resulting in substantial rise in the rate and cost of spine surgery, especially in the United States [1], [2], [3], [4], [5], [6], [7]. To study the prevalence and risk factors for multiple spine surgery in our patient population we conducted the following inquiry.
Methods
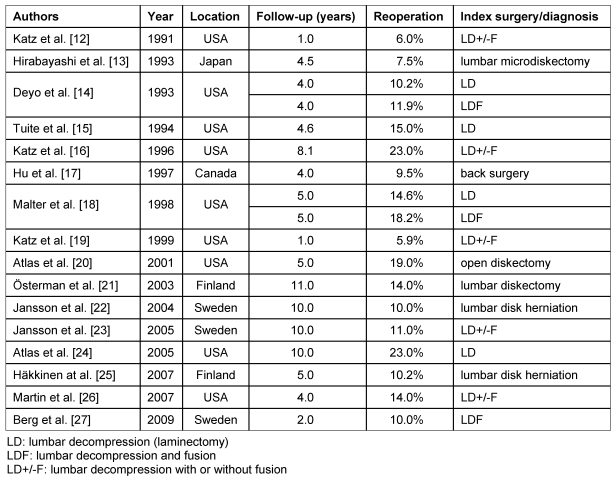
The clinical records of 1,153 spine surgery inpatients operated between Oct 2005 and Sep 2008 were retrospectively reviewed and their clinical course prospectively followed. The index surgery was lumbar microdiskectomy (LMD) in 235 cases, anterior cervical decompression and fusion (ACDF) in 696 and lumbar decompression and fusion patients (LDF) in 222 cases (Figure 1 (Fig. 1)). Recurrent patients were defined as those with previous spine surgery and de novo patients were those with no previous spine surgery.
Figure 1. Study structure in relationship to index surgery.
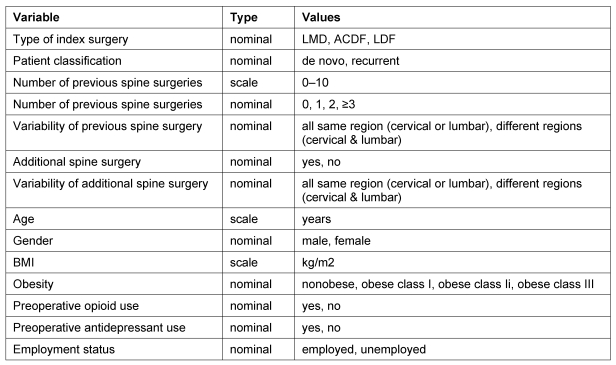
Data on patient demographics, number of previous spine surgeries, location of surgery, number of additional spine surgeries during the follow-up period of 2-5 years (prospective), opioid and antidepressant use were collected (Table 1 (Tab. 1)). Over half of the cohort (53%) was females. The average age was 56±15 for LMD patients, 53±11 for ACDF patients and 56±12 for LDF patients. Regression analysis was applied with the help of SPSS v16.
Table 1. Studied variables.
Results
Age, gender and number of previous spine surgeries (PSS)
De novo patients were slightly younger than recurrent patients. The average age of de novo patients was 53 years while the average age of patients with 1, 2 and ≥3 was 55, 58 and 57 years. There was no significant difference in gender distribution between de novo and recurrent patients (53.6%, 53.9%, 45.5% and 51.9% females, respectively).
Prevalence of recurrent patients
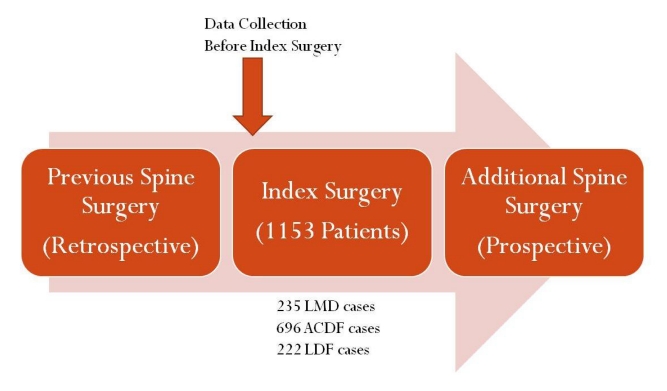
Overall, 365 (31.7%) patients were recurrent spine surgery patients while 788 (68.3%) were de novo spine surgery patients (Figure 2 (Fig. 2)). The prevalence of previous spine surgeries increased with age, from 18.4% in patients less than forty to 37.4% in patients older than sixty five. As per type of index surgery, 31.9% of LMD patients, 27.2% of ACDF patients and 45.5% of LDF patients had previous spine surgery. LDF patients older than 40 years had the highest prevalence of previous spine surgery (47.4%).
