Abstract
Objective
The aim of this study is to describe the interdisciplinary care, including chiropractic services, in a military health care facility of an active duty member of the United States Navy with low back pain, leg pain, and foot numbness.
Clinical Features
A 40-year-old patient developed low back pain, leg pain, and foot numbness after moving furniture. The patient described his symptoms as pain in the right low back, pain shooting into the right lateral thigh and lower leg, and numbness into the right lateral foot. Magnetic resonance imaging confirmed disk extrusion at L4/L5 occupying the lateral recess and abutting the exiting right L5 nerve root.
Intervention and Outcome
Providers, including primary care, chiropractic, and orthopedics, in an established multidisciplinary health care system contributed to the case management. The patient received 11 chiropractic treatments (spinal manipulation, flexion-distraction, abdominal rehab exercises) over 72 days. Subjective complaints resolved, and the patient was released back to full duty.
Conclusion
Integrative care, using medical and chiropractic services, was successful in the conservative management of a patient with low back pain and radicular symptoms secondary to disk extrusion.
Key indexing terms: Manipulation, spinal; Intervertebral disk displacement; Military medicine; Patient care team; Military personnel; Chiropractic
Introduction
Low back pain (LBP) is a major concern to the military.1 Active duty service members may be predisposed to both acute and chronic episodes of LBP, related to their high levels of physical activity. Essential to operational readiness, military physical training programs are used to maintain physical fitness.2 Active duty service members are required to complete a physical readiness test every 6 months. Performance is graded,3 with a less than satisfactory performance leading to a probationary status. Disability discharges related to back conditions are issued when a service member cannot perform his or her job and/or complete the required physical readiness test satisfactorily. A study of 15 268 active duty military personnel hospitalized for musculoskeletal conditions concluded that back conditions had the greatest 5-year cumulative risk of disability, with 40% being related to intervertebral disk displacement and degeneration.4
The clinical management of service members with disk degeneration or injury may be a challenge in the military setting. Each member has a primary care manager (PCM), who manages and coordinates the care of each patient. Deployments, temporary duty assignments, and patient compliance all affect the smooth transition of care between specialists and, ultimately, the outcome of each case. Considering the direct and indirect costs of back surgery5 and the impact surgery may have on a service member's career, it becomes imperative that, when appropriate, nonoperative therapy is included in the management of these cases. Since the addition of their services to the military health care system in 1995, chiropractic physicians have become part of the health care delivery team at 49 military treatment facilities in the United States. An additional 11 sites are scheduled to be opened, including 3 overseas, by the end of 2009.6
This case review demonstrates how one patient, with a confirmed disk extrusion at L4/L5, achieved a successful outcome after interdisciplinary management in a military treatment facility that included chiropractic services.
Case report
A 40-year-old male active duty United States Naval Petty Officer first class presented to his PCM with complaints of LBP, pain shooting into the right lateral thigh and lower leg, and numbness into the right lateral foot. The patient's job consisted of a variety of responsibilities, including desk work, heavy lifting, and a considerable amount of travel, which involved sitting several hours in the back of a C-130 transport plane traveling to and from work sites.
Having experienced mild, intermittent bouts of LBP since driving a truck long distance 4 years prior, this was his first ordeal with pain or numbness into either lower extremity. This episode began after lifting furniture while moving to a new house. The PCM's working diagnosis was LBP with radiculopathy into the right lower extremity to the foot. This patient was part of an elite Navy squadron, with which he was required to travel a considerable amount of the time, both stateside and overseas.
The first clinical contact the patient had for this condition was with his PCM, a naval flight surgeon. It took place 4 days after the onset of pain. Besides the right leg pain, he had experienced transient right testicular pain that lasted for 2 days. No bowel or bladder changes, or lower extremity weaknesses were noted. The PCM prescribed 800 mg ibuprofen and 975 mg acetaminophen twice daily. Lumbar radiographs and a magnetic resonance imaging (MRI) were ordered, and consults were placed to both chiropractic and orthopedic services. The patient was instructed to schedule a follow-up appointment with the PCM after seeing the orthopedic specialist or if symptoms worsened. Over the course of the next 2 weeks, he continued to work with limitations on lifting and exercise, and took his medications as prescribed.
