Abstract
Aim
To assess the reasons for low influenza vaccination coverage in Poland, including knowledge of influenza and attitudes toward influenza vaccination.
Methods
This was a cross-sectional, anonymous, self-administered survey in primary care patients in Lodzkie voivodship (central Poland). The study participants were adults who visited their primary care physicians for various reasons from January 1 to April 30, 2007.
Results
Six hundred and forty participants completed the survey. In 12 months before the study, 20.8% participants had received influenza vaccination. The most common reasons listed by those who had not been vaccinated were good health (27.6%), lack of trust in vaccination effectiveness (16.8%), and the cost of vaccination (9.7%). The most common source of information about influenza vaccination were primary care physicians (46.6%). Despite reasonably good knowledge of influenza, as many as approximately 20% of participants could not point out any differences between influenza and other viral respiratory tract infections.
Conclusions
The main reasons for low influenza vaccination coverage in Poland were patients’ misconceptions and the cost of vaccination. Therefore, free-of-charge vaccination and more effective informational campaigns are needed, with special focus on high-risk groups.
Due to natural variation, influenza incidence in Poland has dropped significantly over the last years in comparison with some years of the last decade of the 20th century. It is nevertheless still high: data from 2008 point to the incidence of approximately 600 per 100 000 population (1). The real incidence of the disease is underestimated, as the considerable portion of influenza cases and the resulting hospitalizations are still not registered (2). Moreover, characteristic for influenza is the occurrence of periodic pandemics. Thus, medical consequences of influenza in the country are serious, putting this infection in the focus of the public health measures.
An effective method of reducing influenza morbidity and mortality is vaccination. There are several inactivated influenza vaccines available in Poland, which were proven to prevent influenza infection and its complications in up to 70%-90% of vaccinated persons (2,3).
Since 1994, influenza vaccination has been recommended by national Protective Vaccination Program. Currently, it is recommended for healthy children (from 6 months to 18 years), elderly patients (55 and over), patients with chronic conditions (asthma, diabetes, heart failure, pulmonary dysfunction, and renal failure), and those with low immunity (4). However, vaccination is still not reimbursed from the national health insurance and the patients need to pay 100% of the price themselves. The average cost of the vaccine approximates € 8. Several initiatives undertaken by local authorities in the recent years enabled some high-risk patient groups provision of free of charge influenza vaccination (5). Unfortunately, these initiatives have been limited and have not resulted in significant improvements in influenza vaccination coverage.
Influenza virus tends to create new strains, characterized by diverse antigen structures. For this reason, the vaccine is modified yearly, according to the recommendations of the World Health Organization (6). Consequently, effective influenza protection is only achievable provided that the vaccination is repeated every year. This makes the influenza vaccination acceptance even more challenging. Recent reports suggest that the influenza vaccination coverage in Poland is far from satisfactory, actually one of the lowest in Europe (7,8). According to recent Vaccine European New Integrated Collaboration Effort Project publication, the number of influenza vaccine doses used in Poland during 2007-8 influenza season in high-risk groups (those aged over 65 and with underlying conditions) was lowest among the 15 studied European countries (9).
In order to help design future informational campaigns, the aim of this study was to assess the knowledge of influenza and attitudes toward influenza vaccination as factors related to low influenza vaccination coverage in Poland.
Material and methods
This was a cross-sectional, anonymous, self-administered survey on a convenience sample (n = 640) of primary care patients aged 18 and over in Lodzkie voivodship (central Poland) in the period January 1 to April 30, 2007 (Table 1). The patients visited their primary care physicians for various reasons and as healthy companions of sick patients. The survey was based on a 28-item questionnaire, specially constructed for this purpose, including questions (in most cases open-ended) assessing patients’ knowledge of influenza (12 items, including 8 open-ended questions), attitudes toward influenza vaccination (5 items, including 2 open-ended questions), practice of influenza vaccination (4 items), and patients’ characteristics (7 items). The English translation of the questionnaire is available in the web-extra material 1.(web extra material 1)
Table 1.