Figure 2. The distribution of patients in the retrospective and prospective branches of the study.
Differences between de novo and recurrent patients
Significant differences were noted between de novo and recurrent patients in average age (53 years vs. 56 years, P<.05), percentage of patient over 65 years of age (16.4% vs. 21.1%, P<.01), percentage of patients on antidepressants (27.0% vs. 34.2% P<.05) and percentage of patients with osteoporosis (1.9% vs. 4.9%, P<.01).
Number and location of previous spine surgeries
The majority of recurrent patients (235) had one previous spine surgery; a smaller group (77) had two previous spine surgeries and a minority (54) had three or more spine surgeries. Overall, 11.3% had two or more PSS and 16.3% had previous surgical interventions on more than one region of the spine, i.e. nearly half of recurrent patients (177) had previous spine surgeries on the same spine region (Figure 2 (Fig. 2)). Specifically, 63.6% of patients with two previous spine surgeries had surgery on different regions of the spine and 81.1% of those with ≥3 previous spine surgeries had surgery on different regions of the spine. Among these patients (with previous spine surgery), LDF patients 40 years of age and younger had the highest prevalence of previous spine surgery on different regions of the spine (87.5%). Patients with ≥3 previous spine surgeries had a higher percentage of osteoporosis (11.1% vs.1.9%) and rheumatoid arthritis (3.7% vs. 1.1%) compared with de novo patients.
Factors affecting the number of previous spine surgeries
Regression analysis using the number of previous spine surgeries as the dependent variable and type of index surgery, spine region (same, variable), age, gender, obesity, antidepressant-opioid use and employment as predictors showed that previous spine surgery on two different spine regions (cervical and lumbar) is the most significant predictor of the number of previous spine surgeries (t=23.396, P=0.000). Other important factors were type of index surgery, age and opioid use. Patients with 0, 1, 2, ≥3 previous spine surgeries had opioid use rates of 47.2%, 49.2%, 50.7% and 68.5% respectively.
The impact of the number of previous spine surgeries on hospital charges
There were significant differences (P<.01) in length of stay (5.2 days vs. 7.4 days) and hospital charges ($55,280 vs. $74,878) between LDF patients with one previous spine versus those with ≥3 previous spine on the same region (Figure 3 (Fig. 3)).
Figure 3. Hospital length of stay and charges per type of index surgery, number of previous spine surgeries and location of surgery.
Impact of previous spine surgery on the rate of additional spine surgery
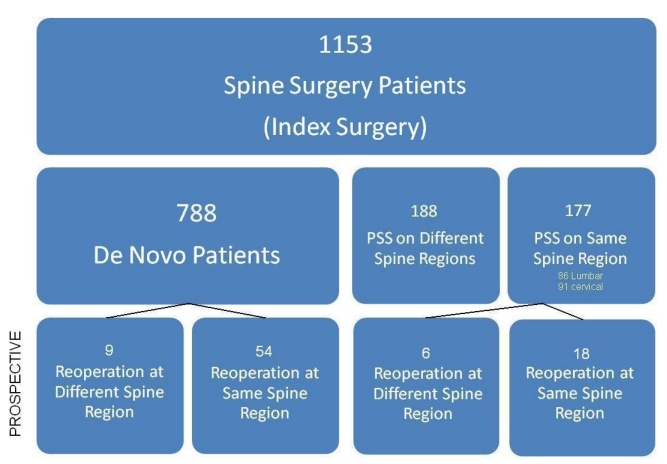
Overall, 10.4% of patients came back for additional spine surgery within the follow-up period of 2–5 years (Figure 4 (Fig. 4)). This was reasonably consistent with the literature (Table 2 (Tab. 2)).
Figure 4. The risk of future spine surgery per patient classification.
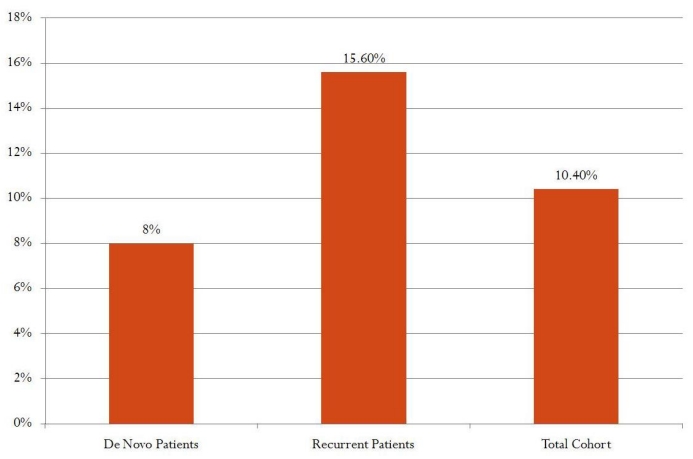
Table 2. Reoperation rates in the literature.