Initial presentation to the chiropractic clinic was 14 days after the appointment with his PCM. The patient indicated that his chief complaint was constant dull aching pain in the low back, radiating into the right “hip” (sacroiliac joint), buttock, and leg and numbness in the lateral right foot. An examination was performed (Fig 1), and copies of a noncontrast MRI were reviewed. This revealed a prominent disk extrusion at L4/L5, occupying the lateral recess and abutting the right L5 nerve root. There was also prominent posterior bulging at L5/S1 (Fig 2).
Fig 1.
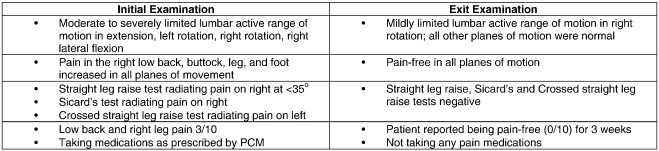
Examination findings.
Fig 2.

Sagittal T2-weighted MRI without contrast showed posterior disk extrusion at the L4/L5 level and diminished disk height with posterior bulging at L5/S1.
The initial chiropractic treatment plan was for appointments 3 times per week for 2 weeks. Treatments consisted of interferential therapy,7 cryotherapy,8,9 moist heat, flexion/distraction,10,11 prone spinal manipulative therapy12,13 with drop pieces, side posture spinal manipulative therapy, and core conditioning exercises14,15 with postural modifications. In addition to these physical techniques and modalities, nutritional16-18 and psychosocial factors19,20 were included in the treatment plan.
The patient's first orthopedic consultation was 33 days after his symptoms began. The orthopedic surgeon recommended surgery; however, spine surgery was not available at this naval hospital. Therefore, a consult was placed with a spine surgeon in the civilian community. By this time, the patient had completed 7 chiropractic appointments.
Another 22 days passed before the patient was seen by the spine surgeon. This was 51 days after originally presenting to his PCM. While waiting to be seen by the spine surgeon, the patient stated that he was compliant with his prescribed home exercise program and he continued with chiropractic management. At the time he presented to the spine surgeon, the patient had kept 9 appointments with the chiropractic physician. The spine surgeon advised against surgical intervention and scheduled one follow-up appointment. The patient continued with chiropractic care.
Seventy-two days after initially seeking care, the patient presented to the chiropractic clinic for his last appointment. The patient had resumed his normal work activities. Indicating that he had been keeping up with the core exercises as prescribed, he reported being pain-free for 3 weeks, had regained the feeling in his toes, and was no longer taking pain medications. After an exit examination (Fig 1), he was released from active care, with instructions to call for an appointment if there were any exacerbations. Later the same day, he kept his second appointment with the civilian spine surgeon, who released him from care.
Throughout the course of care, the patient was on light duty, limiting his exercise to specific activities prescribed by the chiropractic physician. Once released, he returned to his regular exercise routine and was able to perform all required Navy Physical Readiness Tests. Required every 6 months, a passing score for his age group would require him to do 39 crunches and 32 push-ups (having 2 minutes to do each). Also required is to run 1.5 miles in at least 14:45, or swim 500 yards in 12:30.3
In summary, the patient was initially seen by his PCM, who prescribed medications, ordered imaging studies, and placed referrals to chiropractic and orthopedics. Working in the same area as the patient, the PCM was able to monitor progress and coordinate changes to medical follow-up if necessary. The patient was seen 11 times by the chiropractic physician and 3 times by orthopedic surgeons. Before submission for publication, the patient provided consent to have elements of case management published without personal identifiers.
Discussion
This article has described the case management of an active duty United States Navy Petty Officer who presented to his PCM with LBP and right leg pain. Radiologic studies confirmed posterior disk extrusion at L4/L5, abutting the right L5 nerve root, and posterior bulging of the L5/S1 disk.
The primary purpose of this case report was to describe the interdisciplinary collaboration of chiropractic and medical services in a military setting. This article does not go into detail of the chiropractic treatments rendered, as several studies and trials on the use of manipulation and other forms of conservative care to treat patients with acute lumbar radiculopathy may be found in a systematic review by Lawrence et al.21 Rather, it hoped to depict the unique inclusion of chiropractic management as part of available treatments within a military treatment facility.
Integration of chiropractic services into multidisciplinary and military health care facilities is relatively new. This naval hospital added chiropractic services in 2003. Chiropractic in the military is considered a specialty service; therefore, patients are directed to the chiropractic clinic by referral from their PCM. Military health care uses electronic medical records. The referral process is built into the electronic medical record program, making it a simple undertaking. When the PCM decides which specialist(s) a patient should see, a brief history and the diagnosis are entered and sent electronically directly to the specialty clinic as a referral. Each incoming referral to this particular chiropractic clinic is screened by a chiropractic assistant, who will then approve access for an appointment. In this clinic, the patient may contact the chiropractic clinic directly or call a central appointment number to schedule the initial appointment. The chiropractic physician reviews all referrals before the appointment and, if there are any questions, will contact the referring provider.