Comparison of sociodemographic characteristics between the study participants and general population of Poland
| Characteristic | No. (%) of participants (n = 640) | General population (%)* |
|---|---|---|
| Age: |
||
| range |
20-90 |
|
| average (±standard deviation) |
46.3 ± 16.6 |
|
| 18-54 years |
426 (66.6) |
67.4 |
| 55 years and more |
214 (33.4) |
33.6 |
| Sex: |
||
| women |
359 (56.1) |
52.4 |
| men |
281 (43.9) |
42.7 |
| Occupation: |
||
| blue-collar workers |
60 (9.4) |
44.7 |
| white-collar workers |
195 (30.5) |
|
| students |
71 (11.1) |
6.1 |
| farmers |
5 (0.8) |
6.8 |
| unemployed |
29 (4.5) |
6.1 |
| pensioners |
123 (19.2) |
30.2 |
| other |
45 (7.0) |
|
| not provided |
112 (17.5) |
|
| Place of residence (population): |
||
| <10 000 |
98 (15.3) |
45.0 |
| 10 000-50 000 |
147 (23.0) |
17.9 |
| 50 000-100 000 |
50 (7.8) |
8.4 |
| 100 000-500 000 |
86 (13.4) |
17.2 |
| >500 000 | 258 (40.3) | 11.5 |
*Data for general population of Poland (age 18 and older), according to the national Central Statistical Office (10).
The data were analyzed by descriptive statistics. Participants were divided into two groups: 18-54 years and 55 years and older, according to the definition of high-risk groups in the national recommendations on influenza vaccination (4). For the analysis of qualitative variables, χ2 test was used.
Results
Knowledge of influenza and influenza vaccination
The majority of participants (93.0%) believed that influenza was transmitted through the air and 25.9% believed that the infection could be caught by sharing kitchen utensils with the sick person (Table 2). Other ways of influenza spread were mentioned by fewer than 10% of participants.
Table 2.
Knowledge of influenza and influenza vaccination among study participants from Poland (n = 640)
| Item | Percentage |
|---|---|
| Most frequent ways of influenza virus transmission:* |
|
| droplet infection |
93.0 |
| common cutlery and dishes |
25.9 |
| contaminated food products |
8.6 |
| contact with infected blood |
6.1 |
| breast-feeding |
5.3 |
| sexual contact |
3.3 |
| difficult to say |
5.5 |
| Initial symptoms of influenza:† |
|
| fever |
82.0 |
| runny nose |
39.8 |
| muscle pain |
39.1 |
| headache |
29.2 |
| malaise |
28.6 |
| cough |
26.3 |
| bones and joints aches |
21.1 |
| chills |
14.8 |
| sore throat |
7.7 |
| gastrointestinal symptoms |
2.3 |
| In what sense is influenza different from the common cold?† |
|
| higher, longer-lasting temperature |
27.2 |
| influenza leads to complications |
23.1 |
| Influenza has more severe symptoms |
22.5 |
| I do not know |
17.8 |
| muscle, bone, and joints aches |
15.0 |
| influenza is a viral disease |
10.3 |
| long-lasting malaise and weakness |
5.8 |
| cough and runny nose |
4.5 |
| there is no difference |
3.1 |
| headache |
1.9 |
| influenza should be treated with antibiotics |
1.4 |
| gastrointestinal symptoms |
1.3 |
| influenza is accompanied by airways inflammation |
1.3 |
| influenza should not be treated with antibiotics |
1.3 |
| influenza occurs in epidemics |
0.5 |
| Is influenza hazardous to one’s health? |
|
| yes |
91.1 |
| no |
2.2 |
| difficult to say |
6.6 |
| Which influenza consequences might be hazardous for one’s life?† |
|
| heart diseases |
47.1 |
| respiratory disease |
27.8 |
| inflammatory complications |
15.3 |
| I do not know |
14.8 |
| arthritis |
10.3 |
| meningitis |
6.7 |
| death |
3.0 |
| susceptibility to infections |
2.5 |
| otitis media |
2.2 |
| kidney disease |
1.4 |
| myositis |
0.5 |
| lymphadenopathy |
0.3 |
| chronic cough |
0.3 |
| Who should by all means receive influenza vaccine?† |
|
| elderly |
41.9 |
| children |
36.9 |
| people with low immunity to viral infections |
25.0 |
| I do not know |
14.4 |
| health service workers |
12.5 |
| those in contact with large numbers of people |
8.0 |
| everyone |
6.4 |
| chronically ill |
4.7 |
| teachers |
4.4 |
| not everyone needs vaccination |
2.5 |
| farmers, people who have contact with animals |
2.0 |
| those who had influenza and are susceptible to disease |
1.6 |
| pregnant women and breastfeeding mothers |
0.5 |
| Who should not receive influenza vaccine?† |
|
| healthy, immune people |
12.7 |
| chronically ill |
11.1 |
| there is no such group of people |
8.9 |
| people allergic to influenza vaccine |
8.6 |