Patients with more PSS and those with PSS in different regions of the spine were more likely to come for additional spine surgery. The risk of additional spine surgery increased from 8.0% in patients with one previous spine surgery (index surgery) to 25.6% in patients with ≥4 previous spine surgeries on different regions of the spine (including index surgery, Figure 5 (Fig. 5)). These numbers are significantly higher than the risk of spine surgery in the general population, 201 per 100,000 [6] (Figure 5 (Fig. 5)). Regression analysis showed age, employment status and number of previous spine surgeries to be the most important predictors of return for additional spine surgery (Yes/No).
Figure 5. The risk of future spine surgery in the general population vs. patients with a history of spine surgery (index surgery included).
Impact of previous spine surgery on the rate of additional spine surgery on a distant region
After excluding patients with previous spine surgeries on different spine regions, we calculated the risk of additional spine surgery on a distant spine region from the remaining cohort (965 patients). We found that 17.2% of reoperated patients had additional spine surgery on a different spine region. The percentage of additional spine surgery on a distant spine region increased from 14.0% in patients with one spine surgery to 33.0% in patients with two spine surgeries on the same region. However, in patients with three or more spine surgeries on the same spine region there were no additional surgeries on a distant spine region during the follow-up period (Figure 6 (Fig. 6)).
Figure 6. The risk of future spine surgery on the same and distant spine regions based on the number of previous spine surgeries (same region cohort).
Discussion
Our study is not without its limitations. The follow-up period is relatively short and uneven for all patients. Additionally, a substantial number of patients may have been lost to follow-up. Our clinical outcome analysis only reflected reoperation rates ignoring other outcome parameters such as pain, function, neurological exam as well as work and disability status. We limited our economic impact analysis to hospital cost which represents a small part of the total healthcare cost of spine disease patients that also includes physician fees, rehabilitation costs and disability compensation. Large prospective studies with extended follow-up periods and cost-outcome analysis are needed to objectively study the cost-benefit of spine surgery.
With these caveats aside, our study suggests that the more frequent the individual spine operations the greater the likelihood of repeat surgery either at the same level or at a distant site. In cases of reoperation on the same spine region, the greater the number of spine surgeries the higher the hospital cost and length of stay; otherwise hospital cost and length of stay are fairly similar.
It is been well established that surgery at one level of the spine is associated with an increased risk of repeated surgery at that same or adjacent level due mainly to recurrence of the initial spine pathology [8]. As stated earlier, our study suggests that the risk of surgical intervention on a distant site also increases. Several reasons may exist for such a finding. Firstly, the patient undergoing surgery at a different geographical site may be afflicted with a diffuse osseous disease such as osteoporosis. Indeed, such a factor did exist in our study cohort. Osteoporosis is increasing in magnitude with the aging population especially in women. Such patients are prone to develop painful and debilitating spinal deformities which are difficult to treat leading to multiple surgical interventions [9]. Another explanation might be that surgical intervention on one segment of the spine may change spine biomechanics predisposing to new spine difficulties at a distant area. While the presence of such altered biomechanics at adjacent levels is well documented [10]. However, the impact of spine surgery on distant biomechanics of the spine is less clear [11]. Additionally, patients who undergo spine surgery may develop analgesic dependency which predisposes them to request surgery at additional levels. Similarly, patients with recurring vertebral column pain, having obtained relief from earlier operative intervention, may seek surgical treatment more willingly than patients from the general population.
Importantly, the assessment of our patient cohort suggests that a substantial proportion of patients are predisposed to multiple spine surgeries on different regions of the spine – a variable that is not commonly analyzed in reported outcome of spine procedures. If additional spine surgery at a distant spine region is causally connected to initial spine surgery then most present day outcome evaluation and risk-benefit analysis of de novo spine surgery is excessively optimistic. Understanding clinical dynamics in this group may have significant input in promoting therapeutic efficiency and improving surgical outcome.
Notes
Competing interests
The authors declare that they have no competing interests.
Award
This paper was awarded First Place Eposter in the Category of Socioeconomic at the 2011 American Association of Neurological Surgeons Annual Meeting, Denver, Colorado.