Health care notes are entered into the electronic medical record with each visit. Available for all military providers to view, this allows various providers the ability to review respective cases, keeping abreast of all treatments and patient progress. The PCM may survey each case by opening the relevant electronic case file. In the chiropractic clinic, periodic examinations are performed to monitor progress. Once a patient has met established goals or it is deemed maximum improvement has been attained, it is noted in the record; and the patient is released with verbal instructions to follow up with the PCM or as needed in the chiropractic clinic. If there is lack of sufficient progress other follow-up may occur, which includes the patient being released back to the PCM.
Military electronic medical records are maintained in a secure network. If a patient is sent off base for care, that provider does not have direct access to the electronic notes; and arrangements must be made for applicable notes to be delivered. After appointments off base, the daily notes will be sent to the naval hospital, which will then be scanned into the record.
Many military providers may not be familiar with chiropractic. Each facility may vary as to what services are offered. As an example, this chiropractic physician is contracted to provide services to active duty beneficiaries. Attending a weekly meeting with specialty providers is encouraged, at which time specific cases are discussed. Specialists at the weekly meeting often have exchanges on evidence-based approaches to care; this includes evidence supporting chiropractic care. The PCM responsible for overall management of the patient described in this article had visited the chiropractic clinic and was familiar with the approach to care. Other examples of chiropractic integration in this facility include family medicine residents observing in the chiropractic clinic, the chiropractic physician doing in-service presentations, and chiropractic representation on sports medicine and research teams. These open lines of communication between providers have helped chiropractic become better integrated in this particular facility.
Limitations
In this case, the relative contribution of any specific treatment or modality in the interdisciplinary approach to care is unclear. The possibility of natural course of the disorder or spontaneous remission must also be considered. The patient response in this case may not necessarily be the same as others.
Conclusion
The results show integrative and interdisciplinary health care, which includes the integration of chiropractic services in a military treatment facility, may provide a beneficial treatment option for active duty service members. More research is needed to help providers differentiate which patients will respond best from a combined treatment approach including chiropractic care.
Funding sources and conflicts of interest
The views, positions, and/or opinions of this article are those of the author and do not necessarily reflect the policies of the Departments of Defense and Navy.
There were no funding source or conflicts of interest identified.
The author is a contract provider with the Department of Navy, providing chiropractic services for Naval Hospital Pensacola, FL.
Acknowledgment
The author thanks Mark Goto, MD, and Jerrilyn Cambron, DC, PhD, for assistance in organizing and editing of this paper and Ms Connie C Walker for assistance with literature searches.
Footnotes
The views, positions, and/or opinions of this article are those of the author and do not necessarily reflect the policies of the Departments of Defense and Navy.
References
- 1.Woodruff S., Conway T., Bradway L. The U.S. Navy healthy back program: effect on back knowledge among recruits. Mil Med. 1994;159(7):475–484. [PubMed] [Google Scholar]
- 2.Kaufman K., Brodine S., Shaffer R. Military training-related injuries: surveillance, research, and prevention. Am J Prev Med. 2000;18(3S):54–63. doi: 10.1016/s0749-3797(00)00114-8. [DOI] [PubMed] [Google Scholar]
- 3.Physical readiness test standards, appendix A. OPNAVINST 6110.1H; 15AUG05. Available at http://www.jag.navy.mil/careers/careers/docs/PRT.pdf.
- 4.Lincoln A., Smith G., Amoroso P., Bell N. The natural history and risk factors of musculoskeletal conditions resulting in disability among US Army personnel. Work. 2002;18(2):99–113. [PMC free article] [PubMed] [Google Scholar]
- 5.Tosteson A., Lurie J., Tosteson T., Skinner J., Herkowitz H., Albert T. Surgical treatment of spinal stenosis with and without degenerative spondylolisthesis: cost-effectiveness after 2 years. Ann Intern Med. 2008;149(12):845–853. doi: 10.7326/0003-4819-149-12-200812160-00003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.TRICARE Management Activity [homepage on the internet]. Falls Church (VA). Designated locations. [updated 2007 Apr 10; cited 2009 Aug 03]. http://www.tricare.mil/mybenefit/home/overview/SpecialPrograms/ChiropracticCare/DesignatedLocations.