| infants, and children |
6.7 |
| pregnant women and breastfeeding mothers |
4.7 |
| people with immune deficiency |
4.4 |
| people with medical contraindications |
2.2 |
| elderly |
1.4 |
| I do not know |
42.5 |
| When is the best time to get vaccinated against influenza?† |
|
| autumn (September-November) |
66.3 |
| early autumn, before the influenza season |
9.1 |
| spring |
7.5 |
| winter (December-February) |
3.9 |
| summer |
3.3 |
| autumn-winter period |
1.6 |
| I do not know |
14.7 |
| Does influenza vaccine enhance the immunity against all types of viral infections? |
|
| yes |
19.5 |
| no |
47.0 |
| difficult to say |
33.4 |
| Does influenza vaccine protect against the avian flu? |
|
| yes |
7.2 |
| no |
60.5 |
| difficult to say |
31.7 |
| How often should the vaccination against influenza be carried out in order to guarantee the highest effectiveness?† |
|
| 1 time a year |
63.4 |
| 2 times a year |
6.6 |
| at least 1 time a year, before each influenza season |
3.1 |
| every 2 years or less frequently |
0.9 |
| 2 years +1 year break |
0.2 |
| I do not know | 25.6 |
* Participants could choose more than one answer.
†Answers to the open question.
As symptoms characteristic for the initial stage of the infection, participants most often mentioned high temperature (82.0%), runny nose (39.8%), and muscle pain (39.1%). As characteristics differentiating influenza from the common cold, participants most often mentioned higher and longer-lasting temperature (27.2%), complications (23.1%), heavier course of the sickness (22.5%), as well as muscle, bone, and joint pains (15.0%). However, 17.8% of participants could not list any symptom differentiating the common cold from influenza and 3.1% of them believed that these conditions did not differ at all. The vast majority of participants (91.1%) were convinced that influenza infection could be dangerous for health; as its dangerous consequences, participants most often mentioned heart diseases (47.0%) and respiratory tract infections (27.8%).
When asked which groups of people “should by all means receive influenza vaccine,” participants in the first place mentioned elderly people (41.9%), children (36.9%), and people with low immunity to viral infections (25.0%). When asked who did not need to be vaccinated, participants mentioned healthy and immune people (12.7%), as well as the ill, including those with chronic diseases (11.1%). A considerable part of the participants did not know any contraindications for the vaccination (42.5%) and 4.7% mentioned pregnant and breastfeeding women as groups who should avoid vaccination.
According to 66.3% of the participants, it was best to receive vaccination in autumn. The majority of the participants (63.4%) were aware that influenza vaccination should be repeated every year. However, every fourth participant (25.6%) did not have an opinion on that subject. Almost 20% of the participants believed that influenza vaccination improved immunity to all viral infections. The belief that influenza vaccination protects against the avian influenza was shared by 7.2% of the participants. No major differences in patients’ knowledge of influenza were observed depending on age and sex.
Practice of influenza vaccination
There were 20.8% of the participants who had been vaccinated against influenza in the 12 months before the survey. This percentage was similar for both sexes (20.7% of men and 20.6% of women, P > 0.05). It was only slightly higher for older participants (19.2% in 18-54 age group and 23.8% in ≥55 age group, P > 0.05). Altogether 29.7% of participants had received vaccination in the previous years, 60.0% of whom had also received it in the 12 months before the survey. Vaccination was most often done in the primary health settings, work place, and patients’ homes (54.1%, 24.1%, and 18.0% of the vaccination cases, respectively). Before vaccination, fewer than three fourths of vaccinated participants were examined by a physician (74.4%). After vaccination, various adverse effects occurred in 60.2% individuals, most often local pain in the place of injection (34.6%), general bad feeling (24.1%), and muscle pains (12.0%). Majority of the vaccinated participants thought that vaccination had a positive effect on them (65.4%), although some had a contrary opinion (3.8%).