References
- 1.Cherkin DC, Deyo RA, Loeser JD, Bush T, Waddell G. An international comparison of back surgery rates. Spine (Phila Pa 1976) 1994;19(11):1201–1206. doi: 10.1097/00007632-199405310-00001. [DOI] [PubMed] [Google Scholar]
- 2.Davis H. Increasing rates of cervical and lumbar spine surgery in the United States, 1979-1990. Spine (Phila Pa 1976) 1994;19(10):1117–1124. doi: 10.1097/00007632-199405001-00003. Available from: http://dx.doi.org/10.1097/00007632-199405001-00003. [DOI] [PubMed] [Google Scholar]
- 3.Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA. 2010;303(13):1259–1265. doi: 10.1001/jama.2010.338. Available from: http://dx.doi.org/10.1001/jama.2010.338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frymoyer JW. Are we performing too much spinal surgery? Iowa Orthop J. 1989;9:32–36. [Google Scholar]
- 5.Frymoyer JW, Pope MH, Clements JH, Wilder DG, MacPherson B, Ashikaga T. Risk factors in low-back pain. An epidemiological survey. J Bone Joint Surg Am. 1983;65(2):213–218. doi: 10.2106/00004623-198365020-00010. [DOI] [PubMed] [Google Scholar]
- 6.Gray DT, Deyo RA, Kreuter W, Mirza SK, Heagerty PJ, Comstock BA, Chan L. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976) 2006;31(17):1957–1964. doi: 10.1097/01.brs.0000229148.63418.c1. Available from: http://dx.doi.org/10.1097/01.brs.0000229148.63418.c1. [DOI] [PubMed] [Google Scholar]
- 7.Kelsey JL. Idiopathic low back pain: magnitude of the problem. In: White AA III, Gordon SL, editors. American Academy Of Orthopaedic Surgeons Symposium on Idiopathic Low Back Pain. St. Louis: Mosby; 1982. [Google Scholar]
- 8.Lee JK, Amorosa L, Cho SK, Weidenbaum M, Kim Y. Recurrent lumbar disk herniation. J Am Acad Orthop Surg. 2010;18(6):327–337. doi: 10.5435/00124635-201006000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Ponnusamy KE, Iyer S, Gupta G, Khanna AJ. Instrumentation of the osteoporotic spine: biomechanical and clinical considerations. Spine J. 2011;11(1):54–63. doi: 10.1016/j.spinee.2010.09.024. Available from: http://dx.doi.org/10.1016/j.spinee.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 10.Wang S, Xia Q, Passias P, Li W, Wood K, Li G. How Does Degenerated Lumbar Disc Disease Affect the Disc Deformation at the Cephalic Levels In Vivo? Spine (Phila Pa 1976) 2011 Jan 17; doi: 10.1097/BRS.0b013e3181f79e93. Available from: http://dx.doi.org/10.1097/BRS.0b013e3181f79e93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Matsunaga S, Sakou T, Nakanisi K. Analysis of the cervical spine alignment following laminoplasty and laminectomy. Spinal Cord. 1999;37(1):20–24. doi: 10.1038/sj.sc.3100749. Available from: http://dx.doi.org/10.1038/sj.sc.3100749. [DOI] [PubMed] [Google Scholar]
- 12.Katz JN, Lipson SJ, Larson MG, McInnes JM, Fossel AH, Liang MH. The outcome of decompressive laminectomy for degenerative lumbar stenosis. J Bone Joint Surg Am. 1991;73(6):809–816. [PubMed] [Google Scholar]
- 13.Hirabayashi S, Kumano K, Ogawa Y, Aota Y, Maehiro S. Microdiscectomy and second operation for lumbar disc herniation. Spine (Phila Pa 1976) 1993;18(15):2206–2211. doi: 10.1097/00007632-199311000-00010. Available from: http://dx.doi.org/10.1097/00007632-199311000-00010. [DOI] [PubMed] [Google Scholar]
- 14.Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion. A cohort study of complications, reoperations, and resource use in the Medicare population. Spine (Phila Pa 1976) 1993;18(11):1463–1470. doi: 10.1097/00007632-199318110-00010. Available from: http://dx.doi.org/10.1097/00007632-199318110-00010. [DOI] [PubMed] [Google Scholar]
- 15.Tuite GF, Stern JD, Doran SE, Papadopoulos SM, McGillicuddy JE, Oyedijo DI, Grube SV, Lundquist C, Gilmer HS, Schork MA, et al. Outcome after laminectomy for lumbar spinal stenosis. Part I: Clinical correlations. J Neurosurg. 1994;81(5):699–706. doi: 10.3171/jns.1994.81.5.0699. Available from: http://dx.doi.org/10.3171/jns.1994.81.5.0699. [DOI] [PubMed] [Google Scholar]