- 7.Jorge S., Parada C.A., Ferreira S.H., Tambeli C.H. Interferential therapy produces antinociception during application in various models of inflammatory pain. Phys Ther. 2006;86:800–808. [PubMed] [Google Scholar]
- 8.French S.D., Cameron M., Walker B.F., Reggars J.W., Esterman A.J. A Cochrane review of superficial heat or cold for low back pain. Spine. 2006;31:998–1006. doi: 10.1097/01.brs.0000214881.10814.64. [DOI] [PubMed] [Google Scholar]
- 9.Hubbard T.J., Denegar C.R. Does cryotherapy improve outcomes with soft tissue injury? J Athl Train. 2004;39(3):278–279. [PMC free article] [PubMed] [Google Scholar]
- 10.Gudavalli M.R., Cambron J.A., McGregor M., Jedlicka J., Keenum M., Ghanayem A.F. A randomized clinical trial and subgroup analysis to compare flexion-distraction with active exercise for chronic low back pain. Eur Spine J. 2006;15(7):1070–1082. doi: 10.1007/s00586-005-0021-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cambron J.A., Gudavalli M.R., Hedeker D., McGregor M., Jedlicka J., Keenum M. One-year follow-up of a randomized clinical trial comparing flexion distraction with an exercise program for chronic low back pain. J Altern Complement Med. 2006;12(7):659–668. doi: 10.1089/acm.2006.12.659. [DOI] [PubMed] [Google Scholar]
- 12.Chou R., Qaseem A., Snow V., Casey D., Cross J.H., Shekelle P. Diagnosis and treatment of low back pain: a joint clinical practice guideline from the American College of Physicians and the American Pain Society. Ann Intern Med. 2007;147:478–491. doi: 10.7326/0003-4819-147-7-200710020-00006. [DOI] [PubMed] [Google Scholar]
- 13.Chou R., Hoyt Huffman L. Nonpharmacologic therapies for acute and chronic low back pain: a review of the evidence for an American pain society/American college of physicians clinical practice guideline. Ann Intern Med. 2007;147:492–504. doi: 10.7326/0003-4819-147-7-200710020-00007. [DOI] [PubMed] [Google Scholar]
- 14.Stanton T., Kawchuk G. The effect of abdominal stabilization contractions on posteroanterior spinal stiffness. Spine. 2008;33:694–701. doi: 10.1097/BRS.0b013e318166e034. [DOI] [PubMed] [Google Scholar]
- 15.McGill S.M. Stability: from biomechanical concept to chiropractic practice. J Can Chiropr Assoc. 1999;43(2):75–88. [Google Scholar]
- 16.James M.H., Gibson R.A., Cleland L.G. Dietary polyunsaturated fatty acids and inflammatory mediator production. Am J Clin Nutr. 2000;71(1 Suppl):3435–3485. doi: 10.1093/ajcn/71.1.343s. [DOI] [PubMed] [Google Scholar]
- 17.Simopoulos A.P. Essential fatty acids in health and chronic disease. Am J Clin Nutr. 1999;70(3 Suppl):5605–5695. doi: 10.1093/ajcn/70.3.560s. [DOI] [PubMed] [Google Scholar]
- 18.Simopoulos A.P. Omega-3 fatty acids in inflammation and autoimmune diseases. J Am Coll Nutr. 2002;21:495–505. doi: 10.1080/07315724.2002.10719248. [DOI] [PubMed] [Google Scholar]
- 19.Thomas E., Silman A.J., Croft P.R., Papageoraiou A.C., Jayson M.I., Macfarlane G.J. Predicting who develops chronic low back pain in primary care: a prospective study. BMJ. 1999;318(7199):1662–1667. doi: 10.1136/bmj.318.7199.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Macfarlane G., Jones G.T., Hannaford P.C. Managing low back pain presenting to primary care: where do we go from here? Pain. 2006;122(3):219–222. doi: 10.1016/j.pain.2006.03.013. [DOI] [PubMed] [Google Scholar]
- 21.Lawrence D., Meeker W., Branson R. Chiropractic management of low back pain and low back-related leg complaints: a literature synthesis. J Manipulative Physiol Ther. 2008;31(9):659–674. doi: 10.1016/j.jmpt.2008.10.007. [DOI] [PubMed] [Google Scholar]