The majority of participants who had not had influenza vaccination in the 12 months before the study, explained it with good health, lack of belief in the vaccine effectiveness, and the high cost of the vaccine (Table 3). Women listed good health as the reason more often than men (33.1% vs 22.2%, P < 0.01), whereas men listed lack of belief in vaccine effectiveness more often than women (22.2% vs 13.4%, P < 0.01). Younger patients (18-54 years) listed good health as the reason considerably more often than older ones (31.4% vs 18.4%, P < 0.01).
Table 3.
Reasons for not taking the influenza vaccination among study participants from Poland*
| Percent of participants in age group |
|||
|---|---|---|---|
| Reason for not taking influenza vaccination | 18-54 years (n = 344) | 55 years and more (n = 163) | total (n = 507) |
| Good health |
31.4† |
18.4† |
27.2 |
| Lack of belief in vaccination effectiveness |
14.8 |
20.9 |
16.8 |
| High cost of vaccination |
9.3 |
10.4 |
9.7 |
| Lack of time |
10.8 |
5.5 |
9.1 |
| Used to treat influenza with natural remedies |
3.5 |
6.7 |
4.5 |
| Due to the health state (chronically sick, was sick in the vaccination period) |
2.9 |
2.5 |
2.8 |
| Did not have an opportunity to receive vaccination |
1.5 |
3.1 |
2.0 |
| Had vaccination in previous years, and thinks that it is not necessary to repeat it |
2.0 |
1.8 |
2.0 |
| Vaccination reduces immunity; once vaccinated, one have to repeat it every year |
2.3 |
0.6 |
1.8 |
| Difficult to say | 21.2 | 28.8 | 23.7 |
*For the open question “Why have you not taken a vaccine against influenza?”; patients were allowed to give more than one answer. This question was only answered by those who had not received vaccination within 12 mo before the study, hence the number is lower than the total number of participants (507 vs 640).
†χ2 test, P < 0.01.
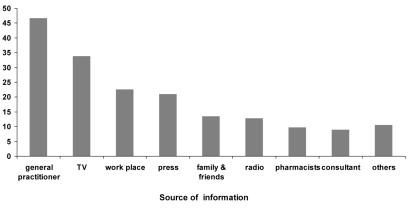
The participants most often learnt about the possibility of influenza vaccination from their family physicians, television, and at work place (Figure 1).
Figure 1.
Sources of participants’ knowledge on the possibility of influenza vaccination, as answers to a closed question. Percentages do not sum up to 100% since participants were allowed to give more than one answer.
Discussion
Our study found that low influenza vaccination coverage in Poland was related to patients’ false beliefs and high cost of influenza vaccination.
Influenza vaccination is a safe, effective, and cost-effective method of preventing influenza infections (11). However, the rate of influenza vaccination use in Poland is still unsatisfactory (7). Although it was growing systematically till 2004 (data from the years 1992-2002 indicate the growth of over 200 times, up to more than 100 doses per 1000 of population) (12), in the following years the trend was reversed, despite lack of problems with vaccination supply. In the epidemiological season 2007/08, only 9.5% of the Polish general population received the vaccine (13). Among persons aged 65 and over, the vaccine coverage increased only from 7% in 2004 to 14% in 2007 (7). The coverage of 13.9% of elderly people in Poland in the 2007/2008 season is the lowest of the 11 studied countries (13). A survey conducted in university hospitals found that only 22.3% of physicians, 10.6% of nurses, and 13.4% of medical students regularly took vaccines against influenza (14). Vaccination coverage among health care workers in Poland in the 2007/2008 season was 6.4%, the lowest among the 11 European countries studied (13).
These vaccination rates place Poland far behind other European countries, where vaccination coverage reaches 25% (15,16), or the USA, where in 2004/2005 season 42% of adults from high-risk groups received vaccination, as well as 62.7% of people aged over 65 years (17). The WHO encouraged member countries to reach the vaccination level of 75% among high-risk patient groups by the year 2010, as did the European Parliament. Recently, the Council of European Union has recommended reaching 75% vaccination coverage in older-age groups as early as possible, and preferably by the 2014-2015 winter season (18). Therefore, the need of popularizing influenza vaccination is of the uttermost importance in the Polish society, particularly in high-risk groups, such as the elderly and chronically ill, and among health care workers.