- 16.Katz JN, Lipson SJ, Chang LC, Levine SA, Fossel AH, Liang MH. Seven- to 10-year outcome of decompressive surgery for degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 1996;21(1):92–98. doi: 10.1097/00007632-199601010-00022. Available from: http://dx.doi.org/10.1097/00007632-199601010-00022. [DOI] [PubMed] [Google Scholar]
- 17.Hu RW, Jaglal S, Axcell T, Anderson G. A population-based study of reoperations after back surgery. Spine (Phila Pa 1976) 1997;22(19):2265–2271. doi: 10.1097/00007632-199710010-00013. Available from: http://dx.doi.org/10.1097/00007632-199710010-00013. [DOI] [PubMed] [Google Scholar]
- 18.Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 1998;23(7):814–820. doi: 10.1097/00007632-199804010-00015. Available from: http://dx.doi.org/10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 19.Katz JN, Stucki G, Lipson SJ, Fossel AH, Grobler LJ, Weinstein JN. Predictors of surgical outcome in degenerative lumbar spinal stenosis. Spine (Phila Pa 1976) 1999;24(21):2229–2233. doi: 10.1097/00007632-199911010-00010. Available from: http://dx.doi.org/10.1097/00007632-199911010-00010. [DOI] [PubMed] [Google Scholar]
- 20.Atlas SJ, Keller RB, Chang Y, Deyo RA, Singer DE. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine (Phila Pa 1976) 2001;26(10):1179–1187. doi: 10.1097/00007632-200105150-00017. Available from: http://dx.doi.org/10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 21.Österman H, Sund R, Seitsalo S, Keskimäki I. Risk of multiple reoperations after lumbar discectomy: a population-based study. Spine (Phila Pa 1976) 2003;28(6):621–627. doi: 10.1097/00007632-200303150-00019. Available from: http://dx.doi.org/10.1097/00007632-200303150-00019. [DOI] [PubMed] [Google Scholar]
- 22.Jansson KA, Németh G, Granath F, Blomqvist P. Surgery for herniation of a lumbar disc in Sweden between 1987 and 1999. An analysis of 27,576 operations. J Bone Joint Surg Br. 2004;86(6):841–847. doi: 10.1302/0301-620X.86B6.14740. Available from: http://dx.doi.org/10.1302/0301-620X.86B6.14740. [DOI] [PubMed] [Google Scholar]
- 23.Jansson KA, Németh G, Granath F, Blomqvist P. Spinal stenosis re-operation rate in Sweden is 11% at 10 years--a national analysis of 9,664 operations. Eur Spine J. 2005;14(7):659–663. doi: 10.1007/s00586-004-0851-9. Available from: http://dx.doi.org/10.1007/s00586-004-0851-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of lumbar spinal stenosis: 8 to 10 year results from the maine lumbar spine study. Spine (Phila Pa 1976) 2005;30(8):936–943. doi: 10.1097/01.brs.0000158953.57966.c0. Available from: http://dx.doi.org/10.1097/01.brs.0000158953.57966.c0. [DOI] [PubMed] [Google Scholar]
- 25.Häkkinen A, Kiviranta I, Neva MH, Kautiainen H, Ylinen J. Reoperations after first lumbar disc herniation surgery; a special interest on residives during a 5-year follow-up. BMC Musculoskelet Disord. 2007;8:2. doi: 10.1186/1471-2474-8-2. Available from: http://dx.doi.org/10.1186/1471-2474-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Martin BI, Mirza SK, Comstock BA, Gray DT, Kreuter W, Deyo RA. Are lumbar spine reoperation rates falling with greater use of fusion surgery and new surgical technology? Spine (Phila Pa 1976) 2007;32(19):2119–2126. doi: 10.1097/BRS.0b013e318145a56a. Available from: http://dx.doi.org/10.1097/BRS.0b013e318145a56a. [DOI] [PubMed] [Google Scholar]
- 27.Berg S, Tullberg T, Branth B, Olerud C, Tropp H. Total disc replacement compared to lumbar fusion: a randomised controlled trial with 2-year follow-up. Eur Spine J. 2009;18(10):1512–1519. doi: 10.1007/s00586-009-1047-0. Available from: http://dx.doi.org/10.1007/s00586-009-1047-0. [DOI] [PMC free article] [PubMed] [Google Scholar]