Participants in this study showed a considerable knowledge of influenza, its symptoms, ways of transmission, and complications. However, several illogicalities and misconceptions are worth pointing out. Over 90% of participants were convinced that influenza can be dangerous for health but only 42% of them believed that that the elderly were a priority population for vaccination. For 11% of participants, chronic conditions seemed to be contraindications to vaccination. Moreover, a large portion of participants could not point out any difference between influenza and other viral respiratory tract infections (common colds). Listing runny nose as a typical influenza symptom and believing that influenza vaccination was effective against all types of viral infections (almost 20% of participants) were also common misconceptions. These misconceptions are important, as in many cases, they may lower the motivation for the vaccination. This is especially important for those who had taken the vaccination before. For them, catching a different type of viral disease may prove the influenza vaccination to be ineffective. According to our study, only 60% of previously vaccinated participants had been revaccinated in the year before the survey. Therefore, there is a need for campaigns designed to increase the influenza vaccination rate in Poland that should clearly inform on the scope of influenza vaccination effectiveness and the differences between influenza and other viral respiratory tract infections.
Recent outbreak of the A(H1N1) 2009 virus (“swine flu”) and the pandemic announced by the WHO experts contributed greatly to this problem (19). Poland was the only EU country that refused to order pandemic vaccine for its citizens (20). The Ministry of Health announced an official statement in the Polish Parliament in which it not only underestimated the risk of the swine flu, but also questioned the effectiveness and safety of the pandemic vaccine (21). The Poles believed that message and it went in parallel with their reluctance toward vaccination: according to the Eurobarometer study, as many as 45% of the Poles believed that the vaccination against swine flu could not protect them from the infection (22). However, it seems that people extended that message to the regular influenza vaccination as well. Recent reports from infective season 2009/2010 prove that this “negative promotion” of influenza vaccination in the mass media was very effective: the coverage rates dropped to 6.5% of the general population (23).
The most frequently mentioned reason for not taking influenza vaccination was good health. However, it is noteworthy that nearly 10% of the participants mentioned financial aspects. Similar observations were made in other studies in Poland. Kroneman et al showed that in Poland in 2004 and 2005, 34% and 36% of participants from high-risk groups, respectively, had misconceptions preventing them from receiving vaccination (ie, they believed they were “resistant to influenza”), while 24% of the participants in both years stated that they would not have a vaccination due to financial difficulties (24). Kalinowski et al found that 37% of students did not receive vaccination due to belief in their good health and 6% due to the cost of the vaccine (25).
Some authors outside of Poland believe that the lack of improvement in influenza vaccination coverage in Poland over the last few years and a constant level of patients’ false beliefs point to a lack of effective national strategy for influenza vaccination promotion (26). The strategy should embrace free-of-charge provision of influenza vaccination, giving priority to the high-risk groups, especially the elderly (27). The need to pay for the vaccination out of pocket is a strong discouraging factor. In the USA, it was found that introducing a fee of US $10 for a vaccine would decrease the number of vaccinated people by 1/3 (28). At the same time, there is evidence that reimbursing costs of influenza vaccination increases vaccination coverage (29).
High percentage of people who made a conscious decision not to receive influenza vaccination in this survey and a lack of belief in the effectiveness of vaccination (16.8%) indicate that benefits of influenza vaccination should be demonstrated to the public, particularly to the high-risk groups.
This survey proved that primary health settings were not only the most frequent setting where influenza vaccination takes place, but also the most frequent source of information about the need for vaccination. This does not mean, however, that further action promoting vaccination against influenza should not be conducted at this level. The experience from other countries teaches us that family physicians are those who are most capable of persuading patients to receive influenza vaccination (16), and interventions taken at this level, including both physicians and patients, contribute to popularization of influenza vaccination (30,31). Personalized invitations to vaccination at family physicians’ practices are worth applying in the national program of influenza vaccination, as they were found to be particularly effective (27). The media, on the other hand, played hardly any role in the promotion of influenza vaccination in Poland (25). We hope that such situation will soon change.
The obvious limitation of this study is the method used for participants’ enrolment. Although the study was performed in a number of primary health care practices in Lodzkie voivodship and the study sample corresponds well with age and sex distribution of the Polish society (Table 1), the convenience sample, with overrepresentation of large-city dwellers, did not guarantee the full representativeness of the study for the Polish population. Moreover, the survey covered the people who visited their primary care physician. Thus, it could be biased toward people with greater interest in one’s health in general and influenza vaccination in particular. We could not perform further analysis of participants’ characteristics except sex and age because almost a quarter of them did not state their occupation or stated “other” in the questionnaire. Other characteristics were not collected.
Since major reasons for low influenza vaccination coverage in Poland include patients’ false beliefs and high cost of vaccination, it is necessary to organize informational campaigns that point out the differences between influenza and other viral respiratory tract infections, as well as to make the vaccination available free of charge, especially for high-risk groups.
Acknowledgments
Funding: None.
Ethical approval: Not required.
Declaration of authorship: PK gave the idea for the study and contributed to its execution. AZ contributed to the execution of the study and data management. JD contributed to study design and collection of the survey data. MS contributed to study design and execution, as well as to drafting of the manuscript.
Competing interests: All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author) and declare: no support from any organization for the submitted work; PK served as consultant to Boehringer Ingelheim Poland, Egis Poland, and Polpharma SA; other authors declare no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years; no other relationships or activities that could appear to have influenced the submitted work.
Additional Material
References
- 1.Romanowska M, Czarkowski MP, Nowak I, Staszewska E, Donevski S, Brydak LB. Influenza in Poland in 2008. Przegl Epidemiol. 2010;64:175–9. [in Polish] [PubMed] [Google Scholar]
- 2.Czarkowski MP, Romanowska M, Nowak I, Brydak LB. Influenza in Poland in 2006. Przegl Epidemiol. 2008;62:235–40. [in Polish] [PubMed] [Google Scholar]
- 3.Jick H, Hagberg KW. Effectiveness of influenza vaccination in the United kingdom, 1996-2007. Pharmacotherapy. 2010;30:1199–206. doi: 10.1592/phco.30.12.1199. [DOI] [PubMed] [Google Scholar]
- 4.Regulation of the Minister of Health of 19 December 2002 on the list of mandatory vaccination and the rules of conduct and documentation of vaccination [in Polish]. Available from: http://www.pis.gov.pl/?dep=141. Accessed: March 28, 2011.
- 5.Anonymous Family physicians from Lodz provide vaccination for free. Praktyka Lekarska. 2008;45:6. [in Polish] [Google Scholar]
- 6.Nichol KL, Treanor JJ. Vaccines for seasonal and pandemic influenza. J Infect Dis. 2006;194(Suppl 2):S111–8. doi: 10.1086/507544. [DOI] [PubMed] [Google Scholar]
- 7.Nitsch-Osuch A, Wardyn K. Influenza vaccine coverage in age-related risk groups in Poland, 2004-2007. Cent Eur J Public Health. 2009;17:198–202. doi: 10.21101/cejph.a3536. [DOI] [PubMed] [Google Scholar]
- 8.Kramarz P, Ciancio B, Nicoll A. Seasonal and pandemic influenza vaccines for the elderly and other risk groups: a review of available data. Pol Arch Med Wewn. 2009;119:654–9. [PubMed] [Google Scholar]
- 9.Mereckiene J, Cotter S, D'Ancona F, Giambi C, Nicoll A, Levy-Bruhl D, et al. Differences in national influenza vaccination policies across the European Union, Norway and Iceland 2008-2009. Euro Surveill. 2010;15. pii: 19700. [DOI] [PubMed] [Google Scholar]
- 10.Central Statistical Office. Demographic yearbook of Poland 2010. Warsaw: Central Statistical Office; 2010. [Google Scholar]
- 11.Nichol KL. Efficacy and effectiveness of influenza vaccination. Vaccine. 2008;26(Suppl 4):D17–22. doi: 10.1016/j.vaccine.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 12.Brydak LB. Is it possible to fight with influenza in 21st century? Zakazenia. 2002;3-4:62–9. [in Polish] [Google Scholar]
- 13.Blank PR, Schwenkglenks M, Szucs TD. Vaccination coverage rates in eleven European countries during two consecutive influenza seasons. J Infect. 2009;58:446–58. doi: 10.1016/j.jinf.2009.04.001. [DOI] [PubMed] [Google Scholar]
- 14.Zielonka TM, Lesinski J, Zycinska K, Machowicz R, Wardyn AK. Vaccination against influenza in medical staff of Warsaw university hospitals and in students of Warsaw Medical University. Med Pr. 2009;60:369–76. [in Polish] [PubMed] [Google Scholar]
- 15.Popowicz W, Wysocki J. Threat of pandemic flu and protective vaccinations. Zakazenia. 2006;5:133–9. [in Polish] [Google Scholar]
- 16.Blank PR, Schwenkglenks M, Szucs TD. Influenza vaccination coverage rates in five European countries during season 2006/07 and trends over six consecutive seasons. BMC Public Health. 2008;8:272. doi: 10.1186/1471-2458-8-272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Centers for Disease Control and Prevention (CDC) Estimated influenza vaccination coverage among adults and children–United States, September 1, 2004-January 31, 2005. MMWR Morb Mortal Wkly Rep. 2005;54:304–7. [PubMed] [Google Scholar]
- 18.Council recommendation of 22 December 2009 on seasonal influenza vaccination, Official Journal of the European Union L 348, 71-2. Available from: http://eur-lex.europa.eu/LexUriServ/LexUriServ.do?uri=OJ:L:2009:348:0071:0072:EN:PDF. Accessed: March 31, 2011.
- 19.Plusa T. Contemporary threat of influenza virus infection. Pol Merkur LekarskiPol Merkuriusz Lek. 2010;28:5–7. [in Polish] [PubMed] [Google Scholar]
- 20.Smith J. WHO official says impact of Poland’s anti-vaccine stance yet to be seen. Elsevier Global Medical News. Available from: http://www.thelancet.com/H1N1-flu/egmn/0c03e13a. Accessed: March 28, 2011.
- 21.Minister Fronczak’s setback after setback due to the swine flu. Available from: http://wiadomosci.gazeta.pl/Wiadomosci/1,80708,7231427,Wpadka_za_wpadka_ministra_Fronczaka__Przez_swinska.html Accessed: March 31, 2011.
- 22.European Comission. Eurobarometer on Influenza H1N1, Flash EB Series #287, March 2010. Available from: http://ec.europa.eu/cyprus/news/20100303_flash_eb_on_influenza_en.htm. Accessed: March 28, 2011.
- 23.Anonymous Doctors themselves do not follow epidemiologists’ advices on vaccinations. Puls Medycyny. 2010;14:10–1. [in Polish] [Google Scholar]
- 24.Kroneman MW, van Essen GA. Stagnating influenza vaccine coverage rates among high-risk groups in Poland and Sweden in 2003/4 and 2004/5. Euro Surveill. 2007;12:E1–2. doi: 10.2807/esm.12.04.00696-en. [DOI] [PubMed] [Google Scholar]
- 25.Kalinowski P, Piechnik B, Pocińska K, Szarek K, Karwat ID. Knowledge of methods of prophylaxis and treatment of influenza and its complications among first year students. Przegl Epidemiol. 2005;59:69–74. [in Polish] [PubMed] [Google Scholar]
- 26.Kroneman MW, van Essen GA. Stagnating influenza vaccine coverage rates among high-risk groups in Poland and Sweden in 2003/4 and 2004/5. Euro Surveill. 2007;12:E1–2. doi: 10.2807/esm.12.04.00696-en. [DOI] [PubMed] [Google Scholar]
- 27.Kroneman M, van Essen GA, John Paget W. Influenza vaccination coverage and reasons to refrain among high-risk persons in four European countries. Vaccine. 2006;24:622–8. doi: 10.1016/j.vaccine.2005.08.040. [DOI] [PubMed] [Google Scholar]
- 28.Steiner M, Vermeulen LC, Mullahy J, Hayney MS. Factors influencing decisions regarding influenza vaccination and treatment: a survey of healthcare workers. Infect Control Hosp Epidemiol. 2002;23:625–7. doi: 10.1086/501984. [DOI] [PubMed] [Google Scholar]
- 29.Blank PR, Freiburghaus AU, Ruf BR, Schwenkglenks MM, Szucs TD. Trends in influenza vaccination coverage rates in Germany over six seasons from 2001/02 to 2006/07. Med Klin (Munich) 2008;103:761–8. doi: 10.1007/s00063-008-1121-0. [DOI] [PubMed] [Google Scholar]
- 30.Humair JP, Buchs CR, Stalder H. Promoting influenza vaccination of elderly patients in primary care. Fam Pract. 2002;19:383–9. doi: 10.1093/fampra/19.4.383. [DOI] [PubMed] [Google Scholar]
- 31.Nicoleau A, Nicoleau CA, Balzora JD, Oboh A, Siddiqui N, Rosenberg C. Elderly African-Americans and the influenza vaccine: the impact of the primary care physicians. J Am Med Dir Assoc. 2001;2:56–9. doi: 10.1016/S1525-8610(04)70161-9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